Abstract
This secondary analysis examined changes in sleep quality associated with participation in a Mindfulness-Based Stress Reduction (MBSR) program among healthy older adults. Data were collected at baseline, 8-weeks post-treatment, and a 6-month follow-up from adults aged ≥ 65 (N = 200), randomly assigned to MBSR or a waitlist control. Group differences were examined using mixed analysis of covariance with repeated measures on the total Pittsburgh Sleep Quality Index (PSQI) score. A small-sized, significant effect was found on overall sleep among MBSR participants with baseline PSQI scores > 5, indicative of a sleep disturbance, F(2, 80) = 4.32, p = .02, . A medium-sized, significant effect was found for MBSR participants with baseline PSQI scores ≥ 10, F(2, 28) = 3.13, p = .04, . These findings indicate that improved sleep quality for older adults who have higher levels of sleep disturbance may be associated with participation in MBSR.
Keywords: older adults, sleep disturbance, mindfulness, mind–body
Introduction
Approximately 5% to 10% of the general adult population in industrialized nations meet diagnostic criteria for insomnia, a condition characterized by consistent difficulty initiating or maintaining sleep (Chung et al., 2015; Ohayon, 2002). Sleep disturbance, a more general and non-diagnostic term encompassing insomnia as well as other reasons for disturbed sleep, is present in one fourth to one third of adults (Ohayon, 2002; Stranges, Tigbe, Gómez-Olivé, Thorogood, & Kandala, 2012). Among older adults specifically, the prevalence of insomnia alone reaches 25%, whereas overall sleep disturbance represents the most commonly reported health problem (Ohayon, 2002; Ohayon & Vecchierini, 2005) with an estimated prevalence rate of up to 41% (Foley, Ancoli-Israel, Britz, & Walsh, 2004).
Mind–body interventions are particularly relevant for addressing factors associated with both sleep disturbance and insomnia, including stress, hyperarousal, and dysfunctional beliefs about sleep. Notably, stress has been attributed as the most common precipitant of insomnia and contributes to poor sleep quality (Åkerstedt et al., 2002; Bastien, Vallières, & Morin, 2004; Pigeon & Cribbet, 2012). Further, hyperarousal is postulated to be a primary etiological factor in the development and maintenance of insomnia, in which sleep initiation is inhibited by both physiological (e.g., elevated cortisol levels at bedtime) and cognitive (e.g., selective attention to perceived threats, rumination, and worry) arousal (Pigeon & Cribbet, 2012; Riemann et al., 2010). Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1990) is a transdiagnostic mind–body intervention that teaches non-judgmental awareness of sensations, cognitions, and emotions as they arise in the present moment (Greeson, Garland, & Black, 2014). Practitioners learn to relate to their body and mind with awareness and acceptance. Mindfulness training in non-judgmental observation of cognitions and physiological and emotional arousal may help to diminish sleep interfering processes (Winbush, Gross, & Kreitzer, 2007). Ong, Ulmer, and Manber (2012) proposed that mindful awareness teaches practitioners to shift attention away from the cognitive and physiological states that may disturb sleep, allowing for a more adaptive way of responding to sleep-related arousal. Participants are taught to respond to cognitive and emotional stimuli, including stressors, with acceptance rather than with conditioned and potentially harmful reactions. In this way, the techniques of mindfulness address many of the responses to the precipitating and/or maintaining stressors associated with disrupted sleep, including hyperarousal. MBSR’s ability to regulate cognitive and physiologic arousal has the potential to significantly improve sleep in older adults.
