Practical Implications
Consider total spinal and brainstem anesthesia in the differential diagnosis of acute brainstem dysfunction.
Paravertebral administration of local anesthetics is an increasingly utilized method of analgesia. Total spinal anesthesia is a known complication characterized by paralysis, cranial neuropathies, coma, hypotension, bradycardia, and apnea. This adverse event has been attributed to local epidural, subdural, or subarachnoid spread of the anesthetic. We report a case of total spinal and brainstem anesthesia following paravertebral administration of ropivacaine and highlight the importance of considering this complication in patients with acute brainstem dysfunction.
A 51-year-old woman with severe chronic obstructive pulmonary disease underwent scheduled lung transplantation. After an uneventful surgery, a left T7-T8 paravertebral catheter was placed under ultrasound guidance. There was no aspiration of fluid upon catheter placement. Infusion of ropivacaine was initiated. Four hours later, she was following commands to move extremities and extubation was anticipated. She then developed quadriparesis, prompting urgent neurology consultation. Approximately 5.5 hours after initiation of ropivacaine infusion, she was alert and following commands to open and close eyes. Her right pupil was fixed and dilated. Power was Medical Research Council grade 0/5 in all extremities. Tone was flaccid. Deep tendon reflexes were absent and toes were mute to plantar stimulation. During the examination, she became unresponsive to vigorous sternal rub. The left pupil was also fixed and dilated. Oculocephalic maneuver revealed absent horizontal eye movements.
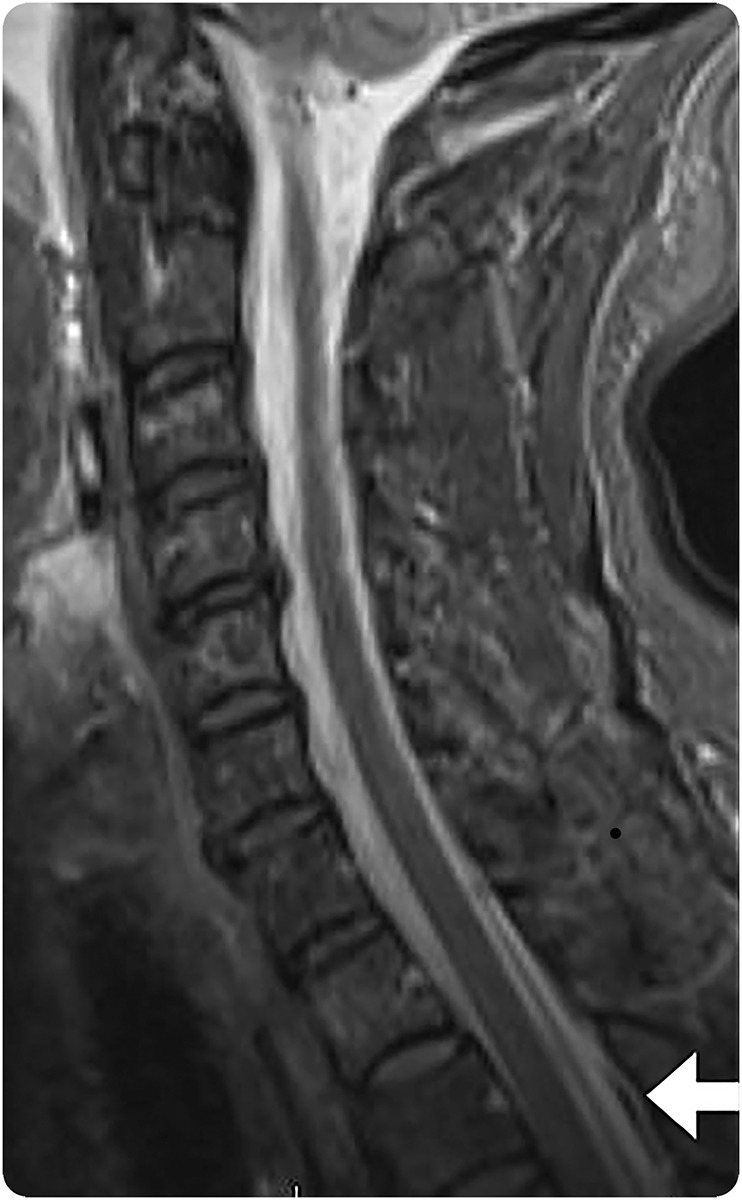
Emergent head CT and CT angiogram showed no hemorrhage, thrombus, or flow-limiting stenosis. The ropivacaine infusion was discontinued. Total administered dose of 0.2% ropivacaine over 6 hours was 120 mg or 1.8 mg/kg. The patient’s systolic blood pressure was consistently above 90 mm Hg on low-dose norepinephrine. With discontinuation of the ropivacaine and elevation of the head of bed, she regained consciousness and antigravity strength in her arms. An hour later, she could move her legs. Then her pupils normalized and she regained full extraocular movements, although bilateral end-gaze nystagmus persisted for several hours. MRI of the brain and cervical spine lacked ischemia but revealed epidural fluid collection (figure). The following day, she was extubated. She reported a headache and nausea that improved with lying flat, as well as with caffeine and analgesics. Ten days later, she went home without neurologic deficits.
