Abstract
This overview of systematic reviews (SRs) aims to evaluate critically the evidence regarding the adverse effects of herbal medicines (HMs). Five electronic databases were searched to identify all relevant SRs, with 50 SRs of 50 different HMs meeting our inclusion criteria. Most had only minor weaknesses in methods. Serious adverse effects were noted only for four HMs: Herbae pulvis standardisatus, Larrea tridentate, Piper methysticum and Cassia senna. The most severe adverse effects were liver or kidney damage, colon perforation, carcinoma, coma and death. Moderately severe adverse effects were noted for 15 HMs: Pelargonium sidoides, Perna canaliculus, Aloe vera, Mentha piperita, Medicago sativa, Cimicifuga racemosa, Caulophyllum thalictroides, Serenoa repens, Taraxacum officinale, Camellia sinensis, Commifora mukul, Hoodia gordonii, Viscum album, Trifolium pratense and Stevia rebaudiana. Minor adverse effects were noted for 31 HMs: Thymus vulgaris, Lavandula angustifolia Miller, Boswellia serrata, Calendula officinalis, Harpagophytum procumbens, Panax ginseng, Vitex agnus-castus, Crataegus spp., Cinnamomum spp., Petasites hybridus, Agave americana, Hypericum perforatum, Echinacea spp., Silybum marianum, Capsicum spp., Genus phyllanthus, Ginkgo biloba, Valeriana officinalis, Hippocastanaceae, Melissa officinalis, Trigonella foenum-graecum, Lagerstroemia speciosa, Cnicus benedictus, Salvia hispanica, Vaccinium myrtillus, Mentha spicata, Rosmarinus officinalis, Crocus sativus, Gymnema sylvestre, Morinda citrifolia and Curcuma longa. Most of the HMs evaluated in SRs were associated with only moderately severe or minor adverse effects.
Key Words: adverse effects, herbal medicine, safety, systematic reviews
Introduction
Herbal medicines (HMs) are popular in many countries, including the UK.1,2 The reasons for this widespread use are complex – see, for example, Ernst and Furnham (2000)3 and Ernst (2008)4 – but the assumption that ‘natural’ can be equated with ‘safe’ is certainly an important factor.5 However, this notion is dangerously misleading: HMs contain pharmacologically active ingredients, some of which have been associated with adverse effects (AEs).6–9
The aim of this article is to provide an overview and critical evaluation of evidence from systematic reviews (SRs) of AEs associated with the use of HM products. It is important to remember that it does not attempt to identify or define all AEs of HM products: in many cases, probable AEs have been implicated but were not documented in an SR.
Methods
Electronic literature searches were conducted in January 2012 to identify SRs of AEs of HMs used in any type of clinical condition. The following electronic databases were used: Medline and Embase (via Ovid), the Allied and Complementary Medicine Database (AMED), CINHAL (via EBSCO) and the Cochrane database. Search terms were constructed using ‘herbal medicine’ and ‘adverse events’ terms and their derivatives, medical subject heading (MeSH) terms and ‘review’ in the title of the article (details of the search strategy are presented in the supplementary Appendix S1). In addition, our own extensive department files were searched by hand.
No restrictions on language or time of publication were imposed. Abstracts of reviews thus located were inspected and those that seemed to meet the inclusion criteria were retrieved for further evaluation by both authors. Systematic reviews were defined as articles that included an explicit and repeatable method. To be included, SRs had to pertain to AEs of HMs in human patients or volunteers. If multiple SRs were found for one specific HM, the most up-to-date, methodologically sound and independent review was chosen. Mixtures of more than one HM were excluded. Non-systematic reviews and reviews pertaining to the effectiveness of HMs were also excluded.
The quality of the methods underlying all SRs was assessed independently by the two reviewers using the modified Oxman score.10,11 This is a validated instrument that consists of the following domains for assessing the quality of the methods of review articles: reporting of search methods and their comprehensiveness, repeatable eligibility criteria, avoidance of selection bias and supportiveness of conclusions. We scored each of the above criteria as 1 (fulfilled), 0 (partially fulfilled) or −1 (not fulfilled). A final result of 0 or lower means the review has major flaws, of 1–2 means minor flaws and 3–5 means minimal or no flaws.
