Abstract
Models suggested for managing acute, non-elective, medical admissions include expanding geriatric services, extending the role of the acute physician and rejuvenating the role of the general physician. We investigated improving inpatient care by changing consultants' work patterns and placing a higher priority on the ward rounds. A focus group and a questionnaire were used to study the impact on several ward round parameters. All respondents reported an overall satisfaction: 93% rated the quality of care as good or excellent, 75% reported increased safe patient discharges and 68% observed improved teamwork. Length of stay reduced to 4 days from 5.3 days without an increase in readmission. The main themes showed improved quality of care, better assured patients and relatives, and better consultant job satisfaction, but also showed reduced junior doctors' independent decision-making and a slight reduction in specialty-related activity. The study concluded that placing a higher priority on ward rounds by altering consultants' work patterns has a positive impact on inpatient care.
Key Words: Ward rounds, medical hospital admissions, general physician, hospitalist, specialist
Introduction
The increasing challenges facing non-elective, medical hospital admissions have been highlighted in several reports.1–3 Despite the growing number of acute medical units (AMUs), acute physicians care for patients only for the first 24–72 hours. In contrast, hospitalists (general physicians) in the USA provide continuity of care throughout admission. Some studies have found that this reduces costs and length of stay without harming the quality of care.4,5 Two recent reports suggested the need to rejuvenate the generalist physician role in the UK. Unfortunately, the evidence base for best practice in organising acute medical care is still limited.6,7 The Royal College of Physician's report Hospital on the edge? The time for action1 also refers to a looming crisis in the medical workforce, which will have a significant impact on the development of generalist posts. Can the quality of inpatients' care be improved by changing the consultants' pattern of work? In this paper the authors present their own experience.
The authors' district general hospital serves a population of 220,000. There is an AMU, which comprises 45 beds, run by four acute medicine physicians, with an average of 30–40 daily admissions. In addition to all medical subspecialties, there are three care-of-the-elderly wards and six geriatricians who receive admissions directly from the AMU. The gastroenterology ward has 28 beds and receives both unselected acute medical patients and patients with gastroenterology problems. On average, on the ward, 60% are elderly general medical patients and 40% are patients with gastroenterology-related problems. There are three consultants who are dually accredited in general medicine and gastroenterology, one locum consultant and one advanced endoscopy consultant. The gastroenterologists take part in acute medicine on call, with a frequency of 1:8 for weekends and 1:16 for weekdays, and cover gastrointestinal tract bleeding on 1:8. The gastroenterology team also includes one specialty registrar (SpR), one staff grade, one foundation year 1 (FY1) trainee, two core medical specialty trainees and one vocational training scheme (VTS) trainee.
Traditionally two consultants provided ward cover at any one time, each doing twice-weekly rounds (two of the four rounds were done in the afternoon). A short early morning daily round was aimed at planning discharges and dealing with urgent problems. This, however, happened only on an ad-hoc basis and the arrangement failed if the allocated person was on leave. Furthermore, with significant pressure on the gastroenterology service from outpatient referrals, endoscopy services and the 18-week wait, ward cover was always rushed and was deemed second priority to other targets. Internally referred patients could wait for 2–5 days to be seen.
As a result of the above shortfalls, one of the gastroenterologists (also a regional adviser of the Royal College of Physicians) suggested a trial of a new model of ward cover, which entailed one of the gastroenterologists dropping his entire specialty-related bar 1 session to cover the full ward (28 beds) and the outliers for a period of 2 weeks on a rotational basis. During this time the gastroenterologist did five daily morning ward rounds and two sessions in the afternoon to review ward referrals and meet families. One session was to cover endoscopic retrograde cholangiopancreatography (ERCP) or bowel cancer screening, which has to be done by a named physician. After a period of 3 months an assessment was made of the experience.
