Abstract
The impact of cancer on healthcare is increasing. Therefore, it is key that all doctors receive oncology training. This study surveyed UK undergraduate medical schools to determine the extent of oncology training provided by their curricula. Data on foundation year (FY) and core medical training (CMT) programmes were obtained and analysed for the proportion of oncology posts. Of the responding medical schools, five (36%) had a defined period dedicated to oncology (mean 2 weeks). Four foundation schools were in London, with 10,094 FY posts in 1699 programmes. Of these, 1.5% of post and 8.7% of programmes were in oncology. For CMT offered by the London deanery specialty schools, 11% of CMT post and 48% of programmes included oncology. Oncology was included in 11% posts and 48% programmes offered by the London Deanery specialty schools. Our results show that <50% of junior doctors receive dedicated undergraduate or postgraduate oncology training. An increase in oncology training is therefore urgently required.
Key Words: foundation programme, core medical training, specialist trainee, medical oncology, clinical oncology
Introduction
With one-in-four people dying from cancer in developed countries, with increasing survivorship and cancer incidence, there is an increased need for knowledge of active cancer management among doctors, irrespective of their primary, secondary or tertiary care specialisation.
The World Health Organisation (WHO) and the International Union Against Cancer1 recommend that medical students spend a minimum of two weeks training in oncology.1 Despite this, in a study of undergraduate oncology teaching in 2007, Cave et al. observed that only 39% of UK medical students received any specific teaching in oncology;2 the authors concluded that greater emphasis should be placed on oncology education, to prepare medical students to work with patients with cancer.2
Consistent with the limited training in cancer care outside the speciality of oncology, a recent National Chemotherapy Advisory Group (NCAG) report has shown that the clinical care needs of patients with cancer in the community are not being met.3 This has led to an initiative to develop the subspeciality of acute oncology.3,4 However, an additional and sustainable solution might be to empower all doctors in primary and/or secondary care settings with the knowledge and experience to manage such patients appropriately until they can be transferred as needed to specialist oncology care.
To our knowledge, except for the study by Cave et al., the extent of oncology training in undergraduate and postgraduate medical training programmes has not been previously evaluated.2 Therefore, the aim of this study was to determine the current levels of training in oncology provided to junior doctors.
Materials and methods
Undergraduate and postgraduate training in oncology
To determine undergraduate exposure to oncology, an email survey of the 29 clinical medical school deans in the UK was performed. Following undergraduate education in medicine, junior doctors in the UK complete two years of postgraduate foundation-year (FY) training before becoming eligible for full registration with the UK General Medical Council. This is followed by two years of specialist training in general and acute medicine, referred to as core medical training (CMT), before junior doctors become eligible to apply for subspeciality programmes. To assess the extent of oncology training in postgraduate training programs, data on numbers of posts by speciality in FY and CMT programmes in 2011 were obtained from the foundation school and CMT websites.5,6 Data on application and competition rates for different specialities were obtained from the Royal College of Physicians speciality application website7 and through direct liaison with the Kent and Surrey (KSS) Deanery, which coordinated the national recruitment programme for oncology in 2011.
