Summary box.
Traumatic brain injury is a major global health issue and requires a functional health system to be optimally managed—often lacking in those low-income and middle-income countries where the burden of this disease is highest.
Clinical care is the emergent property of a complex, adaptive, sociotechnical system: generating improvements in care can benefit from a systems approach.
Systems Engineering can inform a systems approach to healthcare improvement, complementing more traditional improvement techniques.
A systems approach may be a valuable tool in trying to understand, and improve, the clinical care of patients with traumatic brain injury in low-income and middle-income settings.
The Global Burden of Diseases, Injuries and Risk Factors Study showed that in 2010 trauma accounted for 9% of the world’s deaths—around 5 million people—while also resulting in millions of non-fatal injuries with resultant disability. Around 90% of injury-related deaths occurred in low-income and middle-income countries (LMICs), which also saw the greatest rise in these injuries due to road traffic collisions.1 More recent global health estimates from WHO for 2015 show a similar picture.2 As a disease subtype, traumatic brain injury (TBI) is one of the most devastating, with clinical, societal and economic sequelae.3 It is also startlingly common with an estimated 50 million or more cases per year; enough for half of the world’s population to suffer a TBI in their lifetime and again disproportionately affecting lower-income regions.4
TBI is a heterogeneous condition, which can be difficult to both manage and prognosticate in even the best resourced settings and involves an array of prehospital, acute treatment and rehabilitation services.4 5 These are interdependent meaning improvement in any one area of care may not be reflected in overall clinical outcome. While aggressive treatment of TBI can minimise disability in many patients, prevention of mortality can also result in survival with severe disability in others, making the decision to intervene or not an ethically complex one, since the health systems resources required to effectively manage TBI are significant.6
An additional layer of complexity is added by the wider LMIC environment: fragile health systems, a lack of coordinated social support and inadequate infrastructure complicate the management of TBI in both the acute and the rehabilitative phase. Applying the current clinical evidence base, largely generated in high-income countries, may not be appropriate in LMICs. Ethical considerations will be culturally and contextually dependent, and measures of outcome may be hard to agree on.7 Health systems strengthening is recognised as a key challenge in LMICs, yet relating wider systems strengthening to the care of a specific, although heterogeneous, clinical entity is a particular challenge.8 9
What is required to overcome these myriad challenges? Better epidemiological data are essential, both to characterise and quantify injuries being sustained in different contexts, and to map their current management. Clinical medicine clearly has a role to play, with guidelines, protocols and pragmatic trials based in LMICs needed to generate an appropriate and applicable evidence base to guide management, alongside the development of innovative technologies appropriate to the LMIC context.7 However, these will only solve part of the problem. Allied disciplines such as Improvement Science, Implementation Science, Operational Research and Human Factors Engineering may all offer insights as to not only what to do but how to do it.10–14
A central tenet of many of these disciplines is the concept of medical care as delivered by a system. Systems thinking in healthcare is endorsed by WHO as particularly apposite for improvement in healthcare in LMICs, while in the field of global surgery, the Lancet Commission on Global Surgery 2015 notes the importance of focussing on systems with regard to surgical improvement.9 15 16 More specifically in TBI, the importance of the health system is highlighted in the recent Lancet Neurology Commission on Traumatic Brain Injury.4 However, a universal definition of systems thinking, or even of a system in the context of healthcare, is lacking. There is an increasing recognition that healthcare represents a complex, adaptive, sociotechnical system consisting of people and equipment, processes and institutions. The complexity arises from both the number of, and the variability in, the interactions between these different components. Indeed, several elements of complex systems may be observable in healthcare including emergence, path dependence, self-organisation, non-linearity and non-scalability.8 17–19
TBI care may be seen then as the apotheosis of a systems problem: a complex, heterogeneous, clinical entity which requires a functional macro-healthcare system and a coordinated micro-clinical system, has variable and controversial measures of outcome and has a significant cultural and ethical component to its management. The development of a systems understanding of TBI care appears essential to coordinate the more traditional approaches to healthcare improvement.
