Abstract
The Ebola outbreak in West Africa precipitated a renewed momentum to ensure global health security through the expedited and full implementation of the International Health Regulations (IHR) (2005) in all WHO member states. The updated IHR (2005) Monitoring and Evaluation Framework was shared with Member States in 2015 with one mandatory component, that is, States Parties annual reporting to the World Health Assembly (WHA) on compliance and three voluntary components: Joint External Evaluation (JEE), After Action Reviews and Simulation Exercises. In February 2016, Tanzania, was the first country globally to volunteer to do a JEE and the first to use the recommendations for priority actions from the JEE to develop a National Action Plan for Health Security (NAPHS) by February 2017. The JEE demonstrated that within the majority of the 47 indicators within the 19 technical areas, Tanzania had either ‘limited capacity’ or ‘developed capacity’. None had ‘sustainable capacity’. With JEE recommendations for priority actions, recommendations from other relevant assessments and complementary objectives, Tanzania developed the NAPHS through a nationwide consultative and participatory process. The 5-year cost estimate came out to approximately US$86.6 million (22 million for prevent, 50 million for detect, 4.8 million for respond and 9.2 million for other IHR hazards and points of entry). However, with the inclusion of vaccines for zoonotic diseases in animals increases the cost sevenfold. The importance of strong country ownership and committed leadership were identified as instrumental for the development of operationally focused NAPHS that are aligned with broader national plans across multiple sectors. Key lessons learnt by Tanzania can help guide and encourage other countries to translate their JEE priority actions into a realistic costed NAPHS for funding and implementation for IHR (2005).
Keywords: health policy, public health, review
Background
The Ebola virus disease (EVD) epidemic in West Africa (2014–2016) demonstrated a huge negative impact in terms of loss of lives, livelihoods, community disruption and wider socioeconomic losses.1 2 The economic loss in the most affected countries was estimated to be US$2.2 billion, or approximately 16% of their collective income.2–4 Moreover, the global effort to stop the EVD from spreading to other countries cost >US$3.8 billion.5–7
The latter clearly shows that a single public health emergency like EVD in countries with fragile health systems and limited preparedness and response capacity can drastically set back development gains by several years, including any gains made on health systems strengthening. The investment case therefore for building the core capacities for prevention and rapid control of public health threats in the United Republic of Tanzania is compelling.
In Tanzania, a major rift valley fever (RVF) outbreak in 2007 had major consequences on rural household livelihoods, food security and nutrition, in addition to causing direct and indirect losses to livestock producers.8 9 An economic impact assessment study carried out in 2008 demonstrated the negative impact of the RVF outbreak on international animal trade.8 In 2006, 2594 cattle were exported to the Comoros Islands. However, in 2007 the number dropped to 1183, a 54% decline in exports.8 Furthermore, the Government spent another US$3.84 million to control the RVF outbreak.8 9
The Ebola epidemic created renewed momentum in global health security, including impetus for effective implementation of IHR (2005) in all WHO member states by developing core capacities for preventing, detecting and responding to public health emergencies. In an effort to improve health security, in 2015 Tanzania joined the Global Health Security Agenda (GHSA).10 The GHSA was initiated by the USA in collaboration with a number of countries, international organisations and civil society with the aims to make the world safer and more secure from infectious disease threats, and to promote global health security as required under the IHR (2005).11 12 One of the activities of the GHSA was to develop an external country assessment process for health security. In 2015, WHO in developing the new IHR Monitoring and Evaluation Framework, worked with partners to harmonise the GHSA tool, with other existing tools, and the IHR monitoring tool to create the Joint External Evaluation (JEE) tool.13
