Abstract
Introduction
Recent payment reforms promote movement from fee-for-service to alternative payment models that shift financial risk from payers to providers, incentivizing providers to manage patients’ utilization. Bundled payment, an episode-based fixed payment that includes the prices of a group of services that would typically treat an episode of care, is expanding in the United States, including mandatory models in Medicare. Bundled payment has not been developed specifically for substance use disorder (SUD) treatment. Yet, bundled payment has been recommended as a way to pay for comprehensive SUD treatment and has the potential to improve treatment engagement after detox, which could reduce detox readmissions, improve health outcomes, and reduce medical care costs. However, if moving to bundled payment creates large losses for some providers, it may not be sustainable. The objective of this study was to design a bundled payment for detox and follow-up care and to estimate its impact on provider revenues.
Methods
Massachusetts Medicaid beneficiaries’ behavioral health, medical, and pharmacy claims from July 2010–April 2013 were used to build and test a detox bundled payment for continuously enrolled adults (N=5,521). A risk adjustment model was developed using general linear modeling to predict beneficiaries’ episode costs. The projected payments to each provider from the risk adjustment analysis were compared to the observed baseline costs to determine the potential impact of a detox bundled payment reform on organizational revenues. This was modeled in two ways: first assuming no change in behavior and then assuming a supply-side cost sharing behavioral response of a 10% reduction in detox services and an increase of one individual counseling and one group counseling session.
Results
The mean total 90-day detox episode cost was $3,743. Nearly 70 percent of the total mean cost consists of the index detox, psychiatric inpatient care, and short-term residential care. Risk mitigation, including risk adjustment, substantially reduced the variation of the mean episode cost. There are opportunities for organizations to gain revenue under this bundled payment design, but many providers will lose money under a bundled payment designed using historic payment and costs.
Conclusions
Designing a bundled payment for detox and follow-up care is feasible, but low case volume and the adequacy of the payment are concerns. Thus, a detox episode-based payment will likely be more challenging for smaller, independent SUD treatment providers. These providers are experiencing many changes as financing shifts away from block grant funding toward Medicaid funding. A detox bundled payment in practice would need to consider different risk mitigation strategies, pooling providers, and an increased reimbursement rate, but could incentivize care coordination, which is important to reducing detox readmissions and engaging patients in care.
Keywords: Bundled payment, provider payment, care coordination, substance use disorders, detox, health care reform
1. Introduction
Nearly 12 percent of Medicaid beneficiaries over age 18 have a substance use disorder (SUD) (Center for Behavioral Health Statistics and Quality, 2014), and 14 percent of newly eligible low-income adults have a substance use disorder (SUD) (Mark, Wier, Malone, Penne, & Cowell, 2015). Over a fifth of annual admissions to SUD treatment are for detox (Center for Behavioral Health Statistics and Quality, 2014). Studies have shown that continuity of care after detox is associated with better outcomes, including reduced detox readmission (Lee et al., 2014; Mark, Vandivort-Warren, & Montejano, 2006). However, many receiving detox services do not receive follow-up treatment. For example, Carrier et al. found 52% of all patients admitted to New York state-certified treatment centers between January 1, 2007 and June 30, 2997 did not obtain aftercare within 6 months of detox (2011). Similarly, a study using employer health insurance claims showed that only 49.4% of detox episodes were followed by continuing care within 30 days of discharge (Mark, Dilonardo, Chalk, & Coffey, 2003).
Fee-for-service (FFS) is the dominant approach to paying SUD treatment providers. While FFS encourages acceptance of higher severity patients, such as individuals with co-occurring SUD and mental and physical health problems, it can discourage coordination between providers (Robinson, 2001). A payment that bundles detox and follow-up care together has the potential to improve engagement in treatment after detox, which could reduce detox readmissions, improve health outcomes, and reduce medical care costs. However, if this type of payment creates large losses for some providers, it could be unsustainable and lead to unintended consequences.
The Affordable Care Act (ACA) and many states’ health care reforms have sought to foster the implementation of new ways to pay health care providers to drive delivery system innovations and improvements in patients’ health and health care. These payment reforms move away from FFS to alternative models that shift financial risk from payers to providers, incentivizing providers to manage patients’ utilization. New payment models attempt to correct for inefficiencies of FFS and capitation and emphasize efficiency and coordination between providers.
Bundled payment, a fixed payment that includes the prices of a group of services that would typically treat an episode of care in a defined period of time, is considered one of the most promising new payment models (Hussey, Eibner, Ridgely, & McGlynn, 2009; Mechanic & Altman, 2009). Bundled payment is more comprehensive than other episode-based approaches such as case rates and diagnostic-related group payment because it can include hospital, physician, and other clinical services in a single rate, as well as services delivered at different health care organizations. Nationally, Medicare (Centers for Medicare and Medicaid Services, 2014), Medicaid, and private payers have tested bundled payment models. The predominant Medicare bundled payment model works by establishing a target price based on historical Medicare payments for a defined episode, which includes services provided 72 hours prior to hospital admission, the inpatient hospital stay, and services during the 90-day post-acute period (e.g., rehab, skilled nursing facilities, home health, physical therapy, readmissions, drugs) (Iorio et al., 2016). Medicare retrospectively reconciles payment for all services from all providers in the episode to determine if total actual payments were more or less than the target price.
Bundled payment is an example of supply-side cost sharing, which shifts the financial risk for health care costs from insurers to providers. Under traditional payment models, the provider organization would have been reimbursed for each service provided. By accepting bundled payment, provider organizations bear the marginal cost for additional days and services provided beyond services in the bundle. A range of outcomes of supply-side cost sharing can be measured, referred to as “behavioral responses.” For acute care providers, predicted behavioral responses in the literature include premature discharge and inpatient/outpatient substitution (Harrow & Ellis, 1992). A potential unintended consequence of bundled payments is providers increasing the number of bundles in order to make more money, basically recreating FFS where the bundle is the service (Weeks, Rauh, Wadsworth, & Weinstein, 2013).
Bundled payment for surgical procedures has been found to reduce costs without decreasing quality (Dummit, Kahvecioglu, Marrufo, & et al., 2016) and reduce inpatient costs, readmissions, and length of stay (Iorio et al.). Bundled payment implementation (Hussey, Ridgely, & Rosenthal, 2011; Ridgely, De Vries, Bozic, & Hussey, 2014) and the design of bundled payment models for chronic care (O’Byrne et al., 2013) has been challenging, though a bundled payment for diabetes care in the Netherlands did lead to improved care coordination (de Bakker et al., 2012).
Bundled payment has not yet been developed specifically for specialty SUD treatment services despite the burden of SUDs and the need for quality improvement in that sector. A new bundled payment model for Medication-Assisted Treatment (MAT) that includes counseling and prescription drugs is being implemented in Massachusetts (Open Minds, 2017). Drawing from Medicare’s bundled payment work, a bundled payment for detox care could include services immediately preceding detox, the detox stay, and services delivered in the post-detox period, which could include residential care, prescription drugs, counseling, and wraparound services. The objective of this study was to design a bundled payment that covered detox and continuing care, and to estimate the economic impact of the payment on SUD treatment programs.
