Summary
Hypotension, cardiac depression, and elevated microvascular permeability are known problems that complicate resuscitation of patients following traumatic injury, particularly those who are also intoxicated from alcohol consumption. A conscious rat model of combined alcohol intoxication and hemorrhagic shock has been used to study the hemodynamic mechanisms involved. Here, we describe using this model to study microvascular leakage and cardiac electrical activity.
Keywords: Hemorrhage, shock, alcohol, microcirculation, microvascular permeability, electrocardiogram
1. Introduction
Acute alcohol intoxication is a significant health problem in the United States and contributes to an increased risk of traumatic injury, accounting for the majority of alcohol-related cases in emergency rooms (1,2). Binge drinking is a nationwide trend involving at least 38 million adults in the U.S., which by the most recent estimates produced a $223.5 billion cost burden for the U.S. (3). Nearly 40% of injured patients admitted to the ER have a blood alcohol concentration greater than 80 mg/dL (2,4–6). Intoxicated patients present a complex, altered physiologic state associated with increased injury severity (4,6–9). In addition, these patients typically require a significantly greater frequency of interventions in the hospital such as endotracheal intubations, placement of intracranial monitoring devices, and greater use of diagnostic peritoneal lavage (7). Compared to their sober counterparts, alcohol-intoxicated trauma patients have a two-fold increase in infectious complications, development of pulmonary failure, acute respiratory distress syndrome (ARDS) secondary to sepsis, and an overall increase in ARDS-related mortality (10).
One particularly problematic outcome of acute alcohol intoxication is aggravated hemodynamic instability following hemorrhage (9). The dramatic loss of circulating fluids elicits a massive baroreceptor reflex, reducing splanchnic blood flow and causing ischemic injury that disrupts integrity of the gut wall. This leads to a systemic inflammatory response, including systemic microvascular leakage (11–14). The resulting edema complicates fluid resuscitation and can lead to sepsis, ARDS, and abdominal compartment syndrome (15).
A conscious rat model of alcohol intoxication and hemorrhagic shock was developed by Molina and colleagues to test whether an impairments in the baroreceptor reflex or associated neural, endocrine, and metabolic mechanisms that control vascular tone may be responsible for this increased hypotension (14,16–18). Their findings showed that: 1) significantly less blood from alcohol-intoxicated rats is required to produce the same hypotensive pressure during a fixed-pressure hemorrhage; and 2) alcohol-intoxicated rats are significantly more hypotensive following equal volumes of removed blood (14,18). In this same model, alcohol-intoxicated rats had depressed blood bicarbonate levels, lower PO2, elevated PCO2, and lower plasma glucose and lactate compared to control rats (18). Alcohol intoxication also causes altered tissue and plasma cytokine responses during hemorrhagic shock (18). The elevations in plasma levels of epinephrine, norepinephrine, and arginine vasopressin in response to fixed-pressure hemorrhage were all significantly blunted in alcohol intoxicated rats compared to control rats (17). However, their findings also showed that sympathetic control of blood pressure and acetylcholine-induced vasodilation were not impaired by alcohol intoxication (19,20). Intracerebroventricular administration of choline, a precursor of the preganglionic neurotransmitter acetylcholine, did not improve hemodynamic and neuroendocrine counter-responses to hemorrhagic shock in alcohol-intoxicated rats (19). Furthermore, studies using isolated aorta and mesenteric arteries of intoxicated and control rats that underwent experimental hemorrhage showed that the alcohol-induced impairment of hemodynamic regulation is not due to a decrease in responsiveness of blood vessels to vasoconstrictors like phenylephrine, or vasodilators like acetylcholine (20).
Such findings have led us to investigate alternative mechanisms. One such potential mechanism is a reduction in central fluid volume due to elevated microvascular permeability. To approach this, we have combined the aforementioned rat alcohol intoxication model with intravital microscopy. Our results showed that alcohol intoxication increases microvascular leakage in the mesentery, which could potentially contribute to alcohol-induced hypotension (21). In the current paper, details of the combination of these intravital microscopy methods with acute alcohol-intoxication (AAI) and hemorrhagic shock and resuscitation (HSR) in rats are described. A second potential mechanism is direct action on the electrical activity of the heart (22–24). ECG is a minimally invasive procedure that allows recording of cardiac electrical function. Lead II format specifically identifies left ventricular function with higher specificity. The use of lead II ECG recording following combined AAI and HSR in the rat is also described in this protocol.
2. Materials
Catalog numbers are for reference to instruments in the authors’ laboratories. Similar instruments based on cost and preference can be substituted.
