Abstract
BACKGROUND:
During the examination of the sellar region by magnetic resonance imaging, hyperintensity in T1 weighted is a common finding. This signal intensity has different sources, and its significance depends on the clinical context. Pathologic variations in T1 signal hyperintensity may be related to clotting of blood (pituitary apoplexy) or the presence of a high concentration of protein (Rathke cleft cyst). The purpose of this study is to describe the significance of intracystic nodule, a diagnostic characteristic found in Rathke’s cleft cyst, on MRI.
CASE REPORT:
We will present the case of a 20–year-old girl which referral to our hospital for head examination with magnetic resonance imaging because she has a post-traumatic headache. Pathological findings presented in T1-weighted hyperintensity intrasellar which persist even in T1 weighted-Fat suppression. These changes signal the presence of methemoglobin imposes. The patient is a referral to laboratory tests which result in rate except for slight value increase of prolactin. Recommended controller examination after a month but finding the same results which exclude the presence of methemoglobin.
CONCLUSION:
Morphological characteristics and signal intensity can impose the presence of high concentration of protein (Rathke cleft cyst).
Keywords: Rathke Cleft Cyst, Apoplexy, MRI, T1-weighted
Introduction
Rathke cleft cysts (RCC’s) are benign lesions that typically arise within the sella between the anterior and posterior lobes of the pituitary [1]. In 1913 the Goldzieher described the first case of RCC as an incidental postmortem finding. The description of RCC has expanded since the advent of computed tomography (CT) scanning and magnetic resonance imaging (MRI), showing that the incidence of this disease which discovery was only by autopsy was underestimated. Most often asymptomatic, RCCs have been found incidentally in 4% to 33% of autopsies [2] [3] [4] [5]. These lesions, however, can cause mass effect on surrounding structures such as the pituitary gland and optic chiasm, leading to a headache, pituitary dysfunction, or visual disturbance [6] [7] [8]. The epithelium is often ciliary and may contain bowl-shaped cells. The content of a cyst is usually mucous, and less frequently, it is filled with exudates or remnants of exfoliated cells. Rathke cleft cysts are remnants of the Rathke pouch, a structure of ectodermic origin formed during the fourth week of gestation. The Rathke pouch extends caudally to fuse with the infundibulum around the eighth week of gestation, forming the craniopharyngeal duct. The Rathke pouch then leads to the formation of the adenohypophysis and pars intermedia while the infundibulum generates the neurohypophysis. During this time, the Rathke cleft is formed in the region of the pars intermedia. Failure of this cleft to regress during further development can lead to cystic dilation and the formation of an RCC [1] [2] [3] [4] [5] [6]. Larger RCCs can extend upward into the suprasellar region, and comparisons of symptomatic and asymptomatic lesions have suggested that large size and suprasellar extension of RCCs may be associated with a greater tendency toward symptomatic presentation [9] [10]. Although most RCCs originate in the sella, there have been reports of purely suprasellar RCCs. Calcifications of the cyst walls are rarely observed. Although asymptomatic RCCs can safely be followed up with serial imaging, the standard treatment for symptomatic RCCs is surgical decompression, typically through a transsphenoidal approach.
Symptomatic patients have RCCs usually manifest headaches. One such case is reported. The author also reviews published reports on RCCs presented like apoplexy and described radiological characteristics of this rare entity.
This work aims to emphasise the value of MRI in the positive and differential diagnosis of this disease through a case of Rathke’s cleft cyst with a literature review.
Case Report
We are presenting the case of a 20 – year - old girl, on referral to our hospital for head examination with magnetic resonance imaging because she has a post-traumatic headache. The patient was cooperative but slightly confused. Neurological examination revealed no focal deficit including oculomotor palsy or visual field defect, and there was no evidence of neck stiffness
The patient underwent magnetic resonance (MR) imaging of the sella with and without contrast injection. Pathological findings presented heterogeneous signal intensity in T2 - weighted and T1 - weighted hyperintensity intrasellar pituitary which persists even in T1 weighted - Fat suppression. The lesion is with an anteroposterior diameter (AP) 7 mm and craniocaudal (CC) 9 mm which is located at the posterior part of the adenohypophysis (Figure 1), while the pituitary gland has dimensions in AP diameter 13 mm and CC diameter 10 mm. There are no signs of compression on the chiasma opticum although it arrives very close.