Methods and design
The qualitative methods chosen were a focus group and a questionnaire. The focus group method has been advocated as promoting self-disclosure.8 Opinion shift reflects a positive effect of the focus group discussion.9 The questionnaire was used to collect data from a wider group of participants. The use of a focus group and a questionnaire was complementary to the study of the effects of the new working pattern and in data triangulation. Quantitative data relating to discharges, length of stay, readmission within 30 days and comparison with the same period of the previous year was extracted from the hospital database by the information analysis team.
A semi-structured question schedule for the focus group meeting was developed, together with the appropriate prompts for ensuring that the different areas of ward work were covered.10 The aim and purpose of sampling were to target healthcare professionals at different seniority levels. Nine professionals attended: two consultants, two junior doctors, the ward manager, two nurses and two secretaries. Participants were offered a chance to read and verify the transcript, but all declined. Open coding and grounded theory were used for analysis of the transcript. This involved a comparison of events, actions and interactions. Concepts, categories and themes were then grouped and related to form more abstract categories (ie inductive theory building).11
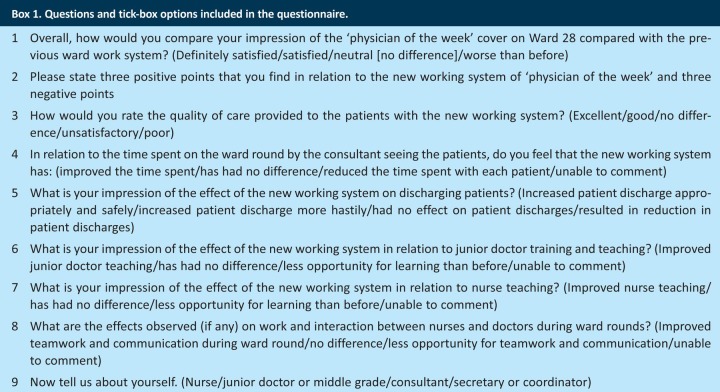
A combination of open and closed questions was used in the questionnaire (Box 1). Questionnaires were sent to all the ward nurses, junior doctors, middle grade staff, secretaries and consultants. One reminder was sent to non-respondents.
Box 1. Questions and tick-box options included in the questionnaire.
Results
Of 25 questionnaires 16 (64%) were returned. All respondents reported an overall satisfaction with the new model: 93% rated the quality of care provided as good or excellent; 81% felt that the time spent on the ward round by consultants seeing patients was improved; 75% reported increased appropriate and safe patient discharges; 68% observed improved teamwork; and 62% reported improved junior doctor teaching, although only 43% noticed improved teaching of nurses on the ward rounds. Patient length of stay was reduced to 4 days from 5.3 days without an increase in the readmission rate.
Analysis of the free text and the focus group script showed the following themes (listed in relation to each healthcare group).
The positive aspects listed by the nurses were:
improved quality of care: better and clearer management plan with quick response to changes in patient's condition linked to daily and sometimes twice-daily review
less anxiety from patients and family who feel assured by regular consultant's review.
The negative aspects listed by the nurses were:
increase in time-consuming tasks for nurses in view of the increased frequency of ward rounds and increased discharges with related paper work
over-reliance of junior doctors on consultants, sometimes waiting for the consultant to review the patients rather than seeing the patients as they land on the ward
lack of multidisciplinary ward rounds.
The positive aspects listed by the junior doctors were:
high-quality patient care with daily experienced decision-making, especially in critically ill patients
better ward-based teaching
better teamwork: junior doctors were able to get to know the consultant better through intensive and daily contact.
The negative aspects listed by the junior doctors were:
reduced opportunities for independent junior doctors' decision-making
increased workload because of increased discharges, which limit the opportunity for juniors to attend outpatient clinics and lunchtime teaching.
The positive aspects listed by the consultants were:
better job satisfaction: consultants felt that they provided a better quality of care to their patients where ward rounds were not rushed and took priority, as opposed to previously when it used to be second to achieving targets in outpatient clinics and the endoscopy unit
earlier discharges ensuring a shorter length of stay
more time to supervise junior doctors and teach them, as well as nurses, and even time to do ward-based assessments.
