Key points
Urinary tract infection (UTI) is common in older people
Older people presenting non-specifically are often incorrectly diagnosed as having a UTI
Asymptomatic bacteriuria is common in frail older people and should not be treated
There is no reliable diagnostic test for UTI
The antibiotic chosen to treat UTI should have as narrow spectrum as possible and be prescribed for the shortest effective duration
Older adults are more prone than younger individuals to developing urinary tract infections (UTIs) for several reasons, including:
incomplete bladder emptying (often related to prostatic enlargement in men)
higher rate of catheter use
increased susceptibility to infection associated with frailty.
A sudden decline in physical and/or cognitive function in older people is usually ascribed to a UTI, yet this commonly adopted clinical practice is not supported by the research evidence.1
Definitions of infection
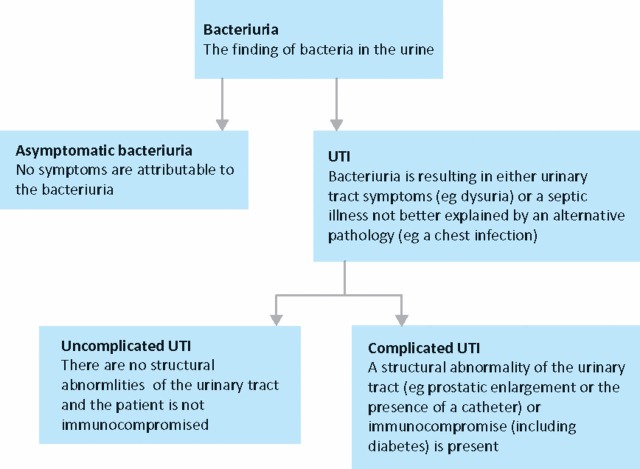
Symptomatic UTI is defined as bacteriuria causing urinary tract symptoms. It can be classified as upper (eg pyelonephritis) or lower (eg cystitis), the former classically presenting with flank pain and renal angle tenderness, the latter as dysuria, frequency and urgency of micturition. Additionally, UTI can be divided into complicated and uncomplicated forms (Fig 1). A complicated UTI occurs in a person with an abnormal urinary tract or an increased susceptibility to infection. This includes people with catheters or diabetes, and all men (due to the frequent association with prostatic enlargement). Bacteraemic UTI occurs when the same organism is identified in the blood and urine simultaneously.
Fig 1.
Diagnostic categories of bacteriuria UTI = urinary tract infection.
Diagnostic problems
One of the major difficulties with diagnosis of UTI in older people is the high prevalence of asymptomatic bacteriuria (ASB): the presence of bacteria in the urine of people without attributable symptoms. ASB is rare in younger people but over the age of 75 years is found in 7–10% of men and 17–20% of women, and in up to 40–50% of non-catheterised people in care homes.2–4 All long-term catheter users have bacteriuria. ASB is associated with white blood cells (WBC) in the urine (pyuria) in over 90% of cases.3 A patient presenting with symptoms unrelated to the urinary tract who is found to have ASB may then mistakenly be labelled as a ‘proven UTI’, which propagates the myth of UTIs as a common cause for non-specific symptoms in older people. Treating ASB does not reduce either mortality or morbidity but increases the risks of antibiotic-related adverse events and colonisation with resistant organisms.5,6
A second major diagnostic difficulty is that many older people presenting with a genuine UTI (even bacteraemic UTI) do not have urinary tract symptoms.7,8 Alternative presentations may include acute functional or cognitive decline. Possible explanations include the presence of either urinary catheters or cognitive impairment (dementia or delirium) that precludes a reliable history. In addition, older people may have chronic urinary symptoms such as incontinence, nocturia and urgency unrelated to a UTI. This group of patients therefore falls outside the conventional ideas of either ASB or symptomatic UTI, making an accurate diagnosis particularly challenging.
Only symptoms of acute onset should be considered relevant to a diagnosis of UTI. It is helpful to distinguish ASB from a genuine UTI by evidence of a septic illness (ie pyrexia, raised serum WBC count or inflammatory markers) in the absence of an alternative more likely explanation (eg a chest infection).
Urine testing
The high prevalence of ASB means that both urine culture and urine dipstick tests are of limited diagnostic value in older people. Moreover, urine samples may be hard to obtain due to urinary incontinence or cognitive impairment, or unreliable due to contamination or the prior receipt of antibiotics.
