Introduction
This diverse and informative conference gave an invaluable update of sexual health and HIV medicine. The importance of early diagnosis of HIV infection and appropriate initiation of antiretrovirals (ARV) before patients present with advanced HIV disease was a strong theme, as were the advances in the prevention of sexual transmission of HIV by using pre-exposure prophylaxis (PrEP). The effect of alcohol consumption on sexual health and potential ability for sexual health clinics to modify patients' lifestyles was also discussed with much interest in view of the UK's current alcohol-related problems.
The Milroy lecture, traditionally given on an aspect of international health, was given by Professor Philippa Easterbrook, who updated delegates on the successes of various international programmes and the ‘roll-out’ of ARV in resource poor settings with all the associated challenges.
The diagnosis and management of primary HIV infection
Making an early diagnosis of HIV during primary HIV infection (PHI) can be challenging but has therapeutic benefits to the patient and can reduce the onward transmission of HIV at a time when patients are highly infectious. There are many non-specific symptoms a patient may complain of during PHI, however the triad of fever, pharyngitis and rash are most commonly present. These symptoms should alert health professionals to do an HIV test. Fourth generation tests, which include both HIV antibody and p24 antigen allow early detection from between two to four weeks following infection and, although a negative test at six weeks is usually accurate, this should be repeated at three months to be fully conclusive.
There are varying guidelines on the treatment of PHI with ARV, however the majority of patients are not treated. Guidelines will hopefully be clearer later this year following the reporting of the SPARTAC study,1 which aims to compare CD4 counts and progression to AIDS in patients receiving ARV for three months, 12 months and not at all following diagnosis of PHI.
The management of the late presenter with advanced HIV disease
Late presenters are patients with either an AIDS-defining opportunistic infection or malignancy and/or a CD4 count <200. These patients have a significant morbidity and mortality. In the UK in 2008, 55% of newly diagnosed patients had a CD4 cell count <350 and 32% had a CD4 count <200.2 An audit by the British HIV Association in 2006 demonstrated that 25% of deaths in people with HIV were due to a diagnosis being made too late for effective treatment.3
The aims of management of the late presenter are to treat any opportunistic infections (OI), identify any tumours, assess for any comorbidity such as hepatitis B or C and correct immunosuppression with ARV. The advantages of starting ARV early (<2 weeks after starting OI treatment) are a faster resolution of the OI and reduced risk of recurrence, however these may be outweighed by drug interactions and immune reconstitution syndrome (IRIS).
HIV and bone disease: an emerging problem
Since the advent of highly active antiretroviral therapy (HAART), a larger proportion of time is spent managing the complications and complexities of the treatment for HIV and the accelerated diseases of aging. High frequencies of osteoporosis and osteopenia are reported in patients with HIV and bone toxicity is listed as a long-term side effect of HAART. As a result, all HIV patients have an increased risk of fractures, especially those over 45 years. Predicting those patients who are most likely to have fractures is difficult as the Fracture Risk Assessment Tool (FRAX) algorithm does not take into account an HIV diagnosis. Screening for reduced bone mineral density (BMD) and risk of fractures should be part of HIV care. Lifestyle advice can be offered in areas such as diet and smoking, dual energy x-ray absorptiometry (DEXA) scans can be arranged appropriately to identify those patients with low BMD, and drug treatment with bisphosphonates can be initiated in those with reduced BMD.
Neurological complications of HIV infection
HIV is neuro-invasive and has the potential to cause disease at any site of the nervous system during the evolution from seroconversion to late stage HIV. Neither presentation (seizure, cerebrovasular accident, neurocognitive impairment, etc) nor treatment has changed radically from the pre-HAART era, although prognosis for conditions such as progressive multifocal leukoencephalopathy and primary central nervous system (CNS) lymphoma have improved somewhat as a result of ARV.
There is considerable research into the longer impact of HIV in those with minimal or minor symptoms indicative of neurocognitve impairment, to establish the role of the virus and the importance of combination ARV, especially when related to CNS penetration.
Non-AIDS defining malignancies
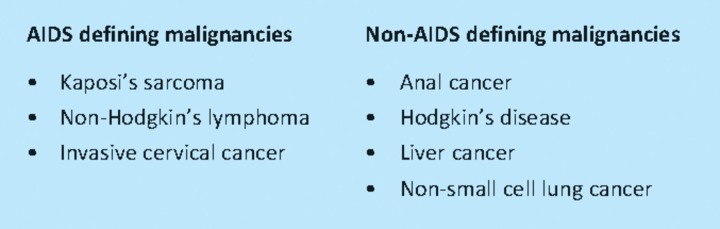
AIDS-related malignancies can be divided into AIDS defining and non-AIDS defining (Table 1). Non-AIDS defining malignancies (NADM) are overall twice as common in ‘matched’ subjects, however they have a similar outcome to non-HIV positive patients. Their risk is not related to CD4 count and incidence has not declined since HAART, unlike that of Kaposi's sarcoma and non-Hodgkin's lymphoma.
