Practical Implications
An atrial esophageal fistula should be considered in a patient who presents with neurologic complications after catheter ablation for atrial fibrillation. Chest CT is the preferred mode of evaluation. Early identification and treatment is crucial to survival.
Atrial-esophageal fistulas, a rare potential complication of ablative procedures for atrial fibrillation (AFib), can have neurologic symptoms as well as bacteremia and cardiac complications.1 Prior reported neurologic symptoms include encephalopathy, seizures, TIA, septic embolic stroke, and air emboli.2 We report a patient whose spinal cord inflammation on pathology is suggestive of septic emboli.
Case report
We report a 62-year-old man with a medical history of hypertension, diabetes, and AFib (on apixaban) who underwent radiofrequency catheter ablation 2 months prior. The patient presented with left-sided hemiparesis, malaise, and chills, and received tissue plasminogen activator (tPA) after the initial head CT was negative for hemorrhage. He was subsequently transferred to our institution an hour after tPA infusion.
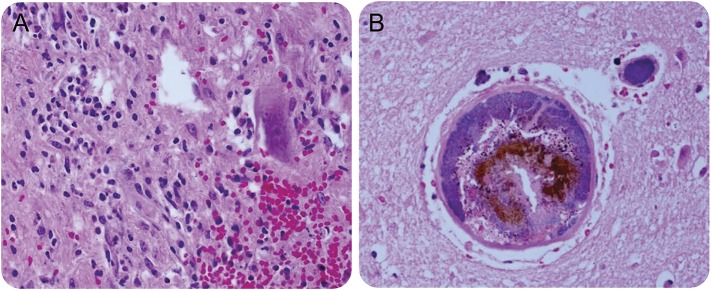
On initial presentation, the patient was afebrile and had a normal leukocyte count. AFib was noted on ECG. Head CT on arrival demonstrated a small volume of hemorrhage in the bilateral high convexities. No aneurysms were noted on vessel imaging. He received aminocaproic acid for the reversal of tPA given persistent coagulopathy in the setting of intracerebral bleeds. The patient had worsening mental status soon after and head CT demonstrated a new left cerebellar hemorrhage. While in the intensive care unit, he developed respiratory failure requiring mechanical ventilation and a flaccid quadriplegia. Head CT repeated 11 hours after presentation showed a right frontal mid convexity epidural hematoma, with unchanged blood products in the bilateral high convexities and left cerebellum. On the initial day of admission, he also developed high fevers and leukocytosis. Blood cultures obtained were positive for Streptococcus viridians. A transthoracic echocardiogram showed a depressed ejection fraction of 35%–40% with septal and apical wall abnormality but no vegetation or thrombus was noted. Esophagogastroduodenoscopy (EGD) was performed on the third day due to heme-positive gastric aspirate and a rapid drop in hemoglobin. During EGD, the patient had cardiac arrest while air insufflation was being performed. Chest CT that followed showed a focus of air along the posterior left atrium and an additional small focus of air just anterior to the esophagus (figure 1). The bacteremia, atrial air, multifocal strokes, and cardiac arrest during air insufflation were highly suggestive of an atrial-esophageal fistula. Surgical repair was considered but not pursued due to the patient's poor prognosis.
Figure 1. Chest CT demonstrates air in the posterior left atrium.
Autopsy demonstrated a fistula between mid-esophagus and left atrium with complete communication via the pericardial sac.
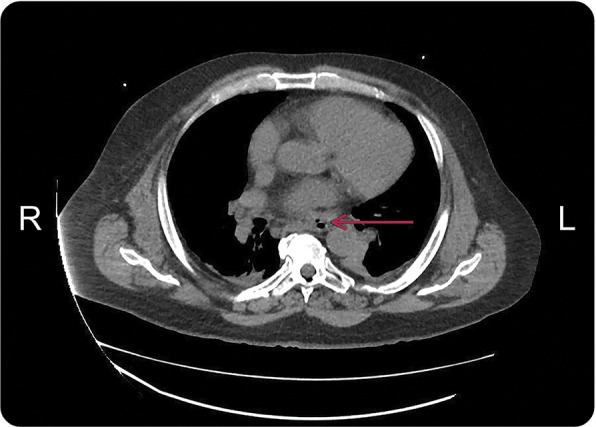
There was adherent blood clot in the fistula. Microscopic examination of this clot revealed it to be composed of purulent, antemortem thrombus and necroinflammatory debris with diffuse bacterial growth. Similar adherent purulent thrombi were noted throughout the heart including the left atrium, valves, and ventricles. The brain had multifocal septic thromboemboli involving bilateral cerebral hemispheres and cerebellum. Axonal pallor with axonal swelling was present in the cervical spinal cord. In addition, the spinal cord demonstrated microhemorrhages along with a predominantly neutrophilic inflammation, which is consistent with septic emboli (figure 2).
