Key points
Allergic disease is widespread and causes significant morbidity
A careful history will identify triggers to avoid
Sensitisation can usually be confirmed by skin prick or specific IgE tests
Stepwise treatment should be followed
Consider immunological therapies in resistant disease
KEY WORDS: allergen immunotherapy, allergens, anti-IgE therapy, atopy, desensitisation
The prevalence of asthma and other allergic diseases such as eczema, rhinoconjunctivitis and food allergies has increased dramatically over the past 30 years. Asthma, in particular, is a serious global health problem and now the most common chronic condition in industrialised nations,1 with 300 million people affected worldwide in 2009 and 250,000 deaths recorded.2 Atopic asthma is the most common form of asthma, affecting 70–90% of children and about 50% of adult sufferers. Exposure to environmental proteins called allergens is responsible for the characteristic symptoms. Allergens are ubiquitous. Knowledge of an individual's provoking triggers via a careful history may lead to successful avoidance measures. Where conventional treatment fails, immunomodulation may be considered in the most severe cases.
Definitions: atopy versus allergy
There is a general misconception that ‘atopy’ and ‘allergy’ are interchangeable. ‘Atopy’ refers to a hereditary predisposition to high levels of immunoglobulin (Ig) E against common environmental proteins. This immune state is widespread, affecting about 30% of the UK population, but it can be totally asymptomatic with no need for avoidance measures. Only a subset of atopic individuals actually develops symptoms, which is when the term ‘allergy’ or ‘atopic disease’ may be used.
This distinction is important as random skin-prick tests and specific IgE (previously called RAST) tests do not diagnose allergy, only atopy. To confirm a directly causative allergy, a history also has to be taken. Although atopy can be asymptomatic, nonetheless it remains the strongest identifiable predisposing factor for developing asthma in the future. A 10–20 fold increased risk may be observed,3 with around 25–30% of atopic subjects developing asthma.4 The initial sensitisation to environmental allergens typically occurs in childhood.
Atopic asthmatic reactions: pathophysiology
The Global Initiative for Asthma defines asthma as a chronic inflammatory disorder of the airways with airway hyperresponsiveness, recurrent wheezing, coughing and shortness of breath (particularly at night or in the early morning), and widespread, variable airflow limitation that is often reversible either spontaneously or with treatment.2
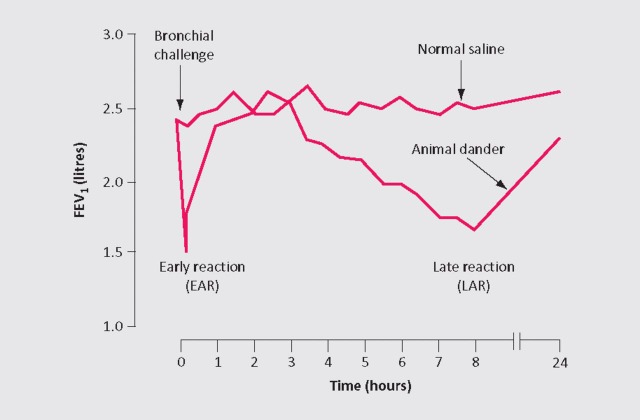
An individual with atopic asthma will have mast cell-bound IgE molecules residing in their airways. Inhalation of the offending allergen leads to cross-linking of adjacent IgE molecules, causing mast cell activation and release of mediators including histamine and tryptase. This leads to an immediate or acute-phase asthmatic reaction, peaking at 15 minutes and resolving within an hour. Around 50% of asthmatics also experience a late-phase reaction at about six hours, due to a Th2 lymphocyte-mediated influx of inflammatory cells, eosinophils in particular, and further release of mediators. This can be replicated under experimental conditions or in clinical practice when investigating occupational asthma using an inhaled allergen challenge with nebulised soluble allergen extract (Fig 1). The late-phase reaction is associated with subsequent bronchial hyperreactivity and symptoms to non-specific stimuli, such as exercise and cold air, for about a further week.
Fig 1.
Inhaled whole allergen challenge.
Airborne allergens
Outdoor allergens
Airborne allergens represent the most common environmental factors that can induce an atopic asthmatic reaction. The main cause of seasonal asthma in the UK is grass pollen, particularly perennial rye and timothy grass. Symptoms peak during June and July. Symptoms in spring are commonly due to tree pollens, whereas in late summer and autumn they may be due to weed pollens and mould spores including Alternaria alternata and Cladosporium herbatum. Some asthmatics are also sensitised to the fungus Aspergillus fumigatus.