Results
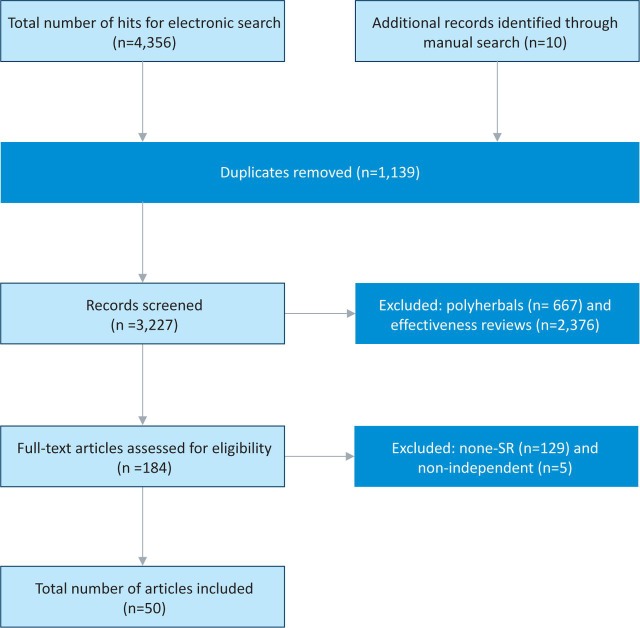
The searches generated 4,366 potentially relevant titles and abstracts, of which 4,316 were excluded (Fig 1). Fifty SRs met our inclusion criteria;12–61 these originated from Canada,21,22 Denmark,26 Germany,17,46 Italy,19,20,62 South Africa,41 the UK12,18,24,29 and the USA.13–16,23,25,27,28,30–40,42–45,47,50–61 In these SRs, adverse effects of the following HMs were evaluated: Agave americana,50 Aloe vera,52 Boswellia serrata,15 Calendula officinalis,16 Camellia sinensis,28 Capsaicin spp.,44 Cassia senna,61 Caulophyllum thalictroides,22 Cimicifuga racemosa,48 Cinnamomum spp.,21 Cnicus benedictus,53 Commifora mukul,36 Crataegus spp.,20 Crocus sativus,59 Curcuma longa,43 Echinacea spp.,24 genus Phyllanthus,26 Ginkgo biloba,29 Gymnema sylvestre,60 Harpagophytum procumbens,17 Herbae pulvis standardisatus,34 Hippocastanaceae,32 Hoodia gordonii,41 Hypericum perforatum,45 Lagerstroemia speciosa,38 Larrea tridentate,33 Lavandula angustifolia Miller,14 Melissa officinalis,35 Mentha piperita,51 Mentha spicata,57 Morinda citrifolia,42 Panax ginseng,18 Pelargonium sidoides,56 Perna canaliculus,54 Petasites hybridus,23 Piper methysticum,37 Rosmarinus officinalis,58 Salvia hispanica,39 Serenoa repens,12 Silybum marianum,25 Stevia rebaudiana,40 Taraxacum officinale,30 Thymus vulgaris,13 Trifolium pretense,27 Trigonella foenum-graecum,47 Vaccinium myrtillus,55 Valeriana officinalis,31 Viscum album46 and Vitex agnus-castus.19 A variety of safety concerns were raised, ranging from clinical AEs12,19,20,22,24,25,31,41,44,46,48 through effects on blood coagulation29 to a combination of drug interactions.13–17,21,23,27,32–40,45,47,50–61 The number of primary studies included in the SRs ranged from 138 to 216.28 The types of primary reports varied from case studies to epidemiological investigations. Some SRs also included secondary analyses such as review articles.15,23,45,47,51,52,59,61 One SR employed a meta-analytical approach.26
Fig 1.
Flow diagram.
Thirty-one SRs concluded that the HM in question was safe.13–21,23–26,29,31,32,35,38,39,42–45,47,50,53,55,57–60 Fifteen SRs reported moderately severe AEs,12,22,27,28,30,36,40,41,46,48,49,51,52,54,56 and four SRs concluded that the HM in question was not safe (see Supplemental Tables S1 and S2).33,34,37,61 Thirteen SRs mentioned the duration of AEs,18,20,22,24,26,28,33,42,44–46,48,50 which ranged from 48 hours to 11 months. Forty-two SRs failed to mention conflict of interest of the authors.13–18,22,23,25–27,30–45,47–61 Thirty-two SRs made no mention of any source of funding.13–17,22,23,27,30,34–41,44,47,48,50–61
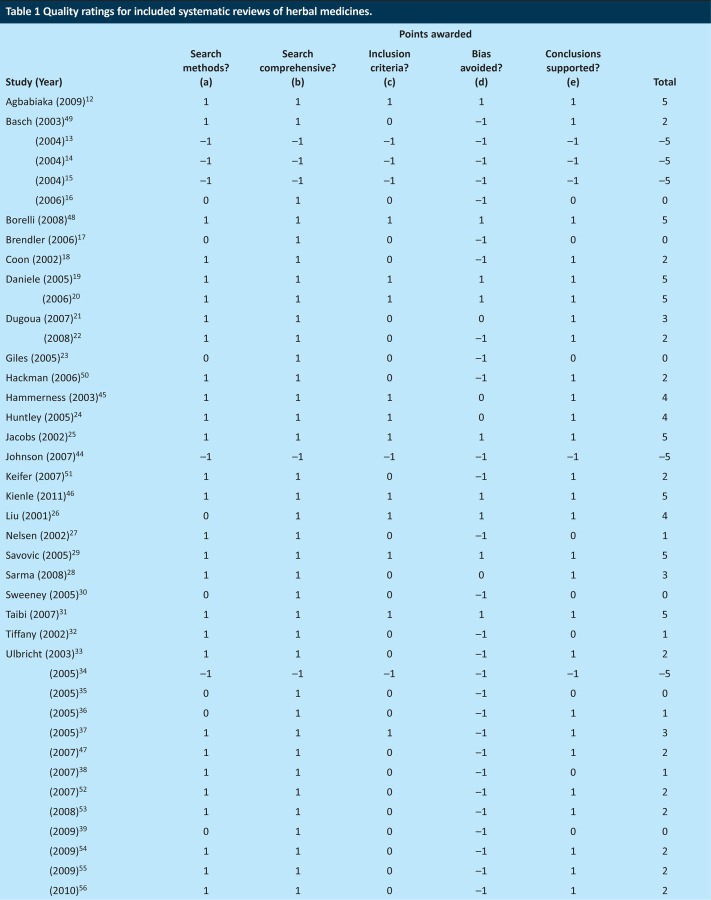
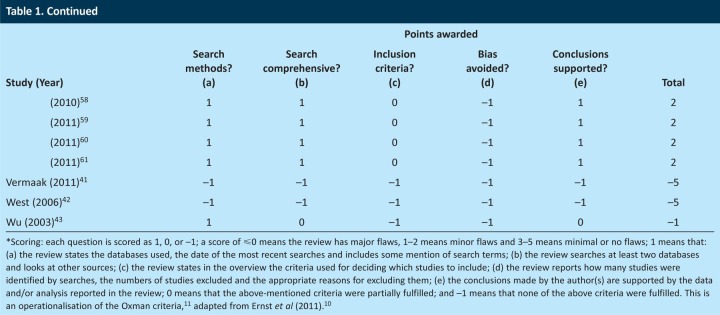
The quality of the methods of the included SRs was mixed (Table 1). Fifteen SRs had only minimal or no flaws (3–5 points on the modified Oxman scale),12,19–21,24–26,28,29,31,37,45,46,48 20 SRs had minor weaknesses (1–2 points)18,22,27,32,33,36,38,47,50–61 and 15 SRs had major flaws in their methods (≤0 points).13–17,23,30,34,35,39–44
Table 1.
Quality ratings for included systematic reviews of herbal medicines.
The HMs were used for a wide variety of clinical conditions, including allergic rhinitis;23 anxiety;14,37 asthma, Crohn's disease and ulcerative colitis;15 bronchitis or cough;13 cardiovascular diseases;20,32,39,40 common colds;56 constipation;61 diabetes;21,38,47,60 depression;45 dyspepsia;53 hyperlipidaemia;36 inflammatory skin conditions;16 insomnia;31 irritable bowel syndrome;34 liver disease;25 lower urinary tract infections or benign prostatic hyperplasia;12 menopausal symptoms;27,48 obesity;41 pain;44,30 pregnancy;22 prevention28 or treatment14,33,42,46 of cancer; rheumatic conditions;15,17,43,54 various clinical conditions18,19,24,29,51,52,55,57–59 and viral infections.26,35 Three SRs also included studies of healthy individuals.18,24,42
