Abstract
Childhood maltreatment increases the risk for posttraumatic stress disorder (PTSD) and comorbid substance use disorder (SUD). One pathway by which this occurs is through impaired emotion regulation. Past research has shown that negative urgency, a deficit in the regulation of negative emotions, is strongly related to PTSD in those with comorbid SUD. However, there is minimal research on the relation between positive urgency and PTSD in those with comorbid SUD. The current study investigated the association between childhood maltreatment, positive urgency, negative urgency, and PTSD symptoms among those with SUD. Results suggested that PTSD was associated with negative urgency and positive urgency overall. Childhood maltreatment did not moderate the association between negative urgency and PTSD. Childhood emotional abuse, emotional neglect, and sexual abuse moderated the relation between positive urgency and PTSD (ΔR2 = .04 to .10). The association between PTSD and positive urgency was only significant at lower levels of emotional abuse and neglect. Future research should further examine the processing of positive emotions in those with PTSD and comorbid SUD. Findings might inform clinical interventions among populations exposed to childhood maltreatment to reduce or prevent the development of psychopathology.
Childhood maltreatment is associated with adulthood psychopathology including posttraumatic stress disorder (PTSD) and substance abuse disorders (SUD; Teicher et al., 2003). Not all people who experience childhood maltreatment go on to develop such conditions, however. Emotion regulation broadly, and the construct of urgency specifically, are proposed as factors that contribute to the development of such conditions among those with maltreatment histories (Weiss, Tull, Viana, Anestis, & Gratz, 2012). It is unclear, however, if these risk factors are independent in their contribution to PTSD or if they interact with each other. Determining if multiple risk factors work in concert is necessary to improve assessment and treatment.
Urgency pertains to difficulty controlling behavior while experiencing emotion (Cyders & Smith, 2007). Urgency occurs both for negative emotions (i.e., negative urgency) and positive emotions (i.e., positive urgency). Prior work has consistently demonstrated an association between PTSD and negative urgency in those with SUD (James, Strom, & Leskela, 2014; Weiss et al., 2012). The only study to examine the relation between PTSD and positive urgency suggested that positive urgency mediated the association between PTSD and risky behaviors in those with SUD (Weiss, Tull, Sullivan, Dixon-Gordon, & Gratz, 2015). This study, and related prior work, have not examined the potential moderating role of maltreatment.
Childhood maltreatment refers to emotional abuse, emotional neglect, physical abuse, physical neglect, and sexual abuse (Hamburger, Leeb, & Swahn, 2008). Maltreatment type and severity is related to later psychopathology (Litrownik et al., 2005). With regards to PTSD, the severity and type of maltreatment is associated with more complex symptoms in adulthood (Jackson, Gabrielli, Fleming, Tunno, & Makanui, 2014). It is unknown if the type of maltreatment experienced is also associated with urgency. Victims of childhood maltreatment often grow up in invalidating environments that punish emotional expression. These experiences promote poor emotion regulation in adulthood (Clohessy & Ehlers, 1999; Cloitre, Miranda, Stovall-McClough, & Han, 2005). Exposure to emotional maltreatment may therefore increase urgency, which increases subsequent PTSD.
The current study examined the moderating effect of urgency on the relation between type of childhood maltreatment and PTSD symptoms among those with SUD. It was hypothesized that urgency was more strongly related to emotional abuse than other maltreatment types. Furthermore, it was hypothesized that the relations between positive and negative urgency and PTSD symptoms were moderated by emotional abuse, but not other maltreatment types.
Method
Participants and Procedure
For this study, 84 participants who met criteria for lifetime SUD were recruited. Each participant reported his or her length of time (in years) using the following substances: heroin (M = 4.87, SD = 5.87), prescription opioids (M = 6.98, SD = 6.02), alcohol (M = 5.64, SD = 7.90), cocaine (M = 5.01, SD = 7.20), and cannabis (M = 10.98, SD = 11.83). The mean age of participants was 35.27 years (SD = 8.25), the majority were male (n = 45, 53.6%) and earned less than $10,000 annually (n = 46, 54.8%). Participants self-identified as White (n = 72, 85.6%), African American (n = 2, 2.4%), Latino (n = 2, 2.4%), Asian American (n = 2, 2.4%), Native American (n = 4, 4.8%), and other (n = 6, 7.1%). Recruitment was conducted through Internet advertisements (e.g., Facebook, Craigslist) and flyers. All participants provided consent. The Institutional Review Board of the University of Vermont in Burlington, VT, approved all procedures.