2.1. Catheter preparation
Polyethylene 50 tubing (Becton Dickinson)
Silastic I.D. 0.51 mm × O.D. 0.94 mm (Dow Corning)
Bunsen burner
Scissors
Paperclip loop
Ring stand and clamp
2.2. Catheter implantation surgery
Fine scissors (Fine Science Tools (FST) 14958-11)
Tissue forceps (FST 11021-14)
Halsey needle holders (FST 12501-13)
Extra fine forceps (FST 11152-10)
Vannas scissors (FST 15000-00)
Bulldog clamp (FST 18054-28)
Micro dissecting forceps (Roboz RS-5069)
Ultra fine hemostats (FST 13021-12)
Bead sterilizer (FST 18000-50)
Beveled trocar I.D. 3 mm × O.D. 4 mm
Hemostats wrapped with Tygon tubing
Betadine scrub (Purdue Products)
Chlorhexidine gluconate scrub (Baxter)
Alcohol
0.9 % sodium chloride USP (Hospira)
10 cc syringes (Becton Dickinson)
23 gauge needles (Becton Dickinson)
Gauze sponges (Fisher)
Ethicon FS-2 suture and needle (Johnson & Johnson)
Ethicon 4-0 silk, black, braided suture without needle (Johnson & Johnson)
Perry style 42 gloves (Ansell)
Lighter
Masking tape
Silastic-tipped vascular catheters
Gastric catheters
Isoflurane USP and vaporizer (Henry Schein and Harvard apparatus)
Cotton-tipped applicators
Akwa tears ophthalmic ointment (Akorn)
Fur trimmers (Oster)
2.3. Initial Preparation Procedures
Mouse-sized cage
Digital scale (Mettler Toledo)
1cc syringe with plunger removed and luer tip cut off (Becton Dickinson)
3cc syringe (Becton Dickinson)
23 gauge needles (Becton Dickinson)
0.9% sodium chloride USP (Hospira)
Fine scissors (Fine Science Tools (FST) 14958-11)
Hemostats wrapped with Tygon tubing
Masking tape
Lighter
Heated water bath (Fisher)
Lactated Ringers USP (Hospira)
2.4. Fixed-pressure Hemorrhage
Heated water-pad and circulating heated water pump (Gaymar)
Software and hardware for measuring MAP: LabChart Pro v7, PowerLab 4/35, Quad Bridge Amp (ADInstruments)
Pressure transducer (ADInstruments)
3cc syringes (Becton Dickinson)
Heparin-coated 3cc syringes
23 gauge needles (Becton Dickinson)
3-way stopcocks (Braun)
1.5 mL centrifuge tubes (Eppendorf)
Refrigerated centrifuge (Eppendorf)
Cryo-vials (Corning)
0.9% sodium chloride USP
Water-filled beaker
2.5. Resuscitation
Software and hardware for measuring MAP: LabChart Pro v7, PowerLab 4/35, Quad Bridge Amp (ADInstruments)
Pressure transducers (ADInstruments)
Warm Lactated Ringers USP (Hospira)
10cc syringes (Becton Dickinson)
30cc syringes (Becton Dickinson)
20 gauge needles (Becton Dickinson)
Polyethylene 90 tubing (Becton Dickinson)
Hemostats wrapped with Tygon tubing
Fine scissors (Fine Science Tools (FST) 14958-11)
Syringe pump (kdScientific)
Lighter
2.6. Intravital microcopy
2 × 2 Gauze sponges (Fisher)
3 × 3 Gauze sponges (Fisher)
Betadine scrub (Purdue Products)
Chlorhexidine gluconate scrub (Baxter)
Alcohol
Fine scissors (Fine Science Tools (FST) 14958-11)
Tissue forceps (FST 11021-14)
Hemostats wrapped with Tygon tubing
Bead sterilizer (FST 18000-50)
Lactated Ringers USP (Hospira)
Heating plate and temperature controller (World Precision Instruments)
Isoflurane USP and vaporizer (Henry Schein and Harvard apparatus)
FITC-albumin (Sigma Aldrich)
Syringe pump (Fisher)
Peristaltic pump (Cole-Palmer)
Water-bathed heating coil (Radnoti)
Circulating water bath and pump (Thermo)
Software and hardware for measuring MAP: LabChart Pro v7, PowerLab 4/35, Quad Bridge Amp (ADInstruments)
Pressure transducer (ADInstruments)
Upright fluorescent microscope (Nikon E600)
Mercury lamp and power source (Nikon)
Fur trimmers (Oster)
Cotton-tipped applicators
Euthasol - pentobarbital sodium and phenytoin sodium (Virbac)
2.7. Surface Lead Electrocardiogram (ECG) recording
Isoflurane USP and vaporizer (Henry Schein and Harvard apparatus)
Three lead monopolar needle electrodes (29 gauge)
Software and hardware for measure ECG: LabChart Pro v7, PowerLab 8/35, Animal Bio Amp (ADInstruments)
Heating plate and temperature controller along with rectal probe (World Precision Instruments)
3. Methods
The fixed-pressure hemorrhage/resuscitation (HSR) protocol requires implantation of polyethylene catheters into the carotid artery, jugular vein, and an indwelling gastric catheter. The carotid catheter is used for withdrawing blood during the HSR phase of the protocol as well as monitoring, in real-time, mean arterial pressure (MAP) during HSR and intravital microscopy. The jugular catheter allows for the infusion of resuscitative fluids during the HSR and FITC-conjugated albumin tracer during intravital microscopy. The indwelling gastric catheter allows for administration of alcohol or water prior to experimentation. This method was chosen over oral gavage to minimize stress on the rats, which can occur with handling. Isovolumic water serves as a control for distension of the stomach. This was chosen over isovolumic, isocaloric dextrose solution, which we observed causes changes in lymphatic pumping (25).
A fixed-pressure HSR protocol was chosen to ensure the rats received the same degree of injury severity. Studies have shown rats that with fixed-volume hemorrhage, the alcohol-intoxicated rats are significantly more hypotensive (14,18). In addition, this protocol is performed in conscious, unrestrained rats, preventing any compounding effects on hemodynamics caused by anesthetics, and stress-induced increases in sympathetic output caused by restraints. This method also better simulates alcohol intoxication and traumatic injury in the human population.
Intravital microscopy is a powerful tool for determining microvascular permeability in vivo (26–28). For this model, the mesenteric microcirculation is a key site of interest due to the ischemia-reperfusion injury on the gut caused by HSR. FITC-albumin is typically used as a tracer for extravasation of plasma macromolecules. Elevated fluorescence in the extravascular spaces over time indicates increased microvascular leakage. To determine that increases in leakage are due to changes in diffusive permeability, diameters of the arterioles feeding the local microvascular bed are also monitored. If these diameters increase, the leakage is likely due to increased filtration, while if these diameters do not change, or even decrease, there is likely an increase in permeability of microvascular endothelium. In addition, rapid acquisition of brightfield images in sequence can be obtained for measurement of red blood cell velocity as well as leukocyte rolling and adhesion in postcapillary venules.
