Abstract
In April 2009 a ‘considerative checklist’ was developed to ensure that all important aspects of care on a team's routine and post-take general internal medicine ward rounds had been addressed and in order to answer the question: How long should a ward round take, when conducted to high standards of quality and safety at the point of care? The checklist has been used on 120 ward rounds: 90 routine ward rounds and 30 post-take ward rounds. Overall, the average time per patient was 12 minutes (10 minutes on routine rounds and 14 minutes on post-take rounds). The considerative checklist has encouraged and enabled documented evidence of high quality and safe medical care, and anecdotally improved team working, communication with patients, and team and patient satisfaction.
Key Words: checklist, medical ward round, patient safety, team working
Introduction
Ward rounds are complex clinical activities where:
clinical diagnosis is revised
a clinical examination is undertaken
decisions about future investigations and treatment options are made
discharge plans are formulated
written and verbal communication is undertaken.1
These important decisions ultimately influence the outcome of each patient.
NHS consultants frequently have fixed time allocations to undertake their wards rounds, regardless of the number and complexity of patients under their care. How long should it take to complete a ward round to a high standard of quality and safety? To answer this question it is important to know how many patients there are to be seen, what the review process entails and some reasonable indicators of quality. Standard measures of quality of care, such as length of stay, mortality and readmission rate, give no reassurance that a particular ward round has been conducted to high standards of quality and safety. There seem to be no indicators of what constitutes a daily or post-take ward round or any useful parameters of quality and safety ‘at the point of care’. This leaves the profession at the mercy of managers who could insist that ward rounds are carried out swiftly to enhance early discharge of patients, and to free up time to attain other targets.
Background
Worthing Hospital is a district general hospital on the south coast of England. It receives about 10,000 acute general internal medicine admissions a year through the acute medical unit (AMU) and coronary care unit (CCU). There is a separate needs-related geriatrics receiving service. Since August 2009, daytime weekday patients have been the responsibility of the acute physicians. When patients are transferred from the AMU to the medical wards, care is transferred to ward-based teams. GC admits patients one day in seven, and does two routine ward rounds a week. The number of junior doctors on ward rounds can vary substantially, in part due to the introduction of the European Working Time Directive.
During this period a bespoke ward round trolley was built to carry the notes, stationery and examination equipment, and to provide a large writing area. This also facilitated team and ‘just in time’ working and reduced non-productive walking time on rounds.
Development of the considerative checklist
GC has conducted ‘instant team assessments of performance’ since November 2004. One of the pages of the proforma allows for a member of the team to assess the ward round leader (Box 1). Over the years GC has used this process to assess the performance of specialist registrars (SpR). In April 2009, the foundation year (FY)1 asked to lead the routine consultant ward round. She performed very well, but expressed concern as to whether she had ‘done it all’. This prompted the team to develop a ward round checklist which could serve as an important tool for ensuring and improving overall standards of patient care.2 The World Health Organization has already recognised the potential of checklists with the introduction of the surgical safety checklist to reduce morbidity and mortality.3
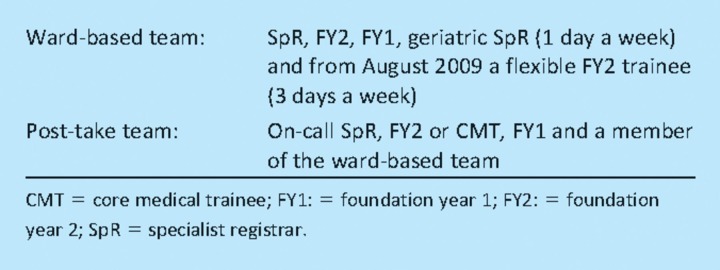
Box 1. The ward round team. Doctors may be absent due to nights shifts, annual/study leave or rest days.
The checklist domains were developed entirely on a rational and pragmatic basis by reflecting on all the work and decisions that were thought to be important for a comprehensive patient review. There was no intention to drive a routine into the round or to limit clinical thinking. The Caldwell considerative checklist process is shown in Fig 1. The checklist domains were grouped into sections to fit with the team's work pattern, ‘preparation’, ‘consultation’, ‘charts’, ‘ceiling of care’, ‘discharge planning’, ‘planning’ and ‘summing up’. Essential check domains were coloured yellow, whereas domains that applied only to some patients, for example blood glucose chart, were left in white. Its simplicity lies in the fact that it takes up only one side of A4 paper and can easily be adapted to a clinical context.
Fig 1.