Discussion
This overview aimed to critically evaluate the data from SRs of AEs of HMs. Most SRs indicated that the HMs in question were reasonably safe.13–21,23–26,29,31,32,35,38,39,42–45,47,50,53,55,57–60 Only four SRs arrived at clearly negative conclusions about the safety of the reviewed HM.33,34,37,61
The AEs ranged from mild to severe. Mild AEs included pain,15,57,61 allergic reactions,13,17,19,20,21,24,36,37,53,58,59 burning sensation,44,51,55,57 constipation,23,34 dermatitis,50,57–59 diarrhoea,17,21,23,31,35,47,52,56,61 ‘difficulties’,16 dizziness,13,20,31,32,40 drowsiness,31 dry mouth,34 fatigue,12,45 gastrointestinal upset,15,19–21,23–26,30,32,36,37,39,43,45,48,53–56 headache18–20,25,31,32,34,35,36,45 loss of appetite,30 menstrual disorders,19 mouth burning,21 muscle spasm,32 muscle weaknesses,40 nausea,12,14,15,19,20,26,31,32,35,40,55,61 rash,24,48,56 sleep disorders18,35 and vomiting.14,21,23,30,53,61 Moderately severe AEs included anorexia, reversible neutropenia,14 coagulation abnormalities,29 confusion, slurred speech, blurred vision, sedation, hyper-reflexia,34 dysphagia, severe nausea,23 electroencephalogram (EEG) changes,35 increased fibrinolysis, inhibition of platelet aggregation,36 loss of consciousness,21 platelet aggregation,30 pruritis32 or vertigo, photophobia and mydriasis.34 Severe AEs included acute psychosis,34 cerebral haemorrhage, death,12,37,52 coma, respiratory arrest, tachycardia,37,51,56 hallucinations, convulsions, rhabdomyolysis and renal failure,36,51 acute lung injury,51,54 haemorrhage, circulation failure,20,56 hepatitis,41,48,52,54,61 hyperkalaemia,42,46 liver damage,28,30,42,46,61 nephrotoxicity,32 cirrhosis, liver failure,37,54 perinatal stroke, acute myocardial infarction, congestive heart failure,54 severe multiorgan hypoxic injury,22 carcinoma,33,61 perforation of the gastrointestinal tract,61 seizures and epilepsy.58
The large number of included SRs means that it is not easy to provide practical guidance through this labyrinth of HMs and multitude of AEs. Readers with an interest in one specific HM or one particular AE might look up the relevant SRs and refer to the primary reports. Readers with a more general interest in the safety of HMs would probably prefer to study those SRs that report serious AEs.33,34,37,61
The quality of the methods of some of the included SRs was frequently not optimal. This could be due to the fact that several of the articles were not designed as typical SRs. Many of the papers that scored poorly on quality were monograph-type publications, which are relatively frequent in the literature on HM. As these articles do nevertheless contribute relevant information, we decided to include them in our overview. Despite the fact that many SRs failed to achieve high-quality scores, we believe that virtually all of them contribute to our knowledge of AEs associated with HMs. In our view, none of the defects noted in Table 1 completely invalidates the SR in question. Even an SR that scored poorly on the formal quality rating can serve an important purpose when it alerts us to the risks associated with the HM in question.