2. Methods
2.1. Study Setting
This study was conducted as part of a research partnership with a managed care organization that the Massachusetts’ Medicaid program contracts with to manage behavioral health care for some of its beneficiaries. In 2014, 85,823 people in Massachusetts received SUD treatment services. Massachusetts residents receiving SUD treatment tend to be single, adult, white men (Bureau of Substance Abuse Services, 2014). The majority use alcohol and heroin, but the primary substance for which Massachusetts residents sought treatment in 2014 was heroin (Bureau of Substance Abuse Services, 2014). This contrasts with national data that indicate the most recent substance adults in the US sought treatment for was alcohol.
Sixty-four percent of Massachusetts Medicaid beneficiaries are enrolled in managed care. The managed care organization in this study served 27 percent (N=383,000) of Medicaid beneficiaries in 2014. For these beneficiaries, the state regulates the reimbursement rate for SUD services. Thirty-seven percent of beneficiaries are enrolled in one of five private managed care organizations. The remaining thirty-three percent of MassHealth beneficiaries are enrolled in FFS—these beneficiaries include some seniors, people with other coverage, and people who are institutionalized. (Massachusetts Medicaid Policy Institute and the Center for Health Law and Economics at University of Massachusetts Medical School, 2014)
2.2. Data
Detoxification bundled payment was developed using claims and insurance eligibility information from July 2010-April 2013, for Massachusetts Medicaid beneficiaries who were enrolled in both the state’s primary care case management program and a managed behavioral health program. The claims recorded beneficiaries’ use of medical, behavioral health (i.e., SUD and mental health), and pharmacy services. Medical claims data included information on the patient, provider, diagnosis, procedure codes, and type of service provided. Behavioral health claims included the same information as medical claims, but more detail on behavioral health care services, and they contained only one diagnosis code per claim line. The pharmacy claims included each prescription filled, the National Drug Code, quantity, strength, date filled, and days supplied, in addition to other variables.
For the initial design work, data from July 2010-April 2013 were used. For risk adjustment modeling, a period 6 months prior to an index service was used to predict total episode costs. Because of this six-month lag, the total episode costs predicted by the risk adjustment model represent the cost of episodes initiated between February 1, 2011 and April 8, 2013.
2.3. Description of Population and Samples
During the study period, 1,143,528 individuals were enrolled in the behavioral health managed care plan. There were a total of 211,531 beneficiaries who used behavioral health services, of whom 69,732 were continuously enrolled during the study period. Bundled payment design and impact analyses were conducted using only continuously enrolled adult beneficiaries to ensure adequate data for each beneficiary would be available. Adolescent and child beneficiaries were excluded because of the different service mix they use. Table 1 presents descriptive characteristics of all continuously enrolled enrollees and the subset who had a detox episode. The majority of the detox sample were men ages 31–50, and 56% of the sample had drug-related disorders. Twenty percent had a prescription for medication for their SUD and 57 percent had at least one emergency department (ED) visit. Over a quarter had mood disorders and eight percent had chronic hepatitis in the 6 months prior to the trigger detox service.
Table 1.
Sample descriptionsa
| All Continuously Enrolled Beneficiariesb | Adult Beneficiaries with Detox Episodesc | |||
|---|---|---|---|---|
| N= | 69,732 | N= | 5521 | |
| N | % | N | % | |
| Age | ||||
| <21 years | 27557 | 40% | 193 | 3% |
| 21–30 years | 8752 | 13% | 1206 | 22% |
| 31–50 years | 19848 | 28% | 3049 | 55% |
| 51+ years | 13540 | 19% | 1070 | 19% |
| Sex | ||||
| Female | 35158 | 50% | 1912 | 35% |
| Male | 34270 | 49% | 3595 | 65% |
| Member Rating Category | ||||
| Disabled | 29780 | 43% | 1996 | 36% |
| Families | 29716 | 43% | 829 | 15% |
| Basic | 3102 | 4% | 867 | 16% |
| Essential | 7091 | 10% | 1829 | 33% |
| Diagnostic Category | ||||
| Alcohol-related disorders | 2959 | 4% | 1787 | 32% |
| Drug-related disorders | 6477 | 9% | 3094 | 56% |
| Mental health-related disorders | 60296 | 86% | 640 | 12% |
| Temporary Assistance for Needy Families Recipient | 30072 | 43% | 832 | 15% |
| Department of Children and Families Member | 4382 | 6% | 142 | 3% |
| Department of Mental Health Member | 6999 | 10% | 84 | 2% |
| Medication Assisted Treatment Prescription in 6-months prior to index detox | - | 1105 | 20% | |
| Emergency Department visit in 6-months prior to index detox | - | 3133 | 57% | |
| Behavioral Health Diagnoses in 6-months prior to index detoxd | ||||
| Mood Disorders | - | 1484 | 27% | |
| Drug Dependence | - | 1441 | 26% | |
| Adjustment Reaction | - | 477 | 9% | |
| Other Depression | - | 473 | 9% | |
| Alcohol Dependence | - | 426 | 8% | |
| Othere | - | 961 | 17% | |
| Medical Diagnoses in 6-months prior to index detoxf | ||||
| Chronic Hepatitis | - | 451 | 8% | |
| Seizure Disorders and Convulsions | - | 308 | 6% | |
| Chronic Obstructive Pulmonary Disease | - | 281 | 5% | |
| Diabetes without Complications | - | 256 | 5% | |
| HIV/AIDS | - | 163 | 3% | |
| Otherg | - | 1313 | 24% | |
Missing less than 1% not shown
Prescription, emergency, and behavioral and medical diagnosis in 6 months prior to index detox not available sample
Only includes first detox for clients with multiple detox episodes
Behavioral health diagnoses are 3-digit ICD-9 diagnostic codes from behavioral health claims; only one diagnosis per claim
Includes alcohol psychoses, drug psychoses, non-dependent drug use, transient organic psychotic conditions, schizophrenia, other nonorganic psychoses, neurotic disorders, disturbance of conduct, disturbance of emotions specific to childhood and adolescence, and hyperkinetic syndrome of childhood
Medical diagnoses are HCC codes from medical claims
Includes: Septicemia, cancer, diabetes with complications, malnutrition, end-stage liver disease, cirrhosis, intestinal obstruction/perforation, pancreatic disease, inflammatory bowel disease, bone/joint muscle infections/necrosis, rheumatoid arthritis and inflammatory connective tissue disease, severe hematological disorders, polyneuropathy, cardio-respiratory failure and shock, congestive heart failure, unstable angina and other acute ischemic heart disease, angina pectoris/old myocardial infarction, specified heart arrhythmias, cerebral hemorrhage, ischemic or unspecified stroke, vascular disease with and without complications, aspiration and specified bacterial pneumonias, renal failure, chronic ulcer of skin, major head injury
2.4. Bundled payment design overview and provider attribution
To create episodes, individual beneficiary claims for detox stays and other substance use disorder and mental health treatment services were aggregated to create an episode-level data set. First, all detox stays were identified by member number, provider number, service start date, and service end date. Beneficiaries’ claims for behavioral health services following a detox stay within a specific length of time (see Section 2.5.3) were identified and grouped into categories. The costs of each category and the total episode of care were then computed, including the following service settings: index detox, detox readmissions, psychiatric inpatient, emergency behavioral health services, community support provider, short-term residential, individual and family counseling, group counseling, structured outpatient addictions program, provider case consultation, and other (services to divert patients from inpatient and residential services, other outpatient services, and inpatient hospital administrative charges while waiting for transfer to another level of care). These cost figures were based on insurer payments, and a provider organization’s actual cost of providing care may be different than the amount reimbursed.
