Abstract
The patient was a 38-year-old Japanese woman who had been diagnosed with hereditary angioedema type I at 7 years of age based on her family history. She had undergone four pregnancies. She gave birth to a healthy baby girl after her first pregnancy and had reported few episodes of angioedema. However, she subsequently required abortions due to frequent angioedema episodes that occurred during her three subsequent pregnancies. Thus, our patient showed two clinical pregnancy courses. After treating her with C1-inhibitor concentrate, her symptoms of angioedema disappeared. The preventive use of C1 inhibitor concentrates should be considered in hereditary angioedema (HAE) patients with frequent angioedema attacks during pregnancy.
Keywords: hereditary angioedema, HAE, pregnancy, C1 inhibitor, replacement therapy
Introduction
Hereditary angioedema (HAE) was first described clinically by Quincke (1) and Osler (2). HAE is an uncommon autosomal dominant disease caused by a disorder of C1-inhibitor (C1-INH), which regulates bradykinin. It is associated with a quantitative (type I), or a functional (type II) C1-INH deficiency caused by mutations in SERPING1 of the C1-INH gene (3, 4). Thus, HAE patients suffer from recurrent angioedema attacks, which may be induced by physical or mental stress (3). Angioedema is characterized by recurrent episodes of subcutaneous and submucosal swelling, which affect the skin, the gastrointestinal tract, and the upper respiratory system, including the oropharynx (5).
In 2000, a third type of HAE was identified, characterized by the normal expression and function of C1-INH, by Bork et al. (6) and Binkley et al. (7). HAE type III, often referred to as HAE with a normal C1-INH function (HAE-nC1-INH), has recently been classified into two categories: one has mutations in the F12 gene, which encodes coagulation protein factor XII; the other that contains no currently known mutations (8-10). Angioedema in patients with HAE-nC1-INH is often estrogen dependent (11, 12), and is often triggered after the intake of oral contraceptives. Thus, there is a very close connection between angioedema attack and pregnancy.
We herein report on the frequency of angioedema attacks, both before and during a successful and unsuccessful pregnancy, in a patient with HAE type I.
Case Report
The patient was a 38-year-old Japanese woman who had been diagnosed with HAE type I at 7 years of age based on her family history. Her father and daughter were also diagnosed with HAE type I. She was introduced to our hospital at 25 years of age, and treatment with C1-INH concentrate was initiated to treat her recurrent angioedema attacks, which affected various body sites (neck, limbs and abdomen). Her symptoms disappeared after treatment with C1-INH concentrate. She had never taken oral contraceptives.
A laboratory evaluation revealed that the patient's CH50 and C4 levels were reduced to <13.0 U/mL (normal range: 30-45 U/mL) and 4 mg/dL (normal range: 10-40 mg/mL), respectively. Her C3 level was 90 mg/dL (normal range: 60-140 mg/mL) and within the normal range. In addition, her C1-INH protein level was reduced (5 mg/dL; normal: 21-39 mg/mL),while her C1-INH activity was markedly reduced (<25%; normal range: 70-130 %). Her C1q level (6.5 mg/dL; normal range: 8.8-15.3 mg/mL) was slightly reduced. Various antinuclear antibodies tests, including a test for anti-double stranded DNA antibodies, were negative. Although we did not perform a genetic investigation, we diagnosed the patient with HAE type I based on her family history.