In a review of the effect of mindfulness-based interventions (MBIs) on sleep disturbance, Winbush and colleagues (2007) found seven studies that qualified for their review, with four uncontrolled studies demonstrating significant improvements in sleep quality or sleep duration in young and middle-aged adults (Carlson & Garland, 2005; Carlson, Speca, Patel, & Goodey, 2004; Heidenreich, Tuin, Pflug, Michal, & Michalak, 2006; Kreitzer, Gross, Ye, Russas, & Treesak, 2005). Though the controlled studies provided mixed support of MBIs on sleep quality, the studies provided preliminary evidence for increased home practice associated with improved sleep (Winbush et al., 2007). In these studies, the measurements of sleep varied, with some studies using self-report sleep diaries to measure sleep continuity and others using a validated self-report measure of sleep (Pittsburgh Sleep Quality Index [PSQI]; Buysse, Reynolds, Monk, Berman, & Kupfer, 1989), which assesses overall sleep quality based on items measuring subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, sleep medication use, and daytime dysfunction. Recently, a randomized controlled trial (RCT) by Gross et al. (2011) found that MBSR-related improvements in sleep quality were comparable to psychopharmacology treatment for individuals with primary chronic insomnia. The investigators found large, significant improvements as measured by validated self-report sleep scales (Insomnia Severity Index [ISI] and PSQI; Bastien, Vallières, & Morin, 2001; Buysse et al., 1989) and wrist actigraphy measuring sleep onset latency.
Three studies to date have examined the effect of an MBI on sleep disturbance among older adults, two of which were RCTs (Black, O’Reilly, Olmstead, Breen, & Irwin, 2015; Foulk, Ingersoll-Dayton, Kavanagh, Robinson, & Kales, 2014; Zhang et al., 2015). Black et al.’s (2015) MBI RCT for older adults aged ≥ 55 with sleep disturbance (N = 49) found that the mindfulness participants experienced significant decreases on the PSQI (Cohen’s d = 0.89) as compared with a sleep hygiene and education active group control. Black et al.’s MBI used standardized mindful awareness practices (MAPs) and their sample was older adults with sleep disturbance as characterized by a PSQI score > 5. Zhang et al.’s (2015) MBSR RCT for older adults aged ≥ 75 in China with chronic insomnia (N = 60) also found that the mindfulness participants experienced significant decreases on the PSQI (Cohen’s d = 1.12) as compared with a waitlist control (WLC) group. A non-randomized study found significant reductions in sleep difficulties among older adults with depression after participation in a Mindfulness-Based Cognitive Therapy program (Foulk et al., 2014). Thus, a small body of work suggests that MBIs have the potential to remediate the prevalent health problem of sleep disturbance among older adults. No study to date has examined changes in sleep associated with participation in an MBSR program among a healthy sample of older adults in the United States with and without sleep disturbance. Examining this association among healthy older adults with and without sleep disturbance is important because it increases generalizability to older adults in the United States for whom sleep is the most common and prevalent health problem.
In this secondary analysis, we report changes in subjective sleep quality of older adults associated with participation in an MBSR program. We first examined MBSR and WLC group differences over time on the global PSQI score for the entire sample of older adults. Given the likely existence of a floor effect in this generally healthy sample, we also compared PSQI scores between MBSR and WLC conditions in two subsamples: those who reported baseline PSQI scores > 5 (n = 85), indicating sleep disturbance, and those who reported PSQI scores ≥ 10 (n = 33), indicating possible insomnia. For each analysis, we hypothesized that participants in the MBSR group would show significant improvements in sleep as compared with the WLC participants. Finally, we examined group differences in PSQI scores over time among older adults in the MBSR condition only and assigned participants to three PSQI severity groups based upon PSQI scores of ≤ 5, 6 to 9, and ≥ 10. We hypothesized that MBSR would be associated with improved sleep quality for older adults with moderate to high levels of sleep disturbance.
Methods
Participants and Procedures
In a prior report, immunological, electrophysiological, and cognitive outcomes were examined among older adults in an RCT of MBSR and a WLC group (Moynihan et al., 2013). The study procedures are available in Moynihan et al. (2013). In brief, older adults from the community were recruited through advertisements in local newspapers and flyers in primary care offices. Eligible participants had to be aged 65 years or older and English speaking. Participants must have had a stable medication regimen for eight weeks prior to enrollment if prescribed antidepressant or anxiolytic medications. Potential participants were excluded for the following mental disorders based on the Structured Clinical Interview (SCID; First, Spitzer, Gibbon, & Williams, 2002) for the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association [APA], 2000): major depression with psychotic features; psychosis; lifetime history of schizophrenia, bipolar disorder, organic brain syndrome, or mental retardation; and alcohol or substance abuse within the previous year.
