Obesity, a mostly lifelong condition, is increasing in prevalence in the United Kingdom, such that approximately 26% of adults are obese.1 Similar proportions of children are also obese. The rates in the United Kingdom are some of the highest in the world, exceeded only by the United States.2 While obesity has a strong heritability, environmental changes interacting with this genetic susceptibility are driving a rapid increase in the prevalence and severity of the condition. Obesity causes, and is linked to, many complications, including type 2 diabetes, hypertension, ischemic heart disease, sleep apnoea, asthma and non-alcoholic fatty liver disease, as well as increasing the risk of several cancers and even dementia.3 Obesity is also modifying the presentation of, and treatment algorithms and strategies for, these associated morbidities.
About nine months ago an obesity working group was set up within the Royal College of Physicians (RCP) to consider and develop recommendations on the illness, and the report of this group has just been published.4
While some services for prevention and early community-based management exist (tier 1 and 2 services), there is inadequate provision for the multidisciplinary management of patients in the UK with obesity, especially when their condition is severe or complex (tier 3 and 4 services). A survey carried out for this report shows that only 37% of the population has recourse to a multidisciplinary bariatric team. There are currently also widespread differences in the rate of bariatric surgical operations in the country. In PCTs in England, the rate of bariatric procedures in hospital per 100,000 ranges from 0.4 to 41.3,5 reflecting rationing decisions rather than clinical need. These inequalities need to be rectified.
The report advocates a multidisciplinary approach to weight management and bariatric surgery. All members of the multidisciplinary team should be trained and experienced and should interact with primary care and tertiary centres. The primary care team has an important role in signposting to relevant services which are known to be effective. Long-term care of patients who have had bariatric surgery is important to avoid potentially serious complications.
Bariatric nursing is an important sub-specialty within obesity management that needs to be developed in collaboration with the Royal College of Nursing. Audit and research are also important, as well as translational and health services research.
Physicians should take a central role in commissioning obesity services for patients with what is best called ‘severe and complex obesity’, rather than concentrating solely on body mass index (BMI). Some patients with a BMI below 35 may have far more complex management needs than those with BMI >40 (previously termed ‘morbid’ obesity). In every NHS Trust, there should be a medical obesity spokesperson who is involved in communication with commissioners, providers and the community and is responsible for the local development of effective care pathways. The role of the general practitioner is key in facilitating access to weight management support care.
Currently weight management support for health service employees with an obesity problem is not adequate.6 Employers should encourage healthy eating amongst staff and encourage physical activity.
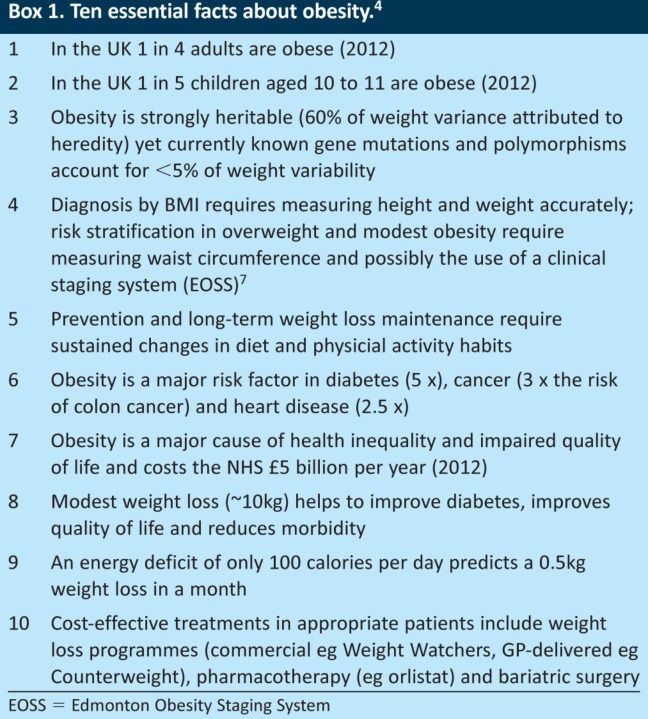
Education is also key, and all health care professionals should know the ten essential facts about obesity (see Box 1).4 Nutritional training and education is also important in undergraduate medicine and in all specialties, and this is recognised by its inclusion in examinations.
Box 1. Ten essential facts about obesity.4.
There is a need to establish a subspecialty for obesity physicians within bariatric medicine, which should probably come under the umbrella of diabetes and endocrinology. A core curriculum needs to be developed.
Importantly, no country has yet got on top of the obesity problem. This is partly due to its complexity. Numerous government departments are involved in the UK, including the Department of Health, the Treasury, the Department of Education, the Ministry of Sport and the Department of Agriculture, as well as the Department of Work and Pensions. This multiple government departmental involvement needs proper coordination and possibly a cross bench peer should be appointed to lead a group to coordinate a strategy in this important field.
Finally, it is suggested that the RCP set up a multidisciplinary intercollegiate group leading on obesity advocacy and ensuring that the recommendations of the report become enacted. This will help to set up multidisciplinary services in the locations where they are not currently established and will provide advice in the future to the government on aspects of the obesity debate.
References
- 1.The NHS Information Centre, Lifestyles Statistics. Statistics on obesity, physical activity and diet: England, 2012. Leeds: The Health and Social Care Information Centre; 2012. [Google Scholar]
- 2.World Health Organisation. Global status report on noncommunicable diseases 2010. Geneva: WHO; 2011. [Google Scholar]
- 3.McPherson K. Marsh T. Brown M. Foresight: tackling obesities: future choices — modelling future trends in obesity and the impact on health. 2nd ed. London: UK Government Office for Science; 2007. [Google Scholar]
- 4.Royal College of Physicians. Report of a working party. London: RCP; 2013. Action on obesity: comprehensive care for all. [Google Scholar]
- 5.NHS Right Care. The NHS Atlas of Variation in Healthcare. Reducing unwarranted variation to increase value and improve quality. London: NHS Right Care; 2011. www.rightcare.nhs.uk/atlas/ [Accessed 7 December 2012]. [Google Scholar]
- 6.Williams J. Jones S for the Health and Work Development Unit Project Development Group. Implementing NICE public health guidance for the workplace: Staff health improvement project Interim report. London: RCP; 2012. [Google Scholar]
- 7.Sharma AM. Kushner RF. A proposed clinical staging system for obesity. International Journal of Obesity. 2009;33:289–95. doi: 10.1038/ijo.2009.2. [DOI] [PubMed] [Google Scholar]