A beneficiaries’ full episode of care was attributed to the index detox provider organization, even if the index detox provider did not deliver services following the index detox. Index detox providers were categorized by the range of services they offer: Detox only, Detox+Outpatient, and Outpatient only. Index Outpatient-only providers offered outpatient detox services. Index providers could have offered services beyond detox and outpatient; however, these services were considered most critical to a detox bundled payment with the goal of improving continuity of care.
2.5. Design Dimensions
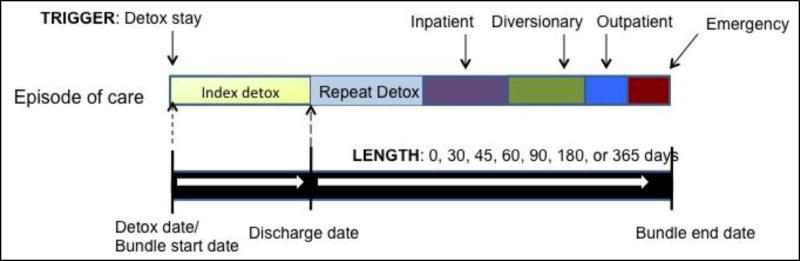
There are a number of key dimensions in bundled payment design: (1) diagnostic specificity, (2) what event triggers the bundled payment, (3) the length of time the payment covers, and (4) service or other exclusions. These dimensions are discussed below. The final design selected is presented in Error! Reference source not found.
2.5.1. Diagnostic specificity
A set of potential episode definitions was considered for development: (1) alcohol use disorders, (2) drug use disorders, and (3) an all-in model that included all diagnoses. It was determined that the detox bundled payment would include all diagnoses because otherwise providers would have incentives to miscode diagnoses, and because many detox claims had only mental health diagnoses associated with them. The ICD-9 five-digit diagnostic code for the index service was used to identify the diagnostic category of the bundled payment (i.e., alcohol-related, drug-related, or mental health).
2.5.2. Trigger
Because the aim of this study was to design a detox bundled payment, it was determined that the trigger service for a detox episode is a detox service in a specialty addiction treatment setting. Review of the claims data showed there were few inpatient hospital detox services. Detox services for the same client within the episode length were considered readmissions, not an episode trigger. The next detox to occur outside of the episode length would initiate a new episode.
2.5.3.. Length
Detox bundled payment for 0-, 30-, 45-, 60-, 90-, 180-, and 365-days were tested. A 0-day bundle represents the costs of the index detox only. For each trigger detox admission identified, the costs of other services for that beneficiary within the episode length were computed. Results from the 90-day design are presented here. 90 days was selected to facilitate comparisons with designs in Medicare’s Bundled Payment for Care Improvement initiative.
2.5.4. Exclusions
Methadone services were excluded because dosing and counseling visits were already bundled in the program we studied.
2.5. Risk Mitigation
Risk adjustment and other risk mitigation strategies are important to include in alternative payment models to minimize probability risk and provider avoidance of patients with SUDs (Ettner, Frank, Mark, & Smith, 2000; Ettner, Frank, McGuire, & Hermann, 2001; Hermann, Rollins, & Chan, 2007). Risk mitigation protects provider organizations from the random, high cost cases that put providers at risk of not breaking even on a per-case basis.
Winsorization is a technique to trim outliers, thus reducing the variation of the bundled payment cost estimates and offering providers “stop-loss” protection against outlier costs. Bundled payment estimates for which the total cost was in the bottom 5 percent of the total cost distribution were truncated at the 5th percentile. On the high end, estimates in the top 5 percent of the total cost distribution were truncated at the 95th percentile plus 20 percent of the observed cost.
Risk adjustment incorporates adjustments for patient and provider characteristics into the estimation of the bundled payment costs/price. A risk adjustment model was developed using regression analysis to predict beneficiaries’ episode costs. General linear modeling (GLM) was used to predict total bundled payment cost. For skewed data like payments, GLM has been recommended as a risk adjustment modeling approach instead of Ordinary Least Squares analysis and data transformations (Blough, Madden, & Hornbrook, 1999; Manning, Basu, & Mullahy, 2005). GLM involves minimal assumptions, does not require transforming data, and the parameter estimates retain the original scale, which facilitates interpretation (Blough et al., 1999).
To identify the optimal model, an approach similar to Ettner et al., 1998 was used. Three models were evaluated. The first (DEM) includes only member and episode of care characteristics as explanatory variables, including age, gender, index detox diagnosis (e.g., alcohol, drug, or mental health), provider region, member rating category (i.e., if member was eligible for Medicaid as disabled, family, basic, or essential beneficiary), and participation in other state and social assistance programs (i.e., Department of Children and Families (DCF), Department of Mental Health (DMH), and Temporary Assistance for Needy Families (TANF)). The second (BH) adds behavioral health diagnoses in the 6 months prior to the index service. The third (MED) adds a SUD medication use indicator and indicators for various general health diagnoses in the 6 months prior to the index service. Diagnostic indicators that applied to fewer than 30 observations were omitted.