Figure 1.
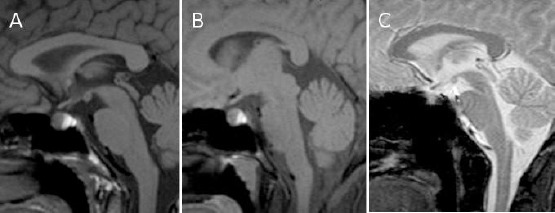
The first examination, magnetic resonance images of a patient presented: The lesion is isointense with hyperintensity on T1 - weighted images and T1 weighted - Fat suppression (A and B). Heterogeneous signal intensity on the T2*weighted image (C)
This increased signal intensity has different sources and is given importance when interpreting the depending on the clinic of imaging findings.
These findings suggested the presence of haemorrhage in a pituitary adenoma, the presence of methemoglobin impose. The patient is a referral to laboratory tests which result in rate except for slight value increase of prolactin (35 ng/ml), and we recommended controller examination after a month but finding the same results which exclude the presence of methemoglobin. Morphological characteristics and signal intensity to impose the presence of high concentration of protein (Rathke cleft cyst) (Figure 2).
Figure 2.
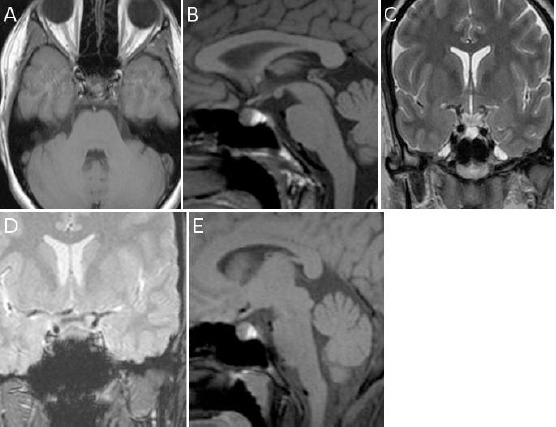
The first examination, magnetic resonance images of a patient presented: The lesion is isointense with hyperintensity on T1 - weighted images axial (A) and sagittal (B), hyperintensity in T1 weighted- Fat suppression (E) and T2 - weighted image (C), while heterogeneous signal intensity on T2*weighted image (D)
Discussion
Rathke’s cleft cysts (RCC) are well - delineated structures that vary in size from several millimetres to 1 – 2 cm. They are found in less than 1% of primary brain tumours. In most cases, RCC is small, asymptomatic mass lesions located in the intrasellar or the intrasuprasellar space [9]. RCC may be seen at any age; however, they are more frequent in adults.
In 1913, Goldzieher described the first case of RCC as an incidental postmortem finding. Rathke cleft cysts are thought to be non - obliterated remnants of the primitive craniopharyngeal duct, which is a part of the Rathke pouch. In the superoinferior plane, RCCs are usually located entirely within the sella or contain both intrasellar and suprasellar components. In the anterior-posterior plane, RCCs typically reside between the pars anterior and pars intermedia of the pituitary gland. Purely suprasellar RCCs situated above a normal sella are rare. The Rathke pouch gives rise to the pars distalis (anterior lobe) and pars intermedia (intermediate lobe) in the sella, as well as the pars tuberalis, a structure that resides above the anterior lobe and the diaphragm sella in the suprasellar cistern. It is therefore thought that purely suprasellar RCCs arise from a remnant of the Rathke pouch within the pars tuberalis in the suprasellar cistern [11] [12] [13].
MRI is the modality of choice for the detection of RCCs [14]. Thin - section sagittal and coronal MRI scans should be obtained through the sella. MRI is superior to CT scanning for evaluating RCC mass extension. Sagittal and coronal MRI scans provide reliable information concerning the relationship of the mass to the optic nerves, optic chiasma and hypothalamus. Coronal MRI is also helpful in the evaluation of the lateral extension of the sellar cyst and its relationship to the internal carotid arteries and cavernous sinuses. MRI also has superior multiplane capabilities and contrast resolution compared with those of CT scanning. The advantage of CT scanning is that it is superior to MRI in depicting small amounts of calcium. This advantage can be important because the presence of calcification tends to indicate an alternative diagnosis, such as craniopharyngioma, although small calcifications are observed in some cases of RCC [15].