Developing a systems approach to understanding and improving TBI care is operationally challenging. The disciplines listed above may rely on a systems understanding but rarely provide examples as to how to model complex systems so that they can be rationally re-engineered. Furthermore, there is little to guide researchers as to how to contextualise the micro-system of clinical care into the macro-system of national health service delivery to ensure these are mutually supportive of each other. Recently, the use of established dynamic systems modelling techniques such as Systems Dynamics Modelling (SDM) and Agent Based Modelling (ABM), in addition to static techniques such as network analysis and scenario planning, have been proposed as helpful to understanding healthcare improvement in LMICs.20 In fact, an array of techniques for modelling healthcare have been put forward, and work done to understand the place of each in intervention design.21–23 In addition, there has been a growth in interest in techniques borrowed from industry such as Lean and Six Sigma.24
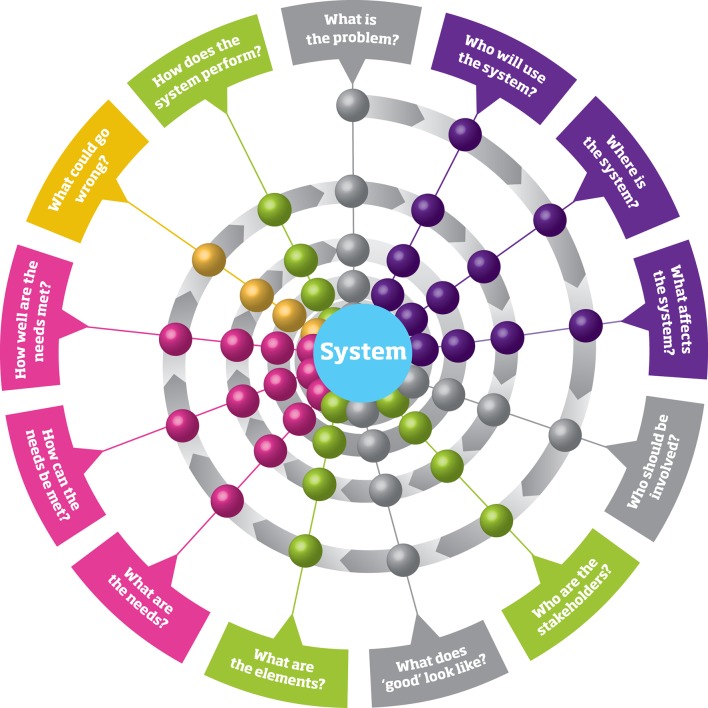
In this arena, the experience of the Engineering community may offer crucial insights.25 This has recently been highlighted through a joint project by the UK Royal Academy of Engineering, the Royal College of Physicians and the Academy of Medical Sciences.26 Their report, ‘Engineering better care: a systems approach to health and care design and continuous improvement’, outlines the value that an engineering-informed systems approach can bring to healthcare, through focussing on understanding the people, systems, design and risk involved when pursuing healthcare improvements. This approach can be summarised in an iterative series of questions, which need to be answered as a project progresses (figure 1). The application of Systems Engineering to patient safety has been widely adopted, but the Royal Academy report emphasises the role a broader systems approach can play in healthcare improvement, with Systems Engineering complementing existing healthcare improvement tools.27–30 Crucially, such a systems approach brings together many of the discrete techniques such as SDM and ABM, but includes a wide variety of other quantitative and qualitative methodologies.
Figure 1.
A systems approach as an ordered series of questions regarding general improvement (grey), people (purple), systems (green), design (pink) and risk (orange). Reproduced with permission from Engineering Better Care, Royal Academy of Engineering, Academy of Medical Sciences and Royal College of Physicians, 2017
How do these four tenets of people, systems, design and risk inform our understanding of complex systems? The first insight is that systems can be interrogated through the lens of many different stakeholders, and that a full understanding of the system can only come about through rigorous and extensive engagement with these stakeholders. The second is that systems can be represented in a variety of ways, and that matching the right model to the right problem is fundamental to generating a common understanding and possible solutions. Third, interventions to improve care benefit from a design process of iterative improvement based on this understanding of people and systems, and fourth that all interventions create risk—both of unintended consequences and of wasted endeavour—which can be formally modelled. Crucially, such a systems approach does not seek to generate generalisable answers to healthcare problems; rather it seeks to use a generalisable process to design context-dependent solutions. It is this context dependence that suits it so well to address some of the difficulties that arrive with the improvement of TBI care in LMICs.