2.6. Organizational revenue impact estimates
In order to assess how a bundled payment reform would affect organizational revenues, beneficiary-level observed and predicted episode costs were aggregated at the organization-level. It was assumed that the index provider organization would be paid a bundled payment equal to the mean predicted (i.e., risk-adjusted and winsorized) episode cost for each case. The amount included all services covered under the bundled payment regardless of whether the index provider organization offered the service. For each index detox organization, the mean observed baseline episode costs for all cases was subtracted from the mean predicted costs to determine the impact on providers. This initial analysis assumed no behavioral response to payment change. More realistically, provider organizations would be expected to change their behavior under bundled payment. We therefore also estimated revenues in the event of a supply-side cost sharing behavioral response: a 10% reduction in detox readmission service costs and an increase of one individual counseling and one group counseling session. A reduction in detox services would be a likely response to the introduction of supply side cost sharing (Ellis & McGuire, 1993). A 10% reduction was assumed. An increase of outpatient services would also be likely under the bundled payment because engagement in outpatient care can reduce detox readmissions, which providers would want to avoid because a readmission would not initiate a new payment. An increase of one individual and one group counseling session was assumed because an individual and group counselling session has been found to be an effective psychosocial SUD treatment approach (Crits-Christoph, Siqueland, Blaine, & et al., 1999). Detox readmission costs were subtracted from, and counseling costs added to, the observed total episode cost to represent an organization’s costs with a behavioral response. These estimates were then subtracted from the predicted costs as in the initial analysis. Organizational revenue total dollar and percent impacts were estimated, separately for Detox only, Detox+Outpatient, and Outpatient only organizations.
3. Results
3.1. Overall mean total costs and costs by setting for different lengths
During the study period, there were 18,869 detox stays with a mean length of 4.3 days. As the length of the episode increases, the number of cases decreases and mean total episode costs increase. For example, the 0-day episode costs, on average, $1,462 while the 60-day is twice as expensive at $3,190 and the 365-day is almost five-times as expensive at $7,171. The decrease in case volume as episode length increases is driven by an increase in the number of detox stays being classified as readmissions within the same episode rather than as index stays. (Data not shown)
3.2. 90-day detox episode costs and service use
There were 9,247 90-day detox episodes during the study period. The mean number of readmissions per episode was 0.8. No specific SUD treatment service other than an index detox was included in more than half of the 90-day detox episodes. Twenty percent of episodes had detox readmissions with the 90-day period. Each readmission has a mean cost of $1,275. The mean number of readmissions for episodes with readmissions was 3.8. (Data not shown)
The total 90-day detox episode cost is, on average, $3,743. Nearly 70 percent of the total mean cost consists of the index stay, inpatient, and short-term residential care (known in Massachusetts as “Clinical Support Services”). Total costs and costs by service setting for a 90-day detox episode are presented in Table 2, including breakouts by primary diagnosis at index detox and provider organization type.
Table 2.
90-day detox episode mean total costs and service setting costs by index diagnosis and provider type
| Number of Episodes | Total Episodes Cost | Index detox | Detox readmissions | Psychiatric Inpatient | Emergency
Behavioral Health Services |
Community
Support Provider |
Short-term
Residential (Clinical Support Services) |
Individual and
Family Counseling |
Group counseling | Structured
Outpatient Addictions Program |
Provider Case Consultation | Othera | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| $ | % | $ | % | $ | % | $ | % | $ | % | $ | % | $ | % | $ | % | $ | % | $ | % | $ | % | |||
| Total | 9247 | $3,743 | $1,290 | 34% | $258 | 7% | $766 | 20% | $192 | 5% | $181 | 5% | $515 | 14% | $86 | 2% | $8 | 0% | $235 | 6% | $3 | 0% | $207 | 5% |
| Diagnostic Categoryb | ||||||||||||||||||||||||
| Alcohol-Related Disorders | 3002 | $3,515 | $1,034 | 29% | $194 | 6% | $737 | 21% | $219 | 6% | $177 | 5% | $554 | 16% | $92 | 3% | $9 | 0% | $283 | 8% | $3 | 0% | $212 | 6% |
| Drug- Related Disorders | 5228 | $3,207 | $1,291 | 40% | $282 | 9% | $497 | 15% | $139 | 4% | $140 | 4% | $406 | 13% | $72 | 2% | $7 | 0% | $201 | 6% | $3 | 0% | $169 | 5% |
| Mental Health Disorders | 1017 | $7,172 | $2,038 | 28% | $326 | 5% | $2,236 | 31% | $382 | 5% | $409 | 6% | $966 | 13% | $140 | 2% | $10 | 0% | $271 | 4% | $4 | 0% | $390 | 5% |
| Index Provider Organization Type | ||||||||||||||||||||||||
| Detox | 714 | $5,629 | $1,779 | 32% | $309 | 5% | $1,715 | 30% | $399 | 7% | $223 | 4% | $383 | 7% | $123 | 2% | $6 | 0% | $300 | 5% | $3 | 0% | $390 | 7% |
| Detox + Outpatient | 8451 | $3,597 | $1,253 | 35% | $254 | 7% | $690 | 19% | $175 | 5% | $179 | 5% | $529 | 15% | $83 | 2% | $8 | 0% | $231 | 6% | $3 | 0% | $193 | 5% |
| Outpatient | 82 | $2,327 | $912 | 39% | $241 | 10% | $422 | 18% | $145 | 6% | $19 | 1% | $286 | 12% | $100 | 4% | $0 | 0% | $134 | 6% | $4 | 0% | $64 | 3% |
Includes services to divert patients from inpatient and residential services, other outpatient services, and inpatient hospital administrative charges while waiting for transfer to another level of care
Primary diagnosis of index detox service. Category defined using ICD-9 code: Alcohol-related diagnoses (2910, 2911, 2912, 2913, 29181, 29189, 2919, 30300, 30301, 30302, 30390, 30391, 30392, 30500, 30501, 30502); Drug-related diagnoses (2920, 29211, 29212, 29281, 29284, 29289, 2929, 30400, 30401, 30402, 30403,30410, 30411, 30420, 30421, 30423, 30430, 30431, 30440, 30450, 30460, 30461, 30470, 30471, 30472, 30473, 30480, 30481, 30490, 30520, 30540, 30541, 30542, 30550, 30551, 30552, 30560, 30563, 30570, 30590, 30590, 30593); Mental Health-related diagnoses (all other diagnoses in behavioral health claims data)
Episodes where the principal diagnosis from the index detox was alcohol-related had a higher total, inpatient psychiatric, and short-term residential costs than drug-related episodes; however, their index detox and readmission costs were lower. Episodes where the principal diagnosis from the index detox was mental health-related, about 10 percent of all episodes, were more than twice as expensive as those with SUD diagnoses. The high cost of episodes with mental health diagnoses was driven by psychiatric inpatient utilization costs, which were 31 percent of the total cost.
3.3. Risk Mitigation
Winsorization and risk adjustment both substantially reduce the variation of the mean cost of episodes. Winsorization reduced the standard deviation of 90-day detox total mean cost from $4,476 to $3,400 (data not shown). Risk adjustment in this study involved predicting total cost of an episode as a function of specific member and provider characteristics from the 6-months prior to the index service and from the index service itself. As seen in Table 3, the basic demographic model (DEM) performed worst. The demographic model R2 values were around 0.16 for detox episodes. The MED model had a slightly higher predictive ability than the BH model, with R2 values around 0.24 for detox episodes.
Table 3.
