Abstract
Patients with Duchenne muscular dystrophy (DMD) often have systemic manifestations with comorbid involvement of the cardiac and respiratory systems that increase the risk of anesthetic and perioperative morbidity. These patients frequently develop progressive myocardial involvement with cardiomyopathy, depressed cardiac function, and arrhythmias. The latter may necessitate the placement of an automatic implantable cardioverter defibrillator (AICD) insertion. As a means of avoiding the need for general anesthesia and its inherent potential of morbidity, regional anesthesia may be used in specific cases. We present two cases of successful AICD insertion in patients with DMD using unilateral pectoralis and intercostal nerve blocks supplemented with intravenous sedation. Relevant anatomy for this regional anesthetic technique is reviewed and benefits of this anesthetic technique compared to general anesthesia are discussed.
Keywords: Duchenne muscular dystrophy, Pectoralis block, regional anesthesia
Introduction
Duchenne muscular dystrophy (DMD) is one of the groups of neuromuscular diseases of dystrophinopathies resulting from a mutation in the cytoskeletal dystrophin gene.[1] It is an X-linked recessive disorder that is often inherited (70%) but can also be the result of a spontaneous mutation.[1] The genetic defect results in defective dystrophin protein, causing an interruption of the dystroglycan complex connection to the intracellular contractile apparatus.[2] The physiological consequence is mechanical skeletal muscle weakness causing membrane damage with cellular contraction. DMD is the most common form of muscular dystrophy affecting 1 in every 5,000 males born in the United States.[3]
Clinically, patients develop scoliosis and kyphosis that contribute to decreased pulmonary function. As many as 77% of patients with DMD also have some form of cardiac involvement.[3,4] The incidence of cardiomyopathy increases with age from 25% of patients at age 6 years, 59% by age 10 years, and more than 90% over 18 years of age. The dilated cardiomyopathy results in arrhythmias and heart failure in this patient population. The placement of an automatic implantable cardioverter defibrillator (AICD) has been used to prevent sudden cardiac death in patients with a left ventricular ejection fraction <35%.[5] Anesthetic management for these patients may present several challenges related to the comorbid involvement of the cardiac and respiratory systems.[6,7] In various clinical scenarios, regional anesthesia may offer an option to general anesthesia. We present two cases of successful AICD insertion in patients with DMD using unilateral pectoralis (PEC) and intercostal nerve blocks supplemented with intravenous sedation. Relevant anatomy for this regional anesthetic technique is reviewed and benefits of this anesthetic technique compared to general anesthesia are discussed.
Case Reports
Institutional Review Board approval is not required for case reports involving two or fewer patients at Nationwide Children's Hospital (Columbus, Ohio).
Patient #1
A 16-year-old, 114 kg adolescent male with the past medical history of DMD, respiratory insufficiency requiring bilevel positive airway pressure (BiPAP) at night, and cardiomyopathy (ejection fraction or EF = 23%) was admitted with episodes of ventricular tachycardia. He was scheduled for AICD placement. After placement of standard American Society of Anesthesiologists’ (ASA) monitors, premedication included midazolam (1 mg increments to a total of 3 mg). PEC and intercostal blocks (see below) were performed with a total of 25 mL of 0.5% ropivacaine with 1:200,000 epinephrine. Sedation for the procedure was provided by a dexmedetomidine infusion at 0.3–0.7 μg/kg/min and additional midazolam. Supplemental local anesthetic was provided at the site of the incision for the AICD generator pocket and additional sedation provided by ketamine (45 mg) before the defibrillator testing. The patient maintained a natural airway supplemented with oxygen administered by nasal cannula at 2 l/min. He tolerated the procedure well and was discharged home the following day.
Patient #2
A 25-year-old, 72 kg man with DMD and cardiomyopathy (EF 25%–35%), was admitted with syncopal episodes, which were demonstrated to be the result of intermittent episodes of ventricular tachycardia. He was scheduled for AICD placement. After placement of ASA monitors, premedication was provided by intravenous midazolam (2 mg). A total of 20 mL of 0.5% ropivacaine with 1:200,000 epinephrine was equally deposited for the PEC and intercostal blocks as well as local subcutaneous infiltration. Sedation for the case was provided dexmedetomidine at 0.6 μg/kg/min, midazolam (2 mg), fentanyl (100 μg), and ketamine (two doses of 35 mg). The first dose of ketamine was administered at the time of incision and the second immediately before defibrillation testing. The patient maintained a natural airway supplemented with oxygen administered by nasal cannula at 2 L/min. He tolerated the procedure well and returned to the inpatient ward following the procedure.