A total of 228 subjects met inclusion criteria, provided written informed consent, and underwent initial assessment. Prior to the post-test, 20 subjects withdrew from the study. Data are presented on the 200 participants who had complete data on all study variables at all three time points. Subject enrollment, intervention completion, and assessment follow-up occurred in several waves between March 2006 and May 2009. Subjects were randomized to participate in either the 8-week program of MBSR (n = 100) or a WLC condition (n = 100). In the parent study, participants meeting inclusion criteria were randomized to an 8-week MBSR intervention or WLC using an Excel spreadsheet function for generating random numbers. This function was used to determine the treatment arm for each subject, with equal chance for either arm. Analyses were conducted to discern the adequacy of the randomization. Data from the subjects assigned to the MBSR and WLC condition were collected following randomization and before beginning the MBSR program (pre-treatment), immediately following completion of the 8-week MBSR program (post-treatment), and 6 months following post-treatment (follow-up). Participant characteristics of the subsample analyzed here are reported in Table 1. The study protocol was approved by the University of Rochester Institutional Review Board (RSRB00012363) and is registered with clinicaltrials.gov (NCT01027780).
Table 1.
Sample Characteristics.
| Entire sample | t | PSQI > 5 | t | PSQI ≥ 10 | t | ||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| MBSR | WLC | MBSR | WLC | MBSR | WLC | ||||
| n | 100 | 100 | 49 | 36 | 18 | 15 | |||
| Age, M (SD) | 72 (6.82) | 73 (6.59) | 1.47 | 71 (7.04) | 73 (6.38) | 1 | 69 (3.91) | 71 (5.71) | 1.39 |
| Gender, % female | 62% | 62% | χ2 = 0 | 66% | 66% | χ2 = 0 | 74% | 82% | χ2 = .39 |
| Baseline PSQI, M (SD) | 6.22 (3.73) | 5.29 (3.58) | −2.06* | 9.27 (3.07) | 9.22 (2.71) | −0.29 | 12.56 (2.59) | 11.93 (1.87) | −1.11 |
Note. PSQI = Pittsburgh Sleep Quality Index total score; MBSR = Mindfulness-Based Stress Reduction; WLC = waitlist control condition.
p < .05.
Intervention
Each participant in the MBSR program attended a group-based (15–20 members) 8-week curriculum that included weekly 120-min sessions and an “all-day intensive” session of 7 hr. The MBSR treatment groups were led by a certified instructor and 25% of the sessions were videotaped and examined for adherence to the MBSR curriculum. Co-directors from the Center for Mindfulness examined the sessions and reported full adherence to the MBSR curriculum. The MBSR program accommodated the mobility, sensory, and cognitive limitations of the participants who met the inclusion criteria. For example, an individual in a wheelchair could complete mindful Hatha yoga with a variety of modified sitting postures.
Measures
Participants were administered the PSQI, a 24-item self-administered questionnaire that assesses sleep over the past month. There are seven component scores which can range from 0 to 3 (sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction). A global sleep quality score based on the sum of the seven component scores can range from 0 to 21, where scores > 5 indicate the presence of a sleep disturbance and scores ≥ 10 may be indicative of insomnia (Buysse et al., 2011). Cronbach’s alpha internal consistency in the current sample was .77, which compares to the .83 reported in the original validation study (Buysse et al., 2011). For this study, we assessed the global PSQI score.
Weekly class attendance was recorded and participants completed weekly practice logs of minutes spent practicing the awareness of breath or sitting meditation, hatha yoga, body scan, and informal practice at home.