Several challenges in methods and concepts were faced when undertaking this overview. We analysed data from SRs of AEs of specific HMs and omitted SRs of polyherbal preparations and effectiveness reviews (see Supplemental Table S3).63–81 It was frequently impossible to differentiate between herb–drug interactions and AEs, as these questions were addressed simultaneously. Herb–drug interactions, adulteration and contamination obviously can also cause AEs.1,82–84 Our plan is to address these issues in specific analyses to be published as separate overviews.
This overview has further limitations that must be kept in mind when interpreting the evidence. Although a comprehensive search strategy was employed, there is no guarantee that all relevant SRs have been located. All SRs are prone to publication bias, and so any such bias may have been transferred to our overview. As we only included SRs, our overview cannot provide information on HMs for which no SR is available. A comprehensive review of all information available to date regarding AEs of HM would be a monumental task that by far exceeds the possibility of a single journal article.85
The nature of the evidence reviewed here also requires a brief comment. Rigorous and comprehensive SRs of AEs should consider anecdotal data such as case reports. Such evidence is clearly relevant for assessing safety issues, but it does not lend itself to establishing cause and effect. We therefore ought to be cautious when interpreting such data and should critically question causality on a case-by-case basis.
In conclusion, numerous SRs of HMs have recently become available. Most of these SRs reveal mild adverse effects associated with HMs; however, some HMs might pose more severe health threats.
Funding
Paul Posadzki was supported by a fellowship from the Royal College of Physicians, London.
References
- 1.Pittler MH. Ernst E. Systematic review: hepatotoxic events associated with herbal medicinal products. Ailment Pharmacol Ther. 2003;18:451–71. doi: 10.1046/j.1365-2036.2003.01689.x. [DOI] [PubMed] [Google Scholar]
- 2.Hunt K. Ernst E. Patients’ use of CAM: results from the Health Survey for England 2005. Focus Altern Complement Ther. 2010;15:101–3. [Google Scholar]
- 3.Ernst E. Furnham A. BMWs and complementary/alternative medicine. Focus Altern Complement Ther. 2000;5:253–4. doi: 10.1111/j.2042-7166.2000.tb02584.x. [DOI] [Google Scholar]
- 4.Ernst E. The healthcare show: an evidence-free zone? Focus Altern Complement Ther. 2008;13:1–2. doi: 10.1211/fact.13.1.0001. [DOI] [Google Scholar]
- 5.Ernst E. Pittler MH. Wider B. Boddy K. The desktop guide to complementary and alternative medicine. 2nd edition. Edinburgh: Elsevier Mosby; 2006. [Google Scholar]
- 6.Russmann S. Helbling A. Kava hepatotoxicity. Ann Intern Med. 2001;135:68–9. doi: 10.7326/0003-4819-135-1-200107030-00036. [DOI] [PubMed] [Google Scholar]
- 7.Bajaj J. Knox JF. Komorowski PAC. Saeian K. The irony of herbal hepatitis. Ma-Huang-induced hepatotoxicity associated with compound heterozygosity for hereditary hemochromatosis. Dig Dis Sci. 2003;48:1925–8. doi: 10.1023/A:1026105917735. [DOI] [PubMed] [Google Scholar]
- 8.Chitturi S. Farrell GC. Herbal hepatotoxicity: an expanding but poorly defined problem. J Gastroenterol Hepatol. 2000;15:1093–9. doi: 10.1046/j.1440-1746.2000.02349.x. [DOI] [PubMed] [Google Scholar]
- 9.Peters D. CAM: doing more good than harm. Focus Altern Complement Ther. 2009;14:176–8. doi: 10.1211/fact.14.3.0006. [DOI] [Google Scholar]
- 10.Ernst E. Posadzki P. Lee MS. Complementary and alternative medicine (CAM) for sexual dysfunction and erectile dysfunction in older men and women: an overview of systematic reviews. Maturitas. 2011;70:37–41. doi: 10.1016/j.maturitas.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Oxman AD. Guyatt GH. Validation of an index of the quality of review articles. J Clin Epidemiol. 1991;44:1271–8. doi: 10.1016/0895-4356(91)90160-B. [DOI] [PubMed] [Google Scholar]
- 12.Agbabiaka TB. Pittler MH. Wider B. Ernst E. Serenoa repens (saw palmetto): a systematic review of adverse events. Drug Saf. 2009;32:637–47. doi: 10.2165/00002018-200932080-00003. [DOI] [PubMed] [Google Scholar]
- 13.Basch E. Ulbricht C. Hammerness P, et al. Thyme (Thymus vulgaris L.), thymol. J Herb Pharmacother. 2004;4:49–67. [PubMed] [Google Scholar]