Technique of pectoralis and intercostal nerve blockade
The PEC block targets the lateral and medial pectoral nerves. These blocks are performed with the patient in the supine position, placing the ipsilateral arm in an adducted 90o position. After anxiolysis with midazolam as needed, a high-frequency linear ultrasound probe is placed in the infraclavicular region, and the axillary vasculature is identified [Figure 1]. Moving caudally and laterally to reach 4th rib, after skin infiltration with lidocaine, the needle is inserted in plane from medial to lateral direction, local anesthetic is deposited between the fascial plane of the PEC major and minor muscle (targeting the lateral pectoral nerve, PEC I) and between the PEC minor and serratus anterior muscle (targeting the medial pectoral nerve, PECS II) [Figure 2].
Figure 1.
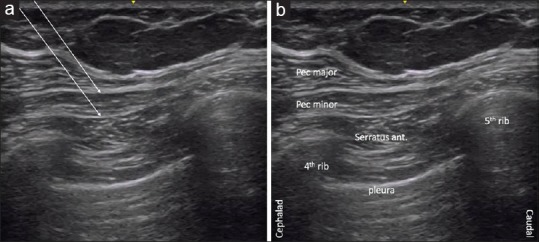
Ultrasound image showing the needle path for the pectolaris blocks (a). The relevant anatomical structures are labeled (b)
Figure 2.

Ultrasound probe placement for the pectolaris blocks, with cephalad on the left and caudad on the right. Needle insertion is in-plane with the ultrasound probe
Intercostal nerve blockade targets the ventral rami of the thoracic nerve roots. These nerves penetrate the posterior intercostal membrane to run along the subcostal groove of each rib with the intercostal vessels. Using a linear high-frequency ultrasound probe at the midaxillary line, the 3rd intercostal space is identified, and local anesthetic agent injected inferior to the intercostal vessels after negative aspiration.
The most significant potential complication of the intercostal nerve block is local anesthetic systemic toxicity (LAST) as absorption from the intercostal space is rapid. Strict attention to dosing recommendations is suggested with careful aspiration before injection to avoid inadvertent systemic injection. The use of ultrasound guidance can limit the amount of local anesthetic that is required thus reducing the risk. In the event of LAST, the administration of intralipid (20% solution) is instrumental in the treatment algorithm. Other possible complications include pneumothorax, vascular injury and resulting hematoma, or nerve injury. Specifically, for the PEC block, anesthesia or nerve injury of the long thoracic nerve or thoracodorsal nerve may occur. The long thoracic nerve runs on the outer surface of the serratus anterior muscle and thoracodorsal nerve runs deep in the posterior axillary wall to supply the latissimus dorsi.
Discussion
Regional anesthesia of the thoracic wall can be accomplished with various techniques including epidural, spinal, paravertebral block, intercostal nerve block, and PEC blockade. The PEC block was introduced as an easier alternative to the paravertebral block by Blanco for analgesia in breast surgery.[8,9] We report the adaptation of this block for a unique patient population as a means of avoiding general anesthesia. Patients with DMD often require ICD insertion due to their coexisting cardiomyopathy and the development of ventricular arrhythmias. Although general anesthesia is often used, patients with compromised cardiac and respiratory function are at risk for significant morbidity and mortality during the induction and maintenance of general anesthesia. Patients who have successfully avoided tracheostomy and mechanical ventilation are also hesitant to undergo procedures that subject them to endotracheal intubation. For the first time, we report anecdotal experience with the successful use of PEC blockade supplemented with either intercostal nerve block or local infiltration for ICD insertion during monitored anesthesia care in patients with DMD.
