Abstract
Importance
Enhanced understanding of factors associated with symptomatic and functional recovery is instrumental to designing personalized treatment plans for people with schizophrenia. To date, this is the first study using network analysis to investigate the associations among cognitive, psychopathologic, and psychosocial variables in a large sample of community-dwelling individuals with schizophrenia.
Objective
To assess the interplay among psychopathologic variables, cognitive dysfunctions, functional capacity, personal resources, perceived stigma, and real-life functioning in individuals with schizophrenia, using a data-driven approach.
Design, Setting, and Participants
This multicenter, cross-sectional study involved 26 university psychiatric clinics and/or mental health departments. A total of 921 community-dwelling individuals with a DSM-IV diagnosis of schizophrenia who were stabilized on antipsychotic treatment were recruited from those consecutively presenting to the outpatient units of the sites between March 1, 2012, and September 30, 2013. Statistical analysis was conducted between July 1 and September 30, 2017.
Main Outcomes and Measures
Measures covered psychopathologic variables, neurocognition, social cognition, functional capacity, real-life functioning, resilience, perceived stigma, incentives, and service engagement.
Results
Of 740 patients (221 women and 519 men; mean [SD] age, 40.0 [10.9] years) with complete data on the 27 study measures, 163 (22.0%) were remitted (with a score of mild or better on 8 core symptoms). The network analysis showed that functional capacity and everyday life skills were the most central and highly interconnected nodes in the network. Psychopathologic variables split in 2 domains, with positive symptoms being one of the most peripheral and least connected nodes. Functional capacity bridged cognition with everyday life skills; the everyday life skills node was connected to disorganization and expressive deficits. Interpersonal relationships and work skills were connected to avolition; the interpersonal relationships node was also linked to social competence, and the work skills node was linked to social incentives and engagement with mental health services. A case-dropping bootstrap procedure showed centrality indices correlations of 0.75 or greater between the original and randomly defined samples up to 481 of 740 case-dropping (65.0%). No difference in the network structure was found between men and women.
Conclusions and Relevance
The high centrality of functional capacity and everyday life skills in the network suggests that improving the ability to perform tasks relevant to everyday life is critical for any therapeutic intervention in schizophrenia. The pattern of network node connections supports the implementation of personalized interventions.
This network analysis assesses the interplay among psychopathologic variables, cognitive dysfunctions, functional capacity, personal resources, perceived stigma, and real-life functioning in individuals with schizophrenia.
Key Points
Question
How are real-life functioning, psychopathologic variables, cognition, personal resources, and sociodemographic variables connected to each other in community-dwelling individuals with schizophrenia?
Findings
In this network analysis of 740 individuals with schizophrenia, functional capacity and everyday life skills were the most central and interconnected nodes, while positive symptoms were the least interconnected nodes. Real-life functioning was connected with several variables belonging to different domains.
Meaning
The high centrality of functional capacity and everyday life skills suggests that improving the ability to perform tasks relevant to everyday life is critical for any therapeutic intervention in schizophrenia, and the pattern of network node connections supports the implementation of personalized interventions for individuals with schizophrenia.
Introduction
Schizophrenia is a severe mental disorder ranking among the top 20 leading causes of disability. Although the outcome of schizophrenia is not always as poor as believed in the past, functional recovery is observed in less than 15% of patients.
Enhanced understanding of factors that hinder real-life functioning of people with schizophrenia is instrumental to design integrated and personalized treatment plans. To this aim, the Italian Network for Research on Psychoses has focused on the identification of variables influencing functioning, in particular, on the interplay among illness-related variables, personal resources, context-related variables, and real-life functioning.
However, modeling these associations and exploring their relative contribution to functioning by using structural equation models requires a priori assumptions concerning the associations among variables and the selection of predictors, mediators, and outcomes. These assumptions may not always hold, as suggested by findings of nonunidirectionality of pathways leading to functioning: illness-related constructs may influence real-life functioning and vice versa. In addition, structural equation models based on cross-sectional data do not allow simultaneous testing of reciprocal influences among predictors, mediators, and outcome measures.
Network analysis represents an important innovation in the study of the interplay among variables. It is a data-driven approach that does not rely on an a priori model of cause-effect relationships among variables and produces spatially ordered networks in which key variables are located at the center of the network and variables with fewer connections at the periphery. By inspecting a network, it is possible to understand the extent to which variables belonging to the same construct are connected and how different constructs are mutually interacting and reinforcing each other.