Statistical Analyses
Using t tests and mixed analysis of covariance (ANCOVA) with repeated measures, we compared MBSR and the WLC groups on baseline variables, and examined changes in outcomes over time. A mixed ANCOVA compares the mean differences between groups that have been split on two factors, a within-subjects factor (i.e., time) and a between-subjects factor (i.e., treatment condition), and includes one or more covariates. All analyses controlled for gender, age, and use of sleep medication. All analyses were conducted in SPSS. Effect sizes were calculated with partial eta squared. For this effect size calculation, .01 is considered small, .09 medium, and .25 large (Cohen, Cohen, West, & Aiken, 2013). First, we examined the MBSR and WLC group differences over time (N = 200) on global PSQI scores. Second, we examined MBSR and WLC group differences over time on a subsample of participants whose Global PSQI score was above 5, indicating poor sleep quality (n = 85; 49 in MBSR, 36 in WLC). Then we examined MBSR and WLC group differences over time in a subsample of participants whose Global PSQI score was ≥ 10, indicating possible insomnia (n = 33; 18 in MBSR, 15 in WLC). Finally, we examined changes in the PSQI associated with participation in the MBSR program by dividing the MBSR participants into three groups based on their baseline global PSQI score: ≤ 5, 6–9, and ≥ 10. We examined regression to the mean (RTM) using scatter-plots of change against the baseline PSQI scores in the subsamples. We did not detect RTM in the main sample or subsamples of participants whose global PSQI score were > 5 and ≥ 10; however, we did detect RTM in the subsample whose PSQI score was 6 to 9. We corrected for RTM using ANCOVA. The Bonferonni method was used to adjust for multiple comparisons. In all instances, the PSQI global score was our main outcome measure, which was measured at study entry as well as 8 weeks post-treatment and a 6-month follow-up.
Results
Baseline Characteristics
At baseline, no significant group differences were found. The majority of the sample was retired (82%), Caucasian (98%), and well-educated (71% college educated or more). The subset of participants with PSQI scores > 5 did not differ significantly from the larger group sample in terms of demographic characteristics; however, the group included slightly more women (see Table 1).
Class Attendance
MBSR participant attendance to the eight sessions and all-day was high (M = 8.29, SD = 1.13) and participants practiced mindfulness meditation an average of 205.84 (SD = 120.08) min per week, which is about 30 min of mindfulness meditation practice per day.
Changes in Sleep Quality for Entire Sample
In examining the entire sample of older adults, the interaction of time and group assignment was significant with a small effect size (Table 2). Baseline PSQI scores decreased .99 points from baseline to post-treatment for the MBSR group and .1 point for the WLC group. The PSQI changes were not correlated with mindfulness practice time for the MBSR group (r = −.06, p = .54).
Table 2.
Changes in Sleep Quality Associated With Participation in MBSR Compared With Wait List Control Using Mixed ANCOVA With Repeated Measures.
| Sample | n | PSQI scores M (SD) |
Repeated measures ANCOVA Time × Condition |
||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Pre-test | Post-test (8 weeks) | Follow-up (6 months) | F | p | Effect sizea | ||
| Entire sample | |||||||
| MBSR | 100 | 6.22 (3.73) | 5.23 (3.36) | 5.44 (3.32) | 3.68 | .03 | 0.02 |
| WLC | 100 | 5.29 (3.58) | 5.19 (3.66) | 5.10 (3.60) | |||
| PSQI > 5 subsample | |||||||
| MBSR | 49 | 9.27 (3.07) | 7.08 (3.05) | 7.37 (2.96) | 4.32 | 0.02 | 0.05 |
| WLC | 36 | 9.22 (2.71) | 8.64 (3.85) | 8.39 (3.49) | |||
| PSQI ≥ 10 subsample | |||||||
| MBSR | 18 | 12.56 (2.59) | 9.17 (3.03) | 8.67 (2.61) | 3.13 | 0.04 | 0.10 |
| WLC | 15 | 11.93 (1.87) | 11.33 (3.85) | 10.33 (3.77) | |||
Note. MBSR = Mindfulness-Based Stress Reduction; ANCOVA = analysis of covariance; PSQI = Pittsburgh Sleep Quality Index total score; WLC = waitlist control condition.
Partial eta squared (.01–.08 is small, .09–.24 is medium, and .25+ is large).
Changes in Sleep Quality for Subsamples With Baseline Scores > 5
We examined effects of MBSR on the global PSQI scores for the participants whose baseline global PSQI was > 5, indicating sleep disturbance. Notably, 43% of the sample (85 of 200) exceeded the validated PSQI cutoff of 5 and one third of the sample reported use of sleep medication. We found a small, significant effect of the time by group interaction on overall sleep quality (Table 2). Among participants with a baseline PSQI score > 5, the mean global PSQI score decreased 2.2 points from baseline to post-treatment for the MBSR group and .58 points for the WLC group. The PSQI changes were not correlated with mindfulness practice time for the MBSR group (r = .02, p = .87).
