Abstract
Background:
The goal of awake craniotomy is to maintain adequate sedation, analgesia, respiratory, and hemodynamic stability and also to provide a cooperative patient for neurologic testing. An observational study carried out to evaluate the efficacy of dexmedetomidine sedation for awake craniotomy.
Materials and Methods:
Adult patients with age >18 year who underwent awake craniotomy for intracranial tumor surgery were enrolled. Those who were uncooperative and had difficult airway were excluded from the study. In the operating room, the patients received a bolus dose of dexmedetomidine 1 μg/kg followed by an infusion of 0.2–0.7 μg/kg/h (bispectral index target 60–80). Once the patients were sedated, scalp block was given with bupivacaine 0.25%. The data on hemodynamics at various stages of the procedure, intraoperative complications, total amount of fentanyl used, intravenous fluids required, blood loss and transfusion, duration of surgery, Intensive Care Unit (ICU), and hospital stay were collected. The patients were assessed for Glasgow outcome scale (GOS) score and patient satisfaction score (PSS).
Results:
A total of 27 patients underwent awake craniotomy during a period of 2 years. Most common intraoperative complication was seizures; observed in five patients (18.5%). None of these patients experienced any episode of desaturation. Two patients had tight brain for which propofol boluses were administered. The average fentanyl consumption was 161.5 ± 85.0 μg. The duration of surgery, ICU, and hospital stays were 231.5 ± 90.5 min, 14.5 ± 3.5 h, and 4.7 ± 1.5 days, respectively. The overall PSS was 8 and GOS was good in all the patients.
Conclusion:
The use of dexmedetomidine infusion with regional scalp block in patients undergoing awake craniotomy is safe and efficacious. The absence of major complications and higher PSS makes it close to an ideal agent for craniotomy in awake state.
Keywords: Awake craniotomy, complication, dexmedetomidine, monitored anesthesia care, propofol
Introduction
Awake craniotomy allows neurological examination to be performed during the excision of lesions located near the eloquent areas of the brain.[1] It may not be considered as a new technique, but the anesthetic and surgical advancements have definitely given it a new direction. The old technique of simple trephination under local anesthesia has been replaced by highly skilled neuronavigation and cortical mapping-assisted surgeries for which anesthetic technique has also seen a changeover. Asleep-awake-asleep (AAA) or monitored anesthesia care (MAC) are the two commonly used anesthesia techniques for carrying out awake craniotomy.[2] The AAA technique involves administration of general anesthesia (GA) with controlled ventilation for the first and last part of the surgery and requires waking up of patient during neurological testing. It involves more intraoperative airway manipulations which may be challenging at times. On the other hand, MAC technique employs combination of scalp block and sedation. The sedation has to be carefully titrated as undersedation may make the patient uncomfortable or anxious whereas oversedation may lead to airway obstruction, hypercapnia, brain bulge, and hypoxia.
Earlier, droperidol-fentanyl combination was used for sedation which has been replaced by propofol-opioid combination.[3] With the availability of dexmedetomidine, an α2-agonist, anesthesiologists all over the world are now preferring it because of its definite advantages over propofol. It provides sedation and analgesia without causing respiration depression and patient is arousable despite being sedated. The safety profile of newer drugs, better monitoring techniques, and advanced supraglottic airways have made awake craniotomy even possible in high-risk patients.
There are several case reports and series on the use of dexmedetomidine during awake craniotomy.[4,5,6] Here, we are describing our experience on the use of dexmedetomidine for MAC technique in a cohort of 24 patients who underwent awake craniotomy.
Materials and Methods
After approval from the Institutional Ethics Committee, written informed consent for participation in the study was obtained from all patients. The study population comprised of patients who underwent awake craniotomy at our center over a period of 2 years. Patients who were uncooperative, had altered consciousness, mental retardation, had anticipated difficult intubation, history of obstructive sleep apnea, or medical conditions preventing them to lie down for several hours, severe bradycardia, A-V block on electrocardiography (ECG), heart failure, and allergy to study drugs were excluded from the study.
