Practical Implications
Rarely, intracranial Avitene may provoke an inflammatory reaction leading to granulomatous meningitis. Awareness of this potential complication of neurosurgical procedures is critical to distinguish it from tumor recurrence or an infectious process.
Avitene, generically termed microfibrillar collagen, is a surgical hemostatic agent. Collagen-based hemostats are widely used to trigger platelet aggregation and reinforce the fibrin clot. Rarely, Avitene has been reported to induce a granulomatous reaction in the CNS, usually as a mass-forming lesion known as a textiloma. We report a case of Avitene-induced granulomatous inflammation presenting as meningitis after neurosurgery for WHO grade II atypical meningioma.
Case report
A 48-year-old man underwent uncomplicated debulking of a cavernous and sphenoid-based WHO grade II meningioma 2 months prior to presentation. Three weeks prior to presentation, he developed rapidly progressive fever, confusion, tremulousness, and hiccups. Brain MRI on presentation showed temporal lobe edema and superficial pial enhancement both near and remote from the operative site (figure 1). CSF evaluation revealed elevated opening pressure with mixed monocytic/lymphocytic pleocytosis and elevated protein. He was initially treated with broad-spectrum antibiotics as well as antivirals due to concern for an infectious process; however, repeat CSF evaluation 3 days later showed a worsening CSF profile and subsequent analysis 7 days after initial CSF sample continued to demonstrate mixed monocytic/lymphocytic pleocytosis and elevated protein. No organisms were identified on cultures. Continuous EEG excluded ongoing seizure. With lack of clinical response following broad-spectrum antibiotics and eventually ventricular shunting, the patient was taken to the operating room for wound exploration. On gross inspection, the brain appeared inflamed but there was no gross purulence. Meningeal and temporal lobe biopsies showed abundant amorphous eosinophilic material with chronic inflammation (figure 2A). In areas, a granulomatous-type reaction was seen encompassing the acellular material with foreign body giant cells and palisading macrophages (figure 2B). In addition, a considerable eosinophilic inflammatory infiltrate was present, suggesting an allergic-type response to the material (figure 2C). Given that pathology suggested an inflammatory rather than infectious process, the patient received treatment with IV corticosteroids. There was marked initial improvement in mental status, but subsequent clinical course was fluctuating, with other complications of illness. Repeat CSF analysis 4 days and 17 days after corticosteroid administration showed resolution of CSF pleocytosis.
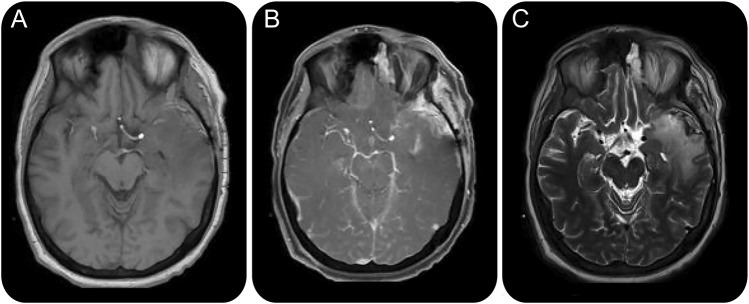
Figure 1. MRI brain.
(A) MRI T1 precontrast axial image. (B) MRI T1 axial postgadolinium contrast image demonstrates superficial pial enhancement. (C) MRI T2 axial image demonstrates edema involving the left temporal lobe.
Figure 2. Brain biopsy.
(A) Hematoxylin & eosin stain of a portion of dura with haphazard accumulation of amorphous pink material and interspersed chronic inflammation (×100). (B) Granulomatous reaction with foreign body giant cells and palisading macrophages surrounding acellular material (×200). (C) Brisk inflammatory infiltrate with abundant eosinophils (×200).