Changes in Sleep Quality for Subsample With Baseline Scores ≥ 10
Examination of changes in sleep quality for participants with a global PSQI ≥ 10, an indicator of possible insomnia, in the MBSR (n = 18) versus WLC (n = 15) conditions revealed a medium, significant effect of the time by group interaction (Table 2). In this latter subsample, the mean global PSQI score (SD) decreased 3.9 points from baseline to follow-up for the MBSR group and .6 points in the WLC group. The PSQI changes were correlated with mindfulness practice time for the MBSR group (r = .53, p = .02).
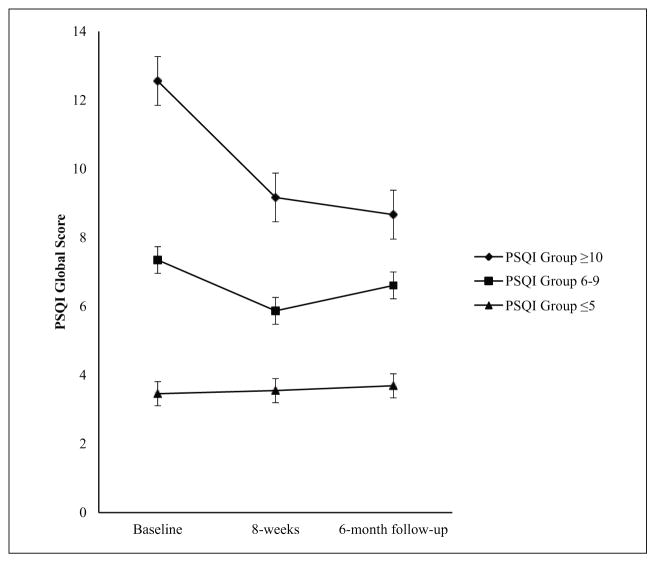
Changes in PSQI by Time and Baseline Sleep Disturbance Severity for MBSR Participants Only
Finally, we examined changes in PSQI scores for only the participants in the MBSR condition categorized on their baseline PSQI scores (≤ 5, 6–9, and ≥ 10; Figure 1). We found a medium, significant effect of time on overall sleep quality for MBSR participants whose baseline global PSQI score was ≥ 10 (see Table 3). No effect of time on overall sleep quality was found for MBSR participants whose baseline global PSQI score was ≤ 5 or 6 to 9.
Figure 1.
Changes in PSQI global score for MBSR participants based on baseline PSQI scores of ≤ 5 (n = 54), 6 to 9 (n = 31), and ≥ 10 (n = 18).
Note. PSQI = Pittsburgh Sleep Quality Index; MBSR = Mindfulness-Based Stress Reduction.
Table 3.
PSQI Scores by Time and Baseline Sleep Disturbance Severity Using Mixed ANCOVA With Repeated Measures.
| Sample | n | PSQI scores M (SD) |
Between group mean differencea (95% CI) | Repeated measures ANCOVA |
||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Pre-test | Post-test (8-weeks) | Follow-up (6-months) | F | p | Effect sizeb | |||
| MBSR participants | ||||||||
| PSQI ≥ 10 | 18 | 12.56 (2.59) | 9.17 (3.03) | 8.67 (2.61) | 5.61 [4.17, 7.11] | 10.74 | <.01 | 0.15 |
| PSQI 6–9 | 31 | 7.35 (1.02) | 5.87 (2.35) | 6.61 (2.92) | ||||
| PSQI ≤ 5 | 54 | 3.46 (1.37) | 3.55 (2.69) | 3.69 (2.60) | ||||
Note. PSQI = Pittsburgh Sleep Quality Index total score; ANCOVA = analysis of covariance; MBSR = Mindfulness-Based Stress Reduction.
Pre-test to post-test for PSQI ≥ 10 and PSQI ≤ 5.
Partial eta squared (.01-.08 is small, .09-.24 is medium, and .25+ is large).
Discussion
Our secondary analysis is the first examination of changes in sleep associated with participation in an MBSR program among a healthy sample of older adults with and without sleep disturbance, thus increasing generalizability to older adults in the United States for whom disturbed sleep is the most common and prevalent health problem. Our findings suggest that participation in MBSR is associated with improved sleep quality for older adults with moderate to high levels of sleep disturbance as measured by the PSQI.