In this study, we applied network analysis to data collected on psychopathologic variables, neurocognition, functional capacity, personal resources, and functioning in a large sample of community-dwelling individuals with schizophrenia to gain a deeper insight into the complex mechanisms that associate these domains with each other.
Methods
Participants
Study participants were community-dwelling patients with schizophrenia who were stabilized on antipsychotic treatment and were seen consecutively at the outpatient units of 26 Italian university psychiatric clinics and/or mental health departments. Participants were recruited between March 1, 2012, and September 30, 2013. Inclusion and exclusion criteria are in eAppendix 1 in the Supplement. All patients provided written informed consent to participate after receiving a comprehensive explanation of study procedures and goals. The study protocol was approved by the local ethics committees of the participating centers (Campania University “Luigi Vanvitelli,” Naples; University of Turin, Turin; University of L’Aquila, L’Aquila; University of Bari, Bari; University of Catania, Catania; University of Foggia, Foggia; University of Genoa, Genoa; University of Cagliari, Cagliari; S. Andrea Hospital, Sapienza University of Rome, Rome; University of Siena, Siena; G. D’Annunzio University, Chieti; University of Pisa, Pisa; Sapienza University of Rome, Rome; University of Parma, Parma; University of Salerno, Salerno; University of Milan, Milan; University of L’Aquila, L’Aquila; University of Padua, Padua; Tor Vergata University of Rome, Rome; University of Brescia and Spedali Civili Hospital, Brescia; University of Eastern Piedmont, Novara; University of Bologna, Bologna; University of Florence, Florence; University of Naples Federico II, Naples; and University of Pisa, Pisa).
Measures
All measures used in the study are reported in Table 1 and described in eAppendix 1 in the Supplement. Comparability of data collection procedures was assured by a centralized training of researchers, as reported in the supplemental document. A complete description of the study procedures is provided in the article by Galderisi et al.
Table 1. Assessment Instruments and Study Measures.
| Domains and Variables | Instruments | Measures |
|---|---|---|
| Psychopathologic variables: negative symptoms, depression, overall psychopathologic variables, positive symptoms, disorganization | BNSS; CDSS; PANSS | BNSS expressive deficit (sum of the subscales blunted affect and alogia), BNSS avolition (sum of the subscales anhedonia, asociality and avolition); CDSS total score; PANSS total, PANSS positive symptom factor (sum of the items delusions, hallucinations, grandiosity and unusual thought content), PANSS disorganization (P2 item; ie, conceptual disorganization) |
| Neurocognition | MCCB | MCCB domain scores: speed of processing, verbal and spatial learning, reasoning and problem solving, attention, working memory |
| Social cognition | MCCB; FEIT; TASIT | MSCEIT managing emotion section score; FEIT total; TASIT-1, TASIT-2, and TASIT-3a |
| Real-life functioning | SLOF | SLOF interpersonal relationships, SLOF everyday life skills, SLOF work skills |
| Functional capacity | UPSA-B | UPSA-B total score |
| Service engagement with mental health services | SES | SES total score |
| Internalized stigma | ISMI | ISMI total score |
| Resilience | RSA | RSA factors: perception of self, perception of the future, social competence, family cohesion |
| Incentives | A count variable was created to reflect the availability of a disability pension, access to family financial and practical support, and registration on employment lists | Total incentives |
Abbreviations: BNSS, Brief Negative Symptom Scale; CDSS, Calgary Depression Scale for Schizophrenia; FEIT, Facial Emotion Identification Test; ISMI, Internalized Stigma of Mental Illness; MCCB, Measurement and Treatment Research to Improve Cognition in Schizophrenia Consensus Cognitive Battery; MSCEIT, Mayer-Salovey-Caruso Emotional Intelligence Test; PANSS, Positive and Negative Syndrome Scale; RSA, Resilience Scale for Adults; SES, Service Engagement Scale; SLOF, Specific Level of Functioning Scale; TASIT, The Awareness of Social Inference Test; UPSA-B, University of California San Diego Performance-based Skills Assessment Brief.
TASIT-1 indicates section 1: emotion evaluation; TASIT-2, section 2: social inference minimal; and TASIT-3, section 3: social inference–enriched.
Statistical Analysis
Statistical analysis was conducted between July 1 and September 30, 2017. Twenty-seven variables were selected for the network analyses (Table 2).