The negative aspects listed by the consultants were:
hard work in view of covering 28 patients on the base ward and 6–8 outliers on average
concern about possible negative impact on StR's general medicine experience. The consultant becomes the focal point for the junior doctors and the nurses. All ward queries are directed to the consultant who knows the patient well, as opposed to the StR, who most of the time is away from the ward fulfilling duties on the AMU or night on calls, or on teaching days.
The positive aspect listed by the secretaries and the managers were:
speedy review of inpatient referrals (24–48 hours) as opposed to previously when some review patients took up to 5 working days to be seen, relying on the consultant finding time in a busy schedule.
The negative aspects listed by the secretaries and the managers were:
a negative effect on outpatient and endoscopic activity as consultants took their annual leave when off the ward, which could mean 4 weeks without an outpatient clinic; this has the potential to spoil the 18-week wait and also the waiting time for endoscopy
increased administrative work.
Supporting quotes
Consultant
My job satisfaction is significantly better. Despite [the fact] I am working harder, I feel I am providing my best to the patients. Previously I [had] to squeeze the ward round among other things with the most [difficult] being the unpredictability of acute medicine and variable outlier numbers. All this added pressure to my job. Now I have enough time to cover in patients properly and look forward to 6 weeks break off ward doing mainly my specialty work.
Nurse
… the presence of the same consultant every day on the ward has been very reassuring for patients and relatives. Patients feel less anxious that things are being sorted out and [are given a] quicker diagnosis.
Junior doctor
… definitely improved quality of care and also teamwork. You get to know the consultant much closer and better by working together almost on a daily basis for 2 weeks. Good bedside teaching, but still very busy job with reduced opportunity for [outpatient] experience and formal teaching. Juniors also have to keep some independence doing their own ward rounds.
Ward manger
I have not seen any negative effects. The junior doctors and the nurses seem happier with the new ward system. Only when the hospital managers pull some of our staff to cover other wards do nurses struggle to join the consultant ward round.
Secretary
Processing ward referrals has become much easier and quicker. We now pass all referrals to the ward consultant who deals with them probably the same day. This means fewer phone calls chasing the referrals. A negative impact, however, has been some loss of endoscopy and [outpatient] activity as consultants now always take their leaves when off the ward.
Discussion
The ward round, once a fixed and inviolable feature of the hospital day, has suffered a gradual and significant decline. Despite being taken seriously by those involved, there is a sense that ward rounds now have to be fitted into a schedule of competing tasks in outpatient clinics and theatres.12 The Royal College of Physicians (RCP) and Royal College of Nursing joint report, Ward rounds in medicine: Principles for best practice, makes a number of suggestions for how deficiencies might be addressed.10 Re-forming the ward round will mean challenging established attitudes and behaviours, and strong medical and nursing leadership. The RCP is already playing a pivotal role in effecting safe acute medicine through a flurry of reports, publications and the Future Hospital Commission project.13
Our study has shown that specialists with dual accreditation can improve inpatient care with positive impact on several areas of the ward round. All questionnaire respondents and attendees at the focus group (25 in total) reported full satisfaction with the new working model. Improved time spent with each patient, improved teamwork and junior doctor and nurse teaching, as well as increased numbers of discharges, are among some of the advantages noticed. The results also showed reduced length of stay with no increase in readmission rate. The average length of stay on this ward is 4.0 days, which is lower than other medical wards' average of 5.7 and the national average of 5.5.14 In a cash-strapped NHS and high bed occupancy, this would be a welcome development. Furthermore, engagement of the staff in the process revealed an eagerness to do better for the patients. For example, one of the outcomes at the end of the focus group was to establish a 30-min multidisciplinary team (MDT) board round twice weekly, when all supporting health professionals (physiotherapist, occupational therapist, dietitian, pharmacist) attend to discuss difficult cases.