Measures
The Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998) is a 28-item self-report scale that assesses emotional neglect, emotional abuse, physical neglect, physical abuse, and sexual abuse. Each abuse and neglect type is assessed with a 5-item scale that ranges from 5 to 25. Higher scores indicate more abuse. Internal consistency in the present sample ranged from good to excellent (Cronbach’s α = .80 to .96).
The 4-item subscales of positive urgency and negative urgency from the Shortened Version of the UPPS-P Impulsive Behavior Scale (SUPPS-P; Cyders, Littlefield, Coffey, & Karyadi, 2014) were used. Scores range from 4 to 16 with lower scores indicating greater urgency and higher scores indicated lower urgency. Internal consistency for the combined subscales was good (Cronbach’s α = .80), was moderate for negative urgency (Cronbach’s α = .77), and borderline for positive urgency (Cronbach’s α = .66).
The PTSD Checklist for DSM-5 (PCL-5; Bovin et al., 2016) is a 20-iem self-report measure of PTSD symptoms. Scores range from 0 to 80 with higher scores corresponding to more severe symptoms. Scores of ≥ 33 indicate likely PTSD. Internal consistency was excellent (Cronbach’s α = .96).
The Addiction Severity Index Lite (ASI-Lite; McLellan et al., 1992) is 169-item structured interview that assesses several domains relevant to substance use. Interviews were conducted by trained research assistants. For the present study, the ASI was used to evaluate substance use history; the other subscales were not relevant. Agreement among interviewers was 100%.
The Structured Clinical Interview for the DSM-5 Disorders (Research Version; SCID-5; First, Williams, Karg, & Spitzer, 2015) is a semistructured interview that determines the presence of mental health disorders according to the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association, 2013) criteria. For the present study, the PTSD module was administered to determine the presence/absence of current PTSD for participants. Interviews were conducted by trained research assistants. Agreement among interviewers was 100%.
Data Analysis
Bivariate correlations assessed the relation between PTSD symptoms, negative urgency, positive urgency, and childhood maltreatment severity. Regressions that included each CTQ subscale, negative urgency or positive urgency, and an interaction term created from the centered product of the CTQ subscale and the urgency scale evaluated the moderating effect of urgency on maltreatment. Age and gender were included as covariates. This approach maximized power for the interaction effects, which are traditionally small (Aiken, West, & Reno, 1991). Using a standard α level of .05, power of .80, the current sample could detect an effect of ΔR2 ≥ .09. Significant interactions were probed at plus or minus 1 SD of the level of urgency. There were no missing data for this analysis.