Urine culture
A urine culture negative for growth when taken prior to the receipt of antibiotics effectively excludes UTI. Ideally, a urine culture should be obtained in all older patients suspected of a UTI to guide antibiotic sensitivities.
Dipstick tests
Urine dipsticks test for both leukocyte esterase (a marker for pyuria) and urinary nitrites (coliform bacteria reduce nitrates in urine to nitrites). Escherichia coli is the most common causative organism in younger and older adults. Other coliforms (Gram-negative organisms found in the intestine, eg klebsiella, proteus and enterobacter) are also frequently detected. However, Gram-positive (eg enterococci) and atypical organisms (eg pseudomonas) account for a larger proportion of UTIs in older people.9 This is relevant because these organisms are less sensitive to commonly used antibiotics and do not reduce urinary nitrates to nitrites. This latter property means that urinary dipsticks will not test positive for nitrites.
It has been suggested that urine dipsticks negative for both leukocytes and nitrites could be used to exclude elderly people without UTI. However, the high rate of positive tests would result in only a small number of patients tested being excluded and a false negative rate of 10–20%.10 For these reasons, urinary dipsticks have only a limited role in diagnosing UTI in older people.
Blood tests
A raised WBC count or C-reactive protein level are consistent with an infective illness. A blood culture positive for a known uropathogen in the absence of an alternative more likely source suggests a UTI, especially if urine culture is also positive for the same organism.
Making a diagnosis
As discussed above, diagnosis of UTI is difficult. Unfortunately, there is no gold-standard diagnostic test for a UTI. The high prevalence of ASB and non-specific presentations (ie without urinary tract symptoms) in older people complicates the situation. The diagnosis of UTI in acutely unwell, hospitalised older patients is probably incorrect in about 40% of cases.8 This results in inappropriate exposure to antibiotics and delay in establishing the correct diagnosis. Guidelines designed for diagnosing younger people often rely on the presence of urinary tract symptoms.4 As stated previously, this alone is insufficiently sensitive to accurately diagnose many frail older adults.
Clinical decision tools have been developed in nursing home populations to try to limit inappropriate antibiotic use.11,12 However, their sensitivities and specificities are poor in comparison to finding bacteriuria and pyuria on urine testing.13
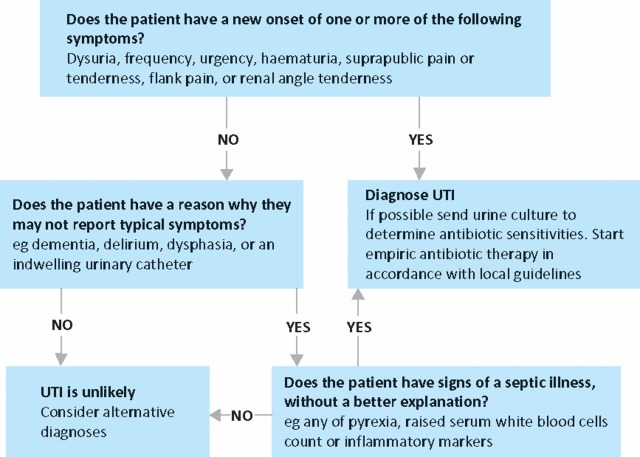
The assessment of acutely unwell older people should be comprehensive in its nature, including cognitive assessment. Some patients with non-specific declines in cognition or functional status will have a UTI but many will not. A suggested scheme to assist diagnosis that takes all these factors into account is shown in Figure 2.14
Fig 2.