During preoperative visit, the detailed explanation of the procedure including potential intraoperative discomforts (pain during local anesthetic infiltration, loud noise of drill during burr-hole, and nausea and vomiting) was made to the patient. Various tests for intraoperative neurological testing were also explained. On admission to the operating room, oxygen inhalation at the rate of 3l/min through nasal prongs was started. Standard monitoring such as ECG, blood pressure, pulse oximetry, respiratory rate, body temperature, and capnography through nasal prongs was started. For antiemetic prophylaxis, ondansetron 4 mg was administered after securing the intravenous (IV) line. Radial artery cannulation was done under local anesthesia in hand, other than the one to be tested. Bispectral index (BIS) sensor was applied, to help titrate the infusion of dexmedetomidine. Patients received a loading dose of dexmedetomidine 1.0 μg/kg infused over 10 min followed by an infusion of 0.5–0.7 μg/kg/h to maintain BIS 60–80. Fentanyl 0.5 μg/kg was administered before anticipated noxious stimuli such as scalp block, pin insertion, skin incision and if the patient still complained of having pain. Once the patient was sedated, scalp block with bupivacaine 0.25% was given by the attending anesthesiologist. Before placement of the head holder and before skin incision, the local site was infiltrated with 2% xylocaine. Just before dural incision, surgeons were asked to infiltrate lignocaine along dural blood vessels to block pain perception. Dexmedetomidine was reduced to 0.2 μg/kg/h after dura was opened and again increased to 0.5–0.7 μg/kg/h once the tumor excision was complete. Ramsay sedation score was additionally used to monitor the sedation level and was kept in range of 3–4 till dura was opened, 2 at the time of neurological testing and again 3–4 once the testing was completed. Total fentanyl used, IV fluids, blood loss, and duration of surgery were noted. Intraoperative complications related to airway (hypoventilation, hypoxia, desaturation, and hypercarbia), hemodynamics (hypotension, hypertension, bradycardia, and tachycardia), pain, nausea/vomiting, brain bulge, seizures, etc., were recorded. After the completion of surgery, patients were shifted to neurosurgical Intensive Care Unit (ICU). The patient's satisfaction was assessed using numerical rating scale (patient satisfaction score [PSS], range 0–10) 1 h after surgery. Duration of ICU, hospital stay, and Glasgow outcome scale (GOS) score were noted at discharge.
Results
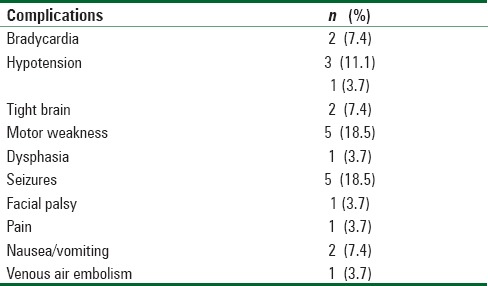
A total of 27 patients were included in this study, out of which 20 were male, and 7 were females. Mean age of the patients was 40 years [Table 1]. All patients were scheduled for craniotomy and excision of supratentorial tumors. Majority of the patients had left-sided tumor except for 3 patients who had tumors on the right side. Figure 1 illustrates the timeline of intraoperative management and hemodynamic changes at different stages of the procedure. Seizures and hemodynamic disturbances were the most common complications in these patients [Table 2]. Two patients had tight brain for which propofol boluses were administered. Intraoperatively, the amount of fentanyl and fluid administered was 161.5 ± 85.0 μg and 2.2 ± 0.8 liters, respectively. Mean duration of surgery was 231.5 ± 90.5 min. The mean duration of ICU stay and hospital stay was 14.5 ± 3.5 h and 4.7 ± 1.5 days, respectively. The average PSS was 8. New neurological deficit occurred in six patients. GOS at discharge was good in all (5 had GOS 4, rest had GOS 5) with mean GOS being 4.8.
Table 1.
Demographic data
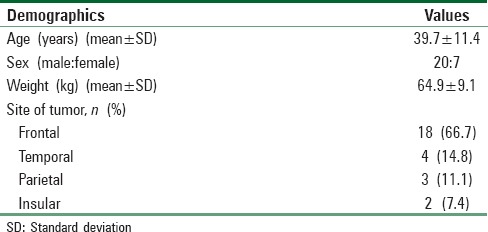
Figure 1.
