Key points
Pleural plaques are often identified incidentally on a chest radiograph and are a marker of previous asbestos exposure
Isolated pleural plaques do not normally need active follow up in asymptomatic patients
Diffuse pleural thickening (DPT) may cause breathlessness and is thought to be a consequence of benign asbestos pleural effusions
Rounded atelectasis is a particular form of DPT that may appear mass-like on chest radiology
Asbestosis is a form of diffuse pulmonary fibrosis that relates to previous asbestos exposure, and appears as a usual interstitial pneumonitis (UIP) type pattern on high resolution computed tomography (HRCT)
Background
Asbestos is a collective name given to a number of naturally occurring mineral silicates, the use of which can be traced back more than 4,000 years, as asbestos mines were certainly in existence in Roman times. Of the six recognised forms of asbestos, the most commercially relevant of these have been the serpentine chrysotile (white asbestos) and the amphiboles amosite (brown asbestos) and crocidolite (blue asbestos).
Asbestos has a wide range of properties that were useful to industrial processes, particularly its strength, heat and electrical resistance and its ability to withstand corrosion by acids and sea water. It was therefore used widely in the UK as a fire-resistant building material, as an industrial insulator, and in the production of ships and railway carriages.
Exposure to asbestos is linked with a number of different respiratory conditions, which can be separated into malignant and non-malignant diseases. This article considers the non-malignant conditions.
Pleural plaques
Background
Pleural plaques are often identified incidentally on a chest X-ray (see Fig 1). They represent areas of hyaline thickening of the parietal pleura and only become visible once calcified. They should be regarded as markers of -previous asbestos exposures and identify that the patient may have an increased risk of developing more serious asbestos-related conditions in the future, depending on the previous level and duration of their exposure.
Fig 1.
Chest radiograph of bilateral calcified pleural plaques.
Symptoms
Pleural plaques are not thought to cause symptoms, and another cause should be sought if symptoms are present. In the authors’ experience, patients with extensive pleural plaques only occasionally report non-specific chest pain that does not have any other clear cause. It is also interesting to note that the presence of plaques has been associated with angina-type chest pain.1
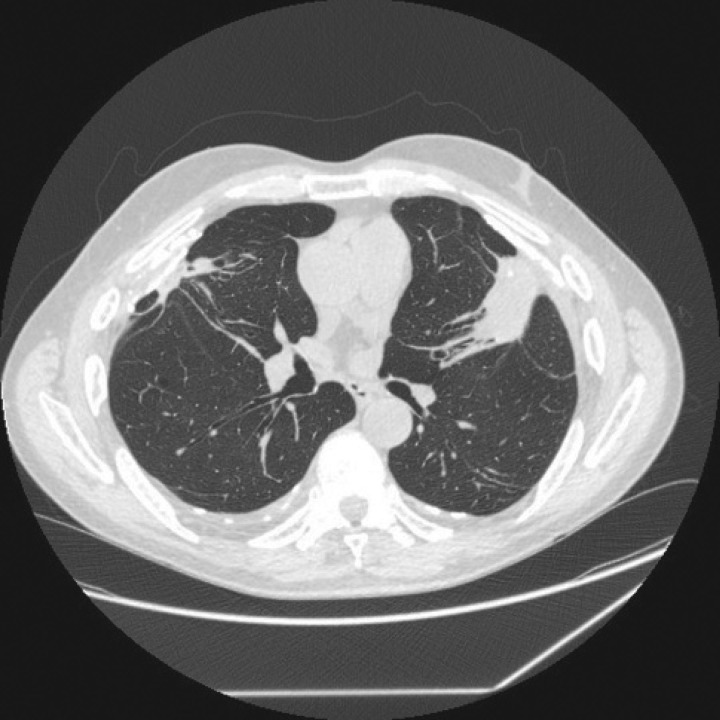
Radiology
A chest X-ray normally shows bilateral -calcified pleural abnormalities. Computerised tomography (CT) will also identify non-calcified plaques and confirm or exclude the presence of diffuse pleural thickening or interstitial lung disease (asbestosis). The lung tissue directly beneath a pleural plaque often looks irregular on a CT image, and this ‘plaque-related fibrosis’ in isolation should not be mistaken for early asbestosis.
Physiology
Isolated pleural plaques do not alter the results of lung function tests.