- 14.Basch E. Foppa I. Liebowitz R, et al. Lavender (Lavandula angustifolia Miller) J Herb Pharmacother. 2004;4:63–78. [PubMed] [Google Scholar]
- 15.Basch E. Boon H. Davies-Heerema T, et al. Boswellia: an evidence-based systematic review by the Natural Standard Research Collaboration. J Herb Pharmacother. 2004;4:63–83. [PubMed] [Google Scholar]
- 16.Basch E. Bent S. Foppa I, et al. Marigold (Calendula officinalis L.): an evidence-based systematic review by the Natural Standard Research Collaboration. J Herb Pharmacother. 2006;6:135–59. doi: 10.1080/J157v06n03_08. [DOI] [PubMed] [Google Scholar]
- 17.Brendler T. Gruenwald J. Ulbricht C. Basch E. Devil's claw (Harpagophytum procumbens DC): an evidence-based systematic review by the Natural Standard Research Collaboration. J Herb Pharmacother. 2006;6:89–126. [PubMed] [Google Scholar]
- 18.Thompson Coon J. Ernst E. Panax ginseng: a systematic review of adverse effects and drug interactions. Drug Saf. 2002;25:323–44. doi: 10.2165/00002018-200225050-00003. [DOI] [PubMed] [Google Scholar]
- 19.Daniele C. Thompson Coon J. Pittler MH. Ernst E. Vitex agnus castus: a systematic review of adverse events. Drug Saf. 2005;28:319–32. doi: 10.2165/00002018-200528040-00004. [DOI] [PubMed] [Google Scholar]
- 20.Daniele C. Mazzanti G. Pittler MH. Ernst E. Adverse-event profile of Crataegus spp.: a systematic review. Drug Saf. 2006;29:523–35. doi: 10.2165/00002018-200629060-00005. [DOI] [PubMed] [Google Scholar]
- 21.Dugoua JJ. Seely D. Perri D, et al. From type 2 diabetes to antioxidant activity: a systematic review of the safety and efficacy of common and cassia cinnamon bark. Can J Physiol Pharmacol. 2007;85:837–47. doi: 10.1139/Y07-080. [DOI] [PubMed] [Google Scholar]
- 22.Dugoua J. Perri D. Seely D, et al. Safety and efficacy of blue cohosh (Caulophyllum thalictroides) during pregnancy and lactation. Can J Clin Pharmacol. 2008;15:e66–73. [PubMed] [Google Scholar]
- 23.Giles M. Ulbricht C. Khalsa K, et al. Butterbur: an evidence-based systematic review by the Natural Standard Research Collaboration. J Herb Pharmacother. 2005;5:119–43. doi: 10.1080/J157v05n03_12. [DOI] [PubMed] [Google Scholar]
- 24.Huntley AL. Thompson Coon J. Ernst E. The safety of herbal medicinal products derived from Echinacea species: a systematic review. Drug Saf. 2005;28:387–400. doi: 10.2165/00002018-200528050-00003. [DOI] [PubMed] [Google Scholar]
- 25.Jacobs BP. Dennehy C. Ramirez G, et al. Milk thistle for the treatment of liver disease: a systematic review and meta-analysis. Am J Med. 2002;113:506–15. doi: 10.1016/S0002-9343(02)01244-5. [DOI] [PubMed] [Google Scholar]
- 26.Liu J. Lin H. McIntosh H. Genus Phyllanthus for chronic hepatitis B virus infection: a systematic review. J Viral Hepat. 2001;8:358–66. doi: 10.1046/j.1365-2893.2001.00307.x. [DOI] [PubMed] [Google Scholar]
- 27.Nelsen J. Ulbricht C. Barrette E, et al. Red clover (Trifolium pratense) monograph: a clinical decision support tool. J Herb Pharmacother. 2002;2:49–72. doi: 10.1080/j157v02n03_06. [DOI] [PubMed] [Google Scholar]
- 28.Sarma DN. Barrett ML. Chavez ML, et al. Safety of green tea extracts: a systematic review by the US Pharmacopeia. Drug Saf. 2008;31:469–84. doi: 10.2165/00002018-200831060-00003. [DOI] [PubMed] [Google Scholar]
- 29.Savovic J. Wider B. Ernst E. Effects of Ginkgo biloba on blood coagulation parameters: a systematic review of randomised controlled trials. Evidence-Based Integrative. Medicine. 2005;2:167–76. [Google Scholar]
- 30.Sweeney B. Vora M. Ulbricht C. Basch E. Evidence-based systematic review of dandelion (Taraxacum officinale) by natural standard research collaboration. J Herb Pharmacother. 2005;5:79–93. [PubMed] [Google Scholar]
- 31.Taibi DM. Landis CA. Petry H. Vitiello MV. A systematic review of valerian as a sleep aid: safe but not effective. Sleep Med Rev. 2007;11:209–30. doi: 10.1016/j.smrv.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 32.Tiffany N. Boon H. Ulbricht C, et al. Horse chestnut: a multidisciplinary clinical review. J Herb Pharmacother. 2002;2:71–85. [PubMed] [Google Scholar]
- 33.Ulbricht C. Basch E. Vora M, et al. Chaparral monograph: a clinical decision support tool. J Herb Pharmacother. 2003;3:121–31. doi: 10.1080/j157v03n01_08. [DOI] [PubMed] [Google Scholar]
