Abstract
Background
The 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults provides recommendations for the definition of hypertension, systolic and diastolic blood pressure (BP) thresholds for initiation of antihypertensive medication and BP target goals.
Objective
Determine the prevalence of hypertension, implications of recommendations for antihypertensive medication and prevalence of BP above the treatment goal among US adults using criteria from the 2017 ACC/AHA and the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC7) guidelines.
Methods
We analyzed data from the 2011–2014 National Health and Nutrition Examination Survey (N=9,623). NHANES participants completed study interviews and an examination. For each participant, blood pressure was measured three times following a standardized protocol and averaged. Results were weighted to produce US population estimates.
Results
According to the 2017 ACC/AHA and JNC7 guidelines, the overall crude prevalence of hypertension among US adults was 45.6% (95% confidence interval [CI] 43.6%,47.6%) and 31.9% (95%CI 30.1%, 33.7%), respectively, and antihypertensive medication was recommended for 36.2% (95%CI 34.2%, 38.2%) and 34.3% (32.5%, 36.2%) of US adults, respectively. Compared to US adults recommended antihypertensive medication by JNC7, those recommended treatment by the 2017 ACC/AHA guideline but not JNC7 had higher CVD risk. Non-pharmacological intervention is advised for the 9.4% of US adults with hypertension according to the 2017 ACC/AHA guideline who are not recommended antihypertensive medication. Among US adults taking antihypertensive medication, 53.4% (95%CI 49.9%, 56.8%) and 39.0% (95%CI 36.4%, 41.6%) had BP above the treatment goal according to the 2017 ACC/AHA and JNC7 guidelines, respectively. Overall, 103.3 (95%CI 92.7, 114.0) million US adults had hypertension according to the 2017 ACC/AHA guideline of whom 81.9 (95%CI 73.8, 90.1) million were recommended antihypertensive medication.
Conclusion
Compared with the JNC 7 guideline, the 2017 ACC/AHA guideline results in a substantial increase in the prevalence of hypertension but a small increase in the percentage of U.S. adults recommended antihypertensive medication. A substantial proportion of US adults taking antihypertensive medication is recommended more intensive BP lowering under the 2017 ACC/AHA guideline.
Keywords: Hypertension, guideline, prevalence, treatment
The American College of Cardiology/American Heart Association (ACC/AHA) Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults provides comprehensive information on the prevention and treatment of hypertension (1). This guideline updated the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC7), which was published in 2003 (2). Compared to the JNC7 guideline, the 2017 ACC/AHA guideline recommends using lower systolic blood pressure (SBP) and diastolic blood pressure (DBP) levels to define hypertension (Table 1). All adults recommended antihypertensive medication by JNC7 are also recommended antihypertensive medication by the 2017 ACC/AHA guideline. Additionally, adults with high cardiovascular disease (CVD) risk with SBP of 130–139 mm Hg or DBP of 80–89 mm Hg and adults ≥ 65 years of age with SBP of 130–139 mm Hg are recommended antihypertensive medication by the 2017 ACC/AHA guideline. The 2017 ACC/AHA guideline recommends treating SBP/DBP to less than 130/80 mm Hg for all adults taking antihypertensive medication. This is lower than the goal recommended by JNC7, with the exception of adults with diabetes or CKD where the treatment goal has not changed. Each of the recommendations in the 2017 ACC/AHA guideline was based on systematic evaluations by an evidence review team and/or members of the Guideline Writing Committee (1).
Table 1.
Blood pressure levels used to define hypertension, recommend antihypertensive medication, and treatment goal according to the 2017 ACC/AHA guideline, the JNC7 guideline and the JNC8 panel member report.
| Guideline – Definition of hypertension | |||
|---|---|---|---|
| 2017 ACC/AHA | JNC7 | JNC8 panel member report | |
| Systolic blood pressure, mm Hg | |||
| General population | ≥ 130 | ≥ 140 | ≥ 140 |
| ≥60 years of age without diabetes or CKD | ≥ 150 | ||
| Diastolic blood pressure, mm Hg | |||
| General population | ≥ 80 | ≥ 90 | ≥ 90 |
| Guideline – Recommended antihypertensive medication | |||
| 2017 ACC/AHA | JNC7 | JNC8 panel member report | |
| Systolic blood pressure, mm Hg | |||
| General population | ≥ 140 | ≥ 140 | ≥ 140 |
| Diabetes or CKD | ≥ 130 | ≥ 130 | ≥ 140 |
| High cardiovascular disease risk† | ≥ 130 | ||
| Age ≥ 65 years | ≥ 130 | ||
| ≥60 years of age without diabetes or CKD | ≥ 150 | ||
| Diastolic blood pressure, mm Hg | |||
| General population | ≥ 90 | ≥ 90 | ≥ 90 |
| Diabetes or CKD | ≥ 80 | ≥ 80 | |
| High cardiovascular disease risk† | ≥ 80 | ||
| Guideline – Treatment goal among those taking antihypertensive medication | |||
| Systolic blood pressure, mm Hg | |||
| General population | < 130 | < 140 | < 140 |
| Diabetes or CKD | < 130 | < 140 | |
| ≥60 years of age without diabetes or CKD | < 150 | ||
| Diastolic blood pressure, mm Hg | |||
| General population | < 80 | < 90 | <90 |
| Diabetes or CKD | < 80 | ||
 No specific blood pressure threshold is provided in the guideline for this population. The other thresholds listed from the guideline should be applied, as appropriate.
No specific blood pressure threshold is provided in the guideline for this population. The other thresholds listed from the guideline should be applied, as appropriate.
Systolic and diastolic blood pressure levels should be based on multiple measurements taken at two or more visits. In the National Health and Nutrition Examination Survey, blood pressure was measured three times at a single visit.
In the top and middle panels, adults with systolic blood pressure or diastolic blood pressure above the levels listed and those taking antihypertensive medication are considered to have hypertension and are recommended antihypertensive medication.
In the bottom panel, to achieve treatment goals, both the systolic and diastolic blood pressure goals have to be met.
High cardiovascular risk is defined as a history of cardiovascular disease or 10-year predicted cardiovascular disease risk ≥ 10% using the Pooled Cohort risk equations.
2017 ACC/AHA guideline - 2017 American College of Cardiology/American Heart Association Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults.
JNC7 guideline - Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure JNC8 panel member report - 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee.
CKD – chronic kidney disease.