Surface lead ECG recordings are a minimally invasive procedure that demonstrates the electrical activity of the heart. In 2005 the FDA issued that well-controlled electrocardiograms (ECG) trials are required to define cardiac risk of new therapies (29). Indeed ECGs have been a powerful tool for cardiovascular health and its ability to acutely sense toxic effects of chemicals and or drugs (30). The QT and QTc duration correspond to the repolarization phase of the cardiac action potential (31,32). The QRS complex and the P wave are also studied utilizing the bipolar limb leads in lead I, II, and III positioning. Lead II positioning provides a clear image of the QRS complex and ST segment the ECG analysis. The ECG protocol is performed while the rats are anesthetized with 2% Isoflurane inhalation. Heart rate is allowed to stabilize (5 minutes) followed by lead II ECG signal acquisition.
All animal protocols should be performed in strict accordance government regulations. In this U.S. this includes the U.S. Animal Welfare Act, U.S. Public Health Service Policy on the Humane Care and Use of Laboratory Animals, and the Guide for the Care and Use of Laboratory Animals. All animal experiments must be performed with the approval of the Institutional Animal Care and Use Committee in the U.S. or equivalent regulatory committee in other countries. Aseptic technique is required for all surgical procedures including catheter implantation and the laparotomy for intravital microscopy. All surgical instruments to be used must be sterilized prior to surgical procedures by autoclave and again just before use with a bead-sterilizer. Areas of skin where incisions will be made for surgery must be properly cleaned with antiseptic cleansers. All fluids and drugs used should be United States Pharmacopeia (USP)-grade. All efforts should be made to minimize pain, including providing analgesics after surgery.
3.1. Catheter preparation
Catheters used for this protocol are hand-made from commercially available Intramedic polyethylene 50 (PE50) tubing from Becton Dickinson.
Using a thick metal paper clip, create a circular loop and mount it to a ring stand. Heat the loop with a Bunsen burner until it glows red then remove the flame (See note 1).
-
Allow a few seconds for the loop to stop glowing then feed about one inch of PE50 through the loop.
The tubing will begin to melt and contract on itself to create a bubbled section of tubing.
This bubble will serve as an anchor point for sutures to prevent the catheters from pulling out (See note 2).
This step is applies to both vascular and gastric catheters.
Measure off about 40 cm from the bubbled end and cut to produce one vascular catheter. For gastric catheters, measure 46 cm from the bubbled end and cut.
Cut off excess PE50 tubing from the bubble-side of the catheter leaving about 0.5 cm from the end to the bubble (See note 3).
-
Catheters implanted into the blood vessels have an additional strip of silastic tubing attached to the catheter.
Trim the silastic down by cutting the end to 3 cm in length from the end of the bubble (See note 6).
Each rat will receive 2 vascular catheters (one for the carotid artery and one for the jugular vein) and 1 gastric catheter (See note 7).
3.2. Catheter Implantation Surgery
In order to perform the fixed-pressure HSR protocol, catheters are implanted into the left common carotid artery and right jugular vein 4–5 days prior to the experiment. An indwelling gastric catheter is also implanted for administration of alcohol or water to the stomach.
For anesthesia, isoflurane is a good choice, however other anesthetics such as ketamine/xylazine will also work. To anesthetize with isoflurane, place the rat into the induction chamber. Set the vaporizer to 4%, open the USP-grade oxygen gas cylinder, and set the flow rate to 1 liter (L) per minute (min).
Once the rat is sufficiently anesthetized, remove from the induction chamber and place with the dorsal side and insert the nose into the nosepiece that will deliver additional isoflurane. Reduce the isoflurane to about 2.5% (See note 8).
To prevent the rat’s eyes from drying out, apply Akwa tears ophthalmic ointment using cotton-tipped applicators.
Using commercially available hair trimmers, shave about a 2 × 2 cm area of fur from the dorsal nape of the neck starting about 5 mm inferior form the ears. This is the location for the incision through which the catheters will be routed out.
Place the rat ventral side up and shave the fur from the ventral neck area. Again, about a 2 × 2 cm area depending on the size of the rat should be shaved of fur.
Clean the shaved areas three times: once with Chlorhexidine gluconate surgical scrub, once with alcohol, and once with Betadine scrub.
Before starting the surgery, the catheters to be used should be flushed and filled with saline using a 10 cc syringe. Ensure there is no air bubbles within the catheters.
With the rat in a dorsally recumbent position, make a 1 cm incision in the ventral neck along the medial long axis.
-
Carefully isolate the left common carotid artery. Ultra-fine hemostats are good for separating tissue and isolating the vessel.
Consultation of a resource such as Anatomy & Dissection of the Rat 3RD ed. by Walker and Homberger for the location of the carotid is recommended.
-
Once the carotid is isolated, suture the brain side of the vessel closed with an 8 cm long strip of 4-0 suture.
Tie off with 2 simple suture knots.
-
Place another 8 cm long strip of 4-0 suture under the isolated carotid artery on the heart side.
Do not tie off this suture yet.
To facilitate insertion of the catheter into the artery, a small drop of lidocaine can be administered to the isolated vessel.
Place a small bulldog clamp on the heart side of the vessel (See note 9).
Using vannas scissors, create a small incision in the carotid artery (See note 10).
Using micro dissecting forceps to hold open the incision, feed one of the silastic-tipped catheters into the vessel with extra fine forceps.
-
Remove the bulldog as the catheter is inserted into the vessel taking care to keep a firm hold on the catheter (See note 11).
-
Replace the bulldog clamp to hold the catheter in place. Secure the catheter inside the vessel with 4-0 suture placed earlier on both sides of the bubble (See note 14).
Two simple suture knots are sufficient on to anchor the catheter.
Remove the bulldog clamp and check for adequate blood flow. Flush a small amount of saline to clear any blood from the catheter and thermally seal the end with a lighter (See note 15).