Job satisfaction is a very important factor in maintaining a healthy balance between work and life. It is clear from the RCP's members' survey that work pressure on consultants is increasing and job satisfaction declining.15 General medicine has become much less appealing to many of the specialists and even to trainees.16,17 The improved consultants' job satisfaction in our study may reflect the relief of the stress imposed on specialists while trying to prioritise their ward work over specialty-related work.
The gastroenterology ward receives a high number of general medical elderly patients from the AMU, despite the associated regular effort for appropriate triage and the fact that 38% of hospital medical beds are allocated for elderly patients. This is, however, consistent with the national trend of increasing emergency bed use by elderly patients, accounting for 68%.18 Although the gastroenterology consultants raised no specific issues in relation to caring for elderly general medical patients, we did not specifically investigate any deficiencies in their skills when looking after this group of patients. Further research is needed to explore this. The best model to manage an ageing population with multiple comorbidities has yet to be determined.
Any future strategy to improve inpatient care should appraise the three models suggested by Kirthi et al,19 namely: extending geriatrician numbers and services, extending acute physicians' role and the development of US-style hospitalists, compared with improving the current situation as suggested by the authors' project. The limited resources of the NHS make significant expansion of the number of geriatricians or AMU physicians quite difficult. Both the hospitalists and the acute physicians run the risk of burning out and of long-term career dissatisfaction.20 Our proposed model for ward cover might therefore be more practical and easier to implement than the three models suggested by Kirthi et al.19
Our study has some limitations, however; it is based on the experience of one ward in one district hospital. This might not apply to teaching hospitals or tertiary referral centres. These results need to be reproduced in other general hospitals.
No formal patient satisfaction questionnaires were done as part of this study. Most of the comments on the experience of patients and relatives came from nurses' responses. The authors also did not look at the optimum length of ward cover; however, on occasions when the cover extended to 3 weeks, the consultant felt strongly that this period of cover was extremely tiring and inappropriate. Despite the length of stay being shorter than the national average in this study, the authors have not explored the issue of delayed discharges and whether the new ward cover has affected it. Delayed discharges cost a 30 bed ward more than £500,000 annually.21
Finally, when estimating the effects on the specialty service, the authors worked towards making it cost neutral by running extra sessions using the off-ward consultants and the staff grade. On application, all consultants took their leave when they were off the ward, which meant that not all planned sessions happened. There is a rough estimate of a 5% loss of specialty-related activity.
Conclusions
Ward rounds can be re-established as a central element of daily hospital routine. Placing a high priority on ward rounds by altering the work pattern of the dually accredited specialists has a positive impact on inpatient care. This may be a way forward for a district general hospital to provide high-quality, safe, efficient, multidisciplinary ward rounds.