Diagnosis
The diagnosis of pleural plaques is usually straightforward, particularly when the typical radiological appearance is accompanied by a history of previous asbestos exposure. Although patients with pleural plaques may not recall previous exposure to asbestos, an occupational history will often highlight relevant job titles that confirm past exposure.2
Computed tomography is very useful to define the pleura and parenchyma in more detail. Although bilateral calcified pleural plaques are usually due to previous asbestos exposure, non-asbestos-related differential diagnoses occasionally need to be considered. These would include previous tuberculosis, haemothorax, pleurodesis, early mesothelioma, myeloma and rib fractures.
Treatment and follow up
After making a diagnosis of isolated pleural plaques, patients should normally be discharged from follow up. However, when patients are anxious about the future risks of more serious asbestos-related complications, it may be sensible to offer follow up to allow patients access to clinicians with a good working knowledge of these issues.
Advice to the patient and future lifetime risks
Patients often wish to discuss future risks, although the evidence base is poor. The authors’ practice is to quote approximate future lifetime risks as follows: 5–10% for ‘progression’ of plaques’ extent or visibility, 2–5% for the development of diffuse pleural thickening and 1–2% for mesothelioma. The latter figure may be higher in patients with certain high-risk occupations such as carpentry – a Health and Safety Executive case–control study quotes a lifetime risk of 5.9% for carpenters born in the 1940s.2
Diffuse pleural thickening
Diffuse pleural thickening is also a common consequence of exposure to asbestos, with about 400–500 new cases assessed for government-funded benefits each year in Great Britain. This condition involves the visceral pleura. than pleural plaques. Benign exudative effusions are often seen in association with diffuse pleural thickening, and both are manifestations of asbestos-related pleuritis.
Symptoms
Pleural thickening can cause significant symptoms, including shortness of breath and chest discomfort.
Radiology
A chest X-ray will normally show evidence of pleural thickening, a typical feature of which is blunting of the costophrenic angle, although it is possible to have significant pleural thickening without loss of this angle. Computed tomography will exclude extra pleural fat as a cause of the appearance on chest X-ray and confirm or exclude the presence of pleural plaques and asbestosis (see Fig 2).
Fig 2.
Computed tomography image of rounded atelectasis.
Physiology
Pleural thickening may cause extra pulmonary restriction.
Diagnosis
This is normally made using a combination of symptoms, radiology and knowledge of the extent and timing of exposure to asbestos. Benign asbestos effusion is a diagnosis of exclusion and commonly requires thoracoscopic biopsies to exclude malignant mesothelioma. It should be noted that these effusions may or may not be associated with pleuritic pain and can recur in the ipsilateral or contralateral pleural space.
Treatment and follow up
Even after negative thoracoscopic biopsies, it may be difficult to differentiate diffuse pleural thickening from desmoplastic mesothelioma. The severity of benign pleural thickening may also progress over time, so patients require careful follow up in a specialist respiratory centre.
Advice to the patient and future lifetime risks
Pleural thickening may progress and may be associated with further interval benign pleural effusions over time. Future risks for lung cancer and mesothelioma are increased, although the evidence for estimates given in this context is again poor.
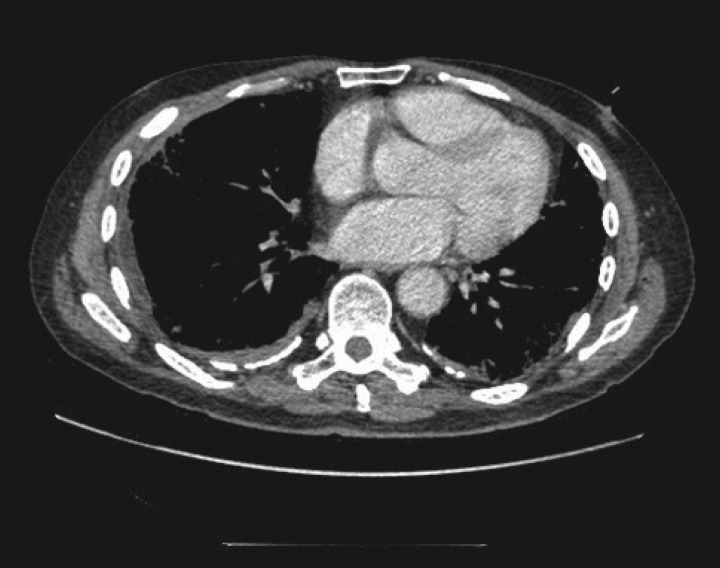
Rounded atelectasis (or Blesovsky syndrome)
This is a form of pleural thickening that causes the particular radiological appearance of a mass-like, rounded opacity. A possible mechanism by which this occurs is a low-grade inflammatory reaction at one pleural site, which results in the fusion of the two pleural surfaces and causes progressive thickening at the fused region.3 This results in compression of the underlying lung with associated collapse. The bronchus and adjacent blood vessels contribute to the ‘tail’ or classic comet sign seen on CT images (see Fig 3). Most cases are not associated with symptoms, but malignancy may need to be excluded because of the mass-like appearance on CT images.