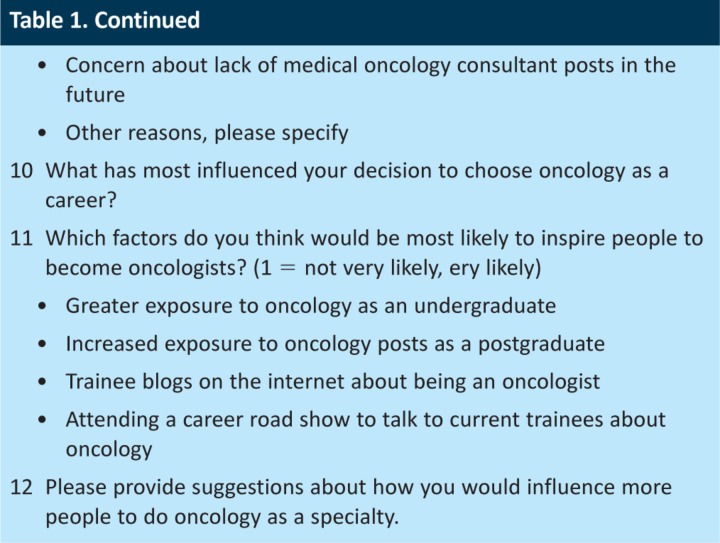
Specialist oncology trainee survey
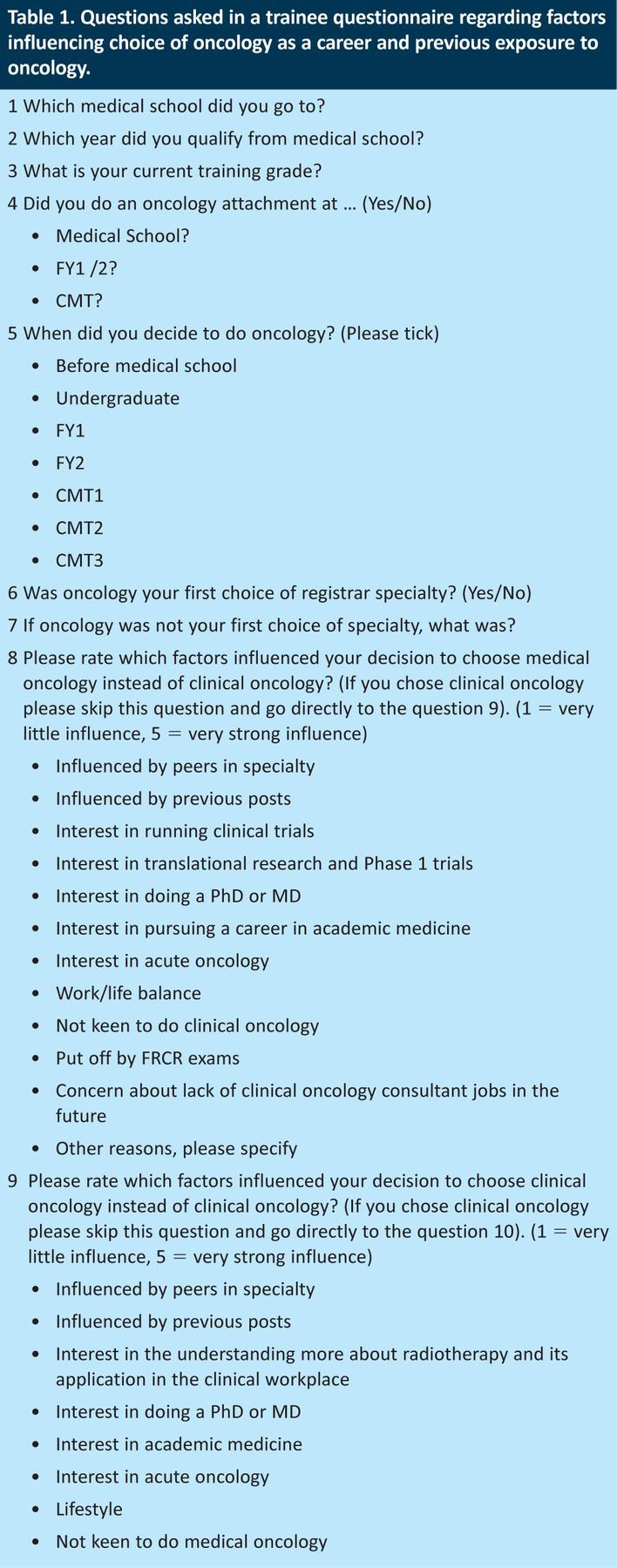
A questionnaire was designed to determine the factors influencing trainees to choose oncology as a career and the level of prior exposure to oncology as an undergraduate or as a postgraduate (Table 1). The survey was performed using Survey Monkey.8 Trainees were emailed via the Association of Cancer Physicians (ACP) and the KSS Deanery, in January 2012. The survey was kept open for three weeks. Trainees in specialty training years 1–2 (ST3 and ST4) were specifically invited to complete the survey, although all trainees could participate. All responses were anonymous.
Table 1.
Questions asked in a trainee questionnaire regarding factors influencing choice of oncology as a career and previous exposure to oncology.
Statistical analysis
Survey monkey computer software and SPSS were used to collect and analyse the data.
Results
Undergraduate education
Of the 31 UK medical schools, 29 provide undergraduate teaching in clinical medicine, and so were asked to detail the total amount of time currently dedicated to oncology (including special study modules (SSMs)). In total, 14 (48%) medical schools responded. Only five (36%) were able to define specifically the dedicated clinical time spent in oncology, and this ranged from two to three weeks (mean two weeks). The remaining medical schools felt that this apparently simple question was not possible to answer easily because of the integrated nature of the modern medical curriculum.