The purpose of the current analysis was to estimate the percentage and number of US adults with hypertension and recommended for pharmacological antihypertensive treatment according to the 2017 ACC/AHA guideline as compared with the JNC7 guideline. Additionally, we estimated the percentage and number of US adults taking antihypertensive medication with BP above goal using targets from each guideline. US adults taking antihypertensive medication with BP above goal according to the 2017 ACC/AHA guideline are recommended more intensive antihypertensive treatment. To accomplish these goals, we analyzed data from the US National Health and Nutrition Examination Survey (NHANES). As a secondary goal, we contrasted prevalence estimates from the 2017 ACC/AHA guideline with those obtained using the 2014 Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC8 panel member report).(3).
Methods
NHANES is conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention with the goal of monitoring the health status of the US general population.(4) Since 1999, NHANES has been conducted in two-year cycles. For each cycle, potential participants are identified through stratified, multistage probability sampling of the non-institutionalized US population. Using sampling weights, nationally representative estimates for the non-institutionalized US population can be generated and NHANES cycles can be combined to provide more stable prevalence estimates when needed. For the current analysis, we pooled data from the 2011–2012 and 2013–2014 NHANES cycles. The current analysis was restricted to adult participants, 20 years of age and older (n=10,907). Participants who did not have three SBP and DBP measurements obtained during their study visit (n=704) or were missing data on self-reported antihypertensive medication (n=13) were excluded. Also, participants missing data on variables (age, gender, race, smoking, total and HDL-cholesterol, and diabetes) used to calculate 10-year predicted CVD risk according to the Pooled Cohort risk equations (n=567) were excluded. After these exclusions were applied, data from 9,623 participants were available for the current analyses. The protocols for NHANES 2011–2012 and 2013–2014 were approved by the National Center for Health Statistics of the Centers for Disease Control and Prevention Institutional Review Board. Written informed consent was obtained from each participant.
Data collection
NHANES data were collected through the administration of standardized questionnaires and a medical evaluation at a mobile examination clinic. Covariates included in this analysis and their method of ascertainment are described in Online Table 1.
Blood pressure measurement and antihypertensive medication use
BP was measured by a trained physician using a mercury sphygmomanometer and an appropriately sized cuff. Cuff sizes were selected after measurement of each participant’s mid-right arm circumference. Readings were obtained after 5 minutes of seated rest. Three blood pressure measurements were obtained at 30 second intervals. The mean of the three measurements was used to define SBP and DBP. Quality control included quarterly re-certification with retraining as needed, and annual retraining of all physicians. Certification required video test recognition of Korotkoff sounds and performing measurements on volunteers. Participants who responded affirmatively to both of the questions “Have you ever been told by a doctor or other healthcare professional that you had hypertension, also called high blood pressure?” and “Are you now taking prescribed medication for high blood pressure?” were considered to be taking antihypertensive medication.
Cardiovascular disease (CVD) risk
History of CVD was defined by self-report of a prior diagnosis of myocardial infarction, coronary heart disease, stroke or heart failure. Among those without a history of CVD, 10-year predicted CVD risk was calculated using the Pooled Cohort risk equations.(5) Participants were categorized into one of five mutually exclusive groups including history of CVD and no history of CVD with 10-year predicted CVD risk <5%, 5% to <10%, 10% to <20% and ≥ 20%. High CVD risk was defined as having a history of CVD or a 10-year predicted CVD risk ≥ 10%.
Definitions of hypertension, recommendations for antihypertensive medication, and blood pressure treatment goals
The 2017 ACC/AHA and JNC7 guideline and JNC8 panel member report definitions of hypertension, criteria for recommending antihypertensive medication, and recommended BP goals for adults taking antihypertensive medication are provided in Table 1.
Statistical Analysis
We calculated the distribution of the population across five groups including those not taking antihypertensive medication with SBP/DBP < 120/<80, 120–129/<80, 130–139/80–89, and ≥ 140/90 mm Hg and those taking antihypertensive medication. These levels represent the BP stages in the 2017 ACC/AHA guideline (Online Table 2). Participants with SBP and DBP in two categories (e.g., SBP< 120 mm Hg and DBP between 80 and 89 mm Hg) were designated into the higher category. We calculated the demographic and clinical characteristics of US adults in each of these groups. Next, we calculated the percentage and number of US adults with hypertension and recommended antihypertensive medication according to the 2017 ACC/AHA guideline, the JNC7 guideline, and the 2017 ACC/AHA guideline but not the JNC7 guideline. Also, we calculated the percentage and number of US adults taking antihypertensive medication with BP above goal according to the 2017 ACC/AHA guideline, JNC7 guideline, and the 2017 ACC/AHA but not the JNC7 guideline. These calculations were done for the overall population and within sub-groups defined by age, gender, race-ethnicity and CVD risk categories. Demographic and clinical characteristics of US adults with hypertension and, separately, taking antihypertensive medication with BP above goal according to the 2017 ACC/AHA guideline, JNC7 guideline, and the 2017 ACC/AHA but not the JNC7 guideline were calculated. In a secondary analysis, we calculated the percentage of US adults with hypertension, recommended antihypertensive medication and with BP above goal according to the JNC 8 panel member report published in 2014.
Table 2.
Characteristics of US adults by blood pressure levels and antihypertensive medication use based on the 2011–2014 National Health and Nutrition Examination Survey.