CT scanning is also superior to MRI in the evaluation of associated bony remodelling and in depicting small amounts of calcium. Coronal MRI is also helpful in the evaluation of the lateral extension of the sellar cyst and its relationship to the internal carotid arteries and cavernous sinuses. MRI also has superior multi-plane capabilities and contrast resolution compared with those of CT scanning.
The best imaging clue is a non - enhancing non - calcified intrasellar and/or suprasellar cyst with an intracystic nodule. While this is the typical picture, the imaging characteristics vary widely.
Approximately half are hyperintense on T1WI, while half are hypointense. On T2WI, 70% are hyperintense, and 30% are isointense or hypointense. Although no characteristic MRI features have been identified, many RCCs are in one of the following two groups:
RCC’s with low signal intensity on T1WI and high signal intensity on T2WI. RCC’s with high signal intensity on T1WI and variable signal intensity on T2WI.
The cystic contents of the first group resemble those of cerebrospinal fluid (CSF). In the second group, an increase in the signal on T1WI has been related to the high content of mucopolysaccharides, which is believed to result from an increase in the number of mucin-secreting cells in the cyst wall, as well as from an increase in the activity of these cells. Rathke cleft cysts do not enhance after contrast material administration, although an enhancing rim of the displaced compressed pituitary gland is present in approximately half of the cases [16].
Forty percentages of RCCs are intrasellar, and 60% are a suprasellar stretch, while rarer are cases with complete suprasellar stretch. Our case is an intrasellar stretch (type I).
The most common approach in the treatment of RCCs is transsphenoidal surgery, in which the cyst is partially excised and drained [17].
The purpose of this study is to describe the significance of intracystic nodule, a diagnostic characteristic found in Rathke’s cleft cyst, on MRI
In conclusion, authors report a rare case of asymptomatic RCC which was presented with hyperintensity in T1 – weight, like pituitary apoplexy. It is hard to differentiate Rathke Cleft Cysts apoplexy from RCCs with hight protein concentration based only MRI image. RCCs should be considered if a patient has symptoms of apoplexy. The MRI is effective in the positive and especially the differential diagnosis of these cysts, and to guide the therapeutic decision. Once the diagnosis is considered, a spaced clinical and MRI monitoring is adopted in cases of the asymptomatic cyst, while a surgical treatment is proposed for the rare symptomatic cysts.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Prabhu VC, Brown HG. The pathogenesis of craniopharyngiomas. Childs Nerv Syst. 2005;21(8-9):622–627. doi: 10.1007/s00381-005-1190-9. https://doi.org/10.1007/s00381-005-1190-9. PMid:15965669. [DOI] [PubMed] [Google Scholar]
- 2.Shanklin WM. On the presence of cysts in the human pituitary. Anat Rec. 1949;104(4):379–407. doi: 10.1002/ar.1091040402. https://doi.org/10.1002/ar.1091040402. PMid:18143226. [DOI] [PubMed] [Google Scholar]
- 3.Fager CA, Carter H. Intrasellar epithelial cysts. J Neurosurg. 1966;24(1):77–81. doi: 10.3171/jns.1966.24.1.0077. https://doi.org/10.3171/jns.1966.24.1.0077. PMid:5903300. [DOI] [PubMed] [Google Scholar]
- 4.McGrath P. Cysts of sellar and pharyngeal hypophyses. Pathology. 1971;3(2):123–131. doi: 10.3109/00313027109071331. https://doi.org/10.3109/00313027109071331. PMid:5094869. [DOI] [PubMed] [Google Scholar]