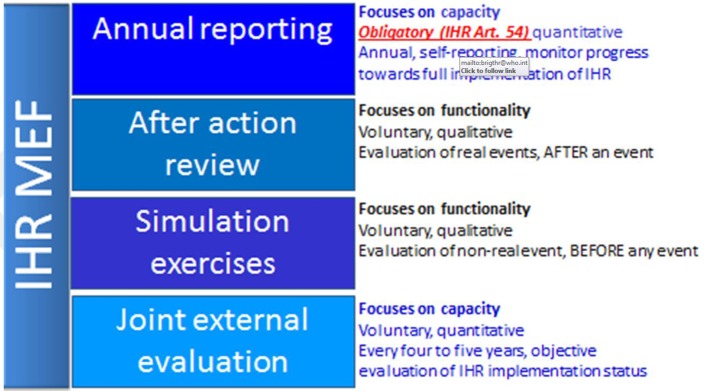
With a revised approach to IHR (2005) core capacity monitoring and evaluation recommended by the IHR review committee (A69/21.2) and the 68th World Health Assembly (Resolution WHA68/22), the JEE fit within the post 2015 IHR monitoring and evaluation framework (IHR-MEF) that consisted of one mandatory component ‘annual reporting’ from all Member States with three voluntary components—JEE, After Action Reviews and Simulation Exercises.14
The JEE process involves the country first conducting a self-evaluation using the JEE tool, and the findings are then validated by independent external subject matter experts during a peer-to-peer evaluation within the country that includes site visits to facilities.13 The JEEs are organised under WHO’s leadership and coordination. It brings various sectors together to jointly identify the most urgent needs within their health security system; to prioritise opportunities for enhanced preparedness, response and action and to engage with current and prospective donors and partners to effectively target resources.15
The National Action Plan for Health Security (NAPHS), also voluntary and supported by WHO on request, takes the approximately 60 priority action recommendations from the JEE to develop a costed national plan to improve the country’s health security under the IHR. By its nature and as it brings all relevant analyses and information onto one common platform, it can act as important political capital to solicit and prioritise allocation of domestic and external resources.16
To date, over 60 JEEs have been conducted globally, with numerous country-specific priority activities identified.17 However, very few countries have embarked on the development of NAPHS following the JEE. To ensure IHR (2005) capacity development, WHO and health development partners (HDP) are strongly encouraging national governments to commit to conducting assessments (JEE) and to ensure that the results of these assessments are translated into costed actions plans, supported by financing proposals and investment cases. Moreover, the political-will must be found to commit tax resources to finance preparedness; ensure donors fulfil their commitments; promote private sector engagement and help ensure that the economic risks of outbreaks are factored into macroeconomic assessments and financial sectors investment decision-making at par with other systematic risks.
WHO and HDP are supporting countries to develop costed NAPHS aligned with broader strategies for building resilient health systems.12 13 Tanzania’s experience is therefore timely. Key lessons learnt by Tanzania can help guide and encourage other countries to translate the priority actions from the JEE into a realistic costed NAPHS for funding and implementation for expedited IHR (2005) core capacity building.
Process for developing the NAPHS
The JEE and other complementary assessments
The JEE evaluated IHR core capacities in 19 technical areas using 48 indicators categorised under: prevent, detect, respond and other IHR hazards and points of entry (PoE).14 Core capacities were graded from score 1 (no capacity) to score 5 (sustainable capacity). Out of the 19 technical areas assessed, none had attained ‘sustainable capacity’ (score 5), while the majority of technical areas had either ‘limited’ or ‘developed’ capacity (score 2 and 3) (table 1).18
Table 1.
Summary scores from Joint External Evaluation, February 2016
| No capacity Score 1 |
Limited capacity Score 2 |
Developed capacity Score 3 |
Demonstrated capacity Score 4 |
| Antimicrobial resistance Emergency operation centre |
National legislation, policy and financing Zoonotic disease Food safety Biosafety and biosecurity Reporting Workforce development (animal workforce) Preparedness Linking public health and security measures Medical countermeasures and personnel deployment Risk communication Points of entry Radiation emergencies |
International health regulations coordination, communication and advocacy National laboratory system Chemical events |
Immunisation Real-time surveillance Workforce development (FELTP) |
FELTP, Field Epidemiology and Laboratory Training Programme.
