Abstract
Patient and visitor violence adversely affects staff and organisations; however, there are few UK data about patient and visitor violence on medical wards. Therefore, we conducted a cross-sectional study using a validated tool (Survey of Violence Experienced by Staff) in six medical wards in three North Wales district general hospitals to assess the prevalence of violence against healthcare staff. A total of 158 staff responded (12 men, 144 women, two not stated). We found that, within the previous 4 weeks, 83% of staff had experienced verbal aggression, 50% had been threatened and 63% had been physically assaulted. Of those assaulted, 56% sustained an injury, with three requiring medical assessment or treatment. Length of experience in the workplace correlated negatively with verbal abuse, but not with threats or assaults. Direct patient contact positively correlated with more overall incidents. There was no correlation between training in aggression management and the experience of incidents. Healthcare support workers and nurses reported a higher prevalence of patient and visitor violence compared with other groups of health worker.
Key Words: Patient and visitor violence, violence and aggression, medical wards, percentage prevalence, general hospital
Introduction
Healthcare workers are one of the most likely groups to experience workplace aggression.1 Although violence and aggression can occur in all health settings, the most extensive evidence comes from psychiatric wards.2 The biggest single data set is the Annual National Audit of Violence conducted by the Royal College of Psychiatrists and funded by the British Healthcare Commission, whose final report was published in 2007 and contained information from 131 psychiatric wards across England and Wales.3 In this report, 58% of nurses reported career incidents that were upsetting or distressing (n=1,809) and 72% had felt threatened or feel unsafe. In addition, 46% had been physically assaulted over the previous year. Fewer doctors and non-clinical staff reported such experiences.3 Despite these results, a comparative international study showed that British psychiatric ward managers perceived violence and aggression to be a smaller problem on their wards compared with their Swiss and German counterparts. This was associated with the availability of control and restraint teams, regular training, clear protocols and, to a lesser degree, risk assessments, but not staffing levels.4
Outside the psychiatric setting, the picture is less clear. Hahn et al, in a systematic review of patient and visitor violence (PVV), concluded that ‘patient and visitor violence is a serious problem for healthcare staff in general hospitals, especially those working in medical and surgical units'.5 Owing to the heterogeneity of the included studies, it was difficult to gauge a comprehensive picture of the true situation. However, the data showed patient or visitor violence was most often separated into three specific types of incident: verbal aggression, threats and physical assaults. With regards to patient violence, the percentage figures for verbal aggression ranged from 9% in a Swedish study to 97% in a Turkish study. The percentages for threats were equally variable, ranging from 5% in a Jamaican study to 70% in a US study. For physical assaults, the range was from 3% in an Israeli study to 58% in a US study. The prevalence figures for visitor aggression were generally smaller. However, one American study reported that 74% of nurses had been subjected to visitor aggression. Most studies evaluated PVV over the whole lifetime career of a staff member, whereas others asked for PVV incidents over the previous 12 months. A finding from many of these studies was that, generally, verbal aggression was the most common occurrence, followed by verbal threats, whereas physical assaults were relatively few.5
In their 2008 systematic review, Hahn et al only included two studies from England.6,7 These studies were well conducted, but are now over 10 years old. A more recent cross-sectional survey by the same group showed that 50% of all staff (n=2,495) in a Swiss University Hospital had experienced PVV over the previous 12 months, with 11% having experienced it in the previous week.8 The authors further reported that ‘the age of the staff and the length of experience in their present workplace influenced the exposure to PVV’, with more experienced staff being subjected to less violence. Furthermore, they observed that violence occurred mainly during interventions involving personal contact.9