Ability of models to predict total Winsorized episode cost
|
R2 if
episode length is: | |||||||
|---|---|---|---|---|---|---|---|
| Model | 0 | 30 | 45 | 60 | 90 | 180 | 365 |
| DEM | 0.24 | 0.17 | 0.16 | 0.16 | 0.16 | 0.15 | 0.15 |
| BH | 0.25 | 0.25 | 0.24 | 0.24 | 0.24 | 0.22 | 0.21 |
| MED | 0.25 | 0.25 | 0.24 | 0.25 | 0.25 | 0.23 | 0.23 |
Model specifications are as follows:
DEM: sex, age, age squared, diagnostic category, provider region, member rating category, state agency affiliations
BH: sex, age, age squared, diagnostic category, provider region, member rating category, state agency affiliations, behavioral health diagnoses
MED: sex, age, age squared, diagnostic category, provider region, member rating category, state agency affiliations, behavioral health diagnoses, SUD prescription, medical diagnoses
The risk adjusted mean total episode cost was $3,502. Table 4 presents the full set of parameter estimates from the MED model for 90-day detox episodes. The parameter estimates represent dollars. The detox model implies that the episode price when all risk adjusters were equal to 0 would be $5,416. 90-day detox episode costs would be significantly increased by any of the following: an increase in age; index provider located in Boston and the metro area, Central Massachusetts, and the Southeast compared to Western Massachusetts; being a DCF and DMH member; having an SUD prescription; prior mental health and SUD diagnoses; and intestinal obstruction/perforation, seizure disorders and convulsions, and angina. Having an alcohol- or drug-related disorder diagnosis at the index service compared to having a mental health diagnosis, having diabetes with ophthalmologic or unspecified manifestations, and having end-stage liver disease significantly reduced detox episode costs. Member rating category and many of the medical diagnoses did not significantly impact total episode costs.
Table 4.
Parameter Estimates for Model for 90-day Detox Total Winsorized Episode Costs
| N=9218 DF=63, F<.0001, R2=0.25 |
|||||
|---|---|---|---|---|---|
| Impact on Bundle Costa |
β | SE | p | ||
| Intercept | N/A | 5416.31 | 387.57 | <.0001 | |
| Index Service | Age | + | −47.09 | 17.02 | 0.0057 |
| Age2 | 0.36 | 0.20 | 0.0717 | ||
| Female | −49.74 | 70.15 | 0.4783 | ||
| Diagnostic Category | |||||
| Alcohol-Related Disorder Diagnosis at Index | − | −2303.07 | 120.36 | <.0001 | |
| Drug-Related Disorder Diagnosis at Index | − | −2503.89 | 116.75 | <.0001 | |
| Mental Health Disorder Diagnosis at Index | Reference group | ||||
| Provider Region | |||||
| Boston | + | 370.63 | 128.51 | 0.0039 | |
| Central Massachusetts | + | 414.41 | 132.24 | 0.0017 | |
| Metro-Boston | + | 615.39 | 207.68 | 0.0031 | |
| Northeast | 223.30 | 116.77 | 0.0559 | ||
| Southeast | + | 980.46 | 119.11 | <.0001 | |
| Western Massachusetts | Reference group | ||||
| Member Rating Category | |||||
| Disabled | −155.69 | 82.73 | 0.0599 | ||
| Families | 130.43 | 164.80 | 0.4287 | ||
| Basic | 123.08 | 92.13 | 0.1816 | ||
| Essential | Reference group | ||||
| 6 months prior to index | Department of Children and Families Member | + | 1983.55 | 223.60 | <.0001 |
| Department of Mental Health Member | + | 2499.13 | 332.06 | <.0001 | |
| Temporary Assistance for Needy Families Recipient | −98.56 | 180.41 | 0.5849 | ||
| SUD Prescription | + | 461.17 | 76.40 | <.0001 | |
| Behavioral Health Diagnosesb | |||||
| Alcohol Dependence | + | 518.71 | 93.20 | <.0001 | |
| Drug Dependence | + | 406.19 | 68.64 | <.0001 | |
| Drug Psychoses | + | 1891.54 | 238.65 | <.0001 | |
| Schizophrenia | + | 2328.24 | 210.74 | <.0001 | |
| Mood Disorders | + | 753.45 | 73.86 | <.0001 | |
| Other nonorganic psychoses | + | 1658.13 | 294.08 | <.0001 | |
| Adjustment Reaction | + | 829.50 | 105.82 | <.0001 | |
| Other Depression | + | 1131.04 | 101.02 | <.0001 | |
| Disturbance of Emotions specific to childhood and adolescence | + | 2106.85 | 531.46 | <.0001 | |
| Hyperkinetic Syndrome of childhood | + | 559.24 | 238.21 | 0.0189 | |
| Medical Diagnosesc | |||||
| Diabetes with Ophthalmologic or Unspecified Manifestations | − | −1168.460984 | 557.3587615 | 0.03 61 | |
| End-Stage Liver Disease | − | −887.98 | 418.74 | 0.034 | |
| Intestinal Obstruction/Perforation | + | 1222.73 | 469.04 | 0.0092 | |
| Seizure Disorders and Convulsions | + | 447.28 | 130.68 | 0.0006 | |
| Angina Pectoris/Old Myocardial Infarction | + | 702.86 | 323.00 | 0.0296 | |
Direction of impact only shown for significant parameters
Only significant behavioral health diagnoses in prior 6 months shown. The following diagnoses were included in the model but were not significant and not shown: non-dependent drug use, transient organic psychotic conditions, neurotic disorders, disturbance of conduct
Only significant medical diagnoses in prior 6 months shown. The following diagnoses were included in the model but were not significant and not shown: HIV/AIDS, septicemia, cancers, diabetes with neurologic or other specified manifestations, diabetes without complications, malnutrition, cirrhosis, chronic hepatitis, pancreatic disease, inflammatory bowel disease, bone/joint muscle infections/necrosis, rheumatoid arthritis and inflammatory connective tissue disease, severe hematological disorders, polyneuropathy, cardio-respiratory failure and shock, congestive heart failure, unstable angina and other acute ischemic heart disease, specified heart arrhythmias, cerebral hemorrhage, ischemic or unspecified stroke, vascular disease with and without complications, chronic obstructive pulmonary disease, aspiration and specified bacterial pneumonias, renal failure, chronic ulcer of skin, major head injury
3.4. Detox Bundled Payment Gains and Losses
Table 5 presents the variation in providers’ projected gains and losses under 90-day detox bundled payment by case volume (less than 100, 100–249, 250–499, and more than 500), under two scenarios. First, assuming no change in utilization. Second, after allowing for a behavioral response by providers: a 10 percent decrease in detox readmission costs and an increase in one individual and one group counseling session.
Table 5.