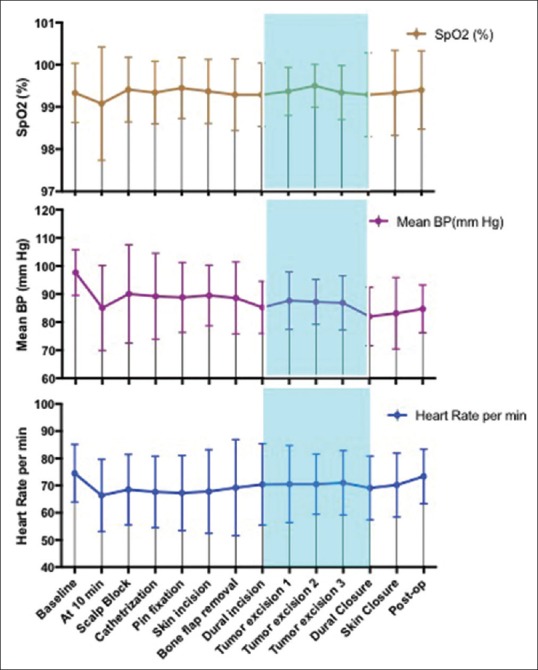
Hemodynamic changes at different stages of awake craniotomy
Table 2.
Intraoperative complications
Discussion
Task-related functional magnetic resonance imaging (fMRI) also helps in delineating the eloquent areas which need to be preserved during surgery for ensuring the optimum quality of patient's life. However, preoperative fMRI may not always be accurate as potential brain shifts may occur during course of anesthesia, positioning, and surgery itself.[7,8] Thus, awake craniotomy with intraoperative cortical stimulation mapping is considered as the gold standard for the identification of functional areas of brain.
The choice of anesthetic technique depends on factors such as patient's state, anesthetist's expertise, and available airway gadgets. AAA technique usually involves GA for the first and last part of surgery and awakening during tumor resection. In a study carried out by Deras et al., 140 patients underwent resection of gliomas under intermittent GA with controlled ventilation for AAA brain surgery.[9] The authors have claimed that it reduces the occurrence of dangerous movements, pain, unpleasant memories, exertion, and anxiety during the craniotomy and wound closure. The authors have stated that adequate depth of sedation is difficult to achieve without a concomitant increased risk of respiratory depression. This may happen in patients sedated with propofol. However, dexmedetomidine has a definite advantage of maintaining the respiration and arousability during sedation. Moreover, securing the airway and converting to GA for the last part of surgery may not always be easy. A fixed head, flexed neck, position other than supine and open cranium with limited access to head, places the anesthesiologist in difficult situation for securing the airway. Even laryngeal mask airway and video laryngoscopes may fail at such times if adequate space for maneuvering them is not available. MAC technique has an advantage that airway manipulation is routinely not required except during possible complications. Thus, it places us at a risk of encountering difficult intubation state less often. At our institute, we routinely practice MAC for all patients undergoing awake craniotomy. Another awake-awake-awake technique has been proposed where craniotomy is carried out without any sedation and only under nerve block along with therapeutic communication provided by a contact person.[10] However, we believe that nerve block itself induces pain and administering analgesia and sedation titrated to BIS is beneficial to patient while avoiding adverse effects. Another recent finding that at equivalent sedation level, midazolam, and propofol augments neurologic dysfunction more frequently than fentanyl and dexmedetomidine in patients having supratentorial tumors, may give more of a reason to favor the use of dexmedetomidine for these procedures.[11]
Other than the reassurance, we did not use anxiolytics for premedication. Benzodiazepines may interfere with electrocorticography (ECoG) and should not be used before surgery. Similarly, use of vagolytics is also controversial, may be used for counteracting bradycardia induced by dexmedetomidine. However, dexmedetomidine also dries up salivary secretions, and this effect may be aggravated by addition of vagolytics.