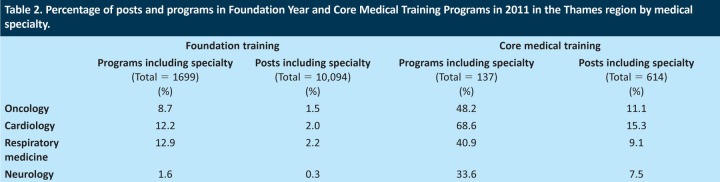
Postgraduate foundation training
There are 25 UK foundation schools, which offered 7,073 FY1 posts to graduating medical students in 2011 in the form of two-year foundation programmes, with four schools in the Thames region offering 1,700 (24%) of the posts. In the Thames region, across both the first and second years of the foundation programmes, there was a total of 10,094 FY posts in 1699 programmes, with 147 (1.5%) posts in 8.7% of programmes in oncology (Table 2). For comparison, 2.0%, 2.2% and 0.3% of posts and 12.2%, 12.9% and 1.6% of programmes were in cardiology, respiratory medicine and neurology, respectively.
Table 2.
Percentage of posts and programs in Foundation Year and Core Medical Training Programs in 2011 in the Thames region by medical specialty.
Postgraduate CMT
There are 16 speciality schools, which offered 1,300 CMT posts, with 268 (20.6%) in the London Deanery in 2011. London represents the largest UK Deanery, with the medicine and medical specialities school with a total of 614 CMT posts across both years of CMT rotations, in 137 programmes. Of these, 68 (11.1%) posts were in oncology and 66 (48.2%) programmes included a post in oncology (Table 2). By contrast, 15.3%, 9.1% and 7.5% of posts were in cardiology, respiratory medicine and neurology, respectively, and 68.6%, 40.9% and 33.6% of CMT programmes included these specialities, respectively (Table 2).
Postgraduate specialisation in oncology
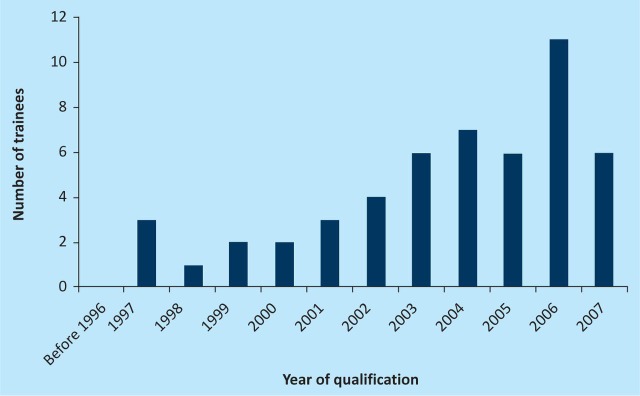
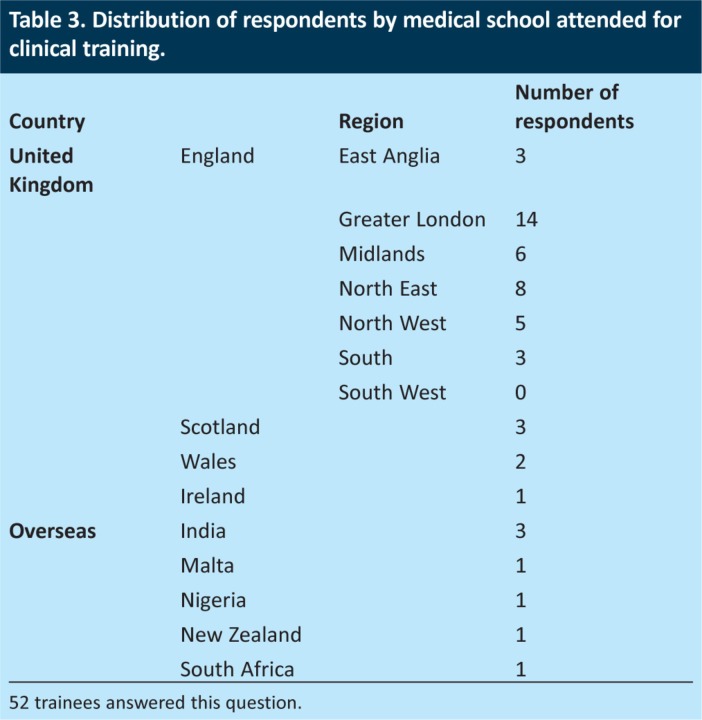
Currently, there are approximately 620 trainees in oncology in the UK, of whom approximately 140 are at the ST3 and/or St4 level. Of those invited to participate through the KSS Deanery and the ACP, 52 trainees (37.1%) responded to the survey (39 in medical oncology and 13 in clinical oncology). Most respondents qualified in 2006 (21%) (Fig 1), and had attended London-based medical schools (27%; Table 3). Of the respondents, 37% were in ST3 and 14% in ST4 training grades.