Key points
Non-elective medical hospital admissions are facing increasing challenges
The best model to manage an aging population with multiple comorbidities is as yet to be determined
The ward round – once a fixed and inviolable feature of the hospital day – has suffered a gradual and significant decline
Rejuvenating the generalist physician role in UK is suggested as a model to improve management of acute hospital admissions and continuity of care
Placing a higher priority on ward rounds by altering work pattern of consultants has a positive impact on inpatients care
References
- 1.Royal College of Physicians. Hospitals on the edge? The time for action. London: RCP; 2012. www.rcplondon.ac.uk/sites/default/files/documents/hospitals-on-the-edge-report.pdf [Accessed 25 September 2013]. [Google Scholar]
- 2.Blunt I, Bardsley M, Dixon J. Trends in emergency admission in England 2004–2009: is greater efficiency breading inefficiency? London: The Nuffield Trust; 2010. www.nuffieldtrust.org.uk/sites/files/nuffield/Trends_in_emergency_admissions_REPORT.pdf [Accessed 25 September 2013]. [Google Scholar]
- 3.Department of Health. GP patient survey Jan–Dec 2011, scaled to general life survey 2009. London: DH; 2011. webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/mediacentre/pressreleases/DH_128890 [Accessed 8 January 2013]. [Google Scholar]
- 4.Auerbach AD, Wachter RM, Cheng Q, et al. Comanagement of surgical patients between neurosurgeons and hospitalists. Arch Intern Med. 2010;170:2004–10. doi: 10.1001/archinternmed.2010.432. doi: 10.1001/archinternmed.2010.432. [DOI] [PubMed] [Google Scholar]
- 5.Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs. non-hospitalists. Mayo Clin Proc. 2009;84:248–54. doi: 10.4065/84.3.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Temple R, Kirthi V, Patterson L. Is it time for a new kind of hospital physician? Editorial. BMJ. 2012:344. doi: 10.1136/bmj.e2240. [DOI] [PubMed] [Google Scholar]
- 7.Wachter R, Bell D. Renaissance of hospital generalists. BMJ. 2012:344. doi: 10.1136/bmj.e652. doi: 10.1136/bmj.e652. [DOI] [PubMed] [Google Scholar]
- 8.Kreuger P. Focus groups: a practical guide for applied research. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 9.Morgan D, editor. Albrecht TL. Understanding communications process in focus group. Successful focus group. Newbury Park, CA: Sage; 1993. [Google Scholar]
- 10.Royal College of Physicians and Royal College of Nursing. A joint report. London: RCP; 2012. Ward rounds in Medicine. Principles for best practice. [Google Scholar]
- 11.Rice P, Ezzy D. Qualitative research methods. Oxford: Oxford University Press; 1999. [Google Scholar]
- 12.Amin Y. How to bring back ward rounds. The Guardian Oct 17. 2012 www.guardian.co.uk/healthcare-network/2012/oct/17/how-to-bring-back-ward-rounds [Accessed 10 January 2013]. [Google Scholar]
- 13.Royal College of Physicians. Hospital for the future: moving forward. Commentary. 2012; Dec:16–17. [Google Scholar]
- 14.NHS Information Centre. Hospital Episode Statistics on line (HES). Main specialty. www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=207 [Accessed 17 January 13].
- 15.Federation of the Royal Colleges of Physicians of the UK. Census of consultant physician and medical registrar in UK, 2010: data and commentary. London: RCP; 2011. www.rcplondon.ac.uk/sites/default/files/census-2010.pdf [Accessed 16 January 2013]. [Google Scholar]
- 16.Goddard A. Census of consultant physicians and medical registrar in the UK (2010) London: Royal College of Physicians; 2011. [Google Scholar]
- 17.Goddard A, Evans T, Phillips C. Medical registrars in 2010: experience and expectation of future consultant physicians of the UK. Clin Med. 2011;11:532–5. doi: 10.7861/clinmedicine.11-6-532. doi: 10.7861/clinmedicine.11-6-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The King's Fund. London: The King's Fund; 2012. Older people and emergency bed use, The King's Fund report. www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/older-people-and-emergency-bed-use-aug-2012.pdf [Accessed 23 February 2013]. [Google Scholar]
- 19.Kirthi V, Temple R, Patterson L. Inpatient care: should the general physician now take charge? Clin Med. 2012;12:316–19. doi: 10.7861/clinmedicine.12-4-316. doi: 10.7861/clinmedicine.12-4-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hodgson H. Hospitalists – too much baggage to travel? Clin Med. 2012;12:307–8. doi: 10.7861/clinmedicine.12-4-307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hendy P, Patel JH, Kordbacheh T, et al. In-depth analysis of delays to patient discharge: metropolitan teaching hospital experience. Clin Med. 2012;12:320–3. doi: 10.7861/clinmedicine.12-4-320. doi: 10.7861/clinmedicine.12-4-320. [DOI] [PMC free article] [PubMed] [Google Scholar]