Indoor allergens
The predominant indoor allergens are from house-dust mites, cats, dogs and cockroaches. Bird feathers (in pillows) can also cause allergy, although testing shows patients to be more commonly allergic to the coexisting house-dust mite. Most particles carrying house-dust mite and cockroach allergens are relatively large (30 mm) and settle quickly. Therefore exposure is largely confined to close exposure to fabrics in bedding, carpets and soft furnishings.
Domestic cats
Proteins from domestic cats are some of the most potent elicitors of allergic disease, affecting 10% of the population in industrialised countries. The allergen, carried by small airborne particles, is ubiquitous in the environment, including public places such as schools and transportation, and is carried on clothing. Even after permanent removal of a cat from the home, it may take many months before the reservoir allergen concentration returns to normal.
Occupational asthma
Occupational asthma can be triggered by a wide range of protein allergens (eg rodent urine, grain, flours, latex, harvest moulds and bacillus subtilis enzymes (in detergents)), as well as low-molecular weight chemicals, including pinewood resin, isocyanates, platinum salts and acid anhydrides.
Food allergens
Typically, food allergy causes multiple, quick onset (minutes, often immediate) symptoms and signs. Features include oral itch, a widespread urticarial rash, nausea and gastrointestinal upset, as well as rhinitis, wheeze or other respiratory symptoms. Isolated respiratory features would be unusual.
Patients allergic to birch and certain other pollens may also have cross-reactions with various plant-derived foods - the so-called ‘oral allergy syndrome’. Classically, raw uncooked fruits and vegetables provoke symptoms but cooking destroys the trigger allergens.
Non-IgE mediated reactions
Non-IgE mediated immediate asthmatic reactions may occur with food additives and colourings, including benzoates, salicylates, sulphites and tartrazine. Preservatives such as sulphites are commonly sprayed on lettuce to maintain freshness. They are also present in dried fruit, including apricots, as well as in alcoholic drinks where they occur both naturally (from grapes) and are further added to prevent microbial growth.
Salicylate sensitivity is another potential problem. High levels of natural salicylates are found in grapes, yeast, wines, beers and other foodstuffs, including certain fruit, vegetables, herbs and spices. Unfortunately, there are no diagnostic tests for reactions to additives and/or colourings as the reactions are non-IgE mediated. Diagnosis depends on suspicion and the use of elimination diets or, rarely, blinded challenges with capsules containing the active ingredient versus placebo.
Assessing the patient
The British Thoracic Society (BTS) guideline on the management of asthma5 recommends a diagnosis of asthma if there is a combination of characteristic symptoms with suggestive changes in lung function tests. In most cases, an allergic element to the disease can be elicited by a careful clinical history alone, without need for further testing. However, skin-prick testing (answer within minutes in clinic) or equivalent allergen-specific IgE blood tests can help to support (or discount) an allergy diagnosis.
Skin-prick testing and specific IgE blood tests
Soluble extracts of suspected allergens are pricked into the skin to provoke a cutaneous wheal and flare (early-phase reaction). Antihistamines should be discontinued for at least 48 hours before testing and positive (histamine) and negative (diluent) controls must be included. Alternatively, serum levels of specific (individual) IgEs against allergens may be measured (formerly known as RAST tests) to demonstrate sensitisation. Unfortunately, unlike aero-allergens, food allergen extracts are poorly standardised, affecting the results of both skin-prick testing and specific IgE tests, sometimes generating misleading results.
The number of available tests is limited. With foods, the ‘prick-prick’ method using the actual foods can extend the repertoire, in many cases generating more reliable results. Requesting a total IgE level alone is unnecessary and provides no information on the specific offending allergen.