DISCUSSION
Avitene assists with hemostasis in surgical procedures by increasing platelet aggregation and facilitation of fibrin formation. It rarely has been reported to cause a granulomatous reaction. There have been prior reports of extracranial granulomatous reaction occurring after orbital, colonic, and ovarian surgical procedures.1–3 Previous reports have identified this reaction as occurring intracranially, and most presented with concern for recurrent/residual mass. One series detailed 3 children who developed a granulomatous reaction after intracranial surgery. Two of the patients underwent initial surgery for tumors, and one for focal cortical dysplasia. Imaging done 4–6 weeks after initial surgery was concerning for residual tumor or abscess. Subsequent surgery instead revealed granulomatous reactions.4 An additional report described a 3-year-old patient who underwent resection for medulloblastoma. He presented 2 months after surgery with concern for tumor recurrence and was found to have granulomatous reaction from Avitene.5 There are 3 cases from Japan involving adult patients who underwent neurosurgical procedures for various gliomas. Two months after the surgery, enhancement was noted on imaging. Histologic diagnosis showed reaction to Avitene.6 Finally, 2 cases were reported among a series of textillomas in which Avitene was contributory to the foreign body reaction—one with oligodendroglioma and one with anaplastic astrocytoma. Each patient presented 1 month after surgery with ring-enhancing lesions in the surgical bed concerning for progressive disease.7
Unique to our case is the clinical presentation of meningitis. Most cases of delayed reaction to a hemostatic agent present with a mass-forming lesion, known as a textiloma, which radiographically is concerning for residual/recurrent tumor. In this case, the radiographic findings of meningeal enhancement both near and far from the cavity site, as well as systemic symptomatology and abnormal CSF, favor a diffuse meningeal reaction. Our case describes this reaction following a meningioma resection, and perhaps this accounts for the predominantly meningeal symptoms rather than a parenchymal mass. IV corticosteroids were used as treatment in our case and demonstrated an improvement in mental status as well as in CSF pleocytosis.
AUTHOR CONTRIBUTIONS
Swetha Renati: drafting/revising the manuscript; study concept or design; analysis or interpretation of data. Supreet Kaur: drafting/revising the manuscript. Jesse L. Kresak: drafting/revising the manuscript; study supervision. Meredith Wicklund: drafting/revising the manuscript. Irene Malaty: drafting/revising the manuscript; study concept or design; acquisition of data; study supervision.
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
S. Renati, S. Kaur, and J.L. Kresak report no disclosures. M. Wicklund receives research support from Florida Department of Health Ed and Ethel Moore Alzheimer's Disease Research Program. I. Malaty has received funding for travel and/or speaker honoraria from National Parkinson Foundation, Tourette Association of America, Tourette Syndrome Association, and American Speech-Language-Hearing Association and receives research support from Abbott/AbbVie, Auspex, Biotie, Merz, Neurocrine, Pfizer, Revance, Teva, National Parkinson Foundation, Tourette Syndrome Association, and Dystonia Coalition. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Abramson DH, Andracchi S. Orbital Avitene granuloma formation after enucleation for intraocular retinoblastoma. Am J Ophthalmol 1997;123:567–569. [DOI] [PubMed] [Google Scholar]
- 2.McGregor DH, MacArthur RI, Carter T. Avitene granulomas of colonic serosa. Ann Clin Lab Sci 1986;16:296–302. [PubMed] [Google Scholar]
- 3.Nakajima M, Kamei T, Tomimatu K, Manabe T. An intraperitoneal tumorous mass caused by granulomas of microfibrillar collagen hemostat (Avitene). Arch Pathol Lab Med 1995;119:1161–1163. [PubMed] [Google Scholar]
- 4.Apel-Sarid L, Cochrane DD, Steinbok P, Byrne AT, Dunham C. Microfibrillar collagen hemostat–induced necrotizing granulomatous inflammation developing after craniotomy: a pediatric case series. J Neurosurg Pediatr 2010;6:385–392. [DOI] [PubMed] [Google Scholar]
- 5.O'shaughnessy BA, Schafernak KT, Dipatri AJ, Goldman S, Tomita T. A granulomatous reaction to Avitene mimicking recurrence of a medulloblastoma. J Neurosurg 2016;104:33–36. [DOI] [PubMed] [Google Scholar]
- 6.Gondo G, Yamashita T, Ishiwata Y, Hirata K, Satoh M. Peculiar computed tomographic images after intracranial use of microfibrillar collagen hemostat: report of three cases [in Japanese]. No Shinkei Geka 1989;17:1067–1071. [PubMed] [Google Scholar]
- 7.Ribalta T, McCutcheon IE, Neto AG, et al. Textiloma (gossypiboma) mimicking recurrent intracranial tumor. Arch Pathol Lab Med 2004;128:749–758. [DOI] [PubMed] [Google Scholar]