Drummond et al. studied the effect of dexmedetomidine on cerebral blood flow (CBF) velocity, cerebral metabolic rate (CMR), and carbon dioxide response in healthy volunteers.[12] They found that it caused a dose-related reduction in both CBF and CMR but maintained CMR-CBF coupling during both normocapnia and hypocapnia. It has also been seen to inhibit the hypercapnic-induced cerebral vasodilation, which may prove beneficial in sedated patients undergoing awake craniotomy.[13] Moreover, at usual doses, it does not reduce the spike activity and enables intraoperative ECoG to be carried out during resection of epileptic foci.[14,15]
Hemodynamic effect of dexmedetomidine infusion is an important concern. It has been seen that a dose of 1 μg/kg dexmedetomidine over 2 min produces a transient increase in blood pressure and concomitant reduction in heart rate (HR) due to stimulation of peripheral α2 β-adrenoceptors.[16] Later, inhibition of central sympathetic outflow results in stabilization of blood pressure and HR to a lower level than baseline. The initial hypertensive effect can be attenuated by slowing down the bolus rate over 10–20 min. Some anesthesiologists may omit the bolus dose and start with the maintenance dose of 0.5–0.7 μg/kg/h to avoid any hemodynamic alterations. These changes may be accentuated during the practice of concomitant administration of propofol/remifentanil. However, increased release of catecholamine in an awake patient who is solely receiving loading dose of dexmedetomidine may not result in excessive sympathetic blockade. We used a bolus dose of 1 μg/kg over 10 min followed by maintenance dose of 0.2–0.5 μg/kg. The bolus dose ensured adequate anxiolysis and sedation while carrying out regional scalp block, urinary catheterization, and additional vascular cannulation. The occurrence of hypertension with bolus dose was not observed in any of these patients. Hypotension occurred in three patients, out of which only one case was attributed to dexmedetomidine infusion, where bradycardia (HR <50/min) and hypotension (mean arterial pressure <60 mmHg) occurred during dural incision. Hypotension was corrected within 4 min after rate of dexmedetomidine infusion was decreased from 0.7–0.2 μg/kg. Another patient had sagittal sinus bleed and associated hypotension which was managed with IV fluids and IV mephentermine. Third patient had bradycardia and transient hypotension during the excision of tumor which also was unrelated to the drug.
None of the patients experienced any airway complication. Episodes of airway obstruction, desaturation, and apnea have been observed to occur in about 11.36% of patients receiving propofol.[17] None of our patients experienced any airway complication which confirms its safe respiratory profile. Most common intraoperative complication was seizures. Sokhal et al. observed the incidence of seizures in dexmedetomidine group was 30% as compared to 4.5% in propofol group (P = 0.03).[17] Dexmedetomidine is a highly selective α2-agonist and it reduces the central noradrenergic activity. This depletion of central norepinephrine may facilitate the seizure activity. Chaitanya et al. assessed the effect of dexmedetomidine on ECoG spikes intraoperatively in 34 patients.[15] The authors found that dexmedetomidine infusion 1 μg/kg over 5 min increased the spike rate in 67.6% patients and thus concluded that it is useful during intraoperative ECoG recording as it enhances or does not alter spike rate in majority of the cases. Mirski et al. studied the proconvulsant effect of dexmedetomidine in 82 male rats. Infusion of dexmedetomidine at 100 and 500 μg/kg resulted in a marked sedative response and reduced the electroencephalogram seizure threshold.[18] This proconvulsant activity was dose dependent and was blocked by α2-receptor antagonist, atipamezole. The dose used in our study was much less. The occurrence of seizures in these patients was mostly due to electrostimulation of cortex and handling of brain parenchyma. Dexmedetomidine may reduce the seizure threshold resulting in increased incidence of seizures, as seen in our patients. This may be an important undesirable side effect of dexmedetomidine which needs further evaluation. Larger prospective trials are required to confirm whether at clinical doses used, this double-sword effect is a boon during ECoG recording or runs the risk of eliciting frank seizures.