A suggested approach to the evaluation of an unwell older adult for suspected urinary tract infection (UTI). Reproduced with permission from Radcliffe Publishing.14
Treatment
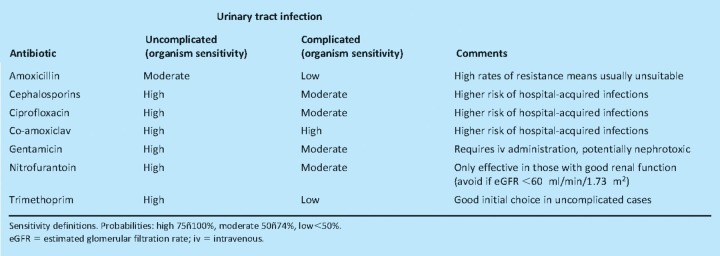
The use of antibiotics is associated with the development of meticillin-resistant Staphylococcus aureus and Clostridium difficile infections. This seems to be particularly true for older people and for broad-spectrum agents (eg ciprofloxacin, co-amoxiclav and cephalosporins). Resistance to commonly used antibiotics, especially amoxicillin and trimethoprim, is rising. Infections caused by multidrug resistant organisms are more common in older adults, especially those with catheters or residing in long-term care.15 Uncomplicated UTI is typically caused by less resistant organisms, so initial treatment with a narrow-spectrum antibiotic (eg trimethoprim) is appropriate. Complicated UTI is usually best initially treated with a broad-spectrum antibiotic. If antibiotic sensitivities subsequently show a narrow-spectrum agent is appropriate, consideration should be given to changing medication to limit the risk of hospital-acquired infection. Table 1 provides a comparison of antibiotics commonly used for treating UTI in the UK.
Table 1.
A comparison of antibiotics commonly used to treat urinary tract infection in older adults in the UK (based on data from reference 8).
Duration of treatment
There is good evidence that three-day courses of antibiotics are effective for patients with uncomplicated UTI.16 Courses of seven days or more are recommended for complicated UTI.4 Patients with a urinary catheter should have it changed prior to antibiotic treatment as this leads to more rapid improvement and less treatment failure.17 It also provides an opportunity to collect a sample of urine from the bladder that is less likely to be contaminated.
Prevention
Two small randomised trials have suggested topical oestrogens may reduce the risk of recurrent UTI. However, they are associated with poor patient concordance and are not recommended for long-term use, thus limiting any potential benefit. Long-term, low-dose antibiotics appear to reduce the risk of UTI in young women but few data are available for older people.18 Concerns with this strategy include antibiotic side effects and colonisation with resistant organisms. Cranberry juice may be an alternative option, with effects that possibly impair the adherence of E. coli to epithelial cells,19 but a benefit has not yet been demonstrated in frail older people.
Arguably, the most important step in preventing unnecessary UTI is through limiting the use of urinary catheters. There is evidence that they are frequently used inappropriately in older people and are associated with adverse outcomes, including longer lengths of hospital stay and higher mortality rates.20 There is no convincing evidence that a particular catheter design is associated with a lower frequency of UTI.21
Conclusions
Older people are frequently diagnosed as having a UTI. Unfortunately they often present with non-specific illnesses without urinary tract symptoms. This makes distinguishing a UTI from ASB challenging. Diagnosis depends on a comprehensive assessment rather than on a specific diagnostic test. Antibiotic use should be limited to the shortest effective duration with the narrowest spectrum agent. Urinary catheters should be inserted only when absolutely necessary and removed as soon as possible.
References
- 1.Ducharme J, Neilson S, Ginn JL. Can urine cultures and reagent test strips be used to diagnose urinary tract infection in elderly emergency department patients without focal urinary symptoms? CJEM. 2007;9:87–92. doi: 10.1017/s1481803500014846. [DOI] [PubMed] [Google Scholar]
- 2.Baldassarre JS, Kaye D. Special problems of urinary tract infection in the elderly. Med Clin N Am. 1991;75:375–90. doi: 10.1016/s0025-7125(16)30460-6. [DOI] [PubMed] [Google Scholar]
- 3.Nicolle LE. Urinary infections in the elderly: symptomatic or asymptomatic? Int J Antimicrob Agents. 1999;11:265–8. doi: 10.1016/S0924-8579(99)00028-X. [DOI] [PubMed] [Google Scholar]