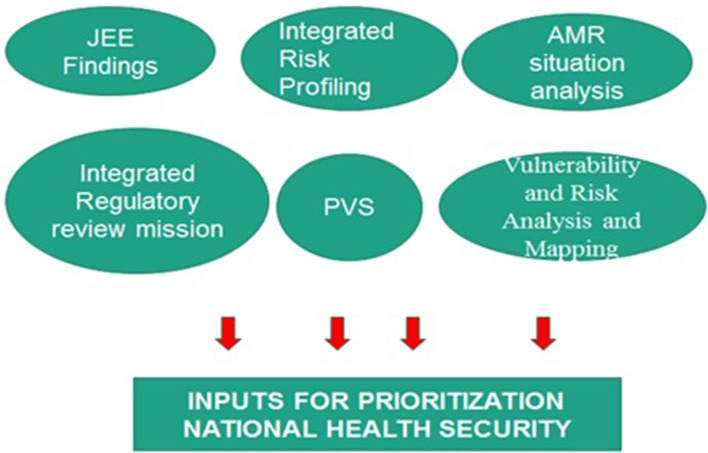
In Tanzania, following the JEE, a detailed situation analysis was conducted by the Ministry of Health, Community Development, Gender, Elderly and Children (MoH-CDGEC) and other relevant sectors to consolidate the JEE and other complementary assessment recommendations (ie, situation analysis on antimicrobial resistance; the disaster vulnerability and the risk assessment and mapping and integrated risk profiling, the World Organisation for Animal Health (OIE) tool for the evaluation of Performance of Veterinary Services (PVS) report). This consolidation of all assessments during the NAPHS development ensured that the planning took into account all the available information with respect to health security in the country (figure 1).
Figure 1.
Integrated review process for setting key priorities and objectives. AMR, antimicrobial resistance; JEE, Joint External Evaluation; PVS, Performance of Veterinary Services.
Planning workshop, November 2016
The Government of Tanzania through the Office of the Prime Minister (PMO), the MoH-CDGEC, the Ministry of Agriculture, Livestock and Fisheries, the Vice President’s Office—Environment, the Ministry of Defence National Service and the Ministry of Home Affairs, worked with WHO (all three levels) and HDP to identify priorities to be included in a 5-year NAPHS. The authorities of six African countries that completed JEEs attended the workshop to use Tanzania experiences in development of NAPHS for their home countries (online supplementary annex 1). A number of progressive criteria were used to review the priorities and develop key actions (box 1).
Box 1. Example of criteria employed to review priorities.
Based on the identified priorities for the 19 technical areas, are there any critical technical gaps that need to be addressed?
Are the activities nominated for inclusion in NAPHS realistic, relevant and achievable with clear milestones and measures from a planning and costing context?
Will activities that are listed in NAPHS develop the health security capacity in a sustainable way and do they take into consideration health systems strengthening and sector-wide development?
bmjgh-2017-000600supp001.pdf (23.9KB, pdf)
Cost driver exercise
After prioritisation of the activities, a cost driver exercise was conducted to categorise the activities into low, moderate or high costs using prior experiences in national procurement. Second, from the priorities with high costs, the major activities and inputs for implementation were identified. From the list, three groups were identified: (1) those that are in the Government’ s budget; (2) those that are not in the Government’s budget but have a development partner or has shown interest and (3) those that are neither in the Government’s budget nor have a development partner (table 2).
Table 2.
Costs drivers for the respond thematic area
| Respond | Categories |
| Preparedness | 3 |
| Emergency response operations | 3 |
| Linking public health and law enforcement | 1 |
| Medical countermeasures | 3 |
| Risk communication | 2 |
Category 1: meetings, trainings.
Category 2: vehicles procurement, procurement of equipment.
Category 3: infrastructure development, buying plots, buildings.