Table 2. Descriptive Statistics of the Variables Used in the Networka.
| Domains and Variables | Mean (SD) Score | Shapiro-Wilk Testb | |
|---|---|---|---|
| z | P Value | ||
| Resilience | |||
| Perception of self | 18.17 (5.49) | 0.210 | .42 |
| Perception of future | 10.73 (4.32) | 3.352 | <.001 |
| Social competence | 18.84 (5.31) | 1.802 | .04 |
| Family cohesion | 20.29 (5.72) | 2.881 | .002 |
| Neurocognition (MCCB domains) | |||
| Verbal learning | 19.37 (5.46) | 0.338 | .37 |
| Problem solving | 9.86 (6.37) | 7.606 | <.001 |
| Visuospatial memory | 16.75 (8.75) | 5.208 | <.001 |
| Attention | 1.70 (.81) | 2.537 | .006 |
| Processing speed | −1.23 (1.09) | 9.902 | <.001 |
| Working memory | −1.05 (.97) | 0.831 | .20 |
| Social cognition | |||
| MSCEIT | 90.79 (14.48) | 3.088 | <.001 |
| FEIT | 37.19 (8.27) | 7.744 | <.001 |
| TASIT-1 | 20.16 (4.97) | 7.408 | <.001 |
| TASIT-2 | 37.84 (10.52) | 4.303 | <.001 |
| TASIT-3 | 38.38 (10.87) | 6.625 | <.001 |
| Real-life functioning | |||
| SLOF interpersonal relationships | 22.56 (6.04) | 2.592 | .005 |
| SLOF everyday life skills | 46.12 (8.19) | 9.657 | <.001 |
| SLOF work skills | 20.27 (6.09) | 3.440 | <.001 |
| Psychopathologic variables | |||
| PANSS disorganization | 2.63 (1.45) | 4.504 | <.001 |
| PANSS positive symptom factor | 15.96 (6.53) | 7.480 | <.001 |
| BNSS expressive deficit domain | 12.72 (8.04) | 6.054 | <.001 |
| BNSS avolition domain | 20.70 (9.60) | 5.332 | <.001 |
| CDSS total score | 4.04 (4.05) | 8.949 | <.001 |
| Other variables | |||
| ISMI total score | 2.19 (0.44) | 2.843 | .002 |
| Engagement with services | 12.55 (7.43) | 5.324 | <.001 |
| UPSA-B functional capacity | 68.38 (21.62) | 5.498 | <.001 |
| No. of incentives enjoyed, No. (%) | |||
| 0 | 94 (12.7) | NA | NA |
| 1 | 204 (27.6) | NA | NA |
| 2 | 251 (33.9) | NA | NA |
| 3 | 138 (18.6) | NA | NA |
| 4 | 53 (7.2) | NA | NA |
Abbreviations: BNSS, Brief Negative Symptom Scale; CDSS, Calgary Depression Scale for Schizophrenia; FEIT, Facial Emotion Identification Test; ISMI, Internalized Stigma of Mental Illness; MCCB, Measurement and Treatment Research to Improve Cognition in Schizophrenia Consensus Cognitive Battery; MSCEIT, MCCB Mayer-Salovey-Caruso Emotional Intelligence Test—managing emotion section; NA, not applicable; PANSS, Positive and Negative Syndrome Scale; SLOF, Specific Level of Functioning Scale; TASIT, The Awareness of Social Inference Test (see footnote a in Table 1 for a description of the sections); UPSA-B, University of California San Diego Performance-based Skills Assessment Brief.
For a total of 740 patients.
A significant Shapiro-Wilk test indicates that the variable distribution departs from normality.
A network is a graphical representation of variables (nodes) and their correlations are depicted as edges (eFigure 1 in the Supplement). Thicker and more saturated edges represent stronger correlations, green edges represent positive correlations, and red edges represent negative correlations.
Different types of networks can be obtained: the association network uses zero-order correlations and provides a first general representation of the pairwise associations among variables. The zero-order correlation matrix of the variables is provided in the eTable in the Supplement. The concentration network is built on partial correlations, where the association between each pair of nodes is controlled for the influence of all the other variables. These correlations control for the shared variance between nodes and express the strength of the unique links connecting pairs of variables. The adaptive least absolute shrinkage and selection operator (LASSO) network is obtained by assigning penalties to partial correlations between variables to make small correlations automatically shrink to 0. Because the study variables were not normally distributed according to the Shapiro-Wilks test, we calculated nonparametric correlations using the nonparanormal transformation.
The network display was based on the algorithm of Fruchterman and Reingold, which places strongly associated nodes at the center of the graph and weakly associated ones at the periphery. The algorithm determines the proximity of nodes by weighing the attractive and repulsive forces on each node, in analogy with forces regulating molecular or planetary equilibrium, such that nodes placed more closely are those that attract each other more. To further facilitate readability, we included in the network diagram only correlations of 0.05 or more.