In the most recent (2012) annual UK National Health Service (NHS) staff survey, 15% of NHS staff reported experiencing physical violence from patients, their relatives or other members of the public over the previous 12 months. In total, 30% of all staff reported that they experienced bullying, harassment and abuse from patients, their relatives or other members of the public over the previous 12 months. Just under two-thirds of incidents of physical violence and 44% of bullying, harassment and abuse cases were reported. Those most likely to report violence or aggression were accident and emergency (A&E) doctors, as well as staff in psychiatry, sexual health and care of the elderly departments, as well as hospital receptionists.10,11
In a recent Australian sample, 70.6% of largely community-based medical practitioners who returned a questionnaire had experienced verbal or written aggression and 32.3% had experienced physical aggression from one or more sources over the previous 12 months. The authors concluded that ‘while patterns of exposure were complex, more female clinicians, international medical graduates and hospital-based clinicians experienced workplace aggression; age and postgraduate experience were significantly negatively associated with aggression exposure’.12
There is consistent evidence that violence towards healthcare staff is damaging on various levels. It affects negatively the psychological and physical well-being of healthcare staff as well as having a negative impact on job motivation and, more importantly, the ability to provide high-quality care.13–15 Workplace violence also has a negative economic impact on organisations in terms of work days lost and sickness absence. The financial losses ensued by healthcare systems through PVV are well documented in several studies.5 Given the relative lack of data regarding PVV on medical wards within the UK, we attempted to investigate its prevalence in acute medical wards across North Wales.
Methods
To investigate the prevalence of PVV on medical wards in the UK, we chose high-risk acute medical environments across North Wales using the Survey of Violence Experienced by Staff (SOVES) as our data collection tool. High-risk areas include assessment wards, gastroenterology and geriatric medical wards.5
The SOVES6,16 is one of the few existing internationally validated tools. This questionnaire includes questions about staff experience with violence within the previous 4 weeks, because this timeframe yields the best results without problems with recall bias. It separates verbal abuse from threats and physical assaults. If staff have experienced any of the former, they are asked to fill in how frequently this happened (1–5, 6–10, or >10). The SOVES collates information about staff training, the number of incidents in all three categories and the response by the organisation, including whether the incident was reported. We have abbreviated the SOVES to focus on the main aspect of percentage prevalence of experienced violence or aggression over the previous 4 weeks. Our adapted SOVES (SOVES-A; Appendix 1) is an abbreviated version of the original SOVES. We omitted information about reporting of incidents and the response of the organisation. We added one item in the physical assault section asking whether any treatment was required. Otherwise, the SOVES remained unchanged.
In our study, we defined PVV as experiencing verbal abuse, threats, and physical assaults from patients or visitors over the previous 4 weeks. We included additional questions about staff as a source of violence to distinguish staff and colleagues from visitors.
We conducted a survey using the SOVES-A in all three district general hospitals in North Wales (Ysbyty Gwynedd (YG), Ysbyty Glan Clwyd (YGC) and Ysbyty Wrecsam Maelor (YWM). The survey was logged with the local NHS audit department. No ethical issues were identified. We identified two geriatric or gastroenterology wards in each of the three hospitals with convenience sampling. These wards were targeted because they were known to be high-risk areas for PVV.5 We asked all staff visiting those wards regularly to participate by completing the SOVES-A in relation to the frequency and source of any aggression experienced by them personally within the previous 4 weeks. The response was improved by repeated prompts and reminders. The study period was between October and November 2011.
We used Pearson's Chi-square analysis on nominal data obtained, with Fisher's exact and trend analysis values being used where appropriate. For continuous data, t-tests and regression were used. All analyses were carried out with SPSS.
Results
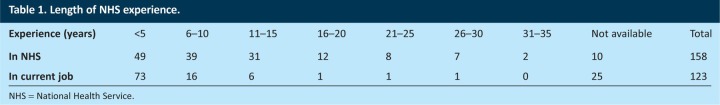
A total of 158 staff (12 male, 144 female, two not stated), including 75 nurses, 38 healthcare support workers (HCSW), eight doctors and 37 others, such as physiotherapists, occupational therapists, phlebotomists or pharmacists, returned the questionnaire. Forty-two percent of nurses and HCSW responded. Seventy percent of staff worked full time. The age of staff was between 18 and 64 years, with a mean of 37 years and a median of 36 years (Table 1).