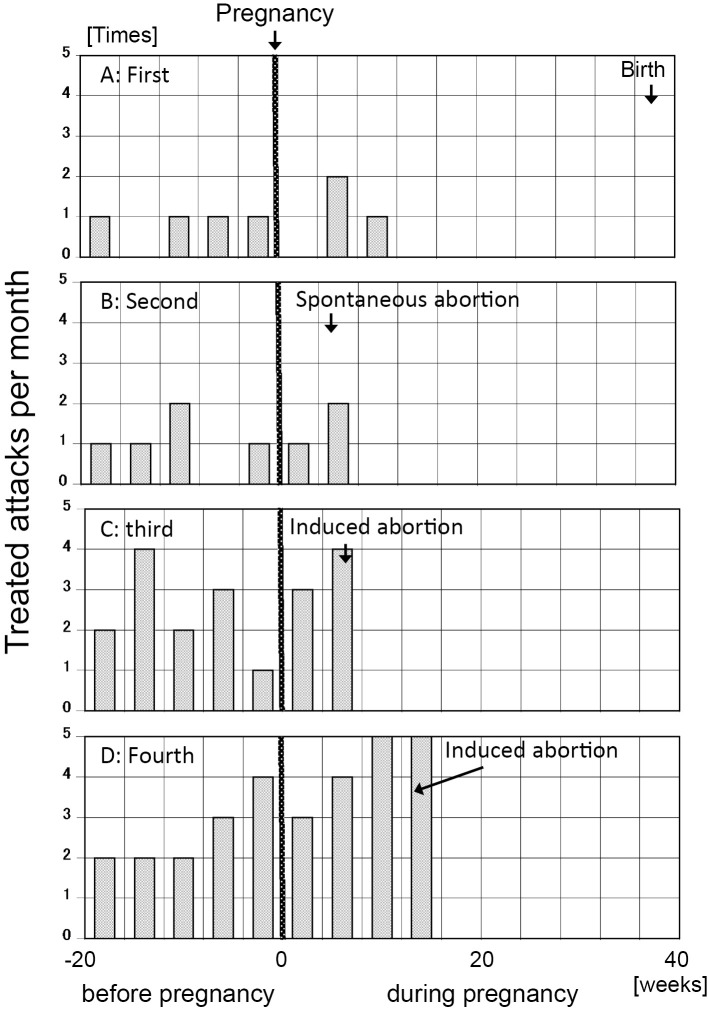
Our patient had four pregnancies. Before her first pregnancy at 29 years of age, she had a few episodes of angioedema of approximately one month in duration. The average numbers of angioedema attacks per month before and during her first pregnancy were 0.8 and 0.3, respectively. The attacks decreased after her first pregnancy (Fig. 1A). She gave birth to a healthy baby girl by cesarean section in her first pregnancy at 37 weeks and 4 days of gestation.
Figure 1.
The number of treated HAE attacks before and during pregnancy. The average numbers of treated angioedema attacks per month before and during her first pregnancy were 0.8 and 0.3, respectively (A). The average numbers of treated angioedema attacks per month before and during her second pregnancy were 1 and 1.5, respectively (B). The average numbers of treated angioedema attacks per month before and during her third pregnancy were 2.4 and 3.5, respectively (C). The average numbers of treated angioedema attacks per month before and during her fourth pregnancy were 2.6 and 4.2, respectively (D).
She had a second pregnancy at 32 years of age. The average numbers of angioedema attacks per month before and during her second pregnancy were 1 and 1.5, respectively. The frequency of angioedema attacks increased slightly during her second pregnancy relative to the period before (Fig. 1B). She had a spontaneous abortion at 5 weeks and 1 day of gestation after abdominal pain due to an angioedema attack.
She had a third pregnancy at 34 years of age. The average numbers of angioedema attacks before and during her third pregnancy were 2.4 and ≥3.5, respectively. The frequency of angioedema attacks increased during her third pregnancy relative to before her third pregnancy (Fig. 1C). The large number of angioedema attacks meant that she could not continue her pregnancy; thus, she had an induced abortion at 8 weeks and 5 days of gestation.
She had a fourth pregnancy at 35 years of age. The average numbers of angioedema attacks before and during her fourth pregnancy were 2.6 (similar to the number in her third pregnancy) and 4.2, respectively. The frequency of angioedema attacks during her fourth pregnancy was higher than in comparison to before her fourth pregnancy (Fig. 1D). Once again, she could not continue the pregnancy due to the large number of angioedema attacks and had an induced abortion at 16 weeks and 2 days of gestation.