Fig 1.
Distribution of year of qualification of oncology specialist trainees. n=54.
Table 3.
Distribution of respondents by medical school attended for clinical training.
In total, 49 trainees (94%) had chosen oncology as their first-choice specialty, and 90% had prior experience of oncology during undergraduate, FY or CMT training (Fig 2). Five had not had any previous experience of oncology before taking up their registrar training, two of whom had trained overseas.
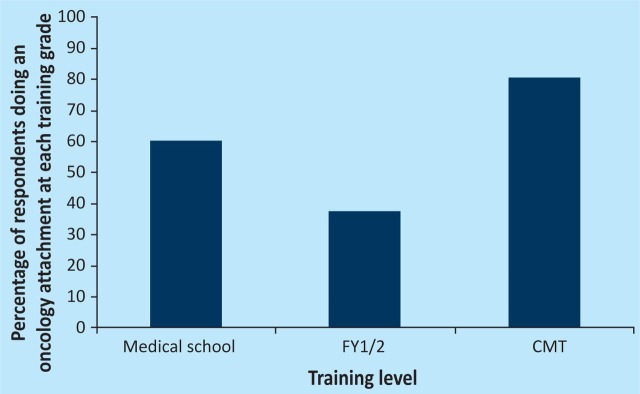
Fig 2.
Prior undergraduate and postgraduate exposure to oncology of specialist trainees. 60% of trainees attended an oncology attachment as an undergraduate. 37.5% of trainees had a FY1/2 rotation including oncology, whereas 80.3% of trainees worked with oncology teams during their CMT training.
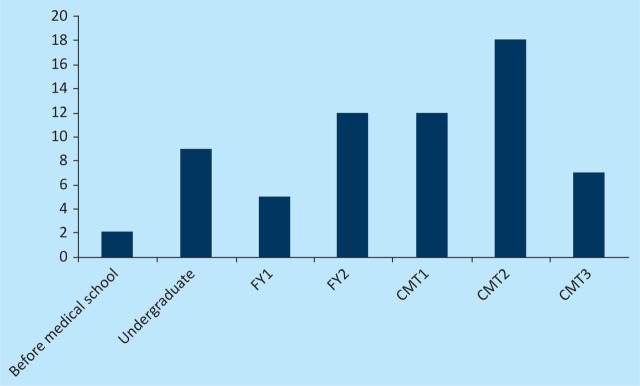
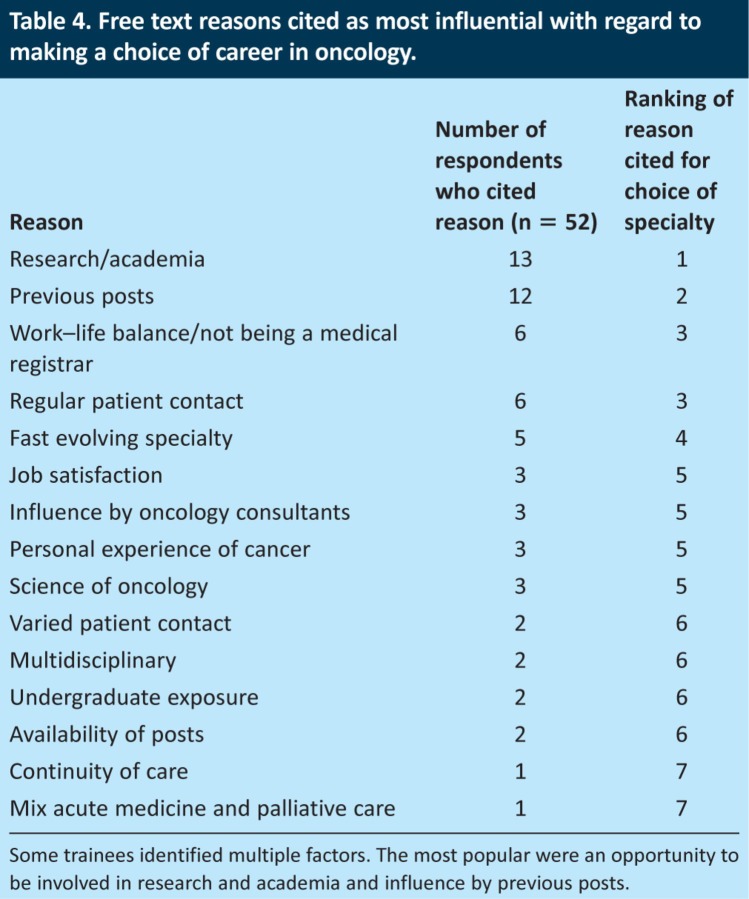
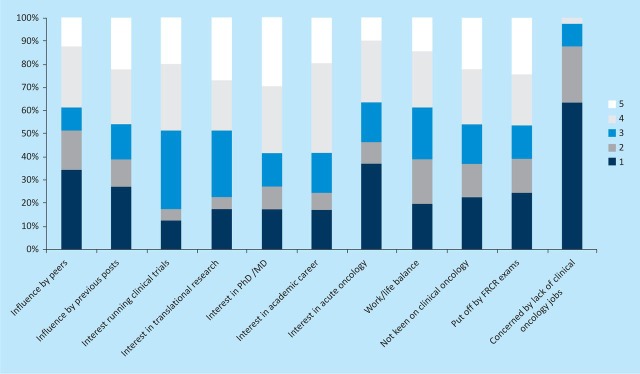
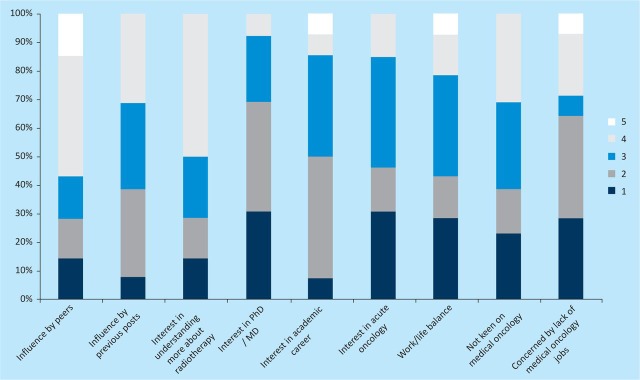
Most trainees (78%) decided to pursue oncology as a career during postgraduate CMT training, most commonly (35%) in CMT year 2 (Fig 3). The most frequently cited reasons for choosing oncology as a career were the opportunity for research (25%) and prior experience of working in oncology (23%) (Table 4). Factors influencing career decision of medical versus clinical oncology included having an interest in research leading to a higher degree (eg PhD), clinical trials, translational research and/or an academic career (Fig 4 and 5).
Fig 3.
Stage at which trainees decided to pursue a career in oncology. Some trainees indicated more than one grade. Most frequently trainees decided to choose oncology as a career at CMT2 training level.
Table 4.
Free text reasons cited as most influential with regard to making a choice of career in oncology.
Fig 4.
Factors influencing choice of medical oncology as a career. A five point scale was used, where 1 was very little influence and 5 was very strong influence. All 39 medical oncology trainees completed this question.
Fig 5.
Factors influencing choice of clinical oncology as a career. A five point scale was used where 1 was very little influence and 5 was very strong influence. 14 trainees answered the question (13 clinical oncology and 1 medical oncology trainee).