| SBP/DBP categories in mm Hg among US adults not taking antihypertensive medication | |||||
|---|---|---|---|---|---|
| <120/80 (n=3,827) |
120–129/<80 (n=1,114) |
130–139/80–89 (n=1,276) |
≥140/90 (n=819) |
Taking antihypertensive medication (n=2,587) |
|
| Percentage (95% CI) of US population | 42.3 (40.3, 44.3) |
12.1 (11.0, 13.3) |
13.7 (12.7, 14.9) |
7.7 (6.8, 8.7) |
24.1 (22.4, 26.0) |
| Population characteristics† | |||||
| Age, years | 38.8 (0.4) | 45.0 (0.7) | 47.1 (0.7) | 54.6 (0.6) | 61.6 (0.3) |
| Male gender, % | 41.1 | 60.4 | 58.0 | 58.1 | 45.0 |
| Race/ethnicity, % | |||||
| Non-Hispanic white | 63.5 | 66.2 | 66.7 | 63.7 | 71.2 |
| Non-Hispanic black | 9.1 | 10.8 | 11.6 | 14.5 | 14.8 |
| Non-Hispanic Asian | 6.5 | 4.9 | 4.7 | 6.0 | 3.4 |
| Hispanic | 18.2 | 14.9 | 14.0 | 12.4 | 8.7 |
| Cigarette smoking, % | 19.8 | 23.8 | 20.6 | 21.0 | 15.5 |
| Total cholesterol, mg/dL | 187.6 (1.0) | 195.3 (1.1) | 201.0 (1.8) | 206.3 (2.1) | 190.2 (1.3) |
| HDL cholesterol, mg/dL | 54.2 (0.4) | 51.9 (0.6) | 52.8 (0.7) | 54.0 (0.9) | 51.6 (0.5) |
| Statin use, % | 6.7 | 12.0 | 12.0 | 13.5 | 47.8 |
| Diabetes, % | 3.7 | 7.6 | 9.1 | 14.1 | 26.7 |
| Reduced eGFR, % | 2.3 | 2.3 | 3.4 | 8.7 | 20.8 |
| Albuminuria, % | 4.7 | 6.1 | 9.4 | 15.6 | 17.6 |
| Systolic blood pressure, mm Hg | 108.9 (0.2) | 124.2 (0.1) | 128.0 (0.3) | 148.3 (0.9) | 130.7 (0.6) |
| Diastolic blood pressure, mm Hg | 66.5 (0.3) | 70.4 (0.4) | 78.6 (0.3) | 82.5 (0.7) | 71.1 (0.4) |
| Mean 10-year predicted CVD risk†† | 2.4 (0.1) | 5.0 (0.2) | 5.9 (0.3) | 13.1 (0.6) | 17.8 (0.4) |
| High risk†††, % | 7.5 | 15.1 | 19.8 | 46.1 | 61.8 |
| 10-year risk categories, % | |||||
| <5% | 85.6 | 69.7 | 63.5 | 37.4 | 21.7 |
| 5% to <10% | 6.9 | 15.2 | 16.7 | 16.4 | 16.6 |
| 10% to <20% | 3.2 | 6.8 | 10.5 | 19.8 | 19.7 |
| ≥20% | 1.5 | 4.7 | 5.1 | 20.4 | 20.1 |
| History of CVD | 2.9 | 3.6 | 4.2 | 6.0 | 21.9 |
Population characteristics in the table are percentage or mean (standard error).
US adults were grouped into the higher category of systolic and diastolic blood pressure. For example, if a person had systolic blood pressure of 146 mm Hg and diastolic blood pressure of 82 mm Hg, they were grouped into the ≥140/90 mm Hg category.
Reduced estimated glomerular filtration rate was defined by levels < 60 ml/min/1.73 m2.
Albuminuria was defined by an albumin-to-creatinine ratio ≥ 30 mg/g.
10-year predicted risk was calculated using the Pooled Cohort risk equations. Mean risk was calculated among adults without a history of cardiovascular disease.
High risk defined as a 10-year predicted cardiovascular disease risk ≥ 10% or history of cardiovascular disease.
SBP – systolic blood pressure; DBP – diastolic blood pressure; eGFR - estimated glomerular filtration rate; CVD – cardiovascular disease.
NHANES sampling weights were used in all calculations to obtain US nationally representative prevalence estimates. These weights were recalibrated based on the proportion of participants missing data by age, gender, and race-ethnicity within each NHANES cycle. Recalibration of the sampling weights corrects for differences in missing data across age, gender and race-ethnicity strata and assumes that data within strata are missing at random.(6) Data management was conducted in SAS version 9.4 (SAS Institute, Cary, NC) and data analysis was conducted in Stata V14 (Stata Corporation, College Station, TX).
Results
In 2011–2014, 42.3%, 12.1%, 13.7% and 7.7% of US adults not taking antihypertensive medication had SBP/DBP levels of <120/80, 120–129/<80, 130–139/80–89, and ≥140/90 mm Hg, respectively (Table 2). Additionally, 24.1% of US adults were taking antihypertensive medication. US adults with higher BP were older, more likely to be non-Hispanic black, taking a statin, and have diabetes, reduced eGFR, albuminuria and a history of CVD. Total cholesterol levels and mean 10-year predicted CVD risk were higher at higher BP levels.
The prevalence of hypertension was 45.6% and 31.9% according to the 2017 ACC/AHA and JNC7 guideline definitions, respectively (Table 3). The prevalence of hypertension was higher when defined by the 2017 ACC/AHA guideline compared to the JNC7 guideline within all age, gender, race-ethnicity, and CVD risk category sub-groups. Antihypertensive medication was recommended for 36.2% of US adults according to the 2017 ACC/AHA guideline compared to 34.3% of adults with hypertension recommended antihypertensive medication according to the JNC7 guideline. An increase in the percentage of the population recommended antihypertensive medication by the 2017 ACC/AHA guideline compared to JNC 7 report was present for all age, sex, race-ethnicity and CVD risk sub-groups investigated. Among US adults with SBP/DBP of 130–139/80–89 mm Hg, 31.3% were recommended antihypertensive medication according to the 2017 ACC/AHA guideline because they had diabetes, CKD, high CVD risk or they had SBP of 130–139 mm Hg and were ≥ 65 years of age (Figure 1).
Table 3.
Percentage of US adults meeting the definition for hypertension and recommended antihypertensive medication according to the 2017 ACC/AHA guideline and the JNC7 guideline based on the 2011–2014 National Health and Nutrition Examination Survey.