Figure 2. Spinal cord pathology and frontal lobe superficial vasculature.
(A) Hematoxylin & eosin stain of the cervical spinal cord demonstrates microhemorrhage (lower right) and acute inflammation (upper left). An anterior horn cell is also seen (upper right). The inflammation consists of primarily neutrophils with scant macrophages consistent with infectious emboli. (B) The frontal lobe shows in the center an artery with bacterial colonies (purple rind near vessel wall) and a smaller artery in the upper right shows complete occlusion of the lumen with bacterial colonies. In light of the bacterial thrombi in the brain, the cervical spinal cord infarct with an abundance of neutrophils is consistent with septic emboli.
DISCUSSION
Atrial-esophageal fistulas are a rare complication following ablation for AFib.1 Ablative damage to the atrial wall and adjacent esophagus may induce an inflammatory reaction/ischemic necrosis, which may subsequently lead to perforation. This perforation can lead to the development of an abnormal anatomic communication tract between the esophagus and left atrium several days after the initial ablation insult.3,4
Fistulization is reported to occur in fewer than 1% of cases post AFib ablation.4,5 Symptoms appear 2–60 days postprocedure and include fever, sepsis, gastrointestinal bleeding, and neurologic deficits. Fever is the most common symptom followed by neurologic deficits and hematemesis.1 Neurologic presentations include encephalopathy, meningitis, seizures, and strokes.2 Leukocytosis is a frequent laboratory finding.2 Our patient presented with strokes, and also developed fevers, leukocytosis, and gastrointestinal bleeding after admission. In addition, on pathology we were able to identify findings suggestive of septic thromboemboli also involving the spinal cord.
Transthoracic echocardiograms are often not helpful in diagnosis. Chest CT is the optimal method for evaluation. Imaging showing air in the mediastinum or pericardium or intracardiac air is highly suggestive of an atrial-esophageal fistula.2 Intraesophageal procedures should be avoided as they can lead to air emboli.2
Treatment includes antibiotic usage, and surgical interventions have better outcome compared with nonsurgical management.1 Surgical options include surgical repair of the fistula vs esophageal stenting.5
A high mortality rate is present with atrial-esophageal fistula. Timely diagnosis is crucial to initiating treatment. One should also consider spinal cord thromboembolic events as a potential complication of atrial-esophageal fistulas.
AUTHOR CONTRIBUTIONS
Swetha Renati: concept and design, main author of manuscript, revision of manuscript. Cui Yang: contributor of data to manuscript. Meggen Walsh: contributor to manuscript, specifically pathology. Jorge Trejo-Lopez: contributor to manuscript, specifically pathology. Anna Khanna: concept and design, supervision, revision of manuscript.
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
The authors report no disclosures. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Patricia C, Messerli FH, Dominguez AC, et al. Atrioesophageal fistula following ablation procedures for atrial fibrillation: systematic review of case reports. Open Heart 2015;2 e000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Claudia S, Pulgram T, Finsterer J. Neurological consequences of atrioesophageal fistula after radiofrequency ablation in atrial fibrillation. Arch Neurol Arch Neurol 2009;66:884–887. [DOI] [PubMed] [Google Scholar]
- 3.Maan A, Shaikh AY, Mansour M, Ruskin JN, Heist EK. Complications from catheter ablation of atrial fibrillation: a systematic review. Crit Pathw Cardiol 2011;10:76–83. [DOI] [PubMed] [Google Scholar]
- 4.Nair GM, Nery PB, Redpath CJ, Lam BK, Birnie DH. Atrioesophageal fistula in the era of atrial fibrillation ablation: a review. Can J Cardiol 2014;30:388–395. [DOI] [PubMed] [Google Scholar]
- 5.Mohonan Nair KK, Danon A, Valaparambil A, Koruth JS, Singh SM. Atrioesophageal fistula: a review. J Atrial Fibrillation 2015;8:79–84. [DOI] [PMC free article] [PubMed] [Google Scholar]