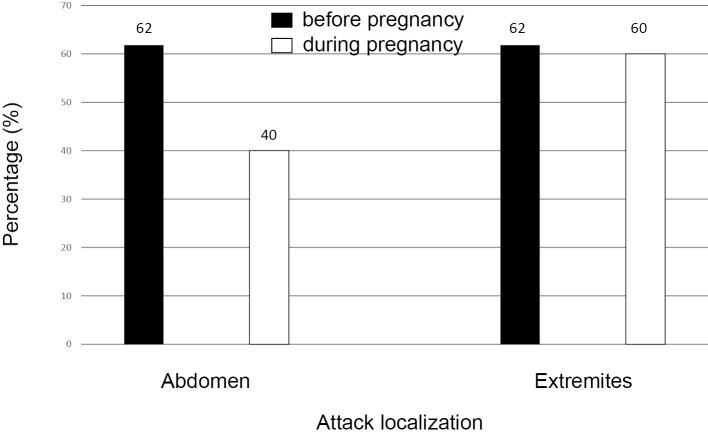
During the six months preceding the pregnancy abdominal edema was the most common occurrence (62%); it occurred either as isolated abdominal attacks (38%) or as combined attacks (24%) that involved simultaneous edema formation in the abdomen and on her extremities (Fig. 2). Eighteen of 30 attacks that occurred during her pregnancy occurred on the extremities (60%), the other attacks (40%) occurred in the abdomen. All of her attacks during pregnancy were isolated. Thirteen of the 34 attacks before her pregnancy occurred on the extremities (38%). Other attacks (62%) occurred in the abdomen, these included attacks that were combined with swelling of the extremities. The rates of edema in the abdomen and extremities before and during pregnancy did not differ to a statistically significant extent (p=0.382, χ2-test).
Figure 2.
The distribution of the treated HAE attacks before and during pregnancy. 18 out of 30 attacks during her pregnancy occurred on the extremities (60%); whilst the other attacks (40%) occurred in the abdomen. 13 out of 34 attacks before her pregnancy occurred on the extremities (38%); the other attacks (62%) occurred either as isolated abdominal attacks (38%) or as combined attacks (24%) that involved simultaneous edema formation in the abdomen and on the extremities.
Discussion
It was difficult for us to predict the frequency of angioedema attacks during the pregnancies of our patient with a type I hereditary angioedema due to C1-INH deficiency. The patient followed various clinical courses during her pregnancy. The angioedema attacks in her first pregnancy were uneventful. In her second, third and fourth pregnancies, she suffered more angioedema attacks during pregnancy than before pregnancy. The stress caused by caring for her first child may have contributed to this. Czaller et al. reported (13) that pregnancy can either aggravate or mitigate angioedematous attacks. González-Quevedo et al. reported (14) that the frequency of angioedema attacks was increased in 59.2% of pregnancies. The influence of pregnancy on the severity of HAE may even change in different pregnancies within the same woman (13, 15, 16). Women are generally considered to have a more severe disease course than men (5). Between 60% and 80% of women with HAE type I and II who use oral contraceptive pills containing estrogen are reported to show an increase in both the frequency and severity of attacks (17-20); thus, exposure to estrogen is considered to promote the clinical attacks of HAE (5). Periods of pregnancy and lactation are associated with an increased number of angioedema attacks (5). Thus, our patient might have been expected to suffer from more angioedema attacks during pregnancy. Hermans reported (21) that a patient with HAE suffered from more angioedema attacks during her second pregnancy than during her first pregnancy. Patients with early-onset angioedema attacks due to C1-INH deficiency have a more severe disease course in comparison to patients with a late-onset disease (5). Especially during pregnancy, the onset of clinical attacks early in life is associated with more frequent and more severe attacks (5, 13). Our patient suffered from angioedema attacks from 7 years of age, which could have led her to have more frequent and more severe attacks, including during pregnancy.