| 2017 ACC/AHA guideline | JNC7 guideline | Difference (2017 ACC/AHA but not JNC7) |
||||
|---|---|---|---|---|---|---|
| Hypertension | Recommended antihypertensive medication |
Hypertension | Recommended antihypertensive medication |
Hypertension | Recommended antihypertensive medication |
|
| Overall | 45.6 (43.6, 47.6) |
36.2 (34.2, 38.2) |
31.9 (30.1, 33.7) |
34.3 (32.5, 36.2) |
13.7 (12.7, 14.9) |
1.9 (1.5, 2.3) |
| Age group | ||||||
| 20–44 | 24.0 (21.8, 26.2) |
12.5 (11.2, 13.9) |
10.5 (9.4, 11.7) |
12.2 (10.9, 13.6) |
13.4 (12.0, 15.0) |
0.3 (0.1, 0.5) |
| 45–54 | 47.1 (44.4, 49.8) |
33.4 (30.8, 36.1) |
29.5 (27.0, 32.2) |
32.7 (30.1, 35.4) |
17.6 (15.1, 20.4) |
0.7 (0.4, 1.2) |
| 55–64 | 66.6 (63.6, 69.5) |
58.2 (54.9, 61.4) |
52.4 (49.1, 55.7) |
55.0 (62.0, 58.0) |
14.2 (12.1, 16.6) |
3.2 (2.1, 4.7) |
| 65–74 | 75.6 (73.4, 77.6) |
74.1 (71.4, 76.6) |
63.6 (60.2, 66.9) |
66.9 (63.7, 69.9) |
12.0 (9.4, 15.2) |
7.2 (5.2, 10.0) |
| 75+ | 82.3 (79.2, 85.0) |
82.3 (79.2, 85.0) |
75.1 (71.9, 78.1) |
78.5 (74.7, 81.8) |
7.1 (5.6, 9.0) |
3.8 (2.5, 5.6) |
| Men | 48.6 (45.9, 51.3) |
37.3 (34.9, 39.8) |
32.0 (29.8, 34.3) |
34.8 (32.4, 37.3) |
16.6 (15.0, 18.3) |
2.5 (2.0, 3.1) |
| Women | 42.9 (40.7, 45.1) |
35.1 (33.1, 37.3) |
31.8 (29.8, 33.8) |
33.8 (31.8, 35.9) |
11.1 (9.8, 12.5) |
1.3 (0.9, 1.9) |
| Race-ethnicity | ||||||
| Non-Hispanic white | 47.3 (44.5, 50.0) |
37.9 (35.3, 40.6) |
33.4 (31.1, 35.8) |
35.7 (33.3, 38.2) |
13.8 (12.4, 15.4) |
2.2 (1.6, 2.8) |
| Non-Hispanic black | 54.9 (52.5, 57.3) |
44.8 (42.5, 47.0) |
41.0 (39.0, 43.1) |
43.6 (41.4, 45.8) |
13.9 (12.2, 15.7) |
1.2 (0.8, 1.8) |
| Non-Hispanic Asian | 36.7 (32.6, 40.9) |
27.9 (24.2, 32.0) |
24.4 (21.1, 28.2) |
26.8 (23.1, 30.8) |
12.2 (10.4, 14.3) |
1.1 (0.6, 2.0) |
| Hispanic | 34.4 (31.8, 37.1) |
25.5 (23.0, 28.1) |
21.1 (18.7, 23.8) |
24.3 (21.8, 26.9) |
13.3 (11.7, 15.1) |
1.2 (0.9, 1.6) |
| Risk categories | ||||||
| <5% | 27.4 (25.6, 29.3) |
14.6 (13.3, 16.0) |
13.2 (12.0, 14.5) |
14.6 (13.3, 16.0) |
14.2 (13.1, 15.4) |
0 |
| 5% to <10% | 61.4 (57.2, 65.3) |
48.4 (44.5, 52.3) |
42.7 (38.5, 47.1) |
46.6 (42.7, 50.5) |
18.6 (15.2, 22.6) |
1.8 (0.9, 3.6) |
| 10% to <20% | 78.2 (74.7, 81.4) |
78.2 (74.7, 81.4) |
63.6 (58.4, 68.5) |
68.3 (63.5, 72.7) |
14.6 (11.5, 18.4) |
9.9 (7.7, 12.7) |
| ≥20% | 85.7 (82.7, 88.2) |
85.7 (82.7, 88.2) |
77.3 (74.0, 80.3) |
81.4 (77.7, 84.6) |
8.4 (7.1, 9.8) |
4.3 (3.1, 5.8) |
| History of CVD | 79.3 (75.6, 82.6) |
79.3 (75.6, 82.6) |
72.1 (68.8, 75.3) |
75.7 (72.7, 78.4) |
7.2 (5.0, 10.3) |
3.7 (2.1, 6.2) |
Numbers in table are percentage of US adults (95% confidence interval)
See Table 1 for the definitions of hypertension and antihypertensive medication treatment recommendations.
2017 ACC/AHA guideline - 2017 American College of Cardiology/American Heart Association Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults.
JNC7 guideline - Seventh Report of the Joint National Committee on Prevention, Detection, and Treatment of High Blood Pressure
CVD – cardiovascular disease
Figure 1. Percentage of US adults with a systolic blood pressure of 130 to 139 mm Hg or diastolic blood pressure 80 to 89 mm Hg recommended antihypertensive medication according to the 2017 ACC/AHA guideline.
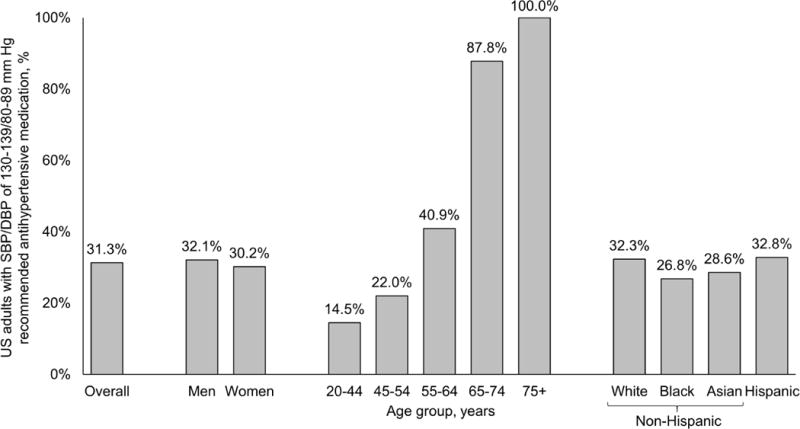
This figure shows the percentage of US adults not taking antihypertensive medication with systolic blood pressure of 130 to 139 mm Hg or diastolic blood pressure 80 to 89 mm Hg who are recommended antihypertensive medication. These individuals are recommended antihypertensive medication according to the 2017 ACC/AHA hypertension guideline because they have systolic blood pressure of 130 to 139 mm Hg or diastolic blood pressure 80 to 89 mm Hg and a history of cardiovascular disease or a 10-year predicted risk for cardiovascular disease ≥ 10%, diabetes or chronic kidney disease or they have systolic blood pressure of 130 to 139 mm Hg and are ≥ 65 years of age. Overall, 31.3% of US adults with systolic blood pressure of 130 to 139 mm Hg or diastolic blood pressure 80 to 89 mm Hg are recommended antihypertensive medication according to the 2017 ACC/AHA guideline. SBP – Systolic blood pressure; DBP – Diastolic blood pressure.
In 2011–2014, 103.3 million US adults met the definition for hypertension according to the 2017 ACC/AHA guideline compared with 72.2 million US adults according to the JNC7 guideline (Table 4). Based on use of the 2017 ACC/AHA guideline, 81.9 million US adults met criteria for treatment with antihypertensive medication in addition to nonpharmacological interventions whereas 21.4 million met criteria for treatment with nonpharmacological therapy on its own. An additional 4.2 million US adults were recommended antihypertensive medication according to the 2017 ACC/AHA guideline compared with the JNC7 guideline.