- 4.Scottish Intercollegiate Guideline Network (SIGN) Management of suspected bacterial urinary tract infection in adults. Guideline 88. 2006. www.sign.ac.uk/pdf/sign88.pdf. [Google Scholar]
- 5.Nicolle LE, Mayhew WJ, Bryan L. Prospective randomized comparison of therapy and no therapy for asymptomatic bacteriuria in institutionalized elderly women. Am J Med. 1987;83:27–33. doi: 10.1016/0002-9343(87)90493-1. [DOI] [PubMed] [Google Scholar]
- 6.Abrutyn E, Berlin J, Mossey J, et al. Does treatment of asymptomatic bacteriuria in older ambulatory women reduce subsequent symptoms of urinary tract infection? J Am Geriatr Soc. 1996;44:293–5. doi: 10.1111/j.1532-5415.1996.tb00917.x. [DOI] [PubMed] [Google Scholar]
- 7.Barkham TM, Martin FC, Eykyn SJ. Delay in the diagnosis of bacteraemic urinary tract infection in elderly patients. Age Ageing. 1996;25:130–2. doi: 10.1093/ageing/25.2.130. [DOI] [PubMed] [Google Scholar]
- 8.Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J Am Geriatr Soc. 2009;57:107–14. doi: 10.1111/j.1532-5415.2008.02073.x. [DOI] [PubMed] [Google Scholar]
- 9.Ronald A. The etiology of urinary tract infection: traditional and emerging pathogens. Am J Med. 2002;113(Suppl 1A):14S–19S. doi: 10.1016/s0002-9343(02)01055-0. [DOI] [PubMed] [Google Scholar]
- 10.Ouslander JG, Schapira M, Fingold S, Schnelle J. Accuracy of rapid urine screening tests among incontinent nursing home residents with asymptomatic bacteriuria. J Am Geriatr Soc. 1995;43:772–5. doi: 10.1111/j.1532-5415.1995.tb07048.x. [DOI] [PubMed] [Google Scholar]
- 11.McGeer A, Campbell B, Emori TG, et al. Definitions of infection for surveillance in long-term care facilities. Am J Infect Control. 1991;19:1–7. doi: 10.1016/0196-6553(91)90154-5. [DOI] [PubMed] [Google Scholar]
- 12.Loeb M, Brazil K, Lohfeld L, et al. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: cluster randomised controlled trial. BMJ. 2005;331:669. doi: 10.1136/bmj.38602.586343.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Juthani-Mehta M, Tinetti M, Perrelli E, et al. Diagnostic accuracy of criteria for urinary tract infection in a cohort of nursing home residents. J Am Geriatr Soc. 2007;55:1072–7. doi: 10.1111/j.1532-5415.2007.01217.x. [DOI] [PubMed] [Google Scholar]
- 14.Woodford HJ. Essential geriatrics. 2nd edn. Oxford: Radcliffe Publishing; 2010. [Google Scholar]
- 15.Wright SW, Wrenn KD, Haynes M, Haas DW. Prevalence and risk factors for multidrug resistant uropathogens in ED patients. Am J Emerg Med. 2000;18:143–6. doi: 10.1016/S0735-6757(00)90005-6. [DOI] [PubMed] [Google Scholar]
- 16.Vogel T, Verreault R, Gourdeau M, et al. Optimal duration of antibiotic therapy for uncomplicated urinary tract infection in older women: a double-blind randomized controlled trial. CMAJ. 2004;170:469–73. [PMC free article] [PubMed] [Google Scholar]
- 17.Raz R, Schiller D, Nicolle LE. Chronic indwelling catheter replacement before antimicrobial therapy for symptomatic urinary tract infection. J Urol. 2000;164:1254–8. [PubMed] [Google Scholar]
- 18.Albert X, Huertas I, Pereiró I, et al. Antibiotics for preventing recurrent urinary tract infection in non-pregnant women. Cochrane Database Syst Rev. 2004;3:CD001209. doi: 10.1002/14651858.CD001209.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McMurdo ME, Argo I, Phillips G, Daly F, Davey P. Cranberry or trimethoprim for the prevention of recurrent urinary tract infections? A randomized controlled trial in older women. J Antimicrob Chemother. 2009;63:389–95. doi: 10.1093/jac/dkn489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holroyd-Leduc JM, Sen S, Bertenthal D, et al. The relationship of indwelling urinary catheters to death, length of hospital stay, functional decline, and nursing home admission in hospitalized older medical patients. J Am Geriatr Soc. 2007;55:227–33. doi: 10.1111/j.1532-5415.2007.01064.x. [DOI] [PubMed] [Google Scholar]
- 21.Jahn P, Preuss M, Kernig A, Seifert-Hühmer A, Langer G. Types of indwelling urinary catheters for long-term bladder drainage in adults. Cochrane Database Syst Rev. 2007;3:004997. doi: 10.1002/14651858.CD004997.pub2. [DOI] [PubMed] [Google Scholar]