Table 1.
Length of NHS experience.
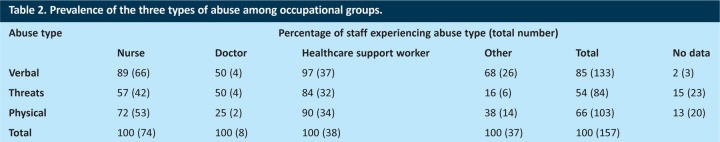
Eighty-three percent of staff (n=131/157) reported being verbally abused over the previous 4 weeks. In total, 55% (n=79/144) reported being threatened and 68% (n = 99/146) reported actual physical assault (Table 2). Of those assaulted, 56% sustained an injury and three needed medical assessment and/or treatment. Table 3 shows the frequency of abuse by role.
Table 2.
Prevalence of the three types of abuse among occupational groups.
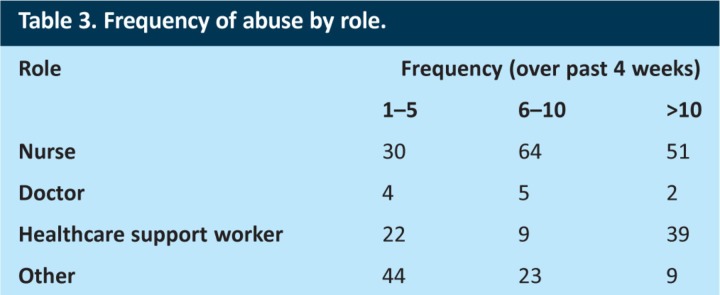
Table 3.
Frequency of abuse by role.
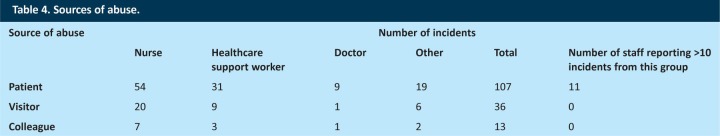
It can be seen from Table 4 that patients were responsible for most incidents. Eleven staff members reported more than 10 personal incidents directed from patients within 4 weeks. Interestingly, there were 13 incidents of horizontal violence (staff on staff), including verbal abuse or threats, but not physical assault.
Table 4.
Sources of abuse.
Not surprisingly, the percentage of staff time spent with patients independently positively correlated with the amount of all types of abuse, meaning that the overall incidence of abuse was higher among full-time staff. However, the relative prevalence of aggression towards part-time staff members was higher (trend analysis: 4.4; p=0.036), whereas the absolute number of incidents of all types was higher among full-time staff. We investigated whether there was a relation between the length of time working in the current post and frequency of abuse. The length of time in the current post was not a statistically significant protective factor against PVV (mean difference between groups was 95, with 95% confidence interval: −11, 201; p=0.074). However, using regression to test the hypothesis that the amount of overall experience (months working in the NHS as a dependent variable) could be a mitigating factor in abuse, we found that verbal abuse was more likely to occur 6.8 years earlier than the average of 23.8 years of service (B −82, T −2.98, p=0.003). This indicates a negative correlation (more experience, less abuse) when it comes to verbal, but not other types of abuse.
Discussion
We found that the most nursing staff and HCSWs had been subjected to PVV in some form in the preceding 4 weeks. In contrast to the common perception of psychiatric wards being a place of a high frequency of violence, we found high levels of PVV in the medical wards studied. Our results make an important contribution to what is currently a little-researched field. Even considering that we studied high-risk medical environments, the levels of violence and aggression we found equalled the highest figures that are internationally known. It emphasises the importance of addressing PVV in medical settings.
There were no statistically significant differences between professional roles because of the relatively limited numbers in our study. However, nurses and HCSWs clearly received the larger proportions of all kinds of aggression. Verbal abuse was more prevalent than all other forms of aggression, in keeping with previous research.