Results
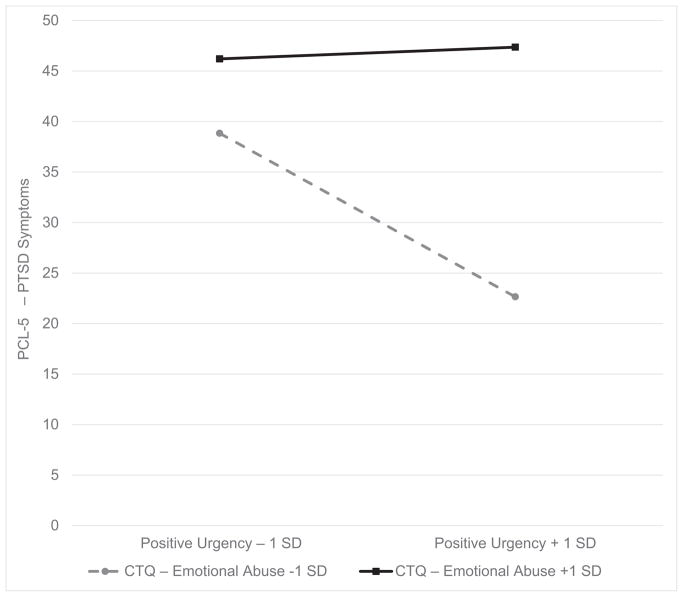
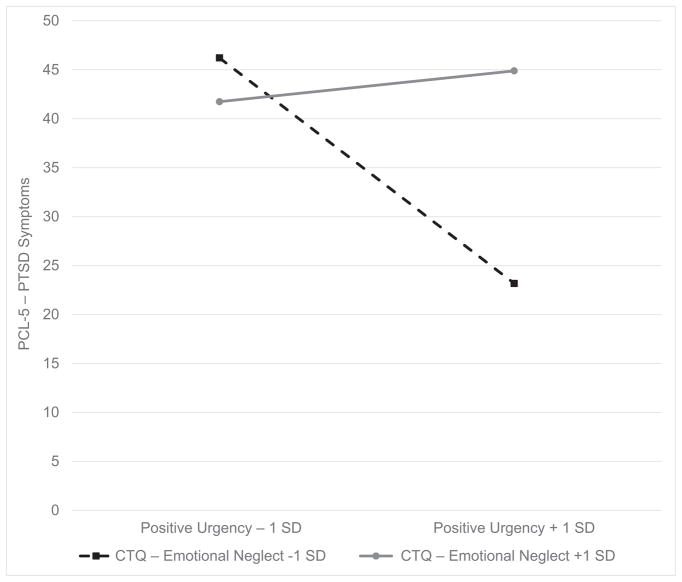
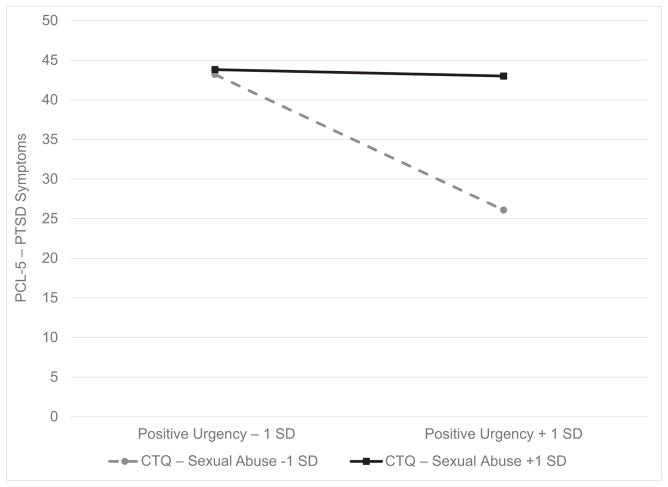
The mean ASI-Lite drug composite score was M = 0.24 (SD = 0.11), which was higher than the ASI reference sample (M = 0.18; Denis, Cacciola, & Alterman, 2013). The majority of the sample met criteria for PTSD (n = 57, 67.9%). All subscales of the CTQ, positive urgency, and negative urgency were significantly related to PTSD severity (Table 1). Positive urgency and negative urgency were not significantly associated with the CTQ subscales. Multiple regressions controlling for age and gender found significant interactions between positive urgency and emotional neglect, emotional abuse, and sexual abuse as related to PTSD severity (Table 2). The interactions between other maltreatment scales and positive urgency were not significant. The interactions between negative urgency and all childhood maltreatment scales were not significant (p = .342 to .945). The interactions for emotional abuse, emotional neglect, and sexual abuse suggested that those who reported less maltreatment had a significant relation between positive urgency and PTSD (Figures 1–3). As the amount of maltreatment increased, the strength of the relation between positive urgency and PTSD severity diminished.
Table 1.
Bivariate Relations Among Variables of Interest
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. PCL-5 | - | |||||||
| 2. CTQ–Emotional Abuse | .42** | - | ||||||
| 3. CTQ–Emotional Neglect | .23* | .74** | - | |||||
| 4. CTQ–Sexual Assault | .31** | .42** | .29** | - | ||||
| 5. CTQ–Physical neglect | .25** | .56** | .65** | .26** | - | |||
| 6. CTQ–Physical Abuse | .38** | .69** | .49** | .43** | .44** | - | ||
| 7. Positive Urgency | −.22* | −.05 | −.07 | −.01 | .10 | < .01 | - | |
| 8. Negative Urgency | −.44** | −.14 | −.13 | −.07 | .01 | −.05 | .52** | - |
| M | 38.16 | 12.4 | 14.26 | 10.88 | 10.44 | 10.63 | 11.54 | 8.85 |
| SD | 18.93 | 5.58 | 5.62 | 7.24 | 4.39 | 5.6 | 2.52 | 2.96 |
Note. PCL-5 scores range from 0 to 80. CTQ scales range from 5 to 25. Positive and negative urgency scales range from 4 to 16. PCL-5 = PTSD Symptom Checklist; CTQ = Childhood Trauma Questionnaire.
p < .05.
p < .01.