Formulating a coordination mechanism
The planning process also identified the need for a high-level coordination platform to map and ensure collaboration between multiple sectors. This platform will also ensure coordination with other existing plans (including disease-specific plans) at all administrative levels of the country. The goal of this mechanism is to limit duplication in resource mapping and planning, and maximise synergies with the National Health Sector Strategic Development Plan (NHSSDP). Moreover, a national coordination mechanism will also allow Tanzania to proactively position available scarce resources from specific programmes into sector-wide development of health systems capable of addressing all hazards and will streamline monitoring and accountability without jeopardising the ongoing objectives of disease-specific programmes.
Costing and NAPHS finalisation workshop, February 2017
In February 2017, the Government of Tanzania convened a follow-up workshop with the same key partners who participated in the November 2016 planning meeting to facilitate a final review of the priorities, sequencing of prioritised activities and costing of the 5-year NAPHS (box 2) (online supplementary annex 1).
Box 2. Criteria employed for final review of the priorities to be costed.
Are the activities considered for costing realistic, measurable and will they exert impact and efficiency to corresponding objective(s) and health systems approach?
Has the technical area adequately considered the activities that will allow the country to demonstrate progress from lower to higher scores as per the Joint External Evaluation tool criteria?
Does the plan allow the country to maintain the capacities in areas where it has showed demonstrated capacities (scores 4–5)?
Do the activities under this technical area identify and include other sectors and levels to ensure a ‘One Health’ approach to health system strengthening?
Do the activities follow a sequential or phased approach (year 1, 2, 3–5) for the plan operationalisation commensurate with resource availability, mobilisation and prediction?
Does the technical area use the best available data to categorise activities in terms of domestic vs external funding?
Has a responsible ministry or ministries/office or offices been identified for implementation?
The process led to a final list of objectives, targets, summary of planned activities and inputs including unit costs. For unit costs, the existing Government procurement guidelines were used and where data were not available, other authoritative sources such as WHO procurement references used.
In the interest of M&E and risk mitigation, participants also reviewed the draft NAPHS and formulated monitoring/performance indicators for the overall plan and individual technical areas. Exercise also included identification of essential enablers and risks that may impact on targets, that is, operationalisation and delivery of the NAPHS.
Linkage with other programmes/initiatives
As part of the development of the NAPHS, the NHSSDP and the Animal Health Sector Plan were reviewed to ensure that key national priorities were captured and to avoid unnecessary duplications. It is intended that the NAPHS coordination mechanism will identify areas for synergy and cost savings with the NHSSDP and other ongoing initiatives across all levels. These initiatives include the national strategy for growth and poverty reduction; overall staff employment and retention strategies and various ongoing collaboration and externally funded projects on health security preparedness and one health.
Summary of costs to implement the NAPHS
The 5-year cost estimate developed during the planning exercise for implementing the Tanzania NAPHS is approximately US$86.6 million (22 million for prevent, 50 million for detect, 4.8 million for response and 9.2 million for other IHR hazards and PoE). When vaccines for addressing zoonotic diseases in animals are included, the cost increases sevenfold (tables 3 and 4). This is due to the fact that there is currently no animal vaccination programme in the country. The cost estimated are based on common diseases in the country, that is, rabies, anthrax, brucellosis and RVF with total number of cows, dogs and goats assumed available. The costs of animal vaccination are included in the final NAPHS launched in September 2017.
Table 3.
Total budget costing with vaccines to address zoonotic diseases in animals
| Category | Total (TSH) | Total (US$) |
| Prevent | 1 184 979 286 153 | 538 626 948 |
| Detect | 110 724 620 164 | 50 329 373 |
| Respond | 10 671 720 000 | 4 850 782 |
| Other IHR hazards and points of entry | 20 419 300 000 | 9 281 500 |
| Cross cutting | 153 900 000 | 69 955 |
| Grand total | 1 326 948 826 317 | 603 158 558 |
TSH, Tanzanian Shiling (local currency).
Table 4.