Repeat steps 8–13 for the right jugular vein (See note 16 and 17).
Turn the rat over onto its ventral side. Create a small 0.5 cm incision on the midline of the dorsal nape of the neck about 1 cm inferior from the ears.
Using a trocar, route the catheters subcutaneously to and out the incision of the dorsal nape of the neck.
Using Ethicon FS-2 suture and needle or similar, close the ventral neck incision with a continuous, locking suture or individual simple suture knots.
-
Lay the rat onto its right side. Using your index finger, feel for the bottom of the rib cage. Make a 2 cm long incision perpendicular to the long axis of the rat (dorsal to ventral) into the skin.
The incision should be about 3.5 cm away from the bottom of the ribcage (about the width of the index and middle finger).
Separate the skin, in the immediate area of the incision, from the muscle layer using extra fine hemostats.
Make a second incision slightly smaller in length into the muscular layer and open the peritoneal cavity.
-
Locate and externalize the stomach through the incision. The stomach should be just under the liver.
Be sure to only grab the stomach by the muscular layer. Do not grab by the transparent tissue.
Using Ethicon FS-2 suture and needle begin a purse-string knot within the muscular layer of the stomach. Do not tighten the suture.
Perforate the stomach with small diameter scissors such as vannas scissors and insert a non-silastic tipped catheter bubble-end first into the perforation. Finish tightening and secure the purse-string knot.
Secure the gastric catheter in place through the top of the muscular layer incision with a single simple suture then finish closing the incision with a continuous locking suture.
Using a trocar, route the gastric catheter subcutaneously to and out the incision of the dorsal nape of the neck. The catheters should be marked with sharpie or marker in unique ways to identify the catheters.
Close the incision in the skin with a continuous locking suture with Ethicon FS-2 suture and needle (See note 18).
-
Place the rat back on its ventral side. Pull the catheters taut and secure them to the incision on the dorsal nape of the neck with simple sutures using Ethicon FS-2 suture and needle.
It helps to secure the carotid catheter to the left side of the incision and the jugular to the right side of the incision and the gastric catheter in between (See note 19).
Once the catheter are secure with suture, close the remaining open incision with simple suture knots.
To prevent the rat from gnawing on the exposed catheters, coil them around your index finger and wrap with masking tape. If secured properly, the taped catheters will stand up perpendicular from the body out of the rat’s reach.
Allow the rat 4–5 days to recover before experimentation.
3.3. Initial preparation procedures
There are several companies that provide software and hardware capable of measuring mean arterial blood pressure (MAP) in real-time. Our lab has used LabChart Pro v7 software and with the PowerLab 4/35 and Quad Bridge Amp provided by ADInstruments.
On the day of the experiment, rats to be used should be weighed and placed into mouse sized-cages. Weighing the rat is important, as this will be used to estimate the total blood volume (TBV) of the rat, calculated as the volume equivalent to 7% of body weight (BW).
Unwrap catheters and feed them through a 1 cc syringe with the plunger removed and luer end cut off. This is to prevent the rat from manipulating the catheters and chewing on them.
Locate the carotid artery line. Cut off the end to ensure flow of arterial blood. If no blood flows from the line, flush with saline using a 3 cc syringe and check again. Remove the syringe and check for blood flow from the line. Once blood is able to flow through the catheter, flush with saline to prevent clotting and thermally seal with a lighter.
Locate the jugular line and clamp it with the hemostat. It is important to clamp the line first with the jugular because once the line is opened it will pull air in. Too much air will cause an air embolism and can cause death. Cut the end of the line and flush it with saline from the 3 cc syringe to ensure fluids can be infused. Thermally seal the catheter with a lighter.
Feed the catheters through a hole made in the top of the mouse cage and secure with tape. Ensure to leave enough slack in the catheters between the rat and the top of the cage to allow for unrestricted movement.
Bring the cage(s) to the HSR equipment. Cages may be placed onto a heated water-pad to help keep the rats warm during the HSR protocol if desired.
The pressure transducers for the PowerLab 4/35 are connected to the carotid catheter via a 23G needle. Connect the carotid catheter to the pressure transducer and flush the line slightly with saline provided by a 10 cc syringe reservoir atop the transducer rig (See note 20).
Open LabChart Pro v7 on the computer. Press the “start” button in the software to begin pressure recordings. If the pulse pressure (PP) is narrow check for kinks created in the catheters and flush the line. This should correct and restore PP. Perform this as needed through the entire HSR protocol.
Because the rats are unrestrained and the catheters are secured to the top of the cage, constant observation of the state of the catheters must be maintained. The rat moving around leads to twists, coils, and even kinks that are further compounded by the fact there are three catheters.
3.4. Alcohol Administration and Fixed-Pressure Hemorrhage
Record 60 minutes of baseline MAP. This will allow the rat time to relax. This permits any sympathetic discharge due to handling, weighing, and transfer from the vivarium to dissipate.
-
Following baseline MAP readings, 2.5-g/kg dose of alcohol or isovolumic water is administered to the rat via the gastric catheter.
MAP readings are recorded for an additional 30 minutes for sufficient absorption of alcohol.
-
During the hemorrhage phase, warm a 500 mL bag of USP-grade lactated Ringer’s (LR) in a water bath set to 37° C.
This will be used for the resuscitation phase of the protocol.
-
The hemorrhage phase of the protocol is initiated 30 minutes after administration of alcohol or water (See note 21). Blood is withdrawn to achieve a fixed-pressure hemorrhage between 40–60 mm Hg for 60 minutes.
Blood withdrawal is achieved using a 3 cc syringe and connecting it to a 3-way stopcock attached to the transducer rig.
A large bolus of blood is removed within the first minute, typically between 4.5 and 6.0 cc of blood depending on the BW of the rat (330–365g range). Remove more if needed to achieve 40–60 mm Hg in this initial phase of the hemorrhage (See note 22).