Table 4.
Number of US adults, in millions, meeting the definition for hypertension and the definition for treatment with antihypertensive medication according to the 2017 ACC/AHA guideline and the JNC7 guideline based on the 2011–2014 National Health and Nutrition Examination Survey.
| 2017 ACC/AHA guideline | JNC7 guideline | Difference (2017 ACC/AHA vs. JNC7) | ||||
|---|---|---|---|---|---|---|
| Hypertension | Recommended antihypertensive medication |
Hypertension | Recommended antihypertensive medication |
Hypertension | Recommended antihypertensive medication |
|
| Overall | 103.3 (92.7, 114.0) | 81.9 (73.8, 90.1) | 72.2 (65.3, 79.1) | 77.7 (70.0, 85.5) | 31.1 (26.6, 35.6) | 4.2 (3.3, 5.1) |
| Age group | ||||||
| 20–44 | 24.7 (21.6, 27.9) | 12.9 (11.3, 14.4) | 10.9 (9.6,12.2) | 12.6 (11.1, 14.1) | 13.9 (11.7, 16.0) | 0.3 (0.1, 0.5) |
| 45–54 | 20.1 (17.7, 22.6) | 14.3 (12.6, 15.9) | 12.6 (11.2,14.0) | 14.0 (12.4, 15.6) | 7.5 (5.9, 9.1) | 0.3 (0.1, 0.4) |
| 55–64 | 26.2 (22.4, 30.0) | 22.9 (19.6, 26.2) | 20.6 (17.7,23.5) | 21.6 (18.5, 24.7) | 5.6 (4.2, 6.9) | 1.3 (0.7, 1.8) |
| 65–74 | 18.5 (16.1, 20.9) | 18.1 (15.9, 20.4) | 15.6 (13.5,17.6) | 16.4 (14.3, 18.4) | 2.9 (2.1, 3.8) | 1.8 (1.1, 2.4) |
| 75+ | 13.8 (11.7, 15.8) | 13.8 (11.7, 15.8) | 12.6 (10.9, 14.3) | 13.1 (11.2, 15.1) | 1.2 (0.8, 1.6) | 0.6 (0.4, 0.9) |
| Men | 52.8 (46.6, 59.1) | 40.6 (35.7, 45.5) | 34.8 (30.6, 39.0) | 37.9 (33.2, 42.6) | 18.1 (15.3, 20.8) | 2.7 (2.0, 3.4) |
| Women | 50.5 (45.4, 55.6) | 41.4 (37.6, 45.1) | 37.4 (34.1, 40.8) | 39.9 (36.2, 43.5) | 13.1 (10.8, 15.4) | 1.5 (0.9, 2.1) |
| Race-ethnicity | ||||||
| Non-Hispanic white | 70.8 (58.3, 83.3) | 56.8 (47.1, 66.4) | 50.1 (41.7, 58.4) | 53.5 (44.4, 62.7) | 20.7 (16.0, 25.4) | 3.2 (2.2, 4.2) |
| Non-Hispanic black | 14.3 (11.3, 17.2) | 11.6 (9.2, 14.1) | 10.7 (8.4, 12.9) | 11.3 (8.9, 13.7) | 3.6 (2.8, 4.4) | 0.3 (0.2, 0.5) |
| Non-Hispanic Asian | 4.4 (3.5, 5.3) | 3.3 (2.6, 4.1) | 2.9 (2.3, 3.6) | 3.2 (2.5, 3.9) | 1.5 (1.1, 1.8) | 0.1 (0.0, 0.2) |
| Hispanic | 11.3 (8.4, 14.2) | 8.4 (6.0, 10.8) | 6.9 (4.8, 9.0) | 8.0 (5.7, 10.3) | 4.4 (3.4, 5.3) | 0.4 (0.2, 0.5) |
| Risk categories | ||||||
| <5% | 38.2 (33.6, 42.7) | 20.4 (18.0, 22.8) | 18.4 (16.2, 20.6) | 20.4 (18.0, 22.8) | 19.8 (16.9, 22.6) | 0 |
| 5% to <10% | 17.1 (14.3, 19.9) | 13.5 (11.3, 15.7) | 11.9 (9.9, 14.0) | 13.0 (11.0, 15.1) | 5.2 (3.8, 6.6) | 0.5 (0.1, 0.9) |
| 10% to <20% | 17.5 (15.3, 19.8) | 17.5 (15.3, 19.8) | 14.3 (12.4, 16.1) | 15.3 (13.4, 17.3) | 3.3 (2.3, 4.3) | 2.2 (1.5, 2.9) |
| ≥20% | 16.1 (13.8, 18.5) | 16.1 (13.8, 18.5) | 14.6 (12.5, 16.7) | 15.3 (13.0, 17.7) | 1.6 (1.2, 1.9) | 0.8 (0.6, 1.1) |
| History of CVD | 14.3 (12.6, 16.1) | 14.3 (12.6, 16.1) | 13.0 (11.4, 14.7) | 13.7 (12.0, 15.4) | 1.3 (0.8, 1.8) | 0.7 (0.3, 1.0) |
Numbers in table are number of US adults in millions (95% confidence interval)
2017 ACC/AHA guideline - 2017 American College of Cardiology/American Heart Association Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults.
JNC7 guideline - Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure
SBP – systolic blood pressure; DBP – diastolic blood pressure; CVD – cardiovascular disease.
See Table 1 for the definitions of hypertension and antihypertensive medication treatment recommendations.
Compared with US adults defined as having hypertension according to the JNC7 guideline, those with hypertension defined by the 2017 ACC/AHA guideline but not the JNC7 guideline were younger, had lower total cholesterol, SBP, DBP and 10-year predicted CVD risk levels, and were less likely to have diabetes, reduced eGFR, albuminuria and a history of CVD (Online Table 3). Those recommended antihypertensive medication by the 2017 ACC/AHA guideline but not the JNC7 guideline had lower mean SBP and DBP levels but a higher mean 10-year CVD risk than their counterparts recommended antihypertensive medication by the JNC7 guideline. Also, US adults in this group were older, more likely to be male, non-Hispanic white, cigarette smokers, and have a history of CVD.
