Suboptimal discharge management of asthmatic patients increases risk of early re-hospitalisation,1,2 creating potentially avoidable burden for patients and medical services. British Thoracic Society (BTS) guidelines propose optimal management standards.3 A 2007 audit in our hospital against those guidelines found poor discharge related asthma management. Consequently, in January 2008 an asthma nurse specialist (ANS) was introduced in parallel with respiratory physician (RP)-led management of acute respiratory admissions.
Aims
Firstly we evaluated the impact of introducing both ANS and RP on discharge management, length of in-patient stay and re-hospitalisation rates within 28 days. Secondly we examined whether review by an ANS made a difference to the above parameters.
Methods
Using case notes, data was collected for asthmatic patients discharged in the first three months of 2007 and 2009. To answer primary research questions, data from 2007 was compared against 2009. To answer the secondary research question cross sectional analysis was performed on the 2009 data.
Results
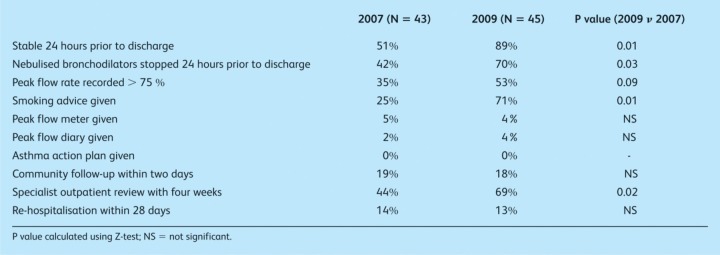
Comparing 2009 to 2007 (Table 1), significant improvements were seen for patients stable for 24 hours prior to discharge, stopping nebulised bronchodilators 24 hours prior to discharge, advice on smoking, specialist outpatient review within four weeks - 80% of follow-ups being at an ANS-led clinic in 2009.
Table 1.
Discharge related outcome measures compared between 2007 and 2009.
In 2009, 76% were managed by RP, 58% reviewed by ANS and 49% seen by both. In 2009, comparing those managed by RP n non-specialist, length of stay was greater (4.1 n 0.9 days (p < 0.001)), but re-hospitalisation within 28 days was lower (9% n 32% (p=0.22)) with RP-led care. Comparing patients reviewed by ANS against those not, significant difference was seen in: lifestyle advice (35% n 0%, p=0.04); checking inhaler technique (50% n 10%, p=0.05); four week follow-up in the ANS clinic (81% n 21%, p < 0.001); re-hospitalisation within 28 days (0% n 32%, p=0.03).
Discussion
This study strengthens the notion that acute specialist intervention significantly improves standards of acute asthma management.4 However, contrary to expectations, RP involvement significantly prolonged admission. Whilst this may reflect that the specialist dealt with more complicated cases, it may indicate potentially misplaced prioritisation for early discharge by non-specialist teams. Re-hospitalisation rates were 0% with ANS input, irrespective of the medical team leading management. This suggests a potent role for ANS in optimising post exacerbation management.
Asthma exacerbations suggest significant loss of asthma control and signal the need for close follow-up to address underlying causes. The increase in specialist follow-up within four weeks, from 2007 to 2009, mostly involved an ANS-led clinic. Such initial follow-up has been shown to be as effective and safe as review at a physician-led clinic.5 ANS clinics could serve a valuable triaging function, ensuring appropriate usage of the physician-led clinic, reducing waiting times and potentially decreasing expenditure for the local health economy.
In conclusion, multidisciplinary specialist care applied early in the care pathway can improve standards of discharge management for inpatients with acute asthma. Further exploration of the novel strategies reported in this paper should be encouraged.
References
- 1.Udwadia ZF, Harriaon BD. An attempt to determine the optimal duration of hospital stay following a severe attack of asthma. J R Coll Physicians Lond. 1990;24:112–14. [PMC free article] [PubMed] [Google Scholar]
- 2.Pearson MG, Ryland I, Harrison BD. National audit of acute severe asthma in adults admitted to hospital. Standards of Care Committee, British Thoracic Society. Qual Health Care. 1995;4:24–30. doi: 10.1136/qshc.4.1.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.British Thoracic Society, Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma: a national clinical guideline. May 2008. (Revised May 2011)
- 4.Vollmer WM, O'Hollaren Ettinger KM, et al. Speciality differences in the management of asthma. A cross sectional assessment of allergists’ patients and generalists’ patients in a large HMO. Arch Intern Med. 1997;157:1201–8. [PubMed] [Google Scholar]
- 5.Nathan JA, Pearce L, Field C, et al. A randomised controlled trial of follow-up of patients discharge from hospital following acute asthma: best performed by specialist nurse or doctor? Chest. 2006;130:51–7. doi: 10.1378/chest.130.1.51. [DOI] [PubMed] [Google Scholar]