-
Once the desired map is achieved, flush the catheter slightly with saline to prevent blood clotting in the line. Do not flush too much saline back during the hemorrhage phase. Just enough to clear most of the blood from the catheter (See note 23).
The catheter must be flushed with saline with each subsequent blood withdrawal.
-
Log the volume of blood withdrawn. We estimate TBV from the rat’s BW (7% of BW). We set 50% of TBV as the upper limit of the volume of blood that can be safely removed.
Generally, 44 ± 2% of TBV from water-treated and 36 ± 1% of TBV for alcohol-treated rats is removed.
-
Once 40–60 mm Hg MAP is achieved, maintain this range by withdrawing blood as necessary for the remaining 60 minutes.
Usually withdrawing 0.5 cc at a time is sufficient to maintain the hemorrhage MAP.
-
Blood samples may be kept from various time points during the protocol. A fresh heparinized 3 cc syringe should be used to withdraw the blood for these samples.
The samples should be spun in a refrigerated centrifuge at 2000 RPM and 4° C to obtain plasma.
Snap freeze the plasma in liquid nitrogen and store at −20° C.
Following one hour of hemorrhage the resuscitation phase of the HSR protocol begins.
3.5. Resuscitation
Resuscitation consists of a 40% total blood volume removed (TBR) bolus and a 2X TBR infusion for one hour of warm (37 °C) LR administered via the jugular catheter. Remember to clamp the jugular prior to cutting off the thermally sealed end of the catheter to prevent air from being pulled in.
Following completion of the hemorrhage, determine the final TBR for each rat and withdraw the appropriate volume of LR pre-warmed to 37° C into a 10 cc syringe (for the 40% TBR bolus) and a 30 cc syringe (for the 2x TBR infusion).
Using a 20-gauge needle and PE90 tubing, connect to the jugular catheter and administer the 40% TBR bolus of warm LR over one minute.
Clamp the jugular line following administration of the bolus and remove the 20 gauge needle from the 10 cc syringe and place it onto the 30 cc syringe containing the infusion fluids (See note 24).
Place the syringe into a syringe pump. Set the appropriate syringe settings based on the brand used, the total volume to be infused, and the rate to infuse that volume over 60 minutes (See note 25). Start the syringe pump.
Continue to record MAP using LabChart and PowerLab during the resuscitation phase of the protocol.
Once the 2x TBR infusion concludes the HSR protocol is complete. Thermally seal catheters and proceed to either the intravital microscopy (3.6) or the ECG (3.7) phase of the protocol.
3.6. Intravital microscopy
Immediately following completion of resuscitation, transfer the rat to the surgery station for intravital microscopy preparation.
Anesthetize the rat with isoflurane (other methods for anesthesia may be used if desired) (4% induction and 2.5 – 1.5% maintenance).
Once sufficiently anesthetized place the rat in a dorsally recumbent position onto a heating pad set to 37° C connected to an adaptive temperature controller. Shave away the fur from the ventral abdominal region using rodent hair clippers.
Clean the shaved area three times with 3×3 gauze sponge: once with Chlorhexidine gluconate surgical scrub, once with alcohol, and once with Betadine scrub.
Perform a midline laparotomy in the ventral abdominal skin. The incision length should be only between 2.5–3.0 cm long (See note 26).
Using single 2×2 gauze sponges, insert one into the left side of the incision and one into the right side. This helps to hold in the abdominal contents and prevent additional intestine from spilling out onto the stage.
Using cotton-tipped applicators, carefully begin to remove the mesentery from the abdominal cavity (See note 27 and 28).
Turn the rat onto its side and move the heating pad and rat to the intravital microscopy stage (See note 29).
Apply some warm LR to the stage
Carefully splay the mesentery flat over the stage using cotton-tipped applicators and only handling by the small intestinal walls. Apply some warm LR to the mesentery to prevent drying out (See note 30).
Once the mesentery is splayed out onto the stage, transfer the entire setup (rat, stage, and heating pad) to the microscope.
Begin a superfusion drip of LR using a peristaltic pump to about 10–12 drips per minute. LR should pumped through a water-bathed heating coil heated to 37° C by a circulating water bath/pump. Remove excess LR from the stage reservoir by a vacuum line.
Begin administration of FITC-albumin to the jugular catheter. FITC-albumin administration consists of a bolus of 1 mg/10 kg in 1 mL LR over 1 to 2 minutes followed by continuous infusion of 0.15 mg/kg/min. The vehicle for FITC-albumin is warm LR.
For the continuous infusion, set the syringe pump to one half the rate used during resuscitation. Wait 10–15 minutes before imaging to allow for uniform distribution of FITC-albumin throughout the circulation.
During the 10–15 minute incubation period, connect the carotid catheter to a pressure transducer to monitor MAP during. The same equipment used during HSR can be used.
Begin imaging of the mesenteric microcirculation using an upright fluorescent microscope. Our lab captures images for 30 minutes at intervals of 0 (baseline), 10, 20, and 30 minutes.
Fluorescent stills are captured with a 4x objective followed by a 30 seconds of brightfield images (time-lapse movie) with a 10x objective. Two separate areas of microcirculation are imaged with at least one containing a lymphatic vessel.
Images are analyzed using ImageJ open-source software. Fluorescent images are used for quantifying extravasation of FITC-albumin by measuring the integrated optical intensity (IOI) of the extravascular regions of the postcapillary venules. The mean 30-minute IOI is calculated and plotted and statistics performed. All data is normalized to the 0 minute baseline.
Brightfield movies are for assessing leukocyte rolling and adhesion, lymphatic pumping, and arteriolar diameter measurements.
3.7. Surface Lead Electrocardiogram (ECG) Recording
Transfer the rat to the ECG station for ECG preparation.