The interaction of group and time on the PSQI global score for the entire sample suggests a significant and relatively small effect associated with participation in MBSR. Perhaps of more interest, is that among subsamples with elevated baseline PSQI scores, MBSR was associated with significant improvements in global sleep as compared with the WLC condition. This effect was most pronounced among participants whose global PSQI score was ≥ 10, a level of disturbance observed in patients with insomnia (Buysse et al., 2011; Buysse et al., 1989).
The statistically significant, but relatively small reduction in the global PSQI score (2.2 points) in the subsample of participants with PSQI scores > 5 may not reflect a clinically meaningful change. In one of the few RCTs of behavioral sleep interventions that reported PSQI scores, for instance, mean PSQI scores in the intervention arm (n = 39) declined 3.5 points from baseline to post-treatment (10.4 to 6.9; Buysse et al., 2011). In comparison, our subsample with the highest baseline PSQI scores achieved reductions from baseline PSQI scores of 3.4 and 3.9 points respectively at post-treatment and 6-month follow-up. Specifically, participants in the MBSR intervention with a global PSQI score ≥ 10 experienced a 3.4 point decrease from baseline (12.6) to post-treatment (9.2) with an additional reduction to 8.7 at the 6-month follow-up assessment. These results are consistent with the effects of mindfulness meditation on PSQI scores reported by Black et al. (2015), whose MBI among older adults aged > 55 with sleep disturbance improved by a mean of 2.8 (effect size, 0.89). Similar results were also found among older adults aged > 75 with insomnia in an MBSR program whose PSQI scores decreased from 11.5 at baseline to 8.2 at post-intervention, a 3.3 point decrease (effect size, 1.12; Zhang et al., 2015). The findings from our study support the hypothesis that MBSR would be associated with improved sleep quality for older adults with moderate to high levels of sleep disturbance.
MBSR is a promising intervention for older adults as it teaches skills to non-judgmentally observe cognitions and physiological and emotional arousal, which may help to diminish the sleep interfering processes associated with disturbed sleep. MBSR is designed to reduce stress, including hyperarousal, which can both contribute to and maintain sleep disturbance (Pigeon & Cribbet, 2012). Interventions designed to address sleep disturbance directly such as Cognitive-Behavioral Therapy for Insomnia (CBT-I) focus on reducing maladaptive thoughts and beliefs that interfere with sleep, but often include a relaxation component (Pigeon, 2010). Mindfulness addresses maladaptive thinking by instructing participants to allow thoughts into conscious awareness and to practice acceptance by making no attempt to change, suppress, or elaborate on the thought (Gross et al., 2011). Non-judgmental observation of physiological and emotional arousal may, therefore, help diminish the sleep interfering processes of hyperarousal associated with disturbed sleep.
Sleep disturbance and insomnia are also thought to be maintained through cognitive and behavioral activities that are initially triggered by psychosocial stress and perpetuated by attentional bias to sleep-related stimuli and behavioral adaptation resulting in conditioned effects (Pigeon & Cribbet, 2012). Mindfulness is the practice of attention regulation and non-reactivity, both of which help to diminish maladaptive cognitions that maintain disturbed sleep. Mindfulness works with attention regulation by instructing practitioners to focus on one object at a time, typically starting with the breath. This allows the practitioner to increase sustained attention and decrease attention to distracting thoughts or attentional bias to sleep-related stimuli. Over time, practitioners of mindfulness report an increased ability to maintain focus on the breath and are less distracted by disturbances (Hölzel et al., 2011). For older adults with moderate levels of sleep disturbance, returning attention back to the breath and away from sleep-related worry and attentional bias on daytime consequences of lack of sleep may reduce psychosocial stress associated with sleep disturbance. In practicing a mindful approach to cognitions and arousal, the MBSR participants learned to respond to stressors in an adaptive way, therefore improving their overall sleep quality by decreasing maladaptive responses to stress that maintained their disturbed sleep.
The study has several limitations worth noting. First, the study was not designed to directly improve sleep. Therefore, objective measures of sleep such as actigraphy or electroencephalogram-based measures were not included and the reliance on self-report may limit the reliability of the sleep outcomes. Second, the sample was not assessed with diagnostic interviews or validated screens for sleep apnea or insomnia. Thus, the nature of the sleep disturbance in this sample is undefined. Third, the findings are limited by the use of a WLC that did not receive any group-based support. Finally, the sample was limited in ethnic diversity, and therefore generalizing to non-Caucasian populations should be done with caution.