- 34.Ulbricht C. Basch E. Hammerness P, et al. An evidence-based systematic review of belladonna by the natural standard research collaboration. J Herb Pharmacother. 2004;4:61–90. doi: 10.1080/J157v04n04_06. [DOI] [PubMed] [Google Scholar]
- 35.Ulbricht C. Brendler T. Gruenwald J, et al. Lemon balm (Melissa officinalis L.): an evidence-based systematic review by the Natural Standard Research Collaboration. J Herb Pharmacother. 2005;5:71–114. doi: 10.1080/J157v05n01_01. [DOI] [PubMed] [Google Scholar]
- 36.Ulbricht C. Basch E. Szapary P, et al. Guggul for hyperlipidemia: a review by the Natural Standard Research Collaboration. Complement Ther Med. 2005;13:279–90. doi: 10.1016/j.ctim.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 37.Ulbricht C. Basch E. Boon H, et al. Safety review of kava (Piper methysticum) by the Natural Standard Research Collaboration. Expert Opin Drug Saf. 2005;4:779–94. doi: 10.1517/14740338.4.4.779. [DOI] [PubMed] [Google Scholar]
- 38.Ulbricht C. Dam C. Milkin T, et al. Banaba (Lagerstroemia speciosa L.): an evidence-based systematic review by the Natural Standard research collaboration. J Herb Pharmacother. 2007;7:99–113. [PubMed] [Google Scholar]
- 39.Ulbricht C. Chao W. Nummy K, et al. Chia (Salvia hispanica): a systematic review by the natural standard research collaboration. Rev Recent Clin Trials. 2009;4:168–74. doi: 10.2174/157488709789957709. [DOI] [PubMed] [Google Scholar]
- 40.Ulbricht C. Isaac R. Milkin T, et al. An evidence-based systematic review of stevia by the Natural Standard Research Collaboration. Cardiovasc Hematol Agents Med Chem. 2010;8:113–27. doi: 10.2174/187152510791170960. [DOI] [PubMed] [Google Scholar]
- 41.Vermaak I. Hamman JH. Viljoen AM. Hoodia gordonii: an up-to-date review of a commercially important anti-obesity plant. Planta Med. 2011;77:1149–60. doi: 10.1055/s-0030-1250643. [DOI] [PubMed] [Google Scholar]
- 42.West BJ. Jensen CJ. Westendorf J. White LD. A safety review of noni fruit juice. J Food Sci. 2006;71:R100–6. doi: 10.1111/j.1750-3841.2006.00164.x. [DOI] [Google Scholar]
- 43.Chainani-Wu N. Safety and anti-inflammatory activity of Curcumin: a component of tumeric (Curcuma longa) J Altern Complement Med. 2003;9:161–8. doi: 10.1089/107555303321223035. [DOI] [PubMed] [Google Scholar]
- 44.Johnson W. Final report on the safety assessment of Capsicum annuum extract, Capsicum annuum fruit extract, Capsicum annuum resin, Capsicum annuum fruit powder, Capsicum frutescens fruit, Capsicum frutescens fruit extract, Capsicum frutescens resin, and Capsaicin. Int J Toxicol. 2007;26:3–106. doi: 10.1080/10915810601163939. [DOI] [PubMed] [Google Scholar]
- 45.Hammerness P. Basch E. Ulbricht C, et al. St. John's wort: a systematic review of adverse effects and drug interactions for the consultation psychiatrist. Psychosomatics. 2003;44:271–82. doi: 10.1176/appi.psy.44.4.271. [DOI] [PubMed] [Google Scholar]
- 46.Kienle GS. Grugel R. Kiene H. Safety of higher dosages of Viscum album L. in animals and humans – systematic review of immune changes and safety parameters. BMC Complement Altern Med. 2011;11:72. doi: 10.1186/1472-6882-11-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ulbricht C. Basch E. Burke D, et al. Fenugreek (Trigonella foenum-graecum L. Leguminosae): an evidence-based systematic review by the natural standard research collaboration. J Herb Pharmacother. 2007;7:143–77. doi: 10.1080/15228940802142852. [DOI] [PubMed] [Google Scholar]
- 48.Borrelli F. Ernst E. Black cohosh (Cimicifuga racemosa): a systematic review of adverse events. Am J Obstet Gynecol. 2008;199:455–66. doi: 10.1016/j.ajog.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 49.Basch E. Ulbricht C. Harrison M, et al. Alfalfa (Medicago sativa L.): a clinical decision support tool. J Herb Pharmacother. 2003;3:69–90. doi: 10.1300/j157v03n02_09. [DOI] [PubMed] [Google Scholar]
- 50.Hackman D. Giese N. Markowitz J, et al. Agave (Agave americana): an evidence-based systematic review by the Natural Standard Research Collaboration. J Herb Pharmacother. 2006;6:101–22. [PubMed] [Google Scholar]
- 51.Keifer D. Ulbricht C. Abrams T, et al. Peppermint (Mentha piperita): an evidence-based systematic review by the Natural Standard Research Collaboration. J Herb Pharmacother. 2007;7:91–143. doi: 10.1300/j157v07n02_07. [DOI] [PubMed] [Google Scholar]