Table 2.
Regression Models Evaluating the Relation Between PTSD Symptoms, Childhood Maltreatment, and Positive Urgency
| Predictor | B | SE | 95% CI | R2Total | ΔR2 |
|---|---|---|---|---|---|
| CTQ–Emotional Abuse | 1.44** | 0.36 | [0.73, 2.14] | .33** | .05* |
| Positive Urgency | −1.49 | 0.77 | [−3.02, 0.04] | ||
| Interaction | 0.31* | 0.13 | [0.04, 0.57] | ||
| Female gender | 6.46 | 3.77 | [−1.06, 13.97] | ||
| Age | −0.50 | 0.22 | [−0.95, −.05] | ||
| CTQ–Emotional Neglect | 0.77* | 0.34 | [0.09, 1.44] | .30** | .10** |
| Positive Urgency | −1.97* | 0.76 | [−3.48, −0.45] | ||
| Interaction | 0.46** | 0.14 | [0.18, 0.74] | ||
| Female gender | 9.97** | 3.68 | [2.64, 17.30] | ||
| Age | −0.46 | 0.23 | [−0.92, 0.01] | ||
| CTQ–Sexual Assault | 0.67* | 0.31 | [0.05. 1.29] | .26** | .05* |
| Positive Urgency | −1.94* | 0.78 | [−3.50, −0.38] | ||
| Interaction | 0.25* | 0.11 | [0.03, 0.46] | ||
| Female gender | 7.40 | 4.24 | [−1.05, 15.84] | ||
| Age | −0.41 | 0.24 | [−0.89, 0.07] | ||
| CTQ–Physical Neglect | 0.86 | 0.49 | [−0.10, 1.83] | .20** | < .01 |
| Positive Urgency | −2.36** | 0.80 | [−3.97, −0.76] | ||
| Interaction | 0.08 | 0.18 | [−0.27, 0.43] | ||
| Female gender | 10.14* | 3.96 | [2.25, 18.04] | ||
| Age | −0.27 | 0.24 | [−0.76, 0.21] | ||
| CTQ–Physical Abuse | 1.21** | 0.35 | [0.51, 1.91] | .20** | .01 |
| Positive Urgency | −1.87* | 0.80 | [−3.47, −0.27] | ||
| Interaction | 0.19 | 0.15 | [−0.11, 0.50] | ||
| Female gender | 9.10* | 3.75 | [1.62, 16.58] | ||
| Age | −0.45 | 0.23 | [−0.91, 0.02] |
Note. Dependent variable = PCL-5. ΔR2 = increase in R2 from interaction. Interaction refers to the interaction between positive urgency and the maltreatment type. PCL-5 = PTSD Symptom Checklist; CTQ = Childhood Trauma Questionnaire.
p < .05.
p < .01.
Figure 1.
Relation between posttraumatic stress disorder and positive urgency at plus or minus 1 SD of emotional neglect. PCL-5 = PTSD Symptom Checklist; CTQ = Childhood Trauma Questionnaire.
Figure 3.
Relation between posttraumatic stress disorder and positive urgency at plus or minus 1 SD of sexual abuse. PCL-5 = PTSD Symptom Checklist; CTQ = Childhood Trauma Questionnaire.
Discussion
The results of the present study suggest that PTSD in those with SUD is associated with impaired emotion regulation, defined as positive and negative urgency. Positive urgency and negative urgency, however, were unrelated to maltreatment histories. The results of this study contribute to the small body of work on the relation between PTSD and the regulation of positive emotions. These findings should be considered preliminary, however, given the modest sample size. The current study had sufficient power to detect an ΔR2 ≥ .09 such that replication is required before firmer conclusions are drawn.