Gains and Losses by Organization Case Volume under 90-day Detox Bundled Payment without and with response of 10% Readmission Reduction and Increase in Outpatient Services
| No Response | With Response | No Response | With Response | No Response | With Response | No Response | With Response | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Less than 100 | Less than 100 | 100 – 249 | 100 – 249 | 250 – 499 | 250 – 499 | More than 500 | More than 500 | |||||||||
| $ | % | $ | % | $ | % | $ | % | $ | % | $ | % | $ | % | $ | % | |
| All Providers | N=2 | N=2 | N=3 | N=3 | N=6 | N=6 | N=6 | N=6 | ||||||||
| Top 25% | $26,806.30 | 10% | $21,334.73 | 8% | $192,798.00 | 36% | $181,134.90 | 34% | $−52,898.60 | −6% | $−68,194.02 | −8% | $−125,214.10 | −4% | $−177,139.80 | −6% |
| Median | $19,435.00 | 8% | $14,546.89 | 6% | $1187.34 | 0% | $−7,384.20 | −2% | $−127,444.60 | −11% | $−147,041.00 | −12% | $−165,510.70 | −5% | $−216,382.30 | −6% |
| Bottom 25% | $12,063.70 | 6% | $7,759.06 | 4% | $−141,609.51 | −9% | $−148,834.80 | −9% | $−261,130.90 | −14% | $−277,798.63 | −15% | $−396,102.50 | −6% | $−438,648.80 | −8% |
There are 17 organizations profiled in Table 5. Three are Detox-only organizations, 13 are Detox+Outpatient organizations, and one is an Outpatient-only organization (Data not shown). Outpatient-only organizations had the smallest case volume, while Detox+Outpatient organizations have higher case volume than other provider types.
3.4.1. Gains and losses under bundled payment
Assuming no behavioral response, providers with 100–249 cases could lose up to 9 percent of revenue or gain up to 36 percent. Providers that had 250–499 cases had less variation in their gains and losses—the impact ranged from −14 percent to −6 percent. All providers with more than 500 cases were Detox+Outpatient providers. While they all would be expected to lose money, there was the least amount of variation between the 25th and 75th percentile: −6 percent to −4 percent.
3.4.2. Gains and losses under bundled payment with potential behavioral responses
Assuming that organizations would reduce readmissions 10 percent and increase outpatient service utilization by one individual counseling visit and one group counseling visit, providers with the lowest case volume would gain 4–8 percent. Providers with 100–249 cases could lose up to 9 percent of revenue or gain up to 34 percent. Providers that had 250–499 cases had less variation in their gains and losses than those with 100–249 cases—the impact ranged from −15 percent to −8 percent. Providers with 500 or more cases (all Detox+Outpatient) would be expected to lose money, but had the least amount of variation: −8 percent to −6 percent.
4. Discussion
This study demonstrates the technical feasibility of bundled payment for detox and follow-up care and provides insights into what such a payment system could look like. Areas of high costs in the detox episode which may present opportunities for cost reduction are detox services, inpatient psychiatric services, and residential care. There appears to be a tradeoff between inpatient and residential services: episodes with high residential costs were often for SUD diagnoses and have lower inpatient costs while episodes with high inpatient costs were often for mental health diagnoses and have lower residential costs. Group therapy and provider case consultation were low cost services that accounted for a small share of costs within the episode. Investment in these services could yield savings from averted detox, inpatient, and residential services due to improved care coordination and quality. Connecting clients with other social services, like housing, could also be important. Housing can provide a stable place for clients to recover and could help reduce health care costs (Doran, Misa, & Shah, 2013).
Winsorization and risk adjustment appear to successfully reduce the variation of total episode costs. However, the historic cost of an episode of detox and follow-up care is low, likely because many clients who need follow-up care after detox do not receive it. Winsorization could be reconsidered to address these low costs. The bottom 25 percent could be considered the lower price limit rather than the bottom 5 percent. The most comprehensive risk adjustment model used explains as much variation in the outcome (total Winsorized episode cost) as the most successful behavioral health risk adjustment models in prior work (Hermann, Chan, Provost, & Chiu, 2006). The behavioral health model has only a slightly lower predictive ability than the medical model, which is a similar finding to prior research on risk adjustment modeling of mental health and substance abuse payments in private health plans (Ettner et al., 1998). This finding is significant because the additional variables in the medical model may not be readily available to behavioral health organizations.
In addition to these risk mitigation strategies, case volume also affects organizations’ risk and uncertainty. Organizations with higher case volume faced less variation in gains and losses on a per-case basis. However, they do face greater revenue risk as suggested by the results presented here that show as the variation decreases, the likelihood of losing money seems to increase. There are some potential explanations for this. First, the cost estimates for an episode of detox and follow-up care are low because few people received follow-up services. A bundled payment based not on historic costs but more on ideal costs that represents high quality care would likely be higher, offering providers a greater likelihood of gaining revenue. Further, the revenue estimates attributed observed and predicted episode costs to the index provider even if all services were not delivered by that provider. The small providers that appear to gain revenue under this payment model are likely not providing all of the services necessary for the episode of care and would need to subcontract other providers to do so, which would decrease their revenue. In contrast, the larger providers are likely to be providing many of the post-detox services and would not need to subcontract other providers.
Payers considering implementing an SUD bundled payment reform would want to consider their own goals, capabilities, and networks in addition to these results and supply-side cost sharing theory. Because a change in payment may not be sufficient to change care delivery, payers could consider including performance measures or additional incentives, such as a readmission penalty, or shared savings arrangements in order to support care delivery. As indicated by supply side cost sharing theory, a detox bundled payment creates a perverse incentive for more detox episodes. The length of the bundled payment could be redesigned to take the frequency of detox and repeat detox events into account to mitigate this perverse incentive.
Provider organizations would also face different risks and may respond differently if a bundled payment is paid prospectively or involves a retrospective reconciliation of a budget. If paid prospectively, index organizations would need to focus on paying other providers, but would be able to use upfront payments to offset necessary capital investments or staff salaries. If paid retrospectively, organizations would need to focus on care and cost management while communicating about utilization across organizations and still following traditional billing requirements. A prospective payment might be more effective in changing care delivery; however, it would require dramatic changes in relationships between provider organizations, selection of an accountable provider, and careful attribution of patients’ and their costs. Under Medicare’s Bundled Payment for Care Improvement initiative, hospitals were able to choose to participate in a prospective or retrospective model and very few selected the prospective model (Hirsch et al., 2015).
In addition to changing relationships with other SUD treatment organizations, under a bundled payment an organization may need to develop relationships with the general health care system and the SUD treatment system, if a general health care organization adopts this approach, and develop relationships between different divisions of one organization and/or across different organizations. Communication about clients’ utilization and outcomes would be important in these relationships, which may require implementing a standard procedure for releasing protected health information across organizations and state agencies. Formal agreements between organizations may also be important. For example, detox and outpatient organizations may want to establish agreements to jointly manage patients in a detox episode.