Total costing without vaccines to address zoonotic diseases in animals
| Thematic area | Total (TSH) | Total (US$) |
| Prevent | 48 520 406 048 | 22 054 730 |
| Detect | 110 724 620 164 | 50 329 373 |
| Respond | 10 671 720 000 | 4 850 781.8 |
| Other IHR hazards and points of entry | 20 419 300 000 | 9 281 500 |
| Cross cutting | 153 900 000 | 69 955 |
| Grand total | 190 489 946 211.64 | 86 586 339 |
The costs associated with the respond thematic area are relatively low compared with the others. However, they include important infrastructure and procurement items which could have a significant influence on the cost scenario but promote long-term sustenance in capacities (table 5).
Table 5.
Cost drivers per Joint External Evaluation thematic areas
| Core component | Cost drivers |
| Prevent | Support councils and health facilities to conduct fixed, outreach and mobile services Support provision of personal protective equipment and equipment Conduct training on linking human and animal health sectors |
| Detect | Potential staff hire for laboratory (veterinary and human laboratories) Train 200 healthcare workers and 200 allied healthcare workers in 26 regions (specimen referral and transport system) Orient community healthcare workers in 10 high-risk regions and provide incentives Train 126 students into masters level in field epidemiology |
| Respond | Include the EOC facility in the new construction planning of Ministry of Health Procure eight ambulances to be used to transport highly infectious patients Procure at least four vans for public address and communication |
| Other IHR hazards and points of entry (PoE) | Identify, construct and equip temporary holding facilities at 12 designated PoE Procure five ambulances for transportation of ill travellers suspected to harbour infectious diseases at biggest PoEs and 6 vehicles and 20 motorcycles to facilitate central and zonal supportive supervision |
EOC, Emergency Operation Centre.
Delivery of the plan: responsible authority
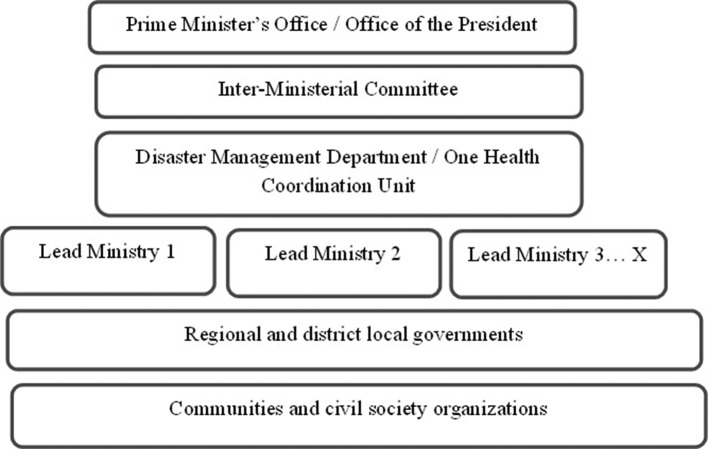
To ensure maximum political and multisectoral buy-in, the delivery of the NAPHS will be done through the PMO, implemented by the Department of Disaster Management. This would ensure effective coordination of activities which fall under the remit of different sectors or ministries. The Disaster Management Act of 2015 established an interministerial steering committee, which will be the functional body for NAPHS implementation (figure 2).
Figure 2.
National health security management structure to oversee the implementation of National Action Plan for Health Security.
Monitoring and evaluation of the NAPHS
Tanzania’s NAPHS clearly stipulates how progress towards the attainment of the targets will be evaluated through quarterly, annual, mid-term and end-term reviews/evaluation. It outlines the data sources, including: surveillance systems in human and animal health, annual reviews/assessments and reporting, after action reviews and simulations exercises, JEE and other relevant assessments such as the OIE PVS tool, in addition to periodic supervision. The NAPHS also captures how building sustainable capacity at all levels (national, local governments, the private sector, facilities and communities) will be done to facilitate supervision, MEF of IHR core capacity building. For some technical areas, the NAPHS is flexible about the need to reconceptualise and reorganise the managerial and support mechanisms and structures at national, subnational and local levels, including defining a clear supervisory mechanism, and roles of the various decentralised levels and the community. The NAPHS stipulates the need to strengthen and ensure a robust IHR (2005) MEF at all levels, which will itself be monitored throughout its life according to the IHR MEF framework (figure 3). It also defines the investments needed, including the development and use of appropriate Information Communication and Technology for improving communication and information. Other areas identified include increasing the training, recruitment and deployment of required human resources for health security and One Health approach at all levels. Moreover, it emphasises the importance of regular utilisation and dissemination of information to all stakeholders for purposes of improving management, sharing experiences, upholding transparency and accountability.