Allergen avoidance
Reducing allergen exposure will reduce not only the frequency of immediate reactions but also the severity of airway hyperresponsiveness and susceptibility to further allergen-induced attacks. Avoidance measures for a single dominant allergen, such as cat, or in occupational asthma are particularly effective. Measures to decrease house-dust mites have not been shown to have an effect on asthma severity. A Cochrane systematic review concluded that house-dust mite control measures cannot be recommended.6 Mite avoidance measures include use of mite-proof covers for bedding, removal of carpets and high temperature washing of bed linen.7
Allergen immunotherapy
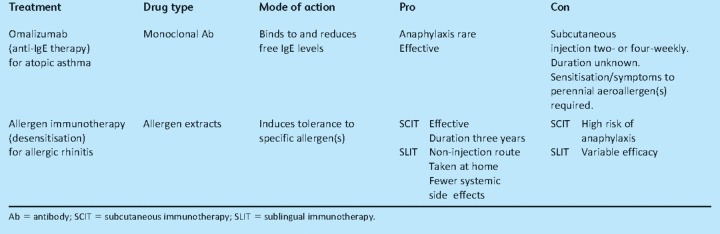
The BTS stepwise pharmacological management of asthma should be followed.5 However, some patients may remain resistant to conventional treatment and need immunological therapy (Table 1). Specific immunotherapy (whole-allergen immunotherapy or desensitisation) is performed in specialist allergy clinics for intractable allergic rhinitis or venom allergy to induce both immunological and clinical tolerance.8 It has also been shown to reduce subsequent development of asthma in children with allergic rhinoconjunctivitis.9
Table 1.
Pros and cons of immunological therapies.
Subcutaneous immunotherapy (SCIT)
Specific immunotherapy is usually undertaken via the subcutaneous route (SCIT) and has proven efficacy. It takes about three years and involves the injection of increasing doses of allergen extracts. There is a risk of IgE-mediated adverse events, including anaphylaxis, so the idea of using SCIT for atopic asthma has always been controversial.
A recent Cochrane meta-analysis examined 88 trials of SCIT in atopic asthma,10 mostly for house-dust mite allergy. Unfortunately, blinding was adequate in only 16 trials and there was significant heterogeneity. However, overall there was a significant reduction in asthma symptoms and medication and improvement in bronchial hyperreactivity. There was no consistent effect on lung function. It was estimated that if nine patients were treated with immunotherapy, one would be expected to develop a local adverse reaction, and if 16 patients were treated, one would be expected to develop a systemic reaction. Currently, SCIT is not used to treat atopic asthma in the UK and chronic asthma is a contraindication for use of SCIT to treat allergic rhinitis.
Sublingual immunotherapy (SLIT)
Sublingual (SLIT) administration using allergen extracts is an emerging effective alternative to SCIT, thus far with a better safety profile and greater convenience since it may be self-administered at home.11 Anaphylaxis has, however, been reported in a patient being treated with multiple allergen extracts.12 There can be variable efficacy,13 but it is particularly effective in the treatment of grass pollen allergy.14
Anti-IgE therapy: omalizumab
Omalizumab is a recombinant humanised monoclonal antibody used as add-on therapy for severe atopic asthma. It works by forming complexes with circulating IgE, thus blocking the interaction of IgE with mast cells and basophils, and also inhibiting other pathways that involve allergen trapping and focusing by IgE. Single doses of omalizumab rapidly reduce serum-free IgE concentrations by over 95%.15 A significant reduction in the rate of clinically significant asthma exacerbations, severe exacerbations and emergency visits in patients with inadequately controlled severe persistent asthma (despite high-dose inhaled corticosteroid, long-acting beta-2 agonist therapy and often additional therapy) has been found in patients using omalizumab.16
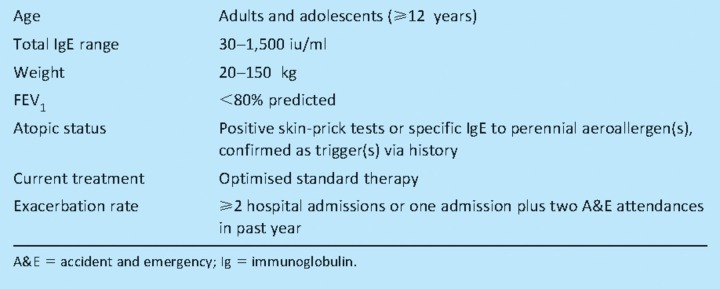
Omalizumab is now recommended by the National Institute for Health and Clinical Excellence (NICE) as a treatment for severe persistent allergic asthma in patients with sensitivity to perennial trigger allergens, confirmed via history and skin-prick tests/specific IgE tests (Table 2; Case 1). Whether omalizumab will be effective in patients with negative skin tests or specific IgE tests (ie with non-atopic asthma; Case 2) remains to be determined and is currently the subject of ongoing studies.
Table 2.
Omalizumab for severe persistent allergic asthma: National Institute for Health and Clinical Excellence (NICE) guidance for eligibility.