- 52.Ulbricht C. Armstrong J. Basch E, et al. An evidence-based systematic review of Aloe vera by the Natural Standard Research Collaboration. J Herb Pharmacother. 2007;7:279–323. doi: 10.1080/15228940802153339. [DOI] [PubMed] [Google Scholar]
- 53.Ulbricht C. Basch E. Dacey C, et al. An evidence-based systematic review of blessed thistle (Cnicus benedictus) by the Natural Standard Research Collaboration. J Diet Suppl. 2008;5:422–37. doi: 10.1080/19390210802519754. [DOI] [Google Scholar]
- 54.Ulbricht C. Chao W. Costa D, et al. An evidence-based systematic review of green-lipped mussel (Perna canaliculus) by the Natural Standard Research Collaboration. J Diet Suppl. 2009;6:54–90. doi: 10.1080/19390210802690191. [DOI] [PubMed] [Google Scholar]
- 55.Ulbricht C. Basch E. Basch S, et al. An evidence-based systematic review of bilberry (Vaccinium myrtillus) by the Natural Standard Research Collaboration. J Diet Suppl. 2009;6:162–200. doi: 10.1080/19390210902861858. [DOI] [PubMed] [Google Scholar]
- 56.Ulbricht C. Abrams TR. Conquer J, et al. An evidence-based systematic review of umckaloabo (Pelargonium sidoides) by the Natural Standard Research Collaboration. J Diet Suppl. 2010;7:283–302. doi: 10.3109/19390211.2010.507116. [DOI] [PubMed] [Google Scholar]
- 57.Ulbricht C. Costa D. Grimes Serrano J, et al. An evidence-based systematic review of spearmint by the Natural Standard Research Collaboration. J Diet Suppl. 2010;7:179–215. doi: 10.3109/19390211.2010.486702. [DOI] [PubMed] [Google Scholar]
- 58.Ulbricht C. Abrams T. Brigham A, et al. An evidence-based systematic review of rosemary (Rosmarinus officinalis) by the Natural Standard Research Collaboration. J Diet Suppl. 2010;7:351–413. doi: 10.3109/19390211.2010.525049. [DOI] [PubMed] [Google Scholar]
- 59.Ulbricht C. Conquer J. Costa D, et al. An evidence-based systematic review of saffron (Crocus sativus) by the Natural Standard Research Collaboration. J Diet Suppl. 2011;8:58–114. doi: 10.3109/19390211.2011.547666. [DOI] [PubMed] [Google Scholar]
- 60.Ulbricht C. Abrams T. Basch E, et al. An evidence-based systematic review of Gymnema (Gymnema sylvestre R. Br.) by the Natural Standard Research Collaboration. J Diet Suppl. 2011;8:311–30. doi: 10.3109/19390211.2011.597977. [DOI] [PubMed] [Google Scholar]
- 61.Ulbricht C. Conquer J. Costa D, et al. An evidence-based systematic review of senna ( Cassia senna) by the Natural Standard Research Collaboration. J Diet Suppl. 2011;8:189–238. doi: 10.3109/19390211.2011.573186. [DOI] [PubMed] [Google Scholar]
- 62.Borrelli E. Evaluation of the quality of life in breast cancer patients undergoing lectin standardized mistletoe therapy. Minerva Med. 2001;92:105–7. [Google Scholar]
- 63.Boon H. Wong J. Botanical medicine and cancer: a review of the safety and efficacy. Expert Opin Pharmacother. 2004;5:2485–501. doi: 10.1517/14656566.5.12.2485. [DOI] [PubMed] [Google Scholar]
- 64.Cameron M. Gagnier JJ. Chrubasik S. Herbal therapy for treating rheumatoid arthritis. Cochrane Database Syst Rev. 2011. p. CD002948. [DOI] [PubMed]
- 65.Chen XY. Wu TX. Liu GJ, et al. Chinese medicinal herbs for influenza. Cochrane Database Syst Rev. 2007. p. CD004559. [DOI] [PubMed]
- 66.Cheng CW. Bian ZX. Wu TX. Systematic review of Chinese herbal medicine for functional constipation. World J Gastroenterol. 2009;15:4886–95. doi: 10.3748/wjg.15.4886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chung V. Liu L. Bian ZX, et al. Efficacy and safety of herbal medicines for idiopathic Parkinson's disease: A systematic review. Mov Disord. 2006;21:1709–15. doi: 10.1002/mds.21008. [DOI] [PubMed] [Google Scholar]
- 68.Cui X. Trinh K. Wang YJ. Chinese herbal medicine for chronic neck pain due to cervical degenerative disc disease. Cochrane Database Syst Rev. 2010. p. 006556. CD. [DOI] [PMC free article] [PubMed]
- 69.Ernst E. Herbal medicinal products during pregnancy: are they safe? BJOG. 2002;109:227–35. doi: 10.1111/j.1471-0528.2002.t01-1-01009.x. [DOI] [PubMed] [Google Scholar]
- 70.Flower A. Liu JP. Chen S, et al. Chinese herbal medicine for endometriosis. Cochrane Database Syst Rev. 2009. p. CD006568. [DOI] [PubMed]
- 71.Guo R. Pittler MH. Ernst E. Herbal medicines for the treatment of COPD: a systematic review. Eur Respir J. 2006;28:330–8. doi: 10.1183/09031936.06.00119905. [DOI] [PubMed] [Google Scholar]