Conclusion
Although the study was not designed to directly improve sleep, the findings from this relatively large sample support observations in prior work that participation in MBSR may be associated with beneficial changes in sleep quality among older adults. Studies which directly examine the effect of MBSR on sleep among older adults, and include sleep diaries and objective measures of hyperarousal will be informative. Further, a comparative efficacy trial of participants with varying levels of sleep disturbance, for example, would be helpful in determining whether (and for whom) MBSR is a reasonable stand-alone intervention for sleep disturbance and/or a useful adjunctive therapy for sleep disturbance. In this regard, conducting an MBSR RCT with an active control for sleep disturbance and insomnia seems worthwhile.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study protocol was approved by the University of Rochester Institutional Review Board (RSRB00012363) and is registered with clinicaltrials.gov (NCT01027780). Study funding came from R01AG025474 (PI: Moynihan) and R24AG031089 (PI: Moynihan). Dr. Pigeon is supported, in part, by the United States Department of Veterans Affairs Center of Excellence for Suicide Prevention.
Biographies
Autumn M. Gallegos, PhD, is a senior instructor of psychiatry and clinical psychologist at the University of Rochester Medical Center (URMC). Her research explores the effects of mind–body interventions on posttraumatic stress symptoms among survivors of trauma. She is also an experienced Mindfulness-Based Stress Reduction (MBSR) instructor and teaches MBSR courses to faculty and staff of URMC.
Jan Moynihan, PhD, is the George L. Engel Professor of psychiatry at the URMC. Her research focuses on determining the consequences of life experiences and individual differences for immune function, and physical and mental health. She is currently most interested in interventions designed to ameliorate the deleterious effects of chronic life stress.
Wilfred R. Pigeon, PhD, is associate professor of psychiatry and Sleep Research Lab director at URMC and VA Center of Excellence for Suicide Prevention Research Director. His research focuses on the mechanisms, consequences, and treatment of sleep disturbance that co-occur with PTSD/trauma, depression/suicidality, and chronic pain as well as developing brief behavioral interventions to address these cooccurring conditions.
Footnotes
The authors’ views or opinions do not necessarily represent those of the Department of Veterans Affairs, the National Institutes of Health, or the United States Government.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Åkerstedt T, Knutsson A, Westerholm P, Theorell T, Alfredsson L, Kecklund G. Sleep disturbances, work stress and work hours: A cross-sectional study. Journal of Psychosomatic Research. 2002;53:741–748. doi: 10.1016/s0022-3999(02)00333-1. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bastien CH, Vallières A, Morin CM. Precipitating factors of insomnia. Behavioral Sleep Medicine. 2004;2:50–62. doi: 10.1207/s15402010bsm0201_5. [DOI] [PubMed] [Google Scholar]
- Black DS, O’Reilly GA, Olmstead R, Breen EC, Irwin MR. Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbances: A randomized clinical trial. JAMA Internal Medicine. 2015;175:494–501. doi: 10.1001/jamainternmed.2014.8081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Germain A, Moul DE, Franzen PL, Brar LK, Fletcher ME, … Monk TH. Efficacy of brief behavioral treatment for chronic insomnia in older adults. Archives of Internal Medicine. 2011;171:887–895. doi: 10.1001/archinternmed.2010.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index (PSQI): A new instrument for psychiatric research and practice. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. International Journal of Behavioral Medicine. 2005;12:278–285. doi: 10.1207/s15327558ijbm1204_9. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29:448–474. doi: 10.1016/s0306-4530(03)00054-4. [DOI] [PubMed] [Google Scholar]
- Chung KF, Yeung WF, Ho FY, Yung KP, Yu YM, Kwok CW. Cross-cultural and comparative epidemiology of insomnia: The Diagnostic and Statistical Manual (DSM), International Classification of Diseases (ICD) and International Classification of Sleep Disorders (ICSD) Sleep Medicine. 2015;16:477–482. doi: 10.1016/j.sleep.2014.10.018. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. New York, NY: Routledge; 2013. [Google Scholar]