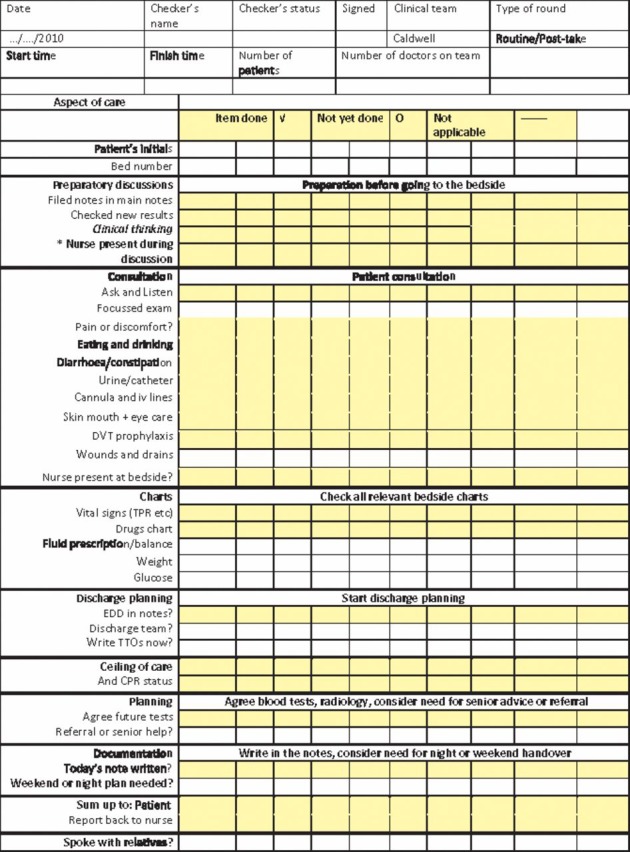
The Caldwell considerative checklist process. CPR = cardiopulmonary resuscitation; DVT = deep vein thrombosis; EDD = estimated date of discharge; iv = intravenous; TPR = temperature, pulse, respiratory rate; TTO = treatment to take away. One member of the team is the ‘Safety checker’ and must highlight any omissions. The tinted sections must be checked in all patients. *Mark tick for nurse present during preparatory discussions © Dr G Caldwell January 2010.
The checklist is called a ‘considerative checklist’, because it is used to record that a matter has been considered and, if necessary, a decision has been made. For example, under ‘DVT prophylaxis’ a decision to start, stop or modify deep vein thrombosis (DVT) prophylaxis can all be marked as a tick. In this way the considerative checklist does not limit clinical thinking, risk assessment and decision making.
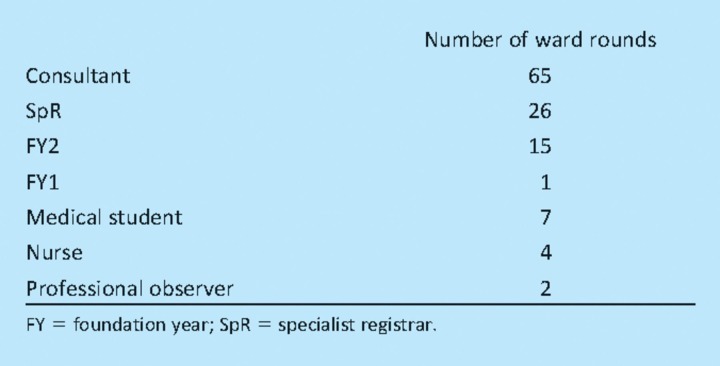
The role of checker
The role of checker has been taken on by the consultant, SpR, FY2, FY1, medical student, nurse and other professional observers (Table 1). The leader tells the checker to closely observe the round and ensure that everything is covered. The checker must be ready at the end of each patient review to report any omissions and have them corrected. They can tick off items as they see them ‘considered’. If a ‘yellow’ (essential) item is not covered they draw a circle in the box and then tick through the circle once the omission is dealt with. ‘White’ domains, eg glucose levels in a non-diabetic patient, can simply be left blank.
Table 1.
The role of the checker.
Quantitative results: how long does a ward round take?
The considerative checklist has been used on 120 wards rounds between April 2009 and March 2010 (90 routine and 30 post-take):
in all, 1,700 patient reviews were undertaken, taking an average of 12 minutes, 10 minutes on routine rounds and 14 minutes on post-take rounds
the shortest average review time was eight minutes and the longest 24 minutes
the shortest round was 90 minutes and the longest was 420 minutes
the largest number of doctors on the round was six and the smallest was one
no breaks were taken on any ward rounds.
There seemed to be a tendency for the time per patient to increase on smaller rounds and this was probably because time was then taken for teaching and assessments of junior doctors' performance. Communication with nurses was deficient both in quantity and quality. Heterogeneous communication can lead to uncertainty.4 Methods to improve clinical communication have been studied extensively in the intensive care setting but there are limited studies looking at the impact on medical ward rounds.5
Qualitative and anecdotal results
It is impossible to count the number of decisions that were made or omissions corrected as a result of this process. Similarly had non-user's performance been audited this would have altered their behaviour. Some of the incoming notes of transferred patients from other consultants' teams were audited and shortfalls in filing of the clerking notes, cardiopulmonary resuscitation (CPR) decisions, DVT prophylaxis decisions, legibility, safety and accountability of prescribing and documentation of the estimated date of discharge were found.