Fig 3.
Computed tomography image of asbestos-related pleural thickening.
Box 1. Useful sources of information.
Asbestosis
Asbestosis is defined as fibrosis of the lung caused by asbestos. There are about 700 new cases of asbestosis each year in Great Britain, with the condition being responsible for around 400 deaths annually.
Symptoms
As pulmonary fibrosis advances, the patient typically will complain of increasing shortness of breath. Cough is also a common feature.
Radiology
This will normally show usual interstitial pneumonitis (UIP)-pattern disease on high-resolution CT (HRCT) images. The UIP pattern seen in asbestosis is not readily distinguishable from UIP of unidentified cause.4 The absence of pleural plaques does not exclude a diagnosis of asbestosis.
Physiology
Typical changes include progressive pulmonary restriction with reduced transfer factor and coefficient.
Diagnosis
The diagnosis of asbestosis would be supported by a history of significant previous asbestos exposure and requires the exclusion of other causes of diffuse pulmonary fibrosis. Most workers who develop asbestosis will have been exposed over prolonged periods – often for longer than 10 years. Lung biopsy is rarely carried out in patients with UIP-pattern disease in Great Britain. Even when tissue is available, there may be difficulties in interpreting current lung fibre counts due to historical exposure. In the authors’ experience, a detailed occupational history (considering job titles if recall of exposure to asbestos is poor) is usually sufficient to establish significant previous exposure to asbestos.
Treatment and follow up
The fibrosis from asbestosis is irreversible and often progresses slowly. Treatment for established asbestosis is therefore supportive, and long-term follow up within an occupational or interstitial lung disease (ILD) service is recommended.
Advice to the patient and future lifetime risks
Asbestosis is usually seen in patients with a history of prolonged and heavy exposure to asbestos, and they therefore also have an increased risk of lung cancer and mesothelioma. Evidence indicates that the future risk of lung cancer is particularly high in heavy smokers, with the risk being more than additive, so it is vital that these patients are given support for smoking cessation.
Financial assistance
Financial assistance varies in different countries. It is sensible to put any advice given to patients on benefits or compensation in writing. The following information relates to the UK:
Government compensation: Further information relating to compensation issues can be found at the relevant Department for Work and Pensions (DWP) website (see Box 1 for useful sources of information).
Civil law: Certain cases may also be compensated under civil law. The details of all such potential claims are best discussed with personal injury lawyers experienced in handling such cases.
Other compensation: Other compensation rights may be available, including those identified under the Pneumoconiosis etc. (Worker's Compensation) Act 1979.
Other financial help: This may be -available for patients with respiratory disability, so patients should check with the DWP via their website (see Box 1) or in person.
Conclusion
Although asbestos was established as a cause of pulmonary fibrosis as early as the 1920s and as a factor contributing to the development of lung cancer in the 1940s, it continued to be widely used until the mid 1980s. Peak exposure to asbestos in Great Britain was during the 1960s and 1970s, which, due to the long latency of asbestos diseases, will account for their continuing high prevalence in the decades to come.
Authors’ note
The content of this publication, including any opinions and/or conclusions expressed, are those of the authors alone and do not necessarily reflect Health and Safety Executive policy.
References
- 1.Mukherjee S, de Klerk N, Palmer LJ, et al. Chest pain in asbestos-exposed individuals with benign pleural and parenchymal -disease. Am J Respir Crit Care Med. 2000;162:1807–11. doi: 10.1164/ajrccm.162.5.9912012. [DOI] [PubMed] [Google Scholar]
- 2.Peto J, Rake C, Gilham C, Hatch J. Occupational, domestic and environmental mesothelioma risks in Britain. A case–control study. London: HSE Books; 2009. Available at: www.hse.gov.uk/research/rrpdf/rr696.pdf. [Accessed 27 November 2013] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cugell DW, Kamp DW. Asbestos and the pleura: a review. Chest. 2004;125:1103–17. doi: 10.1378/chest.125.3.1103. [DOI] [PubMed] [Google Scholar]
- 4.Copley SJ, Wells AU, Sivakumaran P, et al. Asbestosis and idiopathic pulmonary fibrosis: comparison of thin-section CT features. Radiology. 2003;229:731–6. doi: 10.1148/radiol.2293020668. [DOI] [PubMed] [Google Scholar]