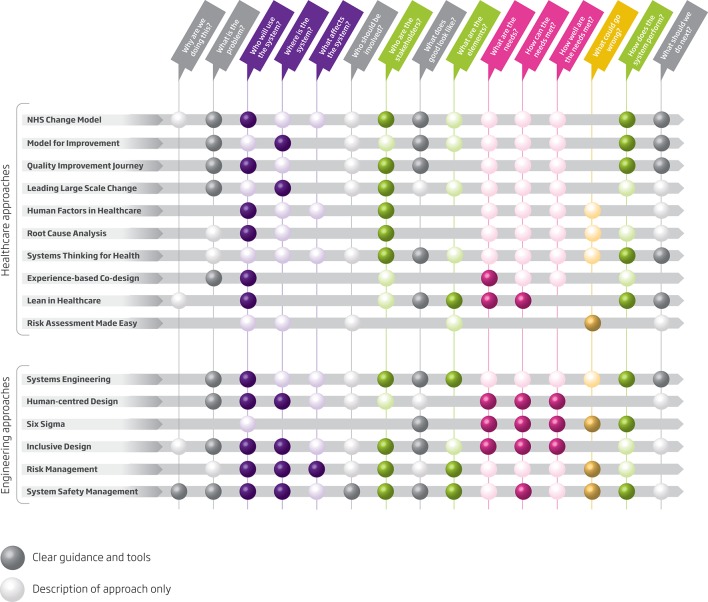
What does a systems approach offer alongside existing schools of improvement or implementation? Figure 2 shows how the series of questions proposed as key to solving systems problems may be answered by both traditional and engineering-informed approaches. While traditional approaches reference many of the questions, they often fail to provide a methodological basis for answering them. In addition, an engineering-informed systems approach provides an academic and operational basis to bridge the gap between the various levels of the healthcare delivery system.
Figure 2.
The ability of both engineering and traditional approaches to healthcare improvement to answer the key questions of a systems approach. Reproduced with permission from Engineering Better Care, Royal Academy of Engineering, Academy of Medical Sciences and Royal College of Physicians,2017
Arguably, the most important element to the LMIC context is that many of the systems modelling techniques used by engineers do not require high-resolution data as a prerequisite. Many of these modelling techniques are based around narrative or workshop data, and use this to graphically represent problems to allow consensus problem solving.19 31 While quantitative modelling and simulation can augment this process, they are not essential.19 Mixed-methods approaches are ideal in LMICs where robust data can be hard to obtain; a ‘soft-systems methodology’ used as part of a systems approach provides a focused, proven method of pragmatic problem structuring with the available data.32 On a more philosophical level, such a systems approach recognises that health systems are best interrogated through an understanding of stakeholders’ perspectives, and that systems design starts first with the elucidation of those stakeholders’ needs. This has clear cross-over with many of the principles of partnership and codevelopment, which have grown out of the global health community.33–38
How can we relate this systems approach back to the clinical problem of TBI in LMICs? Consider the four themes or people, systems, risk and design. The stakeholders are varied and may include neurosurgeons, anaesthetists, patients, nurses, administrators, non-governmental organisations, national and international societies, funding agencies, academics and religious leaders. The systems involved include international, national, regional and local institutions, and span prehospital, acute and rehabilitative care. There is a risk of wasted endeavour, of active harm or of failing to monitor genuine improvement. Any proposed change to care must therefore be carefully designed in order to explicitly account for these elements. A given intervention—such as guideline development, equipment provision or clinical training of neurosurgeons—may cause a number of possible changes to this complex picture. The better our understanding of this system before an intervention is planned, the better our ability to improve outcomes for patients with TBI both directly and indirectly. In addition, by understanding the system there is the possibility for synergy with other improvement efforts within the healthcare ecosystem.
Critics of the systems approach advocated here argue that many of its principles are ‘common sense’; however, the realisation of the Engineering community is that common sense is rarely common and that a framework to embed it in both operational and research work has enormous value. Systems Engineering has an impressive pedigree outside of the medical field and is widely used in other safety-critical industries such as aviation, spaceflight, defence and manufacturing.39–44 The tools and techniques it has developed provide powerful insights into the planning and implementation of interventions to complex systems, and incorporating these into a wider systems approach may be of enormous benefit to clinicians and academics seeking to address global health challenges.
Footnotes
Handling editor: Seye Abimbola
Twitter: @global_neuro
Contributors: TB was responsible for drafting the original manuscript and all other authors reviewed and amended the manuscript before submission. All authors had an opportunity to review the final manuscript before submission, although TB takes overall responsibility for the content.
Funding: This work was funded by the National Institute for Health Research (NIHR) Global Health Research Group on Neurotrauma. PJAH is also supported by an NIHR Research Professorship and the NIHR Cambridge Biomedical Research Centre. This work was also supported by a European Union FP7 Program Grant for CENTER-TBI.
Competing interests: PJC is a Fellow of the Royal Academy of Engineering and lead author of the cited report ‘Engineering better care: a systems approach to health and care design and continuous improvement’.
Patient consent: Detail has been removed from this case description/these case descriptions to ensure anonymity. The editors and reviewers have seen the detailed information available and are satisfied that the information backs up the case the authors are making.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–223. 10.1016/S0140-6736(12)61689-4 [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization. Disease burden and mortality estimates. http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html (accessed 3 Mar 2018).