Organizations that offer a range of services may have advantages in implementing bundled payment because they are larger (i.e., less exposed to the risk of random variation of episode costs), can have a more coordinated response across different levels of care, and can capture savings from shifting care between settings. Conversely, SUD bundled payment would likely be more challenging for smaller, independent SUD treatment providers. These providers are experiencing many changes as their funding source shifts away from block grants toward Medicaid and would be exposed to more risk of random variation of episode costs under a bundled payment.
The study is subject to certain limitations. First, the data do not include the costs of all SUD treatment services that beneficiaries received during the study period, as the state substance abuse agency often pays for certain services that Medicaid does not cover, such as residential care. Not having the full picture of SUD treatment costs is a limitation. Second, the use of Massachusetts Medicaid data limits the generalizability of the results to other payers because Massachusetts regulates payment rates and covered services. However, the same methods could be used by other payers to estimate episode costs and design payment models. Third, assumptions made in these analyses could be reconsidered for future studies. Organizational revenue total dollar and percent impacts were estimated only for the index detox organization, which does not take into account the revenue effects of organizations offering follow-up services. These estimates also assumed a 10% reduction in detox services and increase in outpatient care across the board, while in reality, the reduction in detox may be lower and these responses could differ by organization type. Lastly, the risk mitigation methods to address high cost outliers and adjust bundled payment prices for patient and provider characteristics used in this paper could be reconsidered by payers in light of what information is available in their data, what the sources of risk are deemed beyond the control of providers (e.g., car accident), or what type of services or behaviors you want to incentivize (e.g., inpatient versus outpatient detoxification).
Yet, a strength of the study is the ability to use individual level data to estimate the cost of an episode of treatment as opposed to aggregate data on utilization and cost. The results of this study contribute knowledge of the feasibility of building bundled payment for the episodes of care detox and follow-up care and of the potential impact of bundled payment within the rapidly changing health care context. Even if they are not “ready-to-use” by all payers, the bundled payment model designed in this project is the first for acute and continuing specialty SUD treatment and has the potential to be used in health care practice and future research.
Future research could include refinements to this bundled payment design, particularly estimating costs of episodes of care that meet quality standards; bundled payment models that cover different SUD services; more advanced bundled payment simulations, and bundled payment reform implementation studies. In light of the opioid overdose epidemic, it may be valuable to design bundled payment models with the goal of improving treatment for people who use opioids, including initiating and adhering to medication assisted treatment (e.g., Open Minds, 2017). Services and service pathways for targeted sub-groups (e.g. adolescents) could be valuable to develop and may inform bundled payment designs. The implementation studies could consider the impact on certain populations, including homeless people, women, and people of color. Homelessness and race/ethnicity were not observable in these data.
If a detox bundled payment is implemented, it will be important to assess the effect of the new contracts and relationships that SUD treatment organizations develop. A study that used network analysis methods to examine the effect of interorganizational networks on SUD treatment outcomes found that as the number of network ties a detox facility had increased, the odds of readmission also increased (Spear, 2014). Other studies on detox readmissions found that larger programs (measured by number of beds) had higher readmission rates (Callaghan & Cunningham, 2002; Campbell et al., 2009). SUD treatment organizational characteristics also effect the integration of the SUD treatment system with mental health and public health systems (Guerrero, Aarons, & Palinkas, 2014). Future research could build off this study and this related research to examine the impact of organizational networks on SUD, medical, and other service integration.
Finally, the impact of bundled payment on health outcomes of individuals with SUDs is of great interest and concern. It is possible, for example, that a detox bundle be managed by primary care, not SUD treatment provider. Future research should focus on how SUD bundled payment and other delivery and payment reforms impact health outcomes and other measures of quality of care.
Figure 1.
Detox episode design
Highlights.
An episode-based payment for detox could improve treatment engagement after detox
Mean 90-day detox episode cost was $3,743, mean risk adjusted payment was $3,502
Nearly 70% of the total mean cost consists of detox, inpatient, residential
Some providers gain, but many lose revenue if payment based on low historic costs
Future research should consider different designs and models for MAT engagement
Acknowledgments
This study was supported by NIAAA F31AA023711.
The authors acknowledge the contributions of Stephanie Jordan Brown and Scott Taberner at the Massachusetts Executive Office of Health and Human Services and James Thatcher at Beacon Health Options for input on study development and interpretation; Christopher Tompkins for study design consultation; Pradipta Seal for statistical consultation; and Yuhua Boa at Weill Cornell Medical College for helpful comments on this work
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
The authors report no conflicts of interest.
References
- Blough DK, Madden CW, Hornbrook MC. Modeling risk using generalized linear models. Journal of Health Economics. 1999;18(2):153–171. doi: 10.1016/s0167-6296(98)00032-0. doi: http://dx.doi.org/10.1016/S0167-6296(98)00032-0. [DOI] [PubMed] [Google Scholar]
- Callaghan RC, Cunningham JA. Gender differences in detoxification: predictors of completion and re-admission. Journal of substance abuse treatment. 2002;23(4):399–407. doi: 10.1016/S0740-5472(02)00302-1. [DOI] [PubMed] [Google Scholar]
- Campbell BK, Tillotson CJ, Choi D, Bryant K, DiCenzo J, Provost SE, McCarty D. Predicting outpatient treatment entry following detoxification for injection drug use: The impact of patient and program factors. Journal of substance abuse treatment. 2009;38:S87–S96. doi: 10.1016/j.jsat.2009.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrier E, McNeely J, Lobach I, Tay S, Gourevitch MN, Raven MC. Factors Associated with Frequent Utilization of Crisis Substance Use Detoxification Services. Journal of Addictive Diseases. 2011;30(2):116–122. doi: 10.1080/10550887.2011.554776. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health: Model-Based Prevalence Estimates (50 States and the District of Columbia) 2014 Retrieved from http://www.samhsa.gov/data/sites/default/files/NSDUHStateEst2012-2013-p1/s/NSDUHsaePercents2013.pdf.
- Centers for Medicare and Medicaid Services. 2014). Bundled Payments for Care Improvement Initiative Fact Sheet. 2014 Jan 30; Retrieved from http://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-Sheets/2014-Fact-sheets-items/2014-01-30-2.html.
- Centers for Medicare and Medicaid Services. Episode Payment Models: General Information. 2017 Retrieved from https://innovation.cms.gov/initiatives/epm.