Our results showed that staff such as physiotherapists and phlebotomists, who visited the ward to carry out specific tasks, were subjected to aggression and violence comparatively more often despite relatively short direct patient contact.
We did not find a correlation between aggression management training and a lower frequency of being subjected to aggressive incidents. For all groups, aggression management training did not have a statistically significant impact on the risk of PVV, despite 52.5% (n=83) of staff having received formal de-escalation training and 37% (n=53) having received violence management training. This is the first finding of this kind and might indicate that aggression management training needs to be specifically geared towards medical high-risk areas to have an impact on violence against staff.
With regards to experience, longer service in the NHS was only correlated with less verbal abuse, but not with other forms of PVV. One possible explanation is that more experienced staff are able to de-escalate situations early on to avoid incidents of verbal abuse, whereas it might be more difficult to avoid the more serious incidents of threats and physical assaults once things have escalated to that level.
In contrast to other studies, we found that the numbers of incidents of physical abuse were higher than those of threats (but not verbal abuse). Given that physical abuse seems likely to be preceded by verbal abuse, staff probably recorded the more serious of the two incidents, neglecting to record the lesser one. However we were unable to examine individual incidents qualitatively to prove this.
As in other studies, we confirmed that nurses and HCSWs are more subject to violence and aggression than are doctors and other hospital workers, and this is probably because of their increased direct contact times. This study has contributed significantly to the data set available for general medical wards as opposed to psychiatric wards.
Limitations
Our study was limited to hospitals in North Wales; therefore, extrapolations to other parts of the UK should be made with caution. The study was limited to high-risk medical wards. Thus, studies in different hospital settings might not yield the same results. The study provides a cross-sectional picture and no conclusions should be drawn about specific patterns of PVV over time. Other limitations of our study include the relatively small number of doctors completing our survey. Our response rate was best among nurses and HCSW (42%) and good for a questionnaire study, but we might still have missed important contributions.
Conclusions
PVV appears to be a significant problem in high-risk medical wards. Given that it has negative personal and economic consequences, it needs to be addressed by any medical organisation. There is a need for further research in various healthcare settings to gain a better understanding of prevalence and management of PVV. We were unable to show an association between PVV and staff training, which calls into question the relevance of current training regimes for medical wards. Means to identify and communicate risk of aggression in the hope that this will reduce more serious incidents should be considered by management responsible for high-risk medical wards.
Acknowledgements
We would like to thank Rebecca Hoofe for her administrative support and Jean Burgess from the Betsi Cadwaladr University Health Board audit department for her support in processing the questionnaires. We thank all ward staff who participated in the study.
References
- 1.Chappell D, Di Martino V. Violence at work. 3rd edn. Geneva: International Labour Office; 2006. [Google Scholar]