The administration of C1-INH concentrates to pregnant women is not established in Japan. Thus, C1-INH concentrate may be administered when it is judged that the therapeutic benefit exceeds the risk. Czaller et al. reported (13) that C1-INH concentrate is a safe and effective therapeutic option during pregnancy. Our patient did not report any side effects as a result of the administration of C1-INH concentrate (BerinertⓇ, CSL Behring, Pennsylvania, USA) and it was an effective therapy for controlling her angioedema attacks due to HAE during pregnancy. The indication for the administration of C1-INH concentrates to prevent angioedema episodes during pregnancy are not clear in the social insurance system of the Ministry of Health, Labour and Welfare of Japan. We have recently been advised that that the short-term prophylactic administration of C1-INH concentrate (BerinertⓇ) within six hours before the extraction of teeth is approved in Japan. In Europe, Canada and the USA, recent license changes to some HAE therapies have provided excellent opportunities for more patients to switch to self-administered therapy (22-30). The early administration of C1-INH concentrate (BerinertⓇ) and a bradykinin receptor blocker (Icatibant) has been shown to reduce the duration of acute angioedema attacks (31). The home-based self-administration of HAE therapy permits rapid treatment in the early stages of an angioedema attack and has been shown to reduce their duration (32). Squeglia et al. reported (33) that compliance to therapy was significantly better among patients who received home-based therapy (71.2% and 44.0% of attacks were with C1-INH concentrates and bradykinin receptor blockers, respectively) in comparison to patients who received hospital-based therapy (21.6%, p=0.003). Thus, they conclude that home-based therapy should be offered, especially to patients who experience frequent attacks. In Japan, recurrent attacks of angioedema are a frequent cause of visits to the emergency department and are treated in hospital. According to the Japanese guideline for hereditary angioedema, we should prescribe tranexamic acid or danazol as long-term prophylaxis (34). One pregnant woman was reported to have been prescribed tranexamic acid, and danazol was contraindicated in another (35). Our patient had refused to take either tranexamic acid or danazol since she was admitted to our hospital. Thus, we could not prescribe tranexamic acid for long-term prophylaxis. However, the treatment for patients with frequent and/or severe attacks involves the use C1-INH concentrates (13, 21, 34). Our patient, who experienced frequent attacks, would have been well suited to home-based therapy, which is approved in Europe, Canada and the USA. In the future, we hope that we will be able to prescribe the self-administration of C1-INH concentrates and bradykinin receptor blockers.
With regard to the localization of angioedema attacks, Czaller et al. reported (13) that the frequency of abdominal edema was significantly higher during pregnancy. This was not the case in our patient. Each of her angioedema attacks during pregnancy was isolated to the abdomen or extremities. However, her angioedema attacks before pregnancy were isolated to both her abdomen and extremities (79.4%) and a combination of the two (20.6%). During the early stages of her angioedema attacks during her pregnancy, it might have been more efficient to treat the patient in a hospital
Conclusion
Self-administered C1 inhibitor concentrate and bradykinin receptor blocker therapy (including prophylactic treatment), is becoming the standard therapy in developed countries, including Europe, Canada and the USA. In the future, we hope that we will be able to prescribe C1 inhibitor concentrates to prevent angioedema attacks in HAE in patients who have a high attack frequency during pregnancy.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Quincke HI. Über akutes umschriebenes Hautödem. Monatsh Prakt Dermatol 1: 129-131, 1882. [Google Scholar]
- 2.Osler W. Hereditary angioneurotic edema. Am J Med Sci 95: 362-367, 1888. [Google Scholar]
- 3.Cicardi M, Agostoni A. Hereditary angioedema. N Engl J Med 334: 1666-1667, 1996. [DOI] [PubMed] [Google Scholar]