Anesthetize the rat with isoflurane (other methods may be used if desired) (4% induction and 2.5 – 1.5% maintenance), or keep the rat anesthetized if ECG is recorded after intravital microscopy.
Once sufficiently anesthetized, place the rat in a dorsally recumbent position onto a heating pad set to 37° C connected to an adaptive temperature controller. Insert the rectal probe to establish rat temperature and record.
Remove the hair just below the paws of the rat by shaving and if possible hair removal cream. Clean the limbs three times with 3×3 gauze sponge with alcohol.
For lead II configuration place the positive lead (red wire) into the left hind paw, the negative lead (black wire) into the right front paw, and finally the reference lead (green wire) into the right hind paw. Alternatively if available biopotential “snap on” leads can be used in place of needle leads.
The Animal Bio Amp for the PowerLab (4/35 or 8/35) should be connected to the ECG needle leads.
Open LabChart Pro on the computer. Press the “start” button in the software to begin ECG recordings. If the ECG trace is noisy check the placement of the leads, pause the software and readjust the leads if necessary. Care should be taken to place the leads just under the skin but not deep into the skeletal muscle, which can confound some of the electrical signaling. Perform this as needed through the entire ECG protocol.
Record 5 minutes of baseline ECG to ensure a stable heart rate. This will allow the heart rate to become stable while under anesthesia. Begin acquiring ECG signals in lead II position, pause the software and reposition the leads to I and then III. Lead I position is moving the positive lead (red wire) to the right front paw; and lead III is moving the positive lead (red wire) to the right hind paw and moving the reference lead (green wire) to the left hind paw.
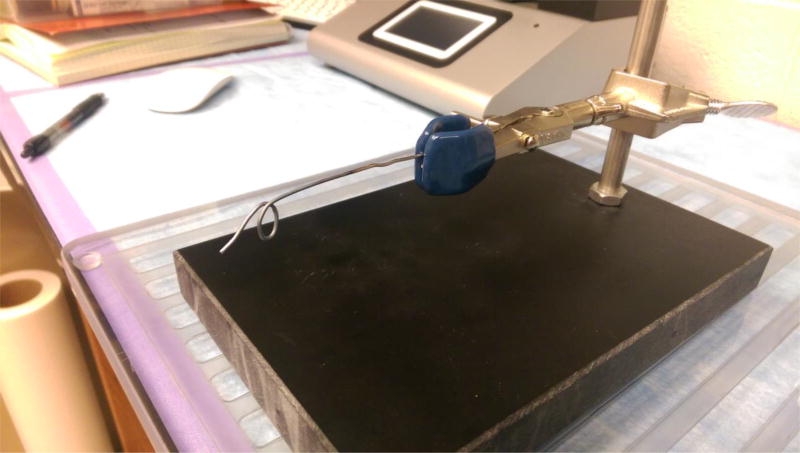
Fig. 1.
Metal loop and ring stand assembly for catheter preparation.
Fig. 2.
PE50 tubing with a bubble formed at one end after holding it within a metal loop heated by a Bunsen burner.
Fig. 3.
PE50 tubing catheter with bubble after trimming.
Fig. 4.
Vascular catheter with silastic tubing attached.
Fig. 5.
The gastric (top) and vascular (bottom) catheters are shown, demonstrating the difference in length of the silastic tubing. Note the slightly beveled tip in the silastic of the vascular catheter.
Footnotes
Notes
The metal loop and ring stand. This loop is simply made by taking a paper clip and straightening out one end and forming a loop on the other. The looped end is heated with a bunsen burner. One end of the PE50 tubing is fed through and the heat from the loop melts the tubing to form a bubble (see Fig. 1).
PE50 tubing with a bubble formed at one end at one end after holding it within a metal loop heated by a Bunsen burner. The bubble serves as an anchor point for securing the catheter inside of the vessel or stomach. This method is used when making both vascular and gastric catheters (see Fig. 2).
Trimmed bubble-end of the catheter. Once the bubble is formed, the end of the catheter should be trimmed to about 0.5 cm from the end of the bubble. Both vessel and gastric catheters undergo this step. Gastric catheters are complete and ready for use after completion of this step (see Fig. 3).
- This helps make the silastic more compliant and easier to get over the bubble of the catheter.
- Perform in a well-ventilated room or under a fume hood.
Vascular catheters are the same as gastric catheters with the addition of a strip of silastic tubing on the bubble-end. Silastic is less rigid and more compliant than polyethylene. It facilitates ease of cannulation of the vessel and protects against vessel damage that otherwise may be caused by the rigid polyethylene tubing. The vascular catheter with silastic tubing attached is shown (see Fig. 4).
After the silastic tubing is placed on the vascular catheter, the silastic is trimmed to about 3 cm from the end of the bubble. This is the average length from where the incision is made in the carotid artery that provides the best signal when recording MAP. The end of the silastic should be trimmed with a slight bevel to facilitate insertion of the catheter into the vessel.
Each rat will receive two vascular catheters (one in the carotid artery and one in the jugular vein) and one gastric catheter. The vascular and gastric catheters are initially made the same way as described in step 3 of catheter preparation. Vascular catheters have an additional strip of silastic tubing. The gastric (top) and vascular (bottom) catheters are shown, demonstrating the differences in length of the silastic tubing. Note the slightly beveled tip in the silastic of the vascular catheter (see Fig. 5).
There is no set percentage value for isoflurane during maintenance. Each rat responds differently. Continually monitor the breathing rate during surgery and adjust the percentage up or down as needed.
Placement of a bulldog clamp is absolutely essential. If no clamp is placed onto the carotid before an incision is made, the rat will begin to hemorrhage and the vessel will be quickly lost under the blood.
Take care not to completely cut through the artery. The remaining blood in the isolated portion of the artery will signal a successful incision.
Blood pressure will push the catheter out if not held firmly inside the vessel.