Figure 3.
IHR MEF to oversee the progress and impact of National Action Plan for Health Security. IHR, International Health Regulations; MEF, monitoring and evaluation framework.
Lessons learnt
Tanzania made history in global health security, by being the first country to finalise a costed NAPHS and in doing so, met the recommendations of the IHR review committee.19 The journey from JEE to NAPHS was not easy; as the first country to go through both process took approximately 1 year. However, this time allowed the facilitation of closer dialogues and joint working involving all relevant authorities and levels including those outside of health sectors.
Tanzania used the existing IHR technical working group to start the initial process of the NAPHS development. While the major focus was on the JEE findings and priority actions, the country also used other previous assessments. This allowed consolidating and integrating all priorities under a single plan, with a single accountability framework which is expected to result in cost savings and enhance intersectorial collaboration.
Key guiding principles that were critical in the development of the NAPHS were: country ownership of the entire process, high-level Government commitment, use of the One Health approach and linking the plan to national planning and budget cycles.
The deep multisectoralism or ‘One Health’ approach ensured that the NAPHS is an integral part of health system strengthening. Indeed, a call for such a broad approach to public health, organised around protection, prevention and promotion was published in March 2016 by the World Federation of Public Health Associations.20 Tanzania’s multisectoral approach is important as it ensures coordination and sharing of activities and responsibilities among those accountable. A similar experience has been observed in Kenya.21
The costing exercise used a simple excel-based tool developed by WHO. National staffs were trained to independently use the tool. Based on ongoing experiences, WHO has now developed an automated tool to share with Member States.
In costing workshop in February 2017, the Chief Medical Officer, on behalf of the Minister for Health noted ‘as we embark on implementation and on resource mobilisation to operationalize the plan, it is important to ensure that this plan aligns and feeds into country planning and budgeting cycles so as to ensure sustainable funding for the plan’. He also emphasised the important role of Parliamentarians in health security implementation and advocacy through Parliament to mobilise domestic resources (financial, human and logistic) for NAPHS. The active involvement of a Parliamentarian in NAPHS development is worth noting and be a good practice for other countries to pursue.
Challenges faced in the development of NAPHS and mitigation
The key challenges incurred during the development of the NAPHS include:
Linking the NAPHS with NHSSDP, other health security or disease-specific plans: this was managed through a consultative process with relevant stakeholders in the country. A cross-walk was also undertaken between JEE recommendations and priorities identified in other plans and assessments. Moreover, the scope of NAPHS allows it to serve as a coordinating platform to mitigate the challenge of linkage and inter-relation with other plans.
Setting top priorities and their sequencing: a consultative process was pursued with relevant stakeholders including those at subnational levels (local government officials) to address this effectively. Key factors employed were cost drivers, activities requiring multiple stakeholders, areas demonstrated very low capacities for IHR (2005), availability of funding/partnerships and gaps.
Translating JEE recommendation into NAPHS: it was also identified that, in some technical areas, JEE recommendations are not specific enough to readily convert them into priority activities under NAPHS. This necessitated consultation with national technical experts to agree on detailed activities corresponding to those recommendations. In other countries, this can be proactively resolved if the expectation for post-JEE NAPHS is factored into JEE processes, that is, start the process for planning during the completion of JEE.