- First MB, Spitzer R, Gibbon ML, Williams JBW. Structured clinical interview for DSM-IV-TR axis I disorders, research version, non-patient edition (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: Results of the 2003 National Sleep Foundation Sleep in America Survey. Journal of Psychosomatic Research. 2004;56:497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- Foulk MA, Ingersoll-Dayton B, Kavanagh J, Robinson E, Kales HC. Mindfulness-based cognitive therapy with older adults: An exploratory study. Journal of Gerontological Social Work. 2014;57:498–520. doi: 10.1080/01634372.2013.869787. [DOI] [PubMed] [Google Scholar]
- Greeson J, Garland EL, Black D. A transtherapeutic approach for transdiagnostic mental processes. In: Ie A, Ngnoumen CT, Langer EJ, editors. The Wiley Blackwell handbook of mindfulness. New York, NY: John Wiley; 2014. pp. 533–562. [Google Scholar]
- Gross CR, Kreitzer MJ, Reilly-Spong M, Wall M, Winbush NY, Patterson R, … Cramer-Bornemann M. Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: A randomized controlled clinical trial. EXPLORE: The Journal of Science and Healing. 2011;7:76–87. doi: 10.1016/j.explore.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidenreich T, Tuin I, Pflug B, Michal M, Michalak J. Mindfulness-based cognitive therapy for persistent insomnia: A pilot study. Psychotherapy and Psychosomatics. 2006;75:188–189. doi: 10.1159/000091778. [DOI] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6:537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Dell; 1990. [Google Scholar]
- Kreitzer M, Gross C, Ye X, Russas V, Treesak C. Longitudinal impact of mindfulness meditation on illness burden in solid-organ transplant recipients. Progress in Transplantation. 2005;15:166–172. doi: 10.1177/152692480501500210. [DOI] [PubMed] [Google Scholar]
- Moynihan JA, Chapman BP, Klorman R, Krasner MS, Duberstein PR, Brown KW, Talbot NL. Mindfulness-based stress reduction for older adults: Effects on executive function, frontal alpha asymmetry and immune function. Neuropsychobiology. 2013;68:34–43. doi: 10.1159/000350949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohayon MM. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Medicine Reviews. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Vecchierini MF. Normative sleep data, cognitive function and daily living activities in older adults in the community. Sleep. 2005;28:981–989. [PubMed] [Google Scholar]
- Ong JC, Ulmer CS, Manber R. Improving sleep with mindfulness and acceptance: A metacognitive model of insomnia. Behaviour Research and Therapy. 2012;50:651–660. doi: 10.1016/j.brat.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pigeon WR. Treatment of adult insomnia with cognitive-behavioral therapy. Journal of Clinical Psychology. 2010;66:1148–1160. doi: 10.1002/jclp.20737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pigeon WR, Cribbet MR. The pathophysiology of insomnia: From models to molecules (and back) Current Opinion in Pulmonary Medicine. 2012;18:546–553. doi: 10.1097/MCP.0b013e328358be41. [DOI] [PubMed] [Google Scholar]
- Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, Nissen C. The hyperarousal model of insomnia: A review of the concept and its evidence. Sleep Medicine Reviews. 2010;14:19–31. doi: 10.1016/j.smrv.2009.04.002. [DOI] [PubMed] [Google Scholar]
- Stranges S, Tigbe W, Gómez-Olivé FX, Thorogood M, Kandala NB. Sleep problems: An emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep. 2012;35:1173–1181. doi: 10.5665/sleep.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winbush NY, Gross CR, Kreitzer MJ. The effects of mindfulness-based stress reduction on sleep disturbance: A systematic review. EXPLORE: The Journal of Science and Healing. 2007;3:585–591. doi: 10.1016/j.explore.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Zhang JX, Liu XH, Xie XH, Zhao D, Shan MS, Zhang XL, … Cui H. Mindfulness-based stress reduction for chronic insomnia in adults older than 75 years: A randomized, controlled, single-blind clinical trial. EXPLORE: The Journal of Science and Healing. 2015;11:180–185. doi: 10.1016/j.explore.2015.02.005. [DOI] [PubMed] [Google Scholar]