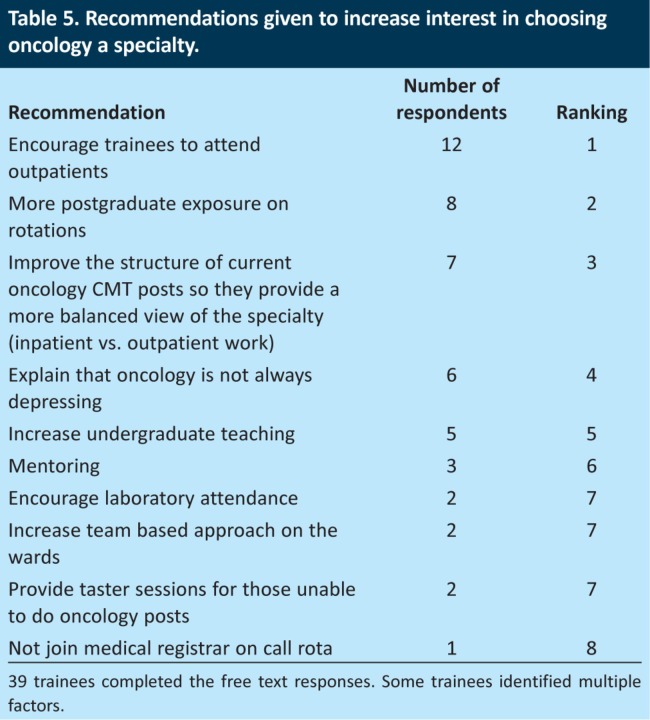
The free-text recommendations given by the trainees to increase interest in choosing oncology as a speciality are given in Table 5.
Table 5.
Recommendations given to increase interest in choosing oncology a specialty.
Discussion
All current doctors are likely to care for patients with cancer; as a consequence, the low percentage of time spent in undergraduate, FY and CMT programmes in oncology identified by this study is of concern. According to our study, only a few medical schools provide a dedicated attachment in oncology (excluding surgical oncology attachments), with an average two-weeks course. Similarly, only 12% and 48% of FY and CMT programmes, respectively, provide an attachment in oncology, despite the highest concentration of oncology centres in the UK being in London. In addition, oncological emergencies in cancer centre and teaching hospital settings are often managed by dedicated oncology teams, unlike cardiology and respiratory emergencies, further limiting exposure of general medical trainees to patients with cancer.9
Studies have previously highlighted deficiencies in the undergraduate oncology programme, including variability in the curriculum.2,10 Although anecdotal, our experience of the stress experienced by junior doctors starting a post in oncology is disproportionate to other medical specialities, owing to limited knowledge of oncology, as also reported previously by Cave et al.2 If care of patients with cancer is to be improved in the UK relative to other European countries, then in addition to translational medicine, urgent attention also needs to be given to postgraduate training of doctors for a period in oncology, irrespective of their final choice of speciality and, perhaps, in particular within general practice.2 Potential benefits include: earlier referral and diagnosis of patients with cancer; better management of oncological emergencies; better palliative care and, hopefully, an impact on combatting the prevalent nihilism associated with cancer care.
With the increasing complexity of medical care, there is a growing pressure on the limited time available for training of medical students and junior doctors. A clear rationalisation of what is crucial is necessary. Curricula in medical school, FY and CMT training programmes need to reflect population needs for training in different specialties and, importantly, this needs to be sensitive to the changing population incidence and prevalence of disease.
Our results suggest that, with respect to oncology, this balance is currently not being achieved. We propose that this could be redressed by increasing the minimum period of oncology attachment in medical school to four weeks and by requiring at least three months (6% of time) in oncology in the four years of FY and/or CMT training. A major expansion in FY and/or CMT in oncology posts to accommodate this is neither practical nor necessarily desirable within the current economic climate. However, reallocation of existing resources might be one answer. For example, in the Thames region, the proportion of postgraduate trainees who have done at least a three-month post in oncology could be increased from 48% to 100% by converting 69 of the 147 FY oncology posts to CMT posts. With 68 existing CMT oncology posts, this would mean there would be a total of 137 oncology CMT posts available for 137 two-year CMT programmes in the Thames region, a relatively cost-neutral solution.
Given the public health importance of cancer, it is also vital that the most able clinicians are encouraged to enter the speciality. The competition ratio (applicants per post) for higher specialty training in 2011 in the UK was 5 for surgery, 3.3 across medical specialities and two for general practitioner (GP) training.7 Among the medical specialities, cardiology is the most popular, with a ratio of over 6, followed by gastroenterology at 4.69.7 The applicant:post ratios were approximately 3:1 for both medical and clinical oncology in 2011, with 90% of posts filled in the Thames region compared with 73% in regional programmes.