- de Bakker DH, Struijs JN, Baan CA, Raams J, de Wildt J-E, Vrijhoef HJM, Schut FT. Early Results From Adoption Of Bundled Payment For Diabetes Care In The Netherlands Show Improvement In Care Coordination. Health Affairs. 2012;31(2):426–433. doi: 10.1377/hlthaff.2011.0912. [DOI] [PubMed] [Google Scholar]
- Doran KM, Misa EJ, Shah NR. Housing as health care—New York’s boundary-crossing experiment. New England journal of medicine. 2013;369(25):2374–2377. doi: 10.1056/NEJMp1310121. [DOI] [PubMed] [Google Scholar]
- Dummit LA, Kahvecioglu D, Marrufo G, et al. ASsociation between hospital participation in a medicare bundled payment initiative and payments and quality outcomes for lower extremity joint replacement episodes. JAMA. 2016;316(12):1267–1278. doi: 10.1001/jama.2016.12717. [DOI] [PubMed] [Google Scholar]
- Ellis RP, McGuire TG. Supply-side and demand-side cost sharing in health care. The Journal of Economic Perspectives. 1993:135–151. doi: 10.1257/jep.7.4.135. [DOI] [PubMed] [Google Scholar]
- Ettner SL, Frank RG, Mark T, Smith MW. Risk adjustment of capitation payments to behavioral health care carve-outs: How well do existing methodologies account for psychiatric disability? Health Care Management Science. 2000;3(2):159–169. doi: 10.1023/a:1019033105715. [DOI] [PubMed] [Google Scholar]
- Ettner SL, Frank RG, McGuire T, Hermann RC. Risk adjustment alternatives in paying for behavioral health care under Medicaid. Health Services Research. 2001;36(4):793. [PMC free article] [PubMed] [Google Scholar]
- Ettner SL, Frank RG, McGuire TG, Newhouse JP, Notman EH. Risk Adjustment of Mental Health and Substance Abuse Payments. Inquiry. 1998;35(2):223–239. doi: 10.2307/29772757. [DOI] [PubMed] [Google Scholar]
- Guerrero EG, Aarons GA, Palinkas LA. Organizational Capacity for Service Integration in Community-Based Addiction Health Services. American Journal of Public Health. 2014;104(4):e40–e47. doi: 10.2105/AJPH.2013.301842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermann RC, Chan JA, Provost SE, Chiu WT. Statistical benchmarks for process measures of quality of care for mental and substance use disorders. Psychiatr Serv. 2006;57(10):1461–1467. doi: 10.1176/appi.ps.57.10.1461. [DOI] [PubMed] [Google Scholar]
- Hermann RC, Rollins CK, Chan JA. Risk-adjusting outcomes of mental health and substance-related care: a review of the literature. Harvard review of psychiatry. 2007;15(2):52–69. doi: 10.1080/10673220701307596. [DOI] [PubMed] [Google Scholar]
- Hirsch JA, Leslie-Mazwi TM, Barr RM, McGinty G, Nicola GN, Silva E, Manchikanti L. The Bundled Payments for Care Improvement Initiative. Journal of NeuroInterventional Surgery. 2015 doi: 10.1136/neurintsurg-2015-011746. [DOI] [PubMed] [Google Scholar]
- Hussey PS, Eibner C, Ridgely MS, McGlynn EA. Controlling U.S. health care spending--separating promising from unpromising approaches. N Engl J Med. 2009;361(22):2109–2111. doi: 10.1056/NEJMp0910315. [DOI] [PubMed] [Google Scholar]
- Hussey PS, Ridgely MS, Rosenthal MB. The PROMETHEUS bundled payment experiment: slow start shows problems in implementing new payment models. Health Aff (Millwood) 2011;30(11):2116–2124. doi: 10.1377/hlthaff.2011.0784. [DOI] [PubMed] [Google Scholar]
- Iorio R, Clair AJ, Inneh IA, Slover JD, Bosco JA, Zuckerman JD. Early Results of Medicare’s Bundled Payment Initiative for a 90-Day Total Joint Arthroplasty Episode of Care. The Journal of Arthroplasty. 2016;31(2):343–350. doi: 10.1016/j.arth.2015.09.004. [DOI] [PubMed] [Google Scholar]
- Lee MT, Horgan CM, Garnick DW, Acevedo A, Panas L, Ritter GA, Reynolds M. A performance measure for continuity of care after detoxification: Relationship with outcomes. Journal of Substance Abuse Treatment. 2014;47(2):130–139. doi: 10.1016/j.jsat.2014.04.002. doi: http://dx.doi.org/10.1016/j.jsat.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. Journal of Health Economics. 2005;24(3):465–488. doi: 10.1016/j.jhealeco.2004.09.011. doi: http://dx.doi.org/10.1016/j.jhealeco.2004.09.011. [DOI] [PubMed] [Google Scholar]
- Mark T, Dilonardo JD, Chalk M, Coffey RM. Factors associated with the receipt of treatment following detoxification. Journal of Substance Abuse Treatment. 2003;24(4):299–304. doi: 10.1016/S0740-5472(03)00039-4. [DOI] [PubMed] [Google Scholar]
- Mark TL, Vandivort-Warren R, Montejano LB. Factors affecting detoxification readmission: Analysis of public sector data from three states. Journal of Substance Abuse Treatment. 2006;31(4):439–445. doi: 10.1016/j.jsat.2006.05.019. [DOI] [PubMed] [Google Scholar]
- Mark TL, Wier LM, Malone K, Penne M, Cowell AJ. National Estimates of Behavioral Health Conditions and Their Treatment Among Adults Newly Insured Under the ACA. Psychiatric Services. 2015;66(4):426–429. doi: 10.1176/appi.ps.201400078. [DOI] [PubMed] [Google Scholar]
- Mechanic RE, Altman SH. Payment reform options: episode payment is a good place to start. Health Affairs. 2009;28(2):w262–w271. doi: 10.1377/hlthaff.28.2.w262. [DOI] [PubMed] [Google Scholar]
- O’Byrne TJ, Shah ND, Wood D, Nesse RE, Killinger PJF, Litchy WJ, Naessens JM. Episode-Based Payment: Evaluating the Impact on Chronic Conditions. Medicare & Medicaid Research Review. 2013;3(3) doi: 10.5600/mmrr.003.03.a07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Open Minds. Beacon Contracts With Column Health For Bundled Rate Medication-Assisted Treatment Program. 2017 Sep 10; Retrieved from: https://www.openminds.com/market-intelligence/news/beacon-contract-expands-access-medication-assisted-treatment-opioid-use-disorder-massachusetts/
- Ridgely MS, De Vries D, Bozic KJ, Hussey PS. Bundled Payment Fails To Gain A Foothold In California: The Experience Of The IHA Bundled Payment Demonstration. Health Affairs. 2014;33(8):1345–1352. doi: 10.1377/hlthaff.2014.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson JC. Theory and practice in the design of physician payment incentives. Milbank Q. 2001;79(2):149–177. doi: 10.1111/1468-0009.00202. III. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear SE. Reducing readmissions to detoxification: An interorganizational network perspective. Drug and Alcohol Dependence. 2014;137:76–82. doi: 10.1016/j.drugalcdep.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks WB, Rauh SS, Wadsworth EB, Weinstein JN. The unintended consequences of bundled payments. Annals of internal medicine. 2013;158(1):62–64. doi: 10.7326/0003-4819-158-1-201301010-00012. [DOI] [PubMed] [Google Scholar]