Two patients presented with tight brain for which propofol bolus and additional dose of mannitol was administered. Both of them were easily arousable and breathing spontaneously having PaCO2 34–38 mmHg. Administration of dexmedetomidine in the presence of intracranial hypertension does not affect intracranial pressure, and it is unlikely to be responsible for tense brain in our patients.[19,20]
One of the rare undesirable side effects of dexmedetomidine described in literature is agitation, which if happens may negatively affect the whole objective of carrying out awake craniotomy. This effect has been proposed to be due to central postsynaptic α-receptor activity.[21] Ard et al. observed, 2/17 cases of agitation during AAA technique using propofol and dexmedetomidine; it was managed with only reassurance.[22] However, no such side effect was observed in our patients, and all stayed calm and cooperative during the procedure. However, neurologic deficit occurred in five patients (motor weakness in four, dysphasia in one). Three patients had seizures followed by postictal motor weakness while 2 developed new deficit while excision of tumor. The overall PSS was high (8/10), and all of them had a good outcome (GOS 4 and 5).
Conclusion
The use of dexmedetomidine infusion with regional scalp block in patients undergoing awake craniotomy is safe and efficacious. Whether it has a propensity to reduce seizure threshold needs further evaluation. Overall, the absence of major complications and higher PSS makes it close to an ideal agent for craniotomy in awake state.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Yordanova YN, Moritz-Gasser S, Duffau H. Awake surgery for WHO grade II gliomas within “noneloquent” areas in the left dominant hemisphere: Toward a “supratotal” resection. Clinical article. J Neurosurg. 2011;115:232–9. doi: 10.3171/2011.3.JNS101333. [DOI] [PubMed] [Google Scholar]
- 2.Rath GP, Mahajan C, Bithal PK. Anaesthesia for awake craniotomy. J Neuroanaesth Crit Care. 2014;1:173–7. [Google Scholar]
- 3.Silbergeld DL, Mueller WM, Colley PS, Ojemann GA, Lettich E. Use of propofol (Diprivan) for awake craniotomies: Technical note. Surg Neurol. 1992;38:271–2. doi: 10.1016/0090-3019(92)90038-o. [DOI] [PubMed] [Google Scholar]
- 4.Garavaglia MM, Das S, Cusimano MD, Crescini C, Mazer CD, Hare GM, et al. Anesthetic approach to high-risk patients and prolonged awake craniotomy using dexmedetomidine and scalp block. J Neurosurg Anesthesiol. 2014;26:226–33. doi: 10.1097/ANA.0b013e3182a58aba. [DOI] [PubMed] [Google Scholar]
- 5.Chung YH, Park S, Kim WH, Chung IS, Lee JJ. Anesthetic management of awake craniotomy with laryngeal mask airway and dexmedetomidine in risky patients. Korean J Anesthesiol. 2012;63:573–5. doi: 10.4097/kjae.2012.63.6.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Everett LL, van Rooyen IF, Warner MH, Shurtleff HA, Saneto RP, Ojemann JG, et al. Use of dexmedetomidine in awake craniotomy in adolescents: Report of two cases. Paediatr Anaesth. 2006;16:338–42. doi: 10.1111/j.1460-9592.2005.01697.x. [DOI] [PubMed] [Google Scholar]
- 7.Giussani C, Roux FE, Ojemann J, Sganzerla EP, Pirillo D, Papagno C, et al. Is preoperative functional magnetic resonance imaging reliable for language areas mapping in brain tumor surgery? Review of language functional magnetic resonance imaging and direct cortical stimulation correlation studies. Neurosurgery. 2010;66:113–20. doi: 10.1227/01.NEU.0000360392.15450.C9. [DOI] [PubMed] [Google Scholar]
- 8.Trinh VT, Fahim DK, Maldaun MV, Shah K, McCutcheon IE, Rao G, et al. Impact of preoperative functional magnetic resonance imaging during awake craniotomy procedures for intraoperative guidance and complication avoidance. Stereotact Funct Neurosurg. 2014;92:315–22. doi: 10.1159/000365224. [DOI] [PubMed] [Google Scholar]