Conclusion and next steps
Tanzania’s journey from the JEE to the finalisation of a costed NAPHS has galvanised multiple in-country stakeholders to work together on health security in the country. It informed the policy makers of the areas with running gaps in funding or technical partnerships. Experiences in Tanzania indicate that, even at the regional and global level, the JEE and subsequent NAPHS workshops have been effective in bringing together multiple HDP and creating one platform for the country.22
In terms of forging partnerships, it is not an overstatement to say that the Tanzania JEE and NAPHS development process has created and continues to create partnerships both across national sectors and with international partners and countries in ways not seen before. The overall process was considered by all parties as transparent, inclusive, multisectoral and brought all priorities onto a common platform for IHR capacity development. Over time, the JEE and NAPHS and anticipated impact would allow WHO, member states and HDP to review the benefit and limitation of revised IHR MEF.
The NAPHS was launched at a Parliamentary session in September 2017. The event ensured that Parliamentarians are fully aware of the plan and can advocate for increased domestic funding including from private sectors. The Tanzania Government is committed to ensuring implementation of the plan and to sharing its experiences with other countries in Africa and beyond. Benefitting from Tanzania’s experience, other countries can streamline the development of a costed, multisectoral NAPHS by considering planning process at the time of JEE, applying good practices identified in Tanzania and using existing planning and costing tools.
Ensuring sustainable funding for the NAPHS is critical. A concerted effort was made to identify domestic funding to be supplemented with funding from partners. Moreover, through the leadership of the oversight body (interministerial group), a wider stakeholder meeting involving key HDP will be held to identify sustainable financing mechanisms including domestic financing for the NAPHS.
Acknowledgments
The authors would like to acknowledge the active participation of national experts from volunteering countries, the members of the international roster of experts and the invaluable partnerships with governments including the governments of Finland, Germany and the USA; with other intergovernmental organisations, particularly the United Nations Food and Agriculture Organization (FAO), the World Organisation for Animal Health (OIE) and the International Civil Aviation Organization (ICAO); many public health institutions such as the US Centers for Disease Control (CDC), the Africa CDC, the European CDC (ECDC) and Public Health England (PHE); private entities such as the Bill and Melinda Gates Foundation and many other partners, including the members of the Global Health Security Agenda and of the JEE Alliance. The authors would like to acknowledge the continuing support and commitment of all of these to the implementation and principles of the International Health Regulations (2005).
Footnotes
Handling editor: Seye Abimbola
Contributors: JMM, AOT, GES, MM, MB, NR, MA, JB, RB, MM, RS, RE conducted both the JEE and NAPHs. SN, KS conducted the JEE. SL, SS, PV conducted the NAPHS. ISF, GR, SC, AHY supervised the JEE and NAPHS. All authors contributed to the manuscript, read and approved the final manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Author note: The approval for publication of findings (JEE, NAPHS and associated process) including authorship of Tanzania Government Officials was obtained from the Ministry of Health Tanzania and its Chief Medical Officer.
References
- 1. World Health organization (WHO). Ebola situation report-30 March 2016. http://apps.who.int/ebola/current-situation/ebola-situation-report-30-march-2016 (accessed 12 Aug 2017).
- 2. United Nations Development Group (UNDG). Socio-economic impact of Ebola virus disease in West African Countries. A call for national and regional containment, recovery and prevention. http://www.africa.undp.org/content/dam/rba/docs/Reports/ebola-west-africa.pdf (accessed Aug 2017).
- 3. The World Bank. Ebola: most African countries avoid major economic loss but impact on Guinea, Liberia, Sierra Leone Remains Crippling. http://www.worldbank.org/en/news/press-release/2015/01/20/ebola-most-african-countries-avoid-major-economic-loss-but-impact-on-guinea-liberia-sierra-leone-remains-crippling (accessed 14 Aug 2017).
- 4. The World Bank. The Economic Impact of the 2014 Ebola Epidemic: short and medium term estimates for West Africa. 2014. http://www.worldbank.org/en/region/afr/publication/the-economic-impact-of-the-2014-ebola-epidemic-short-and-medium-term-estimates-for-west-africa (accessed 14 Aug 2017).