Among US adults taking antihypertensive medication, 53.4% had above goal BP according to the 2017 ACC/AHA guideline compared to 39.0% with above goal BP according to the JNC7 guideline (Table 5). BP above goal, defined using thresholds from the 2017 ACC/AHA guideline instead of the JNC7 guideline, was more than 10 percentage points higher in each sub-group investigated except for those ≥ 75 years of age and taking ≥ 4 classes of antihypertensive medication, where the prevalence was 7.1 and 9.3 percentage points higher, respectively. In 2011–2014, 54.7 million US adults were taking antihypertensive medication of whom 29.2 and 21.3 million US adults had BP above goal according to the 2017 ACC/AHA and JNC7 guidelines, respectively (Online Table 4). Characteristics of US adults taking antihypertensive medication with BP above goal according to the 2017 ACC/AHA guideline, the JNC7 guideline, and the 2017 ACC/AHA but not the JNC7 guideline are presented in Online Table 5. Overall, 47.9% and 31.8% of US adults with BP above goal according to the 2017 ACC/AHA but not the JNC7 guideline were taking 1 and 2 classes of antihypertensive medication, respectively.
Table 5.
Percentage of US adults taking antihypertensive medication with blood pressure above the 2017 ACC/AHA guideline and the JNC7 guideline treatment goal based on the 2011–2014 National Health and Nutrition Examination Survey.
| Blood pressure above goal according to: | 2017 ACC/AHA but not the JNC guideline | ||
|---|---|---|---|
| 2017 ACC/AHA guideline | JNC7 guideline | ||
| Overall† | 53.4 (49.9, 56.8) | 39.0 (36.4, 41.6) | 14.4 (12.4, 16.5) |
| Age group | |||
| 20–44 | 46.3 (38.6, 54.3) | 23.2 (17.5, 30.0) | 23.1 (17.7, 29.7) |
| 45–54 | 46.0 (38.6, 53.5) | 29.5 (24.2, 35.5) | 16.4 (12.6, 21.2) |
| 55–64 | 50.5 (44.9, 56.0) | 33.1 (27.9, 38.6) | 17.4 (13.2, 22.6) |
| 65–74 | 54.4 (48.6, 60.1) | 43.4 (38.5, 48.4) | 11.0 (13.2, 22.6) |
| 75+ | 67.2 (61.4, 72.4) | 60.1 (54.1, 65.7) | 7.1 (5.1, 9.8) |
| Men | 51.8 (47.9, 55.7) | 37.5 (34.5, 40.6) | 14.3 (11.8, 17.2) |
| Women | 54.7 (50.1, 59.2) | 40.3 (36.6, 44.0) | 14.4 (11.9, 17.3) |
| Race-ethnicity† | |||
| Non-Hispanic white | 50.6 (46.6, 54.6) | 36.4 (33.3, 39.5) | 14.2 (11.7, 17.2) |
| Non-Hispanic black | 63.0 (58.4, 67.4) | 48.6 (44.2, 53.1) | 14.4 (12.2, 16.9) |
| Non-Hispanic Asian | 62.9 (53.6, 71.3) | 47.1 (39.0, 55.4) | 15.8 (12.0, 20.5) |
| Hispanic | 56.0 (50.7, 61.1) | 41.7 (36.4, 47.1) | 14.3 (11.6, 17.5) |
| Number of antihypertensive classes | |||
| 0 | 54.7 (38.3, 70.2) | 44.3 (28.2, 61.7) | 10.5 (3.0, 30.6) |
| 1 | 57.5 (52.9, 61.9) | 38.5 (35.0, 42.1) | 19.0 (16.1, 22.3) |
| 2 | 47.7 (41.4, 54.0) | 35.3 (30.0, 41.0) | 12.4 (9.6, 15.7) |
| 3 | 56.1 (47.8, 64.0) | 44.3 (37.3, 51.6) | 11.8 (8.0, 17.0) |
| ≥ 4 | 55.3 (47.8, 62.4) | 45.9 (39.4, 52.6) | 9.3 (5.6, 15.1) |
Numbers in table are percentage of US adults (95% confidence interval)
2017 ACC/AHA guideline - 2017 American College of Cardiology/American Heart Association Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults.
JNC7 guideline - Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure
See Table 1 for the definition of blood pressure treatment goals in the JNC7 and 2017 ACC/AHA guidelines.
SBP – systolic blood pressure; DBP – diastolic blood pressure; CVD – cardiovascular disease.
Comparison of the 2017 ACC/AHA guideline with JNC8 panel member report
Overall, 31.1% of US adults had hypertension according to the JNC8 panel member report (Online Table 6). Compared with the JNC8 panel member report, an additional 5.1% of US adults were recommended antihypertensive medication according to the 2017 ACC/AHA guideline. The percentage of US adults recommended antihypertensive treatment according to the 2017 ACC/AHA guideline but not the JNC8 panel member report was higher at older ages, among men compared with women, among non-Hispanic whites compared with other race/ethnic groups and was highest for US adults with 10-year predicted CVD risk of 10% to <20% and ≥20% compared with the their counterparts in the other risk categories. Overall, 28.7% of US adults had BP above goal according to the thresholds in the 2017 ACC/AHA guideline but met the BP goal according to the JNC8 panel member report (Online Table 7).
Discussion
The current study documents the potential impact of the 2017 ACC/AHA guideline definition of hypertension, recommendation for antihypertensive medication in addition to nonpharmacological interventions and BP goals with antihypertensive drug treatment for US adults (Central Illustration). We estimate that the 2017 ACC/AHA hypertension guideline will result in a substantial increase in the proportion of US adults defined as having hypertension. However, by using a combination of BP levels and CVD risk to guide treatment with antihypertensive medication, there will be only a small increase (1.9%) in the percentage of US adults who are recommended antihypertensive medication according to the 2017 ACC/AHA guideline compared to the JNC7 guideline. Also, 14.4% of US adults taking antihypertensive medication had a BP above the goal defined by the 2017 ACC/AHA guideline whereas they would have met the BP goal according to the JNC7 guideline. More intensive antihypertensive treatment is recommended to achieve the 2017 ACC/AHA guideline BP goal for these individuals.
Central Illustration. Prevalence of hypertension, recommendation for pharmacologic antihypertensive treatment, and blood pressure above goal among US adults according to the 2017 ACC/AHA guideline and the JNC7 guideline.