Case 1.
Case 2.
Suggested websites
-
1
British Society for Allergy and Clinical Immunology: www.bsaci.org (for healthcare professionals).
-
2
Allergy UK: www.allergyuk.org (for patients).
References
- 1.Barnes PJ. The size of the problem of managing asthma. Respir Med. 2004;98(Suppl B):S4–8. doi: 10.1016/j.rmed.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 2.Global Initiative for Asthma (GINA) Global Strategy for Asthma Management and Prevention. NIH Publication 02–3659, issued January 1995 (last updated 2009). www.ginaAsthma.com.
- 3.Holgate ST. Genetic and environmental interaction in allergy and asthma. J Allergy Clin Immunol. 1999;104:1139–46. doi: 10.1016/S0091-6749(99)70005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holt PG, Macaubas C, Stumbles PA, Sly PD. The role of allergy in the development of asthma. Nature. 1999;402(Suppl):B12–7. doi: 10.1038/35037009. [DOI] [PubMed] [Google Scholar]
- 5.British Thoracic Society Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. Thorax. 2008;63(Suppl 4):iv1–121. doi: 10.1136/thx.2008.097741. Revised June 2009. [DOI] [PubMed] [Google Scholar]
- 6.Go tzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev 2004;(4):CD001187. Update in. Cochrane Database Syst Rev. 2008;(2):CD001187. [Google Scholar]
- 7.Simpson A, Simpson B, Custovic A, Craven M, Woodcock A. Stringent environmental control in pregnancy and early life: the long term effects on mite, cat and dog allergen. Clin Exp Allergy. 2003;33:1183–9. doi: 10.1046/j.1365-2745.2003.01679.x. [DOI] [PubMed] [Google Scholar]
- 8.Bousquet J, Lockey R, Malling HJ. Allergen immunotherapy: therapeutic vaccines for allergic diseases. A WHO position paper. J Allergy Clin Immunol. 1998;102(4 Pt 1):558–62. doi: 10.1016/S0091-6749(98)70271-4. [DOI] [PubMed] [Google Scholar]
- 9.Jacobsen L, Niggemann B, Dreborg S, et al. Specific immunotherapy has long-term preventive effect of seasonal and perennial asthma: 10-year follow-up on the PAT study. Allergy. 2007;62:943–8. doi: 10.1111/j.1398-9995.2007.01451.x. [DOI] [PubMed] [Google Scholar]
- 10.Abramson MJ, Puy RM, Weiner JM. Injection allergen immunotherapy for asthma. Cochrane Database Syst Rev. 2010;(8):CD001186. doi: 10.1002/14651858.CD001186.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Radulovic S, Calderon MA, Wilson D, Durham S. Sublingual immunotherapy for allergic rhinitis. Cochrane Database Syst Rev. 2010;(12):CD002893. doi: 10.1002/14651858.CD002893.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dunsky EH, Goldstein MF, Dvorin DJ, Belecanech GA. Anaphylaxis to sublingual immunotherapy. Allergy. 2006;61:1235. doi: 10.1111/j.1398-9995.2006.01137.x. [DOI] [PubMed] [Google Scholar]
- 13.Greenberger PA, Ballow M, Casale TB, Platts-Mills TA, Sampson HA. Sublingual immunotherapy and subcutaneous immunotherapy: issues in the United States. J Allergy Clin Immunol. 2007;120:1466–8. doi: 10.1016/j.jaci.2007.08.055. [DOI] [PubMed] [Google Scholar]
- 14.Calderón M, Brandt T. Treatment of grass pollen allergy: focus on a standardized grass allergen extract–Grazax. Ther Clin Risk Manag. 2008;4:1255–60. doi: 10.2147/tcrm.s3544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corne J, Djukanovic R, Thomas L, et al. The effect of intravenous administration of a chimeric anti-IgE antibody on serum IgE levels in atopic subjects: efficacy, safety, and pharmacokinetics. J Clin Invest. 1997;99:879–87. doi: 10.1172/JCI119252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Humbert M, Beasley R, Ayres J, et al. Benefits of omalizumab as add-on therapy in patients with severe persistent asthma who are inadequately controlled despite best available therapy (GINA 2002 step 4 treatment): INNOVATE. Allergy. 2005;60:309–16. doi: 10.1111/j.1398-9995.2004.00772.x. [DOI] [PubMed] [Google Scholar]