- 5. The World Bank. Summary on the Ebola recovery plan: Sierra Leone. 2015. http://www.worldbank.org/en/topic/ebola/brief/summary-on-the-ebola-recovery-plan-sierra-leone (accessed 14 Aug 2017).
- 6. The World Bank. Summary on the Ebola recovery plan: Guinea. 2015. http://www.worldbank.org/en/topic/ebola/brief/summary-on-the-ebola-recovery-plan-guinea (accessed 14 Aug 2017).
- 7. The World Bank. Summary on the Ebola recovery plan: Liberia – Economic Stabilization and Recovery Plan (ESRP). 2015. http://www.worldbank.org/en/topic/ebola/brief/summary-on-the-ebola-recovery-plan-liberia-economic-stabilization-and-recovery-plan-esrp (accessed 14 Aug 2017).
- 8. Sindato C, Karimuribo E, Mboera LE. The epidemiology and socio-economic impact of rift valley fever epidemics in Tanzania: a review. Tanzan J Health Res 2011;13:305–18. [DOI] [PubMed] [Google Scholar]
- 9. Peyre M, Chevalier V, Abdo-Salem S, et al. A systematic scoping study of the socio-economic impact of rift valley fever: research gaps and needs. Zoonoses Public Health 2015;62:309–25. 10.1111/zph.12153 [DOI] [PubMed] [Google Scholar]
- 10. Bali S, Taaffe J. The sustainable development goals and the global health security agenda: exploring synergies for a sustainable and resilient world. J Public Health Policy 2017;38:257–68. 10.1057/s41271-016-0058-4 [DOI] [PubMed] [Google Scholar]
- 11. World Health Organisation. International health regulations. 3rd edn, 2005. http://apps.who.int/iris/bitstream/10665/246107/1/9789241580496-eng.pdf?ua=1 (accessed 14 Aug 2017).
- 12. World Health Organization. Implementation of the International Health Regulations (2005): report of the review committee on second extensions for establishing national public health capacities and on IHR implementation. Geneva: WHO, 2015. (accessed 13 Aug 2017). [Google Scholar]
- 13. World Health Organisation. Joint external evaluation tool: International Health Regulations. 2005. http://apps.who.int/iris/handle/10665/204368 (accessed 14 Aug 2017).
- 14. World Health Organisation. Strategic partnership portal. IHR monitoring and evaluation framework. https://extranet.who.int/spp/ihrmef (accessed 10 Aug 2017).
- 15. World Health Organisation IHR. Monitoring and evaluation framework. Joint external evaluation tool and process overview. 2005. http://apps.who.int/iris/bitstream (accessed 14 Aug 2017).
- 16. World Health Organisation. Strategic partnership portal. country planning for health security. https://extranet.who.int/spp/country-planning (accessed Aug14 2017).
- 17. World Health Organisation. Strategic partnership portal. joint external evaluation assessments. https://extranet.who.int/spp/joint-external-evaluation-tool-assessment (accessed 14 Aug 2017).
- 18. World Health Organisation. Strategic partnership portal. joint external evaluation assessments. https://extranet.who.int/spp/jeeta/united-republic-tanzania (accessed 14 Aug 2017).
- 19. World Health Organisation. IHR review committee (WHA A69/21, recommendations 2.1.5, and 5.2). https://extranet.who.int/spp/country-planning (accessed Jun 2017).
- 20. Lomazzi M. A Global Charter for the Public’s Health-the public health system: role, functions, competencies and education requirements. Eur J Public Health 2016;26:210–2. 10.1093/eurpub/ckw011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bolo AZ, Nkirote KC. Bottlenecks in the execution of Kenya vision 2030 strategy: an empirical study. Prime Journal of Business Administration and Management 2012;2:505–12. [Google Scholar]
- 22. Kandel N, Sreedharan R, Chungong S, et al. Lancet global health. 2017:e857–8. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2017-000600supp001.pdf (23.9KB, pdf)