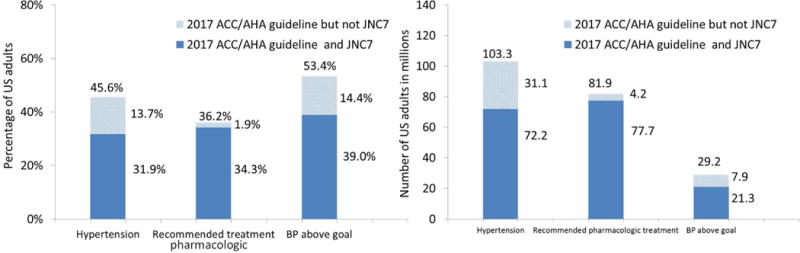
This graph shows the percentage (left panel) and number (right panel) of US adults with hypertension, recommended pharmacological treatment and with blood pressure above goal among those receiving pharmacological treatment according to the 2017 ACC/AHA guideline (full bar height), the JNC7 guideline (dark blue bar), and the 2017 ACC/AHA guideline but not the JNC7 guideline (light blue bar).
The lower SBP and DBP levels (130 and 80 mm Hg, respectively) used to define hypertension in the 2017 ACC/AHA guideline were based on data from observational studies and clinical trials. Large observational studies demonstrate a graded association between higher BP and increased risk for CVD, end-stage renal disease, subclinical atherosclerosis, and all-cause mortality.(7,8) While many studies have reported increased risk associated with SBP/DBP of 120–129/80–84 mm Hg versus <120/80 mm Hg, the association is substantially stronger for a SBP/DBP of 130–139/85–89 mm Hg versus <120/80 mm Hg.(9–12) Randomized controlled trials of lifestyle modification (13–15) and low dose antihypertensive medication(16–18) have demonstrated BP and CVD risk reduction benefits among adults with BP lower than those used to identify hypertension in the JNC7 guideline. In addition, intensive antihypertensive drug treatment in patients with hypertension to BP goals below those recommended in the JNC7 guideline have been associated with CVD and mortality risk reduction benefits.(19–26) Nonpharmacological therapy on its own is the recommended treatment for the majority of US adults with SBP/DBP of 130–139/80–89 mm Hg. The 2017 ACC/AHA guideline writing committee concluded there is insufficient evidence to support a recommendation for antihypertensive drug treatment in addition to nonpharmacological therapy for adults with SBP/DBP of 130–139/80–90 mm Hg and low CVD risk. However, the diagnosis of hypertension provides an opportunity for healthcare providers and patients to discuss the value of nonpharmacological therapy in lowering BP, to implement recommended lifestyle changes and to emphasize that BP is a risk factor that can be controlled.
CVD risk is used in conjunction with BP levels to guide the recommendation to initiate antihypertensive medication in the 2017 ACC/AHA guideline. This decision was based on a diverse set of data from randomized trials, observational studies and simulation analyses.(27) In a meta-analysis of 11 trials (n=51,917 participants), the absolute CVD risk reduction over 5 years of follow-up was −1.41, −1.95, −2.41, and −3.84 events per 1,000 participants with 5-year predicted risk <11%, 11%–15%, 15%–21%, and >21%, respectively.(28) Also, simulation analyses have showed that using CVD risk in conjunction with BP levels has the potential to prevent more CVD events than basing treatment on BP levels alone and using CVD risk in conjunction with BP levels to guide antihypertensive medication may be cost-effective.(29,30) In the current study, we estimated that the 2017 ACC/AHA and JNC7 guidelines would result in a small increase in the percentage of US adults being recommended antihypertensive medication. US adults recommended antihypertensive medication according to the 2017 ACC/AHA but not the JNC7 guideline had high CVD risk with 15.8% of this population having a history of CVD and a mean 10-year predicted CVD risk of 15.6% among those without a history of CVD. Based on the randomized trial evidence, this group should experience a large absolute reduction in CVD risk with antihypertensive medication (28).
A number of randomized controlled trials have evaluated the potential CVD risk reduction benefits of BP goals lower than those used in JNC7.(20–22) The best evidence supporting BP treatment targets is derived from meta-analyses of these trials.(19,23–26) In a meta-analysis of 42 trials (n=144,220 participants), the risk for CVD mortality was lowest with SBP levels between 120 and 124 mmHg.(23) Although some adults will benefit from treatment to lower BP levels, the 2017 ACC/AHA guideline writing committee selected SBP/DBP goals of 130/80 mm Hg to account for the specific inclusion and exclusion criteria used in randomized trials and the more careful conduct of BP measurement performed in trials compared with clinical practice (20).
The current analysis has several strengths. NHANES provides nationally representative estimates for the non-institutionalized US population and the results of this analysis have broad generalizability. NHANES enrolled a large sample size and oversampled population groups that facilitated the conduct of sub-group analysis. Blood pressure was measured following a standardized protocol. The results should also be interpreted in the context of known and potential limitations. Blood pressure was measured at a single visit in NHANES. Also, the BP measurement protocol including the use of a mercury sphygmomanometer likely differs from the typical approach used in most settings. The 2017 ACC/AHA and JNC7 guidelines recommend the diagnosis of hypertension be based on the average of multiple blood pressure measurements obtained at two or more visits.
In conclusion, the current analysis suggests a substantial increase in the prevalence of hypertension using the 2017 ACC/AHA guideline. However, the percentage of US adults recommended antihypertensive medication increased modestly with nonpharmacological interventions alone being recommended for the majority of US adults with hypertension according to the 2017 ACC/AHA guideline but not the JNC7 guideline. Additionally, over 50% of US adults taking antihypertensive medication do not meet the SBP/DBP goal of < 130/80 mm Hg set forth in the 2017 ACC/AHA guideline. More intensive antihypertensive drug therapy is recommended for this group. Given the high predicted CVD risk in this group, a substantial CVD risk reduction benefit should occur with more intensive antihypertensive medication treatment. The 2017 ACC/AHA hypertension guideline has the potential to increase hypertension awareness, encourage lifestyle modification and focus antihypertensive medication initiation and intensification on US adults with high CVD risk.
Supplementary Material
Condensed abstract.
The 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults provides recommendations for the definition of hypertension, antihypertensive medication treatment and blood pressure target goals. According to this guideline, 45.6% of US adults have hypertension and 36.2% are recommended antihypertensive treatment. Non-pharmacological intervention is advised for US adults (9.4%) with hypertension according to this guideline who are not recommended antihypertensive medication. Among US adults taking antihypertensive medication, 53.4% had BP above the treatment goal according to the 2017 ACC/AHA guideline and are recommended more intensive antihypertensive treatment.
Perspectives.