- 5.Teramoto A, Hirakawa K, Sanno N, Osamura Y. Incidental pituitary lesions in 1,000 unselected autopsy specimens. Radiology. 1994;193(1):161–164. doi: 10.1148/radiology.193.1.8090885. https://doi.org/10.1148/radiology.193.1.8090885. PMid:8090885. [DOI] [PubMed] [Google Scholar]
- 6.Aho CJ, Liu C, Zelman V, Couldwell WT, Weiss MH. Surgical outcomes in 118 patients with Rathke cleft cysts. J Neurosurg. 2005;102(2):189–193. doi: 10.3171/jns.2005.102.2.0189. https://doi.org/10.3171/jns.2005.102.2.0189. PMid:15739543. [DOI] [PubMed] [Google Scholar]
- 7.Benveniste RJ, King WA, Walsh J, Lee JS, Naidich TP, Post KD. Surgery for Rathke cleft cysts: technical considerations and outcomes. J Neurosurg. 2004;101(4):577–584. doi: 10.3171/jns.2004.101.4.0577. https://doi.org/10.3171/jns.2004.101.4.0577. PMid:15481709. [DOI] [PubMed] [Google Scholar]
- 8.Zada G, Lin N, Ojerholm E, Ramkissoon S, Laws ER. Craniopharyngioma and other cystic epithelial lesions of the sellar region: a review of clinical, imaging, and histopathological relationships. Neurosurg Focus. 2010;28(4):E4. doi: 10.3171/2010.2.FOCUS09318. https://doi.org/10.3171/2010.2.FOCUS09318. PMid:20367361. [DOI] [PubMed] [Google Scholar]
- 9.Voelker JL, Campbell RL, Muller J. Clinical, radiographic, and pathological features of symptomatic Rathke’s cleft cysts. J Neurosurg. 1991;74(4):535–544. doi: 10.3171/jns.1991.74.4.0535. https://doi.org/10.3171/jns.1991.74.4.0535. PMid:2002366. [DOI] [PubMed] [Google Scholar]
- 10.Sade B, Albrecht S, Assimakopoulos P, Vezina JL, Mohr G. Management of Rathke’s cleft cysts. Surg Neurol. 2005;63(5):459–466. doi: 10.1016/j.surneu.2004.06.014. https://doi.org/10.1016/j.surneu.2004.06.014. PMid:15883073. [DOI] [PubMed] [Google Scholar]
- 11.Barrow DL, Spector RH, Takei Y, Tindall GT. Symptomatic Rathke’s cleft cysts located entirely in the suprasellar region: review of diagnosis, management, and pathogenesis. Neurosurgery. 1985;16(6):766–772. doi: 10.1227/00006123-198506000-00005. https://doi.org/10.1227/00006123-198506000-00005. PMid:4010898. [DOI] [PubMed] [Google Scholar]
- 12.Itoh J, Usui K. Anentirely suprasellar symptomatic Rathke’s cleft cyst: case report. Neurosurgery. 1992;30(4):581–584. PMid:1584358. [PubMed] [Google Scholar]
- 13.Wenger M, Simko M, Markwalder R, Taub E. An entirely suprasellar Rathke’s cleft cyst: case report and review of the literature. J Clin Neurosci. 2001;8(6):564–567. doi: 10.1054/jocn.2000.0925. https://doi.org/10.1054/jocn.2000.0925. PMid:11683607. [DOI] [PubMed] [Google Scholar]
- 14.Rathke’s cleft cyst: computed tomographic scan and magnetic resonance imaging. Nakasu Y, Isozumi T, Nakasu S, Handa J. Acta Neurochir (Wien) 1990;103(3-4):99–104. doi: 10.1007/BF01407513. https://doi.org/10.1007/BF01407513. [DOI] [PubMed] [Google Scholar]
- 15.Le BH, Towfighi J, Kapadia SB, et al. Comparative immunohistochemical assessment of craniopharyngioma and related lesions. Endocr Pathol. 2007;18:23–30. doi: 10.1007/s12022-007-0011-y. https://doi.org/10.1007/s12022-007-0011-y. [DOI] [PubMed] [Google Scholar]
- 16.V Naik VD, Thakore NR. A case of symptomatic Rathke’s cyst. BMJ Case Rep 2013. 2013 doi: 10.1136/bcr-2012-006943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cavallo LM, Prevedello D, Esposito F, et al. The role of the endoscope in the transsphenoidal management of cystic lesions of the sellar region. Neurosurg Rev. 2008;31:55–64. doi: 10.1007/s10143-007-0098-0. https://doi.org/10.1007/s10143-007-0098-0. PMid:17922153. [DOI] [PubMed] [Google Scholar]