Although local anesthesia with sedation for ICD insertion has been reported previously, cooperation with such techniques may be limited related to the pain associated with widespread infiltration of the local anesthetic agent.[10,11] Some patients may not tolerate the use of surgeon delivered local anesthetic agents, instead requiring a more profound level of sensory blockade. The PEC blocks can effectively be used to anesthetize the anterior chest wall of these patients and provide adequate operating conditions. More recent reports describe several adaptations of the PEC block technique for breast surgery.[12] PEC blocks are easier to perform and can be placed in the supine position, which limits the amount of manipulation required for positioning in high-risk patients. Insertion of a needle from a medial to lateral direction reduces the likelihood of vascular or pleura puncture. The surgical incision site is immediately below the clavicle in the infraclavicular space, which highlights a limitation of the PEC block in this surgical setting. In both cases, we administered additional superficial local to the site of incision in the infraclavicular area. Discomfort and anxiety experienced with the deposition of the local anesthetic agent into this site were easily treated with a small dose of ketamine. In addition, supplemental doses of intravenous sedation may be required as noted in our cases when the AICD is tested following placement.
In summary, patients with DMD suffer from cardiomyopathy and its resulting depressed LV function and arrhythmias. They often require AICD placement. Associated respiratory comorbid conditions include chronic respiratory insufficiency and OSA. These factors may increase the risk of perioperative complications in this tenuous patient population. We present anecdotal experience with the successful use of PEC and intercostal blocks for AICD insertion. This option may be consider in both pediatric and adult patients for ICD placement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kamdar F, Garry DJ. Dystrophin-deficient cardiomyopathy. J Am Coll Cardiol. 2016;67:2533–46. doi: 10.1016/j.jacc.2016.02.081. [DOI] [PubMed] [Google Scholar]
- 2.Rybakova IN, Patel JR, Ervasti JM. The dystrophin complex forms a mechanically strong link between the sarcolemma and costameric actin. J Cell Biol. 2000;150:1209–14. doi: 10.1083/jcb.150.5.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emery AE. The muscular dystrophies. Lancet. 2002;359:687–95. doi: 10.1016/S0140-6736(02)07815-7. [DOI] [PubMed] [Google Scholar]
- 4.Nigro G, Comi LI, Politano L, Bain RJ. The incidence and evolution of cardiomyopathy in Duchenne muscular dystrophy. Int J Cardiol. 1990;26:271–7. doi: 10.1016/0167-5273(90)90082-g. [DOI] [PubMed] [Google Scholar]
- 5.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American college of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147–239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 6.Cripe LH, Tobias JD. Cardiac considerations in the operative management of the patient with Duchenne or Becker muscular dystrophy. Paediatr Anaesth. 2013;23:777–84. doi: 10.1111/pan.12229. [DOI] [PubMed] [Google Scholar]
- 7.Birnkrant DJ, Panitch HB, Benditt JO, Boitano LJ, Carter ER, Cwik VA, et al. American College of Chest Physicians consensus statement on the respiratory and related management of patients with Duchenne muscular dystrophy undergoing anesthesia or sedation. Chest. 2007;132:1977–86. doi: 10.1378/chest.07-0458. [DOI] [PubMed] [Google Scholar]
- 8.Blanco R. The ’pecs block’: A novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66:847–8. doi: 10.1111/j.1365-2044.2011.06838.x. [DOI] [PubMed] [Google Scholar]
- 9.Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of pecs II (modified pecs I): A novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59:470–5. doi: 10.1016/j.redar.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 10.Fox DJ, Davidson NC, Royle M, Bennett DH, Clarke B, Garratt CJ, et al. Safety and acceptability of implantation of internal cardioverter-defibrillators under local anesthetic and conscious sedation. Pacing Clin Electrophysiol. 2007;30:992–7. doi: 10.1111/j.1540-8159.2007.00797.x. [DOI] [PubMed] [Google Scholar]
- 11.Marquié C, Duchemin A, Klug D, Lamblin N, Mizon F, Cordova H, et al. Can we implant cardioverter defibrillator under minimal sedation? Europace. 2007;9:545–50. doi: 10.1093/europace/eum060. [DOI] [PubMed] [Google Scholar]
- 12.Fajardo-Pérez M, Altınpulluk EY, García-Miguel J, Quintana-Gordon B. Ultrasound-guided continuous interpectoral block for patient undergoing mastectomy and axillary clearance. Turk J Anaesthesiol Reanim. 2017;45:112–5. doi: 10.5152/TJAR.2017.43815. [DOI] [PMC free article] [PubMed] [Google Scholar]