Clinical Competencies: Hypertension is a major risk factor for cardiovascular disease in the US and worldwide. Using cardiovascular risk in conjunction with blood pressure levels is an efficient approach to direct pharmacological antihypertensive treatment to those who are likely to benefit most. Many US adults are recommended more intensive antihypertensive medication according to the 2017 ACC/AHA Hypertension Guideline.
Translation outlook: Implementation of the 2017 ACC/AHA Hypertension Guideline has the potential to increase the prevalence of hypertension and use of antihypertensive medication among US adults. This should translate into a reduction in cardiovascular disease events.
Acknowledgments
Paul Muntner receives research support through grant 15SFRN2390002 from the American Heart association.
Abbreviations
- ACC/AHA
American College of Cardiology/American Heart Association
- CKD
Chronic kidney disease
- CVD
Cardiovascular disease
- DBP
Diastolic blood pressure
- JNC7
Seventh Report of the Joint National Committee on Prevention–Detection, Evaluation and Treatment of High Blood Pressure
- NHANES
National Health and Nutrition Examination Survey
- SBP
Systolic blood pressure
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Dr. Muntner has received research support and honoraria from Amgen, Inc. unrelated to this manuscript. All other authors report no disclosures.
References
- 1.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. J Am Coll Cardiol. 2017 [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 3.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 4.NHANES. 1999–2002 addendum to the NHANES III analytic guidelines. 2004 Available at http://www.cdc.gov/nchs/data/nhanes/guidelines1.pdf. Accessed September 7, 2004.
- 5.Goff DC, Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2935–59. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. AmJ Kidney Dis. 2003;41:1–12. doi: 10.1053/ajkd.2003.50007. [DOI] [PubMed] [Google Scholar]
- 7.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet (London, England) 2014;383:1899–911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 9.Shen L, Ma H, Xiang MX, Wang JA. Meta-analysis of cohort studies of baseline prehypertension and risk of coronary heart disease. Am J Cardiol. 2013;112:266–71. doi: 10.1016/j.amjcard.2013.03.023. [DOI] [PubMed] [Google Scholar]
- 10.Huang Y, Wang S, Cai X, et al. Prehypertension and incidence of cardiovascular disease: a meta-analysis. BMC Med. 2013;11:177. doi: 10.1186/1741-7015-11-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang Y, Cai X, Li Y, et al. Prehypertension and the risk of stroke: a meta-analysis. Neurology. 2014;82:1153–61. doi: 10.1212/WNL.0000000000000268. [DOI] [PubMed] [Google Scholar]
- 12.Huang Y, Cai X, Zhang J, et al. Prehypertension and Incidence of ESRD: a systematic review and meta-analysis. Am J Kidney Dis. 2014;63:76–83. doi: 10.1053/j.ajkd.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 13.The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, Phase I. JAMA. 1992;267:1213–20. doi: 10.1001/jama.1992.03480090061028. [DOI] [PubMed] [Google Scholar]
- 14.Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. The Trials of Hypertension Prevention Collaborative Research Group. Arch Intern Med. 1997;157:657–67. [PubMed] [Google Scholar]
- 15.Cook NR, Cutler JA, Obarzanek E, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP) BMJ. 2007;334:885–8. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Julius S, Nesbitt SD, Egan BM, et al. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med. 2006;354:1685–1697. doi: 10.1056/NEJMoa060838. [DOI] [PubMed] [Google Scholar]
- 17.Fuchs SC, Poli-de-Figueiredo CE, Figueiredo Neto JA, et al. Effectiveness of Chlorthalidone Plus Amiloride for the Prevention of Hypertension: The PREVER-Prevention Randomized Clinical Trial. J Am Heart Assoc. 2016;5 doi: 10.1161/JAHA.116.004248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luders S, Schrader J, Berger J, et al. The PHARAO study: prevention of hypertension with the angiotensin-converting enzyme inhibitor ramipril in patients with high-normal blood pressure: a prospective, randomized, controlled prevention trial of the German Hypertension League. J Hypertens. 2008;26:1487–96. doi: 10.1097/HJH.0b013e3282ff8864. [DOI] [PubMed] [Google Scholar]
- 19.Verdecchia P, Angeli F, Gentile G, Reboldi G. More Versus Less Intensive Blood Pressure-Lowering Strategy: Cumulative Evidence and Trial Sequential Analysis. Hypertension. 2016;68:642–53. doi: 10.1161/HYPERTENSIONAHA.116.07608. [DOI] [PubMed] [Google Scholar]
- 20.Wright JT, Jr, Williamson JD, Whelton PK, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373:2103–16. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benavente OR, Coffey CS, et al. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013;382:507–15. doi: 10.1016/S0140-6736(13)60852-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cushman WC, Evans GW, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–85. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bundy JD, Li C, Stuchlik P, et al. Systolic Blood Pressure Reduction and Risk of Cardiovascular Disease and Mortality: A Systematic Review and Network Meta-analysis. JAMA Cardiol. 2017;2:775–781. doi: 10.1001/jamacardio.2017.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bangalore S, Toklu B, Gianos E, et al. Optimal Systolic Blood Pressure Target after SPRINT Insights from a Network Meta-Analysis of Randomized Trials. Am J Med. 2017 doi: 10.1016/j.amjmed.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 25.Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387:435–43. doi: 10.1016/S0140-6736(15)00805-3. [DOI] [PubMed] [Google Scholar]
- 26.Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 7. Effects of more vs. less intensive blood pressure lowering and different achieved blood pressure levels - updated overview and meta-analyses of randomized trials. J Hypertens. 2016;34:613–22. doi: 10.1097/HJH.0000000000000881. [DOI] [PubMed] [Google Scholar]
- 27.Muntner P, Whelton PK. Using Predicted Cardiovascular Disease Risk in Conjunction With Blood Pressure to Guide Antihypertensive Medication Treatment. J Am Coll Cardiol. 2017;69:2446–2456. doi: 10.1016/j.jacc.2017.02.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sundstrom J, Arima H, Woodward M, et al. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384:591–8. doi: 10.1016/S0140-6736(14)61212-5. [DOI] [PubMed] [Google Scholar]
- 29.Sussman J, Vijan S, Hayward R. Using benefit-based tailored treatment to improve the use of antihypertensive medications. Circulation. 2013;128:2309–17. doi: 10.1161/CIRCULATIONAHA.113.002290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moise N, Huang C, Rodgers A, et al. Comparative Cost-Effectiveness of Conservative or Intensive Blood Pressure Treatment Guidelines in Adults Aged 35–74 Years: The Cardiovascular Disease Policy Model. Hypertension. 2016;68:88–96. doi: 10.1161/HYPERTENSIONAHA.115.06814. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