Patient reviews have become more systematic but still retain all of the humanity of high quality professional consultations. In the early weeks it was realised that many important aspects of reviews had been missed including: careful checking of results, and legible and accountable prescribing. It was common to find cannulas that had been unused and which posed a risk for cellulitis or septicaemia, or to find a catheter that should have been removed. The team now talks much more with patients about the importance of drinking to speed the discontinuation of intravenous infusions, and eating to ensure appropriate nutrition. The nursing staff appreciate that the team has made ‘For’ or ‘Not for CPR’ decisions. The number of tests requested has been reduced, by forcing the planning of tests on each round. The junior doctors no longer decide on blood test frequency have also streamlined handover.
Ward round leaders have all expressed that the considerative checklist:
provides reassurance that quality care has been provided
aids active participation from healthcare professionals and patients
encourages improvement.
Discussion
High quality safe care can result in saving a patient's life, a return to full health or the calm death of a patient. Measuring quality and safety at the point of care, however, is fraught with problems. Traditional measures of quality, such as length of stay, mortality and readmission rates, and retrospective audits of care pathways have little immediate impact on improving quality and safety, and are subject to many variables, resulting in endless debates about cause and effect. The ultimate measure of quality and safety might be the correct diagnosis and the application of appropriate evidence-based treatments. However, clinicians would struggle to agree on the same terminology for the diagnoses let alone come to any sort of agreement about the appropriate evidence-based treatment in the individual's context. Another approach to measuring quality has been retrospective audit of specific conditions. These processes are costly, time consuming, oversimplify the clinical context and may encourage treatment of the audited conditions, for example acute coronary syndrome, over the not audited conditions, for example being severely ill with no yet established diagnosis.
This study attempted to measure whether the processes were more likely to support safe high quality care for all patients, rather than to measure the outcomes in a comparative process. It may be impossible to find measurable reliable indicators of the outcomes of safe high quality care in acute general internal medicine without distorting appropriate care of all patients.
How long should a ward round take when attention is paid to ‘quality and safety at the point of care’? This study shows that currently it is 10 minutes per patient for a routine round and 14 for a post-take ward round. This process does not include teaching and assessment within the domains but, on quieter rounds, the time per patient was increased because of teaching and assessment time.6 Students found the checklists very instructive, as some learning could be included even in the busiest wards. Two other consultants are using this checklist, to improve quality and safety, and as an apprenticeship tool.
The considerative checklist may have a role in revalidation. It would be a practical method to demonstrate competence. Completion of a semi-structured assessment of performance of the ward round lead, developed as part of the immediate ward round feedback process, would add to the validity of revalidation in one working session, when observed by another professional.7
Conclusion
This article has presented rational evidence based on a pragmatic analysis of the complexity of ward rounds that show an improvement in quality and safety at the point of care, and provide evidence from one team to answer the question ‘How long should a ward round take when attention is paid to ‘quality and safety at the point of care’?’.
References
- 1.Brown N, Webster A. New medical technologies and society: reordering life. Cambridge: Polity; 2004. [Google Scholar]
- 2.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. New Engl J Med. 2009;6:491–9. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 3.Hales B, Terblanche M, Fowler R, Sibbald W. Development of medical checklists for improved quality of patient care. Int J Qual Health Care. 2008;20:22–30. doi: 10.1093/intqhc/mzm062. [DOI] [PubMed] [Google Scholar]
- 4.Iedema R, Long D, Forsyth R, Lee B. Visibilising clinical work: video ethnography in the contemporary hospital. Health Soc Rev. 2006;15:156–68. doi: 10.5172/hesr.2006.15.2.156. [DOI] [Google Scholar]
- 5.Carroll K, Iedema R, Kerridge R. Reshaping ICU ward round practices using video-reflexive ethnography. Qual Health Res. 2008;18:380–90. doi: 10.1177/1049732307313430. [DOI] [PubMed] [Google Scholar]
- 6.Stanley P. Structuring ward rounds for learning: can opportunities be created? Med Educ. 1998;32:239–43. doi: 10.1046/j.1365-2923.1998.00201.x. [DOI] [PubMed] [Google Scholar]
- 7.Caldwell G. Real-time assessment and feedback of junior doctors improves clinical performance. The Clinical Teacher. 2006;3:185–8. doi: 10.1111/j.1743-498X.2006.00100.x. [DOI] [Google Scholar]