- 9.Deras P, Moulinié G, Maldonado IL, Moritz-Gasser S, Duffau H, Bertram L, et al. Intermittent general anesthesia with controlled ventilation for asleep-awake-asleep brain surgery: A prospective series of 140 gliomas in eloquent areas. Neurosurgery. 2012;71:764–71. doi: 10.1227/NEU.0b013e3182647ab8. [DOI] [PubMed] [Google Scholar]
- 10.Hansen E, Seemann M, Zech N, Doenitz C, Luerding R, Brawanski A, et al. Awake craniotomies without any sedation: The awake-awake-awake technique. Acta Neurochir (Wien) 2013;155:1417–24. doi: 10.1007/s00701-013-1801-2. [DOI] [PubMed] [Google Scholar]
- 11.Lin N, Han R, Zhou J, Gelb AW. Mild sedation exacerbates or unmasks focal neurologic dysfunction in neurosurgical patients with supratentorial brain mass lesions in a drug-specific manner. Anesthesiology. 2016;124:598–607. doi: 10.1097/ALN.0000000000000994. [DOI] [PubMed] [Google Scholar]
- 12.Drummond JC, Dao AV, Roth DM, Cheng CR, Atwater BI, Minokadeh A, et al. Effect of dexmedetomidine on cerebral blood flow velocity, cerebral metabolic rate, and carbon dioxide response in normal humans. Anesthesiology. 2008;108:225–32. doi: 10.1097/01.anes.0000299576.00302.4c. [DOI] [PubMed] [Google Scholar]
- 13.Takenaka M, Iida H, Iida M, Dohi S. Intrathecal dexmedetomidine attenuates hypercapnic but not hypoxic cerebral vasodilation in anesthetized rabbits. Anesthesiology. 2000;92:1376–84. doi: 10.1097/00000542-200005000-00028. [DOI] [PubMed] [Google Scholar]
- 14.Souter MJ, Rozet I, Ojemann JG, Souter KJ, Holmes MD, Lee L, et al. Dexmedetomidine sedation during awake craniotomy for seizure resection: Effects on electrocorticography. J Neurosurg Anesthesiol. 2007;19:38–44. doi: 10.1097/01.ana.0000211027.26550.24. [DOI] [PubMed] [Google Scholar]
- 15.Chaitanya G, Arivazhagan A, Sinha S, Reddy KR, Thennarasu K, Bharath RD, et al. Dexmedetomidine anesthesia enhances spike generation during intra-operative electrocorticography: A promising adjunct for epilepsy surgery. Epilepsy Res. 2015;109:65–71. doi: 10.1016/j.eplepsyres.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 16.Bloor BC, Ward DS, Belleville JP, Maze M. Effects of intravenous dexmedetomidine in humans. II. Hemodynamic changes. Anesthesiology. 1992;77:1134–42. doi: 10.1097/00000542-199212000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Sokhal N, Rath GP, Chaturvedi A, Dash HH, Bithal PK, Chandra PS, et al. Anaesthesia for awake craniotomy: A retrospective study of 54 cases. Indian J Anaesth. 2015;59:300–5. doi: 10.4103/0019-5049.156878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mirski MA, Rossell LA, McPherson RW, Traystman RJ. Dexmedetomidine decreases seizure threshold in a rat model of experimental generalized epilepsy. Anesthesiology. 1994;81:1422–8. doi: 10.1097/00000542-199412000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Zornow MH, Scheller MS, Sheehan PB, Strnat MA, Matsumoto M. Intracranial pressure effects of dexmedetomidine in rabbits. Anesth Analg. 1992;75:232–7. doi: 10.1213/00000539-199208000-00014. [DOI] [PubMed] [Google Scholar]
- 20.James ML, Olson DM, Graffagnino C. A pilot study of cerebral and haemodynamic physiological changes during sedation with dexmedetomidine or propofol in patients with acute brain injury. Anaesth Intensive Care. 2012;40:949–57. doi: 10.1177/0310057X1204000605. [DOI] [PubMed] [Google Scholar]
- 21.Banik S, Rath GP, Huygen FJ. Dexmedetomidine infusion may cause agitation during procedural sedation. Pain Pract. 2016;16:E89. doi: 10.1111/papr.12434. [DOI] [PubMed] [Google Scholar]
- 22.Ard JL, Jr, Bekker AY, Doyle WK. Dexmedetomidine in awake craniotomy: A technical note. Surg Neurol. 2005;63:114–6. doi: 10.1016/j.surneu.2004.02.029. [DOI] [PubMed] [Google Scholar]