Figure. Epidural fluid collection on cervical MRI (sagittal STIR image).
DISCUSSION
We report a case of total spinal and brainstem anesthesia, defined as anesthetic block of the cervical cord and brainstem or cranial nerves, following paravertebral ropivacaine anesthesia. Although total spinal anesthesia is a known complication of regional anesthesia,1 the rapid, sequential loss of brainstem function culminating in complete brainstem dysfunction is rare. Prior reports of total spinal anesthesia are namely in the anesthesiology literature and emphasize cardiopulmonary compromise, paralysis, and coma, although cranial nerve dysfunction, including fixed, dilated pupils, ophthalmoplegia, and absent gag reflex, have also been described.2–7 In these reports, deficits improved within 2 hours of discontinuation of regional anesthesia and completely resolved within 24 hours.
Acute brainstem and cranial nerve dysfunction has a restricted but potentially devastating differential diagnosis. Rapid diagnosis of compression, ischemic, or hemorrhagic injury is necessary for appropriate clinical management. We initially considered basilar arterial insufficiency as a cause of our patient's symptoms, but imaging was without vessel occlusion, restricted diffusion, hemorrhage, mass effect, or herniation. Our patient's symptoms worsened when she lay flat and improved with upright posture, which is inconsistent with brainstem hypoperfusion.
Inadvertent subarachnoid administration of local anesthetic is a well-known complication of epidural injection1 and has been reported with paravertebral injection.5 In the case of our patient, we suspect that local anesthetic spread from the intended paravertebral region to the subarachnoid space, directly infiltrating the brainstem and cranial nerves and resulting in blocked action potential propagation and clinical deterioration. Evidence for compromised dura and arachnoid includes our patient's classic low-pressure headache and imaging with epidural fluid collection.
Physicians should be aware that acute brainstem dysfunction can be caused by total spinal and brainstem anesthesia and consider this complication of regional anesthesia in the appropriate patient, as prompt discontinuation of regional analgesia and appropriate supportive care until medication clears and cardiopulmonary compromise has abated may prevent permanent disability.
AUTHOR CONTRIBUTIONS
Laura A. Foster: design of case report, drafting and revising manuscript. Cole K. Deutz: design of case report, revising manuscript. Jacob L. Hutchins: design of case report, revising manuscript. Jeffrey A. Allen: design of case report, drafting and revising manuscript.
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
L.A. Foster and C.K. Deutz report no disclosures. J.L. Hutchins has served on speakers' bureaus for Pacira Pharmaceuticals and Halyard Health; serves on the editorial board of Practical Reviews in Anesthesiology; serves as a consultant for Heron Therapeutics, Pacira Pharmaceuticals, Insitu Biologics, Worrell, AtriCure, and GLG; is an anesthesiologist who provides regional anesthesia to patients with elastomeric pumps; receives research support from Pacira Pharmaceuticals and Acel Rx; and holds stock/stock options in Insitu Biologics and SpineThera. J.A. Allen has received a speaker honorarium from Grifols and serves as a consultant for Axcelacare, CSL Behring, and Grifols. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Drasner K, Larson MD. Spinal and epidural anesthesia. In: Miller RD, Pardo MC, eds. Basics of Anesthesia. 6th ed. Philadelphia: Saunders Elsevier; 2011:252–283. [Google Scholar]
- 2.Garutti I, Hervias M, Barrio JM, Fortea F, De La Torre J. Subdural spread of local anesthetic agent following thoracic paravertebral block and cannulation. Anesthesiology 2003;98:1005–1007. [DOI] [PubMed] [Google Scholar]
- 3.Gillies IDS, Morgan M. Accidental total spinal analgesia with bupivacaine. Anaesthesia 1973;28:441–445. [DOI] [PubMed] [Google Scholar]
- 4.Grefkens JM, Burger K. Total spinal anesthesia after an attempted brachial plexus block using the posterior approach. Aneasthesia 2006;61:1105–1108. [DOI] [PubMed] [Google Scholar]
- 5.Lekhak B, Bartley C, Conacher ID, Nouraei SM. Total spinal anaesthesia in association with insertion of a paravertebral catheter. Br J Anaesth 2001;86:280–282. [DOI] [PubMed] [Google Scholar]
- 6.Piccioni F, Colombo J, Fumagalli L. Inadvertent high central neuroaxial block and possible total spinal anaesthesia occurring after nerve stimulation-guided thoracic paravertebral block. Anaesth Intensive Care 2014;42:270–271. [PubMed] [Google Scholar]
- 7.Yuen EC, Layzer RB, Weitz SR, Olney RK. Neurologic complications of lumbar epidural anesthesia and analgesia. Neurology 1995;45:1795–1801. [DOI] [PubMed] [Google Scholar]