- To prevent this the catheter should be clamped with a Tygon-wrapped hemostat.
- Clamping catheters with hemostats without a rubber wrapping or coating will crimp the PE50 tubing.
- These hemostats can be easily made by sliding a strip of Tygon tubing onto the ends of a hemostat.
Using the bulldog to hold the catheter in place while suturing is recommended. The rat’s blood pressure will push the catheter out if it is not secured in place by the bulldog clamp.
- A small break in the seal will allow enough of a pressure differential to fill the catheter with blood. By the end of the recovery period, this blood will be coagulated and the catheter will be useless.
The jugular vein is extremely thin-walled and easy to tear when isolating with ultra fine hemostats.
The jugular catheter will pull in air if not clamped. Ensure it is clamped before incision to prevent air emboli.
When suturing the skin incision, be careful not to pierce the gastric catheter with the needle.
Take care not to pierce the catheters especially the carotid and jugular with the needle.
- One end of the transducer has a 10 cc syringe reservoir with 0.9% saline USP for flushing blood from the carotid after each withdrawal.
- The other end has a three-way stopcock and 23-gauge needle for connection to the carotid line.
Total baseline MAP readings are 90 minutes. Sixty minutes are recorded before and 30 minutes after alcohol or water is administered intragastrically.
It is extremely important to get the rats MAP down to 40–60 mm Hg as quickly as possible. Otherwise the rat’s sympathetic compensatory mechanisms will keep MAP close to normal until the rat decompensates and death occurs.
- Take precautions not to withdraw blood or flush the line during these time points or whichever you choose to plot.
Clamp the line when changing the bolus syringe for the infusion syringe. This will prevent introduction of air bubbles inside the jugular line that could cause air emboli.
Most commercially available syringe pumps are preprogramed with the most common brands, composition, and volume syringes. However, if the syringe is not pre-programmed, it will be necessary to know the diameter of the syringe and program it into the syringe pump manually.
Generally, it is helpful to make the incision just off the midline to the side with which the rat will be laying. This will help the mesentery lay flat on the stage for microscopy imaging.
The microcirculation within the mesentery is delicate. To prevent hemorrhaging of microvessels, the mesentery should only be handled and manipulated by the intestinal walls of the small intestines.
At this point, when externalizing the mesentery, take time to untwist it. This will make splaying the mesentery flat, as well as moving new areas onto and off the stage much easier.
There are commercially available intravital microscopy stages or one can be engineered from materials. Our stage is a simple design consisting of a Plexiglas base, 3 cm culture dish serving as stage, and walled-off superfusion fluid reservoir.
The warm LR often facilitates intestinal motility, including the migrating myoelectric complex. These are rhythmic, migrating muscle contractions along the length of the intestinal wall that can interfere with microscopy of the mesenteric microcirculation. To control for this, use 2×2 gauze sponges soaked with LR and place them onto the small intestinal wall. This weighs down the intestine and helps to hold the imaging area in place.
References
- 1.Howard RJ, Slesinger PA, Davies DL, et al. Alcohol-binding sites in distinct brain proteins: the quest for atomic level resolution. Alcohol Clin Exp Res. 2011;35(9):1561–1573. doi: 10.1111/j.1530-0277.2011.01502.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whitaker AM, Sulzer JK, Molina PE. Augmented central nitric oxide production inhibits vasopressin release during hemorrhage in acute alcohol-intoxicated rodents. Am j Physiol Regul Inter Comp Phsyiol. 2011;301(5):R1529–1539. doi: 10.1152/ajpregu.00035.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC. Vital signs: binge drinking prevalence, frequency, and intensity among adults - United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(1):14–19. [PubMed] [Google Scholar]
- 4.Vonghia L, Leggio L, Ferrulli A, et al. Acute alcohol intoxication. Eur J Intern Med. 2008;19(8):561–567. doi: 10.1016/j.ejim.2007.06.033. [DOI] [PubMed] [Google Scholar]
- 5.Cherpitel CJ, Bond J, Ye Y, et al. Alcohol-related injury in the ER: a cross-national meta-analysis from the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) J Stud Alcohol. 2003;64(5):641–649. doi: 10.15288/jsa.2003.64.641. [DOI] [PubMed] [Google Scholar]
- 6.Madan AK, Yu K, Beech DJ. Alcohol and drug use in victims of life-threatening trauma. J Trauma. 1999;47(3):568–571. doi: 10.1097/00005373-199909000-00026. [DOI] [PubMed] [Google Scholar]
- 7.Jurkovich GJ, Rivara FP, Gurney JG, et al. Effects of alcohol intoxication on the initial assessment of trauma patients. Ann Emerg Med. 1992;21(6):704–708. doi: 10.1016/s0196-0644(05)82783-0. [DOI] [PubMed] [Google Scholar]
- 8.Hadfield RJ, Mercer M, Parr MJ. Alcohol and drug abuse in trauma. Resuscitation. 2001;48(1):25–36. doi: 10.1016/s0300-9572(00)00315-4. [DOI] [PubMed] [Google Scholar]
- 9.Shih HC, Hu SC, Yang CC, et al. Alcohol intoxication increases morbidity in drivers involved in motor vehicle accidents. Am J Emerg Med. 2003;21(2):91–94. doi: 10.1053/ajem.2003.50025. [DOI] [PubMed] [Google Scholar]