- 4.Craig T, Aygören-Pürsün E, Bork K, et al. . WAO guideline for the management of hereditary angioedema. World Allergy Organ J 5: 182-199, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bork K, Meng G, Staubach P, Hardt J. Hereditary angioedema: new findings concerning symptoms, affected organs, and course. Am J Med 119: 267-274, 2006. [DOI] [PubMed] [Google Scholar]
- 6.Bork K, Barnstedt SE, Koch P, Traupe H. Hereditary angioedema with normal C1-inhibitor activity in women. Lancet 356: 213-217, 2000. [DOI] [PubMed] [Google Scholar]
- 7.Binkley KE, Davis A 3rd. Clinical, biochemical, and genetic characterization of a novel estrogen-dependent inherited form of angioedema. J Allergy Clin Immunol 106: 546-550, 2000. [DOI] [PubMed] [Google Scholar]
- 8.Bork K. Hereditary angioedema with normal C1 inhibition. Curr Allergy Asthma Rep 9: 280-285, 2009. [DOI] [PubMed] [Google Scholar]
- 9.Bowen T, Cicardi M, Farkas H, et al. . 2010 International consensus algorithm for the diagnosis, therapy and management of hereditary angioedema. Allergy Asthma Clin Immunol 6: 24, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cicardi M, Aberer W, Banerji A, et al. . HAWK under the patronage of EAACI (European Academy of Allergy and Clinical Immunology). Classification, diagnosis, and approach to treatment for angioedema: consensus report from the Hereditary Angioedema International Working Group. Allergy 69: 602-616, 2014. [DOI] [PubMed] [Google Scholar]
- 11.Vitrat-Hincky V, Gompel A, Dumestre-Perard C, et al. . Type III hereditary angio-oedema: clinical and biological features in a French cohort. Allergy 65: 1331-1336, 2010. [DOI] [PubMed] [Google Scholar]
- 12.Craig TJ, Bernstein JA, Farkas H, Bouillet L, Boccon-Gibod I. Diagnosis and treatment of bradykinin-mediated angioedema: outcomes from an angioedema expert consensus meeting. Int Arch Allergy Immunol 165: 119-127, 2014. [DOI] [PubMed] [Google Scholar]
- 13.Czaller I, Visy B, Csuka D, et al. . The natural history of hereditary angioedema and the impact of treatment with human C1-inhibitor concentrate during pregnancy: a long-term survey. Eur J Obstet Gynecol Reprod Biol 152: 44-49, 2010. [DOI] [PubMed] [Google Scholar]
- 14.González-Quevedo T, Larco JI, Marcos C, et al. . Management of pregnancy and delivery in patients with hereditary angioedema due to C1 inhibitor deficiency. J Investig Allergol Clin Immunol 26: 161-167, 2016. [DOI] [PubMed] [Google Scholar]
- 15.Caballero T, Canabal J, Rivero-Paparoni D, Cabañas R. Management of hereditary angioedema in pregnant women: a review. Int J Womens Health 6: 839-848, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Caballero T, Farkas H, Bouillet L, et al. . C-1-INH Deficiency Working Group. International consensus and practical guidelines on the gynecologic and obstetric management of female patients with hereditary angioedema caused by C1 inhibitor deficiency. J Allergy Clin Immunol 129: 308-320, 2012. [DOI] [PubMed] [Google Scholar]
- 17.Bork K, Fischer B, Dewald G. Recurrent episodes of skin angioedema and severe attacks of abdominal pain induced by oral contraceptives or hormone replacement therapy. Am J Med 114: 294-298, 2003. [DOI] [PubMed] [Google Scholar]
- 18.Yip J, Cunliffe WJ. Hormonally exacerbated hereditary angioedema. Australas J Dermatol 33: 35-38, 1992. [DOI] [PubMed] [Google Scholar]
- 19.Bouillet L, Longhurst H, Boccon-Gibod I, et al. . Disease expression in women with hereditary angioedema. Am J Obstet Gynecol 199: e1-e4, 2008. [DOI] [PubMed] [Google Scholar]
- 20.Borradori L, Marie O, Rybojad M, et al. . Hereditary angioedema and oral contraception. Dermatologica 181: 78-79, 1990. [DOI] [PubMed] [Google Scholar]
- 21.Hermans C. Successful management with C1-inhibitor concentrate of hereditary angioedema attacks during two successive pregnancies: a case report. Arch Gynecol Obstet 276: 271-276, 2007. [DOI] [PubMed] [Google Scholar]
- 22.Caballero T, Sala-Cunill A, Cancian M, et al. . Current status of implementation of self-administration training in various regions of Europe, Canada and the USA in the management of hereditary angioedema. Int Arch Allergy Immunol 161 (Suppl 1): 10-16, 2013. [DOI] [PubMed] [Google Scholar]
- 23. CSL Behring: CSL Behring Receives European Health Authorities’ Approval for Self-Administration of BerinertⓇ [Internet]. 2011 [cited 2017 Feb. 8] . Available from: https://www.ots.at/presseaussendung/OTE_20110825_OTE0010/csl-behring-receives-european-health-authorities-approval-for-self-administration-of-berinert .