The relation between negative urgency and PTSD suggests that poor emotion regulation is a key source of impairment in those with SUD. Recent work suggests that PTSD may best be defined as a deficit in the regulation of fearful responses to trauma-related cues (Norrholm et al., 2015). This deficit may lead those with PTSD to engage in risky behavior, such as substance use, when exposed to trauma cues to manage the resulting negative emotions. Increased maladaptive behaviors while experiencing negative affect may explain the increased impairment among those with PTSD and comorbid SUD (Mills, Teesson, Ross, & Darke, 2007).
The relation between positive urgency and PTSD was significant, but markedly weaker than that between negative urgency and PTSD. The difference in the strength of this relation can be attributed to the moderating effect of emotional and sexual maltreatment on the association between PTSD and positive urgency. Those who reported minimal matreatment demonstrated the hypothesized relation between PTSD and positive urgency. However, this relation diminished for those who reported severe maltreatment. Those with significant histories of maltreatment may process positive emotions differently such that a reckless response to positive emotions is not viewed as troublesome and thus unrelated to PTSD. Prior work has suggested that PTSD is associated with an altered processing of rewarding experiences (Hopper et al., 2008). Additional evidence has suggested that those with PTSD demonstrate increased negative affect when exposed to positive events, which further speaks to an alteration in their response to positive experiences (Frewen, Dozois, & Lanius, 2012). For those with comorbid SUD, the use of substances that directly impacts reward processing brain circuits may further exacerbate these alterations.
The present study had several limitations. All constructs were measured via self-report, which are prone to biased responses. Future research should use objective measures including behavioral tasks and interviews. The design was cross-sectional, yet the findings imply longitudinal relations. Additional work is needed to evaluate the longitudinal nature of these associations. The urgency scales in the present study had lower internal consistency than in prior samples that used the same measure. Finally, the current study did not assess relevant environmental factors such as an invalidating childhood environment. Such constructs may further elucidate the role between urgency and PTSD symptoms.
The present study is among the first to evaluate the relation between PTSD, positive urgency, and maltreatment histories. These results set the stage for further investigation into the moderating effect of other factors that may help explain the association between emotion regulation and posttrauma mental health.
Figure 2.
Relation between posttraumatic stress disorder and positive urgency at plus or minus 1 SD of emotional abuse. PCL-5 = PTSD Symptom Checklist; CTQ = Childhood Trauma Questionnaire.
Acknowledgments
This research study was supported by the National Institute of Mental Health (1K08MH107661-01A1; PI: Price) and a Small Faculty Research Award (PI: Price).
References
- Aiken LS, West SG, Reno RR. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: Author; 2013. [Google Scholar]
- Bernstein DP, Fink L. Childhood Trauma Questionnaire: A retrospective self-report manual. San Antonio, TX: Psychological Corp; 1998. [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment. 2016;28:1379–1391. doi: 10.1037/pas0000254. https://doi.org/10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Clohessy S, Ehlers A. PTSD symptoms, response to intrusive memories and coping in ambulance service workers. British Journal of Clinical Psychology. 1999;38:251–265. doi: 10.1348/014466599162836. https://doi.org/10.1348/014466599162836. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Miranda R, Stovall-McClough KC, Han H. Beyond PTSD: Emotion regulation and interpersonal problems as predictors of functional impairment in survivors of childhood abuse. Behavior Therapy. 2005;36:119–124. https://doi.org/10.1016/S0005-7894(05)80060-7. [Google Scholar]