- 72.Liu TT. Shi J. Epstein DH, et al. A meta-analysis of Chinese herbal medicine in treatment of managed withdrawal from heroin. Cell Mol Neurobiol. 2009;29:17–25. doi: 10.1007/s10571-008-9290-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Martin KW. Ernst E. Herbal medicines for treatment of fungal infections: a systematic review of controlled clinical trials. Mycoses. 2004;47:87–92. doi: 10.1046/j.1439-0507.2003.00951.x. [DOI] [PubMed] [Google Scholar]
- 74.May BH. Lit M. Xue CCL, et al. Herbal medicine for dementia: a systematic review. Phytotherapy Res. 2009;23:447–59. doi: 10.1002/ptr.2656. [DOI] [PubMed] [Google Scholar]
- 75.Pittler MH. Schmidt K. Ernst E. Adverse events of herbal food supplements for body weight reduction: systematic review. Obesity Rev. 2005;6:93–111. doi: 10.1111/j.1467-789X.2005.00169.x. [DOI] [PubMed] [Google Scholar]
- 76.Rathbone J. Zhang L. Zhang MM, et al. Chinese herbal medicine for schizophrenia – Cochrane systematic review of randomised trials. Br J Psychiatry. 2007;190:379–84. doi: 10.1192/bjp.bp.106.026880. [DOI] [PubMed] [Google Scholar]
- 77.Shi J. Tong Y. Shen JG. Li HX. Effectiveness and safety of herbal medicines in the treatment of irritable bowel syndrome: a systematic review. World J Gastroenterol. 2008;14:454–62. doi: 10.3748/wjg.14.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tu X. Huang GM. Tan SK. Chinese herbal medicine for dysfunctional uterine bleeding: a meta-analysis. Evid Based Complement Alternat Med. 2009;6:99–105. doi: 10.1093/ecam/nem063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhu X. Proctor M. Bensoussan A, et al. Chinese herbal medicine for primary dysmenorrhoea. Cochrane Database Syst Rev. 2008. p. CD005288. [DOI] [PMC free article] [PubMed]
- 80.Ulbricht C. Weissner W. Hashmi S, et al. Essiac: systematic review by the Natural Standard Research Collaboration. J Soc Integr Oncol. 2009;7:73–80. [PubMed] [Google Scholar]
- 81.Qin F. Wu X. Tang Y, et al. Meta-analysis of randomized controlled trials to assess the effectiveness and safety of free and Easy Wanderer Plus, a polyherbal preparation for depressive disorders. J Psychiatr Res. 2011;45:1518–24. doi: 10.1016/j.jpsychires.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 82.Setty AR. Sigal LH. Herbal medications commonly used in the practice of rheumatology: Mechanisms of action, efficacy, and side effects. Semin Arthritis Rheum. 2005;34:773–84. doi: 10.1016/j.semarthrit.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 83.Naser B. Schnitker J. Minkin MJ, et al. Suspected black cohosh hepatotoxicity: no evidence by meta-analysis of randomized controlled clinical trials for isopropanolic black cohosh extract. Menopause. 2011;18:366–75. doi: 10.1097/gme.0b013e3181fcb2a6. [DOI] [PubMed] [Google Scholar]
- 84.Frazier T. Krueger K. Hepatotoxic herbs: will injury mechanisms guide treatment strategies? Curr Gastroenterol Rep. 2009;11:317–24. doi: 10.1007/s11894-009-0046-y. [DOI] [PubMed] [Google Scholar]
- 85.Aronson JK. Meyler's side effects of herbal medicines. Oxford: Elsevier Science; 2008. [Google Scholar]
- 86.Borrelli F. Capasso R. Aviello G, et al. Effectiveness and safety of ginger in the treatment of pregnancy-induced nausea and vomiting. Obstet Gynecol. 2005;105:849–56. doi: 10.1097/01.AOG.0000154890.47642.23. [DOI] [PubMed] [Google Scholar]
- 87.Canter PH. Lee HS. Ernst E. A systematic review of randomised clinical trials of Tripterygium wilfordii for rheumatoid arthritis. Phytomedicine. 2006;13:371–7. doi: 10.1016/j.phymed.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 88.Thompson Coon J. Ernst E. Andrographis paniculata in the treatment of upper respiratory tract infections: a systematic review of safety and efficacy. Planta Med. 2004;70:293–8. doi: 10.1055/s-2004-818938. [DOI] [PubMed] [Google Scholar]
- 89.Mehri A. Hasani-Ranjbar S. Larijani B. Abdollahi M. A systematic review of efficacy and safety of Urtica dioica in the treatment of diabetes. Int J Pharmacol. 2011;7:161–70. doi: 10.3923/ijp.2011.161.170. [DOI] [Google Scholar]
- 90.Pittler MH. Ernst E. Feverfew for preventing migraine. Cochrane Database Syst Rev. 2004. p. CD002286. [DOI] [PubMed]
- 91.Vogler BK. Ernst E. Aloe vera: a systematic review of its clinical effectiveness. Br J Gen Pract. 1999;49:823–8. [PMC free article] [PubMed] [Google Scholar]