- 2.Steinert T, Lepping P, Bernhardsgrütter R, et al. Incidence of seclusion and restraint in psychiatric hospitals: a literature review and survey of international trends. Soc Psychiatry Psychiatr Epidemiol. 2010;45:889–97. doi: 10.1007/s00127-009-0132-3. doi: 10.1007/s00127-009-0132-3. [DOI] [PubMed] [Google Scholar]
- 3.Royal College of Psychiatrists. Healthcare Commission National Audit of Violence 2006–7. Final Report – Working age adult services. London: RSPysch; 2007. www.rcpsych.ac.uk/pdf/WAA%20Nat%20Report%20final%20with%20all%20appendices.pdf [Accessed 27 September 2013]. [Google Scholar]
- 4.Lepping P, Steinert T, Needham I, et al. Ward safety perceived by ward managers in Britain, Germany and Switzerland: identifying factors that improve ability to deal with violence. J Psychiatr Ment Health Nurs. 2009;16:629–35. doi: 10.1111/j.1365-2850.2009.01425.x. doi: 10.1111/j.1365-2850.2009.01425.x. [DOI] [PubMed] [Google Scholar]
- 5.Hahn S, Zeller A, Needham I, et al. Patient and visitor violence in general hospitals: a systematic review of the literature. Aggression Violent Behav. 2008;13:431–41. doi: 10.1016/j.avb.2008.07.001. doi: 10.1016/j.avb.2008.07.001. [DOI] [Google Scholar]
- 6.Whittington R, Shuttleworth S, Hill L. Violence to staff in a general hospital setting. J Adv Nurs. 1996;24:326–33. doi: 10.1046/j.1365-2648.1996.18114.x. doi: 10.1046/j.1365-2648.1996.18114.x. [DOI] [PubMed] [Google Scholar]
- 7.Winstanley S, Whittington R. Aggression towards health care staff in a UK general hospital: variation among professions and departments. J Clin Nurs. 2004;13:3–10. doi: 10.1111/j.1365-2702.2004.00807.x. doi: 10.1111/j.1365-2702.2004.00807.x. [DOI] [PubMed] [Google Scholar]
- 8.Hahn S, Müller M, Needham I, et al. Measuring patient and visitor violence in general hospitals: feasibility of the SOVES-G-R, internal consistency and construct validity of the POAS-S and the POIS. J Clin Nurs. 2011;20:17–8. doi: 10.1111/j.1365-2702.2011.03768.x. doi: 10.1111/j.1365-2702.2011.03768.x. [DOI] [PubMed] [Google Scholar]
- 9.Hahn S, Hantikainen V, Needham I, et al. Patient and visitor violence in the general hospital, occurrence, staff interventions and consequences: a cross-sectional survey. J Adv Nurs. 2012;68:2685–99. doi: 10.1111/j.1365-2648.2012.05967.x. doi: 10.1111/j.1365-2648.2012.05967.x. [DOI] [PubMed] [Google Scholar]
- 10.NHS Staff survey 2011 – Detailed spreadsheets. www.nhsstaffsurveys.com/Page/1022/Past-Results/Staff-Survey-2011-Detailed-Spreadsheets/ [Accessed 30 October 2013].
- 11.National Health Service. Violence towards NHS staff from the public. London: NHS; 2011. www.nhsbsa.nhs.uk/SecurityManagement/Documents/violence_towards_NHS_staff_from_the_public.pdf [Accessed 30 October 2013]. [Google Scholar]
- 12.Hills DJ, Joyce CM, Humphreys JS. A national study of workplace aggression in Australian clinical medical practice. Med J Aust. 2012;197:336–40. doi: 10.5694/mja12.10444. doi: 10.5694/mja12.10444. [DOI] [PubMed] [Google Scholar]
- 13.Winstanley S, Whittington R. Violence in a general hospital: comparison of assailant and other assault-related factors on accident and emergency and inpatient wards. Acta Psychiatr Scand. 2002;106(Suppl 412):144–7. doi: 10.1034/j.1600-0447.106.s412.31.x. doi: 10.1034/j.1600-0447.106.s412.31.x. [DOI] [PubMed] [Google Scholar]
- 14.Needham I, Abderhalden C, Halfens RJG, et al. Non-somatic effects of patient aggression on nurses: a systematic review. J Adv Nurs. 2005;49:283–96. doi: 10.1111/j.1365-2648.2004.03286.x. doi: 10.1111/j.1365-2648.2004.03286.x. [DOI] [PubMed] [Google Scholar]
- 15.Arnetz JE, Arnetz BB. Violence towards health care staff and possible effects on the quality of patient care. Social Sci Med. 2001;52:417–27. doi: 10.1016/S0277-9536(00)00146-5. doi: 10.1016/S0277-9536(00)00146-5. [DOI] [PubMed] [Google Scholar]
- 16.McKenna K. North Eastern Health Board. Ireland: Committee on Workplace Violence; 2004. Study of work-related violence (project report) [Google Scholar]