Table 1.
HIV-related malignancies.
Conference programme.
Anal cancer is of particular concern as its risk in men having sex with men (MSM) is 35 times higher than the risk in heterosexual men and an additional two to five times greater in HIV positive MSM. This increased risk has led to much discussion about the routine screening of anal cancer in at-risk groups; however, this has not yet been implemented in the UK.
Pre-exposure prophylaxis to prevent HIV transmission
Despite the clear dangers of unprotected sexual intercourse (UPSI) in HIV serodiscordant relationships, there remain situations when individuals cannot or will not avoid this risk. Post-exposure prophylaxis with a three-drug combination of ARVs for four weeks is advised but where such risks are planned or frequent the use of prophylactic ARVs taken before sexual intercourse may provide additional benefits.
Various lines of evidence support this strategy. Pre-exposure oral or topically applied ARVs (to the genital and rectal epithelium) prevent infection with SHIV in macaques. Animal studies also indicate that single doses taken pre-exposure do not provide effective prophylaxis even if these are timed to achieve maximal genital concentrations of the drug. These studies suggest that it is likely that PrEP will have to be combined to some extent with post-exposure therapy. Some ARVs are preferentially concentrated in genital secretions for both sexes (tenofovir and emtricitabine) and studies of PrEP have tended to concentrate on these agents. Large studies of PrEP in heterosexual couples are well underway and should allow the effectiveness of such a strategy to be determined. However, concerns remain as to the impact of PrEP on the emergence of resistant virus and whether it may have a deleterious effect on condom use - these effects may only become apparent in the longer term.
Periconceptual interventions in serodiscordant relationships
The prevention of infection at conception of HIV negative female partners of HIV positive males may be an indication for PrEP. Assisted reproductive techniques (ART) are available including sperm washing, intrauterine insemination, intracytoplasmic sperm injection and in vitro fertilisation. Such methods are effective and as many as 70% of couples will achieve a pregnancy with these techniques. However, funding of ART is not universally available and up to 60% of couples do not persist with ART when offered a referral. Increasingly couples are requesting low technology solutions for their fertility problems The conjecture that ‘an HIV infected individual without an additional sexually transmitted disease and on antiviral therapy with completely suppressed viraemia is sexually non-infectious’ has not been universally accepted and the demonstration of occasional disjuncture between semen and plasma viral loads has led some fertility specialists to advocate PrEP to couples who wish to conceive naturally. In the absence of human trial data, the timing of therapy is based on our understanding of the pharmacokinetics of these agents (one series reports the use of tenofovir 245 mg given with the LH surge, and then 24 hours later - sexual intercourse is timed 12 hours after the second dose, most couples achieved a pregnancy within three attempts, 30% did not after 12 attempts). Couples must be aware that currently little experience exists with PrEP and sperm washing remains the recommended means of managing this risk.
Developing new interventions in sexual health units
Those parts of the country with the highest levels of alcohol-related hospital admissions also have the highest teenage pregnancy rates. The recent demonstration of effective ER-based short interventions to modify alcohol consumption and reduce subsequent risk behaviour raises the possibility for similar interventions in other medical areas.
Sexual health units may be well placed for such interventions. Not only do departments see a large number of young people, there is growing evidence that poor sexual health is closely linked to alcohol consumption. Older patients who drink higher levels also report more UPSI. Although it does not follow that all these associations are causal, it may be time for sexual health units to consider how the promotion and provision of alcohol to young people in their communities may be impacting on patterns of teenage pregnancy, sexually transmitted infection rates and sexual assault. As the number of simple therapeutic options to manage sexual dysfunction has grown, many more patients have started to come forward with milder and earlier stage disease. In recent studies, over 40% of 40-year-old men complain that they have some difficulties with erectile function. The associations between erectile dysfunction (ED) and metabolic, cardiovascular and neurological disease are well established. The penile arteries are half the diameter of the coronary vessels and ED may be the earliest warning sign of impending catastrophic vascular disease. Physicians need to be aware of this feature and should make a careful assessment of any case of erectile failure, even in the young.
References
- 1.Medical Research Council Clinical Trials Unit. SPARTAC: short pulse anti-retroviral therapy at sero-conversion. Does taking anti-HIV treatment soon after infection delay damage to the immune system? (Trial ongoing) London: MRC; 2010. www.ctu.mrc.ac.uk/research_areas/study_details.aspx?s=32. [Google Scholar]
- 2.Health Protection Agency. Estimated late diagnosis of HIV by prevention group aged ≥ 15, UK 2008–HIV in the United Kingdom: 2009 Report. London: HPA; 2009. www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1259151891830. [Google Scholar]
- 3.BHIVA Audit and Standards Sub-Committee. Mortality audit 2006: scenario leading to death. London: BHIVA; 2006. [Google Scholar]