- 3. Hyder AA, Wunderlich CA, Puvanachandra P, et al. The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation 2007;22:341–53. [PubMed] [Google Scholar]
- 4. Maas AIR, Menon DK, Adelson PD, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol 2017;16:987–1048. 10.1016/S1474-4422(17)30371-X [DOI] [PubMed] [Google Scholar]
- 5. Stocchetti N, Carbonara M, Citerio G, et al. Severe traumatic brain injury: targeted management in the intensive care unit. Lancet Neurol 2017;16:452–64. 10.1016/S1474-4422(17)30118-7 [DOI] [PubMed] [Google Scholar]
- 6. Hutchinson PJ, Kolias AG, Timofeev IS, et al. Trial of decompressive craniectomy for traumatic intracranial hypertension. N Engl J Med 2016;375:1119–30. 10.1056/NEJMoa1605215 [DOI] [PubMed] [Google Scholar]
- 7. Rubiano AM, Carney N, Chesnut R, et al. Global neurotrauma research challenges and opportunities. Nature 2015;527:S193–S197. 10.1038/nature16035 [DOI] [PubMed] [Google Scholar]
- 8. Adam T, Hsu J, de Savigny D, et al. Evaluating health systems strengthening interventions in low-income and middle-income countries: are we asking the right questions? Health Policy Plan 2012;27(Suppl 4):iv9–19. 10.1093/heapol/czs086 [DOI] [PubMed] [Google Scholar]
- 9. Adam T, de Savigny D. Systems thinking for strengthening health systems in LMICs: need for a paradigm shift. Health Policy Plan 2012;27(Suppl 4):iv1–3. 10.1093/heapol/czs084 [DOI] [PubMed] [Google Scholar]
- 10. Wagstaff DT, Bedford J, Moonesinghe SR. Improvement science in anaesthesia. Curr Anesthesiol Rep 2017;7:432–9. 10.1007/s40140-017-0234-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ridde V. Need for more and better implementation science in global health. BMJ Glob Health 2016;1:e000115 10.1136/bmjgh-2016-000115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zachariah R, Harries AD, Ishikawa N, et al. Operational research in low-income countries: what, why, and how? Lancet Infect Dis 2009;9:711–7. 10.1016/S1473-3099(09)70229-4 [DOI] [PubMed] [Google Scholar]
- 13. Burt J. Getting to grips with the beast: the potential of multi-method operational research approaches. BMJ Qual Saf 2017;26:611–2. 10.1136/bmjqs-2017-006484 [DOI] [PubMed] [Google Scholar]
- 14. Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, et al. Human factors systems approach to healthcare quality and patient safety. Appl Ergon 2014;45:14–25. 10.1016/j.apergo.2013.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Meara JG, Leather AJM, Hagander L, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. The Lancet 2015;386:569–624. 10.1016/S0140-6736(15)60160-X [DOI] [PubMed] [Google Scholar]
- 16. Swanson RC, Atun R, Best A, et al. Strengthening health systems in low-income countries by enhancing organizational capacities and improving institutions. Global Health 2015;11:5 10.1186/s12992-015-0090-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Paina L, Peters DH. Understanding pathways for scaling up health services through the lens of complex adaptive systems. Health Policy Plan 2012;27:365–73. 10.1093/heapol/czr054 [DOI] [PubMed] [Google Scholar]
- 18. Atun R. Health systems, systems thinking and innovation. Health Policy Plan 2012;27(Suppl 4):iv4–iv8. 10.1093/heapol/czs088 [DOI] [PubMed] [Google Scholar]
- 19. Hettinger LJ, Kirlik A, Goh YM, et al. Modeling and simulation of complex sociotechnical systems: Envisioning and analyzing work environments. Ergonomics 2012;58:1–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Borghi J, Chalabi Z. Square peg in a round hole: re-thinking our approach to evaluating health system strengthening in low-income and middle-income countries. BMJ Glob Health 2017;2:e000406 10.1136/bmjgh-2017-000406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jun GT, Morris Z, Eldabi T, et al. Development of modelling method selection tool for health services management: from problem structuring methods to modelling and simulation methods. BMC Health Serv Res 2011;11:108 10.1186/1472-6963-11-108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jun GT, Ward J, Clarkson PJ. Systems modelling approaches to the design of safe healthcare delivery: ease of use and usefulness perceived by healthcare workers. Ergonomics 2010;53:829–47. 10.1080/00140139.2010.489653 [DOI] [PubMed] [Google Scholar]
- 23. Jun GT, Ward J, Morris Z, et al. Health care process modelling: which method when? Int J Qual Health Care 2009;21:214–24. 10.1093/intqhc/mzp016 [DOI] [PubMed] [Google Scholar]
- 24. Soliman M, Saurin TA. Lean production in complex socio-technical systems: a systematic literature review. Journal of Manufacturing Systems 2017;45:135–48. 10.1016/j.jmsy.2017.09.002 [DOI] [Google Scholar]
- 25. Taneva S, Grote G, Easty A, et al. Decoding the perioperative process breakdowns: a theoretical model and implications for system design. Int J Med Inform 2010;79:14–30. 10.1016/j.ijmedinf.2009.10.001 [DOI] [PubMed] [Google Scholar]
- 26. Royal Academy of Engineering, Academy of Medical Sciences and Royal College of Physicians. Engineering better care: a systems approach to health and care design and continuous improvement. 2017.