It is recognised that preferences for a particular type of medical career not only can be apparent before attending medical school, but are also influenced by factors during undergraduate and postgraduate medical training.11,12 In the UK, doctors considering a career in medical or clinical oncology can apply for speciality trainee (ST) posts, after completing two years of postgraduate foundation (FY1 and FY2), and two years of CMT in general and/or acute medicine (CMT1 and CMT2). One-third of the oncology trainees in the current study reported that an oncology post had been included in their foundation year rotation, whereas 80% of trainees reported that their CMT training had included a post in oncology. Several trainees highlighted the importance of mentoring and the influence of their oncology consultant in steering them towards a career in oncology. This fits with the recognised importance of role models influencing career choice.13 Therefore, our results suggest that some of the difficulties in recruitment of STs to posts outside London reflect the lower proportion of oncology posts in FY and CMT programmes in these regions. However, this needs to be interpreted with caution, because the effect of selection bias for previous posts in oncology during speciality recruitment interviews is also likely to be significant.
The main limitation of the survey was the low response rate from the medical schools and STs. Therefore, caution is required in the interpretation of these results, with the potential for selection bias. Despite this, the survey clearly identified a paucity of dedicated oncology teaching in the undergraduate curriculum and highlighted the importance of a positive postgraduate experience in oncology to attract prospective trainees to consider a career in the speciality. These results, although focused on the current situation in the UK, are relevant globally, given the increasing incidence of cancer in developing countries, and the fact that medical education in many countries is modelled on the UK system. Indeed, it is likely that current UK oncology training for junior doctors is greater than in other countries and, as such, the problem this poses for other healthcare systems might be more acute.
In summary, despite the high and increasing prevalence of cancer, dedicated undergraduate exposure to oncology is currently limited and <50% of medical trainees undertake a post in oncology at FY or CMT grades. Urgent efforts are needed to increase the number of junior doctors rotating through oncology posts to support their training in cancer medicine. This will improve the overall knowledge base of cancer and cancer care, and the quality of care of patients with cancer in the community and secondary care settings, as well as encouraging a larger pool of junior doctors to consider a career in oncology.
Declarations
RA is funded by a Clinician Scientist award from Cancer Research UK.
References
- 1.International Union Against Cancer (UICC) Cancer education for undergraduate medical students: curricula from around the world. Geneva: UICC; 1994. [Google Scholar]
- 2.Cave J. Woolf K. Dacre J. Potts HW. Jones A. Medical student teaching in the UK: how well are newly qualified doctors prepared for their role caring for patients with cancer in hospital? Br J Cancer. 2007;97:472–8. doi: 10.1038/sj.bjc.6603888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Department of Health. 2010. www.dh.gov.uk/en/Publicationsandstatistics/Publications/DH_104500 [Accessed 5 December 2012].
- 4.Leonard P. What is an acute oncology service? Br J Hosp Med (Lond) 2011;72:184–5. doi: 10.12968/hmed.2011.72.4.184. [DOI] [PubMed] [Google Scholar]
- 5.The Foundation Programme, 1012. www.foundationprogramme.nhs.uk/pages/home/deaneries-foundation-schools [Accessed 5 December 2012]
- 6.Royal College of Physicians. 2012. www.ct1recruitment.org.uk [Accessed 7 December 2012].
- 7.Royal College of Physicians. 2011. www.st3recruitment.org.uk/post-information [Accessed 7 December 2012].
- 8.Survey Monkey. 2012. www.surveymonkey.com.
- 9.National Confidential Enquiry into Patient Outcome and Death (NCEPOD) For better, for worse? A review of the care of patients who died within 30 days of receiving systemic anti-cancer therapy. London: NCEPOD; 2008. [Google Scholar]
- 10.Gaffan J. Dacre J. Jones A. Educating undergraduate medical students about oncology: a literature review. J Clin Oncol. 2006;24:1932–9. doi: 10.1200/JCO.2005.02.6617. [DOI] [PubMed] [Google Scholar]
- 11.Vanasse A. Orzanco MG. Courteau J. Scott S. Attractiveness of family medicine for medical students: influence of research and debt. Can Fam Physician. 2011;57:e216–27. [PMC free article] [PubMed] [Google Scholar]
- 12.Meurer LN. Influence of medical school curriculum on primary care specialty choice: analysis and synthesis of the literature. Acad Med. 1995;70:388–97. doi: 10.1097/00001888-199505000-00015. [DOI] [PubMed] [Google Scholar]
- 13.Wright S. Wong A. Newill C. The impact of role models on medical students. J Gen Intern Med. 1997;12:53–6. doi: 10.1007/s11606-006-0007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]