- 24. CSL Behring Receives FDA Approval of Expanded Label on BerinertⓇ for Self-administration and Treatment of Acute Laryngeal Attacks of Hereditary Angioedema. CSL Behring Newsroom : News Archives 2012 [Internet]. [cited 2017 Feb. 8] . Available from: https://www.cslbehring.com/vita/newsroom .
- 25. ViroPharma Inc.: ViroPharma's CinryzeⓇ (C1 inhibitor [human]) granted European marketing authorization for hereditary angioedema (HAE) [Internet]. 2011 [cited 2017 Feb. 8] . Available from: https://www.prnewswire.com/news-releases/viropharmas-cinryze-c1-inhibitor-human-granted-european-marketing-authorization-for-hereditary-angioedema-hae-123912304.html .
- 26. Pharmiweb.com: European Commission approves self-administration label for FirazyrⓇ (icatibant) for the symptomatic treatment of acute hereditary angioedema attacks [Internet]. 2011 [cited 2017 Feb. 8] . Available from: https://www.prnewswire.com/news-releases/european-commission-approves-self-administration-label-for-firazyrr-icatibant-for-the-symptomatic-treatment-of-acute-hereditary-angioedema-attacks-117306118.html .
- 27. Food and Drug Administration: FDA approves Firazyr to treat acute attacks of hereditary angioedema [Internet]. 2011 [cited 2017 Feb. 8] . Available from: https://www.fiercepharma.com/pharma/fda-approves-firazyr-to-treat-acute-attacks-of-hereditary-angioedema .
- 28. CSL Behring: CSL Behring receives European Health Authorities' approval of BerinertⓇ for short-term prophylaxis in adults and children [Internet]. 2013 [cited 2017 Feb. 8] . Available from: https://www.prnewswire.com/news-releases/csl-behring-receives-european-health-authorities-approval-of-berinert-for-short-term-prophylaxis-in-adults-and-children-203186131.html .
- 29. CSL Behring: CSL Behring received MHRA approval for self-administration of BerinertⓇ (C1 esterase inhibitor, human) [Internet]. 2012 [cited 2017 Feb. 8] . Available from: https://www.medicines.org.uk/emc/product/7043 .
- 30. ViroPharma Inc.: ViroPharma receives Complete Response letter for CinryzeTM supplemental Biologics License Application for acute treatment of hereditary angioedema [Internet]. 2009 [cited 2017 Feb. 8] . Available from: http://files.shareholder.com/downloads/ABEA-4ZUL1I/0x0x434585/5891844f-9fc3-4f9b-930f-4ae179fa4e46/VPHM_News_2009_6_4_General_Releases.pdf .
- 31.Maurer M, Aberer W, Bouillet L, et al. . IOS Investigators: Hereditary angioedema attacks resolve faster and are shorter after early icatibant treatment. PLoS ONE 8: e53773, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Levi M, Choi G, Picavet C, Hack CE. Self-administration of C1-inhibitor concentrate in patients with hereditary or acquired angioedema caused by C1-inhibitor deficiency. J Allergy Clin Immunol 117: 904-908, 2006. [DOI] [PubMed] [Google Scholar]
- 33.Squeglia V, Barbarino A, Bova M, et al. . High attack frequency in patients with angioedema due to C1-inhibitor deficiency is a major determinant in switching to home therapy: a real-life observational study. Orphanet J Rare Dis 11: 133, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Horiuchi T, Ohi H, Ohsawa I, et al. . Guideline for hereditary angioedema (HAE) 2010 by the Japanese Association for Complement Research - secondary publication. Allergol Int 61: 559-562, 2012. [DOI] [PubMed] [Google Scholar]
- 35.Lindoff C, Rybo G, Astedt B. Treatment with tranexamic acid during pregnancy, and the risk of thrombo-embolic complications. Thromb Haemost 70: 238-240, 1993. [PubMed] [Google Scholar]