- 27. Carayon P, Schoofs Hundt A, Karsh BT, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care 2006;15(Suppl 1):i50–i58. 10.1136/qshc.2005.015842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics 2013;56:1669–86. 10.1080/00140139.2013.838643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wooldridge AR, Carayon P, Hundt AS, et al. SEIPS-based process modeling in primary care. Appl Ergon 2017;60:240–54. 10.1016/j.apergo.2016.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Carayon P. Sociotechnical systems approach to healthcare quality and patient safety. Work 2012;41(Suppl 1):3850–4. 10.3233/WOR-2012-0091-3850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Buckle P, Clarkson PJ, Coleman R, et al. Systems mapping workshops and their role in understanding medication errors in healthcare. Appl Ergon 2010;41:645–56. 10.1016/j.apergo.2009.12.013 [DOI] [PubMed] [Google Scholar]
- 32. Checkland PB. Soft systems methodology. Human Systems Management 1989;8:273–89. [Google Scholar]
- 33. Macpherson L, Collins M. Training responsibly to improve global surgical and anaesthesia capacity through institutional health partnerships: a case study. Trop Doct 2017;47:73–7. 10.1177/0049475516665999 [DOI] [PubMed] [Google Scholar]
- 34. Lipnick M, Mijumbi C, Dubowitz G, et al. Surgery and anesthesia capacity-building in resource-poor settings: description of an ongoing academic partnership in Uganda. World J Surg 2013;37:488–97. 10.1007/s00268-012-1848-x [DOI] [PubMed] [Google Scholar]
- 35. Parry EH, Percy DB. Anaesthesia and hospital links: strengthening healthcare through South-North hospital partnerships. Anaesthesia 2007;62(Suppl 1):15–20. 10.1111/j.1365-2044.2007.05292.x [DOI] [PubMed] [Google Scholar]
- 36. Cadotte DW, Blankstein M, Bekele A, et al. Establishing a surgical partnership between Addis Ababa, Ethiopia, and Toronto, Canada. Can J Surg 2013;56:E19–E23. 10.1503/cjs.027011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Elobu AE, Kintu A, Galukande M, et al. Evaluating international global health collaborations: perspectives from surgery and anesthesia trainees in Uganda. Surgery 2014;155:585–92. 10.1016/j.surg.2013.11.007 [DOI] [PubMed] [Google Scholar]
- 38. Tyson S, Gordon M. United Kingdom government aid. Anaesthesia 2007;62(Suppl 1):11–14. 10.1111/j.1365-2044.2007.05291.x [DOI] [PubMed] [Google Scholar]
- 39. Wu S, Duan N, Wisdom JP, et al. Integrating science and engineering to implement evidence-based practices in health care settings. Adm Policy Ment Health 2015;42:588–92. 10.1007/s10488-014-0593-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kalawsky RS. The next generation of grand challenges for systems engineering research. Procedia Comput Sci 2013;16:834–43. 10.1016/j.procs.2013.01.087 [DOI] [Google Scholar]
- 41. Piaszczyk C. Model based systems engineering with department of defense architectural framework. Systems Engineering 2011;14:305–26. 10.1002/sys.20180 [DOI] [Google Scholar]
- 42. Khayal I, Bartels SJ, Bruce ML, et al. Developing an integrated behavioral health system model using engineering design Proceedings of the 2017 Industrial and Systems Engineering Conference, 2017:500–6. [Google Scholar]
- 43. Haskins C. Systems engineering handbook Incose 185, 2006. [Google Scholar]
- 44. BKCASE Editorial Board. The guide to the systems engineering body of knowledge (SEBoK). 2016. http://sebokwiki.org/wiki/Guide_to_the_Systems_Engineering_Body_of_Knowledge_ (accessed 11 Feb 2018).