- 10.Maier RV. Ethanol abuse and the trauma patient. Surg Infect (Larchmt) 2001;2(2):133–141. doi: 10.1089/109629601750469456. discussion 141-134. [DOI] [PubMed] [Google Scholar]
- 11.Carden DL, Granger DN. Pathophysiology of ischaemia-reperfusion injury. J Pathol. 2000;190(3):255–266. doi: 10.1002/(SICI)1096-9896(200002)190:3<255::AID-PATH526>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 12.Childs EW, Tharakan B, Hunter FA, et al. Apoptotic signaling induces hyperpermeability following hemorrhagic shock. Am J Physiol Heart Circ Physiol. 2007;292(6):H3179–3189. doi: 10.1152/ajpheart.01337.2006. [DOI] [PubMed] [Google Scholar]
- 13.Childs EW, Tharakan B, Byrge N, et al. Angiopoietin-1 inhibits intrinsic apoptotic signaling and vascular hyperpermeability following hemorrhagic shock. Am J Physiol Heart Circ Physiol. 2008;294(5):H2285–2295. doi: 10.1152/ajpheart.01361.2007. [DOI] [PubMed] [Google Scholar]
- 14.Mathis KW, Zambell K, Olubadewo JO, et al. Altered hemodynamic counter-regulation to hemorrhage by acute moderate alcohol intoxication. Shock. 2006;26(1):55–61. doi: 10.1097/01.shk.0000215320.06866.30. [DOI] [PubMed] [Google Scholar]
- 15.Kumar P, Shen Q, Pivetti CD, et al. Molecular mechanisms of endothelial hyperpermeability: implications in inflammation. Expert Rev Mol Med. 2009;11:e19. doi: 10.1017/S1462399409001112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greiffenstein P, Mathis KW, Stouwe CV, et al. Alcohol binge before trauma/hemorrhage impairs integrity of host defense mechanisms during recovery. Alcohol Clin Exp Res. 2007;31(4):704–715. doi: 10.1111/j.1530-0277.2007.00355.x. [DOI] [PubMed] [Google Scholar]
- 17.Molina PE, Zambell KL, Norenberg K, et al. Consequences of alcohol-induced early dysregulation of responses to trauma/hemorrhage. Alcohol. 2004;33(3):217–227. doi: 10.1016/j.alcohol.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Phelan H, Stahls P, Hunt J, et al. Impact of alcohol intoxication on hemodynamic, metabolic, and cytokine responses to hemorrhagic shock. J Trauma. 2002;52(4):675–682. doi: 10.1097/00005373-200204000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Mathis KW, Molina PE. Transient central cholinergic activation enhances sympathetic nervous system activity but does not improve hemorrhage-induced hypotension in alcohol-intoxicated rodents. Shock. 2009;32(4):410–415. doi: 10.1097/SHK.0b013e31819e2d13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Molina MF, Whitaker A, Molina PE, et al. Alcohol does not modulate the augmented acetylcholine-induced vasodilatory response in hemorrhaged rodents. Shock. 2009;32(6):601–607. doi: 10.1097/SHK.0b013e31819e2b9a. [DOI] [PubMed] [Google Scholar]
- 21.Doggett TM, Breslin JW. Acute alcohol intoxication-induced microvascular leakage. Alcohol Clin Exp Res. 2014;38(9):2414–2426. doi: 10.1111/acer.12525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y, Post WS, Dalal D, et al. Coffee, alcohol, smoking, physical activity and QT interval duration: results from the Third National Health and Nutrition Examination Survey. PLoS One. 2011;6(2):e17584. doi: 10.1371/journal.pone.0017584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aasebo W, Erikssen J, Jonsbu J, et al. ECG changes in patients with acute ethanol intoxication. Scand Cardiovasc J. 2007;41(2):79–84. doi: 10.1080/14017430601091698. [DOI] [PubMed] [Google Scholar]
- 24.Lorsheyd A, de Lange DW, Hijmering ML, et al. PR and OTc interval prolongation on the electrocardiogram after binge drinking in healthy individuals. Neth J Med. 2005;63(2):59–63. [PubMed] [Google Scholar]
- 25.Souza-Smith FM, Kurtz KM, Molina PE, et al. Adaptation of mesenteric collecting lymphatic pump function following acute alcohol intoxication. Microcirculation. 2010;17(7):514–524. doi: 10.1111/j.1549-8719.2010.00050.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duran WN, Sanchez FA, Breslin JW. Microcirculatory Exchange Function. In: Tuma RF, Duran WN, Ley K, editors. Handbook of Physiology: Microcirculation. 2. Academic Press - Elsevier; San Diego, CA: 2008. pp. 81–124. [Google Scholar]
- 27.Breslin JW, Wu MH, Guo M, et al. Toll-like receptor 4 contributes to microvascular inflammation and barrier dysfunction in thermal injury. Shock. 2008;29(3):349–355. doi: 10.1097/shk.0b013e3181454975. [DOI] [PubMed] [Google Scholar]
- 28.Hatakeyama T, Pappas PJ, Hobson RW, 2nd, et al. Endothelial nitric oxide synthase regulates microvascular hyperpermeability in vivo. J Physiol. 2006;574(Pt 1):275–281. doi: 10.1113/jphysiol.2006.108175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morganroth J. Cardiac repolarization and the safety of new drugs defined by electrocardiography. Clin Pharmacol Ther. 2007;81(1):108–113. doi: 10.1038/sj.clpt.6100010. [DOI] [PubMed] [Google Scholar]
- 30.Farraj AK, Hazari MS, Cascio WE. The utility of the small rodent electrocardiogram in toxicology. Toxicol Sci. 2011;121(1):11–30. doi: 10.1093/toxsci/kfr021. [DOI] [PubMed] [Google Scholar]
- 31.Couderc JP. Measurement and regulation of cardiac ventricular repolarization: from the QT interval to repolarization morphology. Philos Trans A Math Phys Eng Sci. 2009;367(1892):1283–1299. doi: 10.1098/rsta.2008.0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varro A, Baczko I. Cardiac ventricular repolarization reserve: a principle for understanding drug-related proarrhythmic risk. Br J Pharmacol. 2011;164(1):14–36. doi: 10.1111/j.1476-5381.2011.01367.x. [DOI] [PMC free article] [PubMed] [Google Scholar]