- Cyders MA, Littlefield AK, Coffey S, Karyadi KA. Examination of a short English version of the UPPS-P Impulsive Behavior Scale. Addictive Behaviors. 2014;39:1372–1376. doi: 10.1016/j.addbeh.2014.02.013. https://doi.org/10.1016/j.addbeh.2014.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Smith GT. Mood-based rash action and its components: Positive and negative urgency. Personality and Individual Differences. 2007;43:839–850. https://doi.org/10.1016/j.paid.2007.02.008. [Google Scholar]
- Denis CM, Cacciola JS, Alterman AI. Addiction Severity Index (ASI) summary scores: Comparison of the recent status scores of the ASI-6 and the composite scores of the ASI-5. Journal of Substance Abuse Treatment. 2013;45:444–450. doi: 10.1016/j.jsat.2013.06.003. https://doi.org/10.1016/j.jsat.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, Spitzer RL. Structured Clinical Interview for DSM-5—Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV) Arlington, VA: American Psychiatric Association; 2015. [Google Scholar]
- Frewen PA, Dozois DJA, Lanius RA. Assessment of anhedonia in psychological trauma: Psychometric and neuroimaging perspectives. European Journal of Psychotraumatology. 2012;3:1–12. doi: 10.3402/ejpt.v3i0.8587. https://doi.org/10.3402/ejpt.v3i0.8587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamburger ME, Leeb RT, Swahn MH. Childhood maltreatment and early alcohol use among high-risk adolescents. Journal of Studies on Alcohol and Drugs. 2008;69:291–295. doi: 10.15288/jsad.2008.69.291. https://doi.org/10.15288/jsad.2008.69.291. [DOI] [PubMed] [Google Scholar]
- Hopper JW, Pitman RK, Su Z, Heyman GM, Lasko NB, Macklin ML, … Elman I. Probing reward function in posttraumatic stress disorder: Expectancy and satisfaction with monetary gains and losses. Journal of Psychiatric Research. 2008;42:802–807. doi: 10.1016/j.jpsychires.2007.10.008. https://doi.org/10.1016/j.jpsychires.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson Y, Gabrielli J, Fleming K, Tunno AM, Makanui PK. Untangling the relative contribution of maltreatment severity and frequency to type of behavioral outcome in foster youth. Child Abuse & Neglect. 2014;38:1147–1159. doi: 10.1016/j.chiabu.2014.01.008. https://doi.org/10.1016/j.chiabu.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James LM, Strom TQ, Leskela J. Risk-taking behaviors and impulsivity among veterans with and without PTSD and mild TBI. Military Medicine. 2014;179:357–363. doi: 10.7205/MILMED-D-13-00241. https://doi.org/10.7205/MILMED-D-13-00241. [DOI] [PubMed] [Google Scholar]
- Litrownik AJ, Lau A, English DJ, Briggs E, Newton RR, Romney S, Dubowitz H. Measuring the severity of child maltreatment. Child Abuse & Neglect. 2005;29:553–573. doi: 10.1016/j.chiabu.2003.08.010. https://doi.org/10.1016/j.chiabu.2003.08.010. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, … Argeriou M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. https://doi.org/10.1016/0740-5472(92)90062-S. [DOI] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Ross J, Darke S. The impact of post-traumatic stress disorder on treatment outcomes for heroin dependence. Addiction. 2007;102:447–454. doi: 10.1111/j.1360-0443.2006.01711.x. https://doi.org/10.1111/j.1360-0443.2006.01711.x. [DOI] [PubMed] [Google Scholar]
- Norrholm SD, Glover EM, Stevens JS, Fani N, Galatzer-Levy IR, Bradley B, … Jovanovic T. Fear load: The psychophysiological over-expression of fear as an intermediate phenotype associated with trauma reactions. International Journal of Psychophysiology. 2015;98:270–275. doi: 10.1016/j.ijpsycho.2014.11.005. https://doi.org/10.1016/j.ijpsycho.2014.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP, Kim DM. The neurobiological consequences of early stress and childhood maltreatment. Neuroscience & Biobehavioral Reviews. 2003;27:33–44. doi: 10.1016/s0149-7634(03)00007-1. https://doi.org/10.1016/S0149-7634(03)00007-1. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Sullivan TP, Dixon-Gordon KL, Gratz KL. Posttraumatic stress disorder symptoms and risky behaviors among trauma-exposed inpatients with substance dependence: The influence of negative and positive urgency. Drug and Alcohol Dependence. 2015;155:147–153. doi: 10.1016/j.drugalcdep.2015.07.679. https://doi.org/10.1016/j.drugalcdep.2015.07.679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Viana AG, Anestis MD, Gratz KL. Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders. 2012;26:453–458. doi: 10.1016/j.janxdis.2012.01.007. https://doi.org/10.1016/j.janxdis.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]