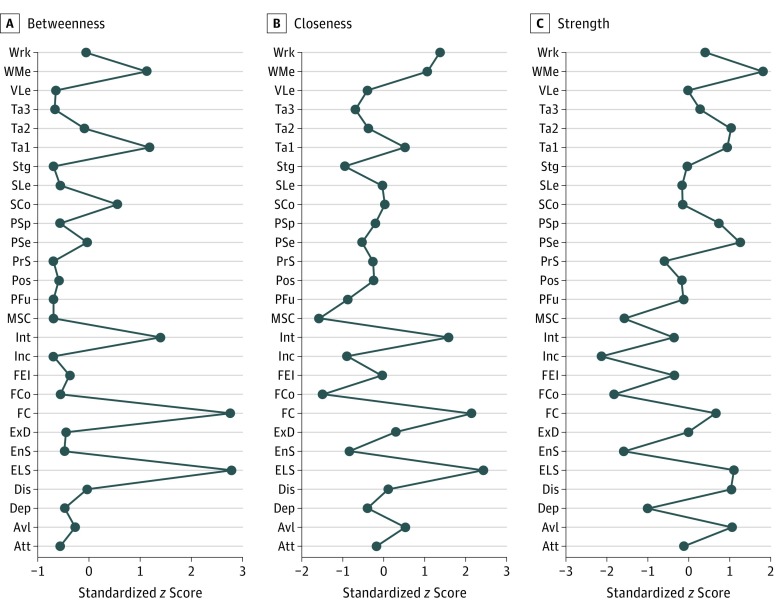
To quantify the importance of each node in the adaptive LASSO network, we computed the centrality indices of betweenness, closeness, and strength. The betweenness of a node equals the number of times that it lies on the shortest path length between any 2 other nodes. Closeness indicates how easy it is to reach all other nodes from the node of interest and is computed as the inverse of the weighed sum of distances of a given node from all other nodes in the network. Nodes with high betweenness are those that facilitate connections in the network, while nodes with high closeness affect the other nodes more quickly or are more affected by the other nodes. Last, the node strength is the sum of the correlations of 1 node to all other nodes. For each index, high values reflect great centrality in the network, but high strength may also derive from very strong correlations between peripheral nodes belonging to the same domain. Centrality plots were created to represent these indices. As suggested by Epskamp et al the robustness of the network solution was assessed by estimating the accuracy of edge weights and the stability of centrality indices. Details on these analyses are provided in eAppendix 2 in the Supplement. Adaptive LASSO networks were also obtained for male and female patients separately, to test whether known sex-specific associations among variables were confirmed.
Data management and descriptive analyses were conducted using Stata, version 13.1 (StataCorp). We used R, version 3.3.3 (R Foundation for Statistical Computing) to perform the network analysis; specifically, the package qgraph was used to obtain the network and centrality indices; bootnet, to evaluate the network stability; and NetworkComparisonTest, to test network replicability in split samples as well as in men and women.
Results
Patient Characteristics
The study sample consisted of 740 patients with complete data on the 27 variables used to build the network. Comparison of patients with complete data vs the rest of the recruited sample (n = 181) revealed no significant differences in sex, age, educational level, and severity of illness. Thus, the subgroup of patients included in the network analysis can be considered to be representative of the overall sample. Demographic and clinical characteristics of included participants are reported in Table 3.
Table 3. Demographic and Clinical Characteristics of the Study Sample .
| Characteristic | Total Participants (N = 740) |
|---|---|
| Age, mean (SD), y | 40.0 (10.9) |
| Male sex, No. (%) | 519 (70.1) |
| Married, No. (%) | 58 (7.8) |
| Working, No. (%) | 216/713 (30.3) |
| Educational level, mean (SD), y | 11.7 (3.3) |
| Age at onset, mean (SD), y | 24.1 (7.1) |
| Duration of illness, mean (SD), y | 16.4 (10.7) |
| Antipsychotic treatment at first episode, No. (%) | |
| First generation | 261 (35.3) |
| Second generation | 236 (31.9) |
| Both | 33 (4.5) |
| Unknown | 210 (28.4) |
| Current antipsychotic treatment (last 3 mo), No. (%) | |
| First generation | 107 (14.5) |
| Second generation | 510 (68.9) |
| Both | 100 (13.5) |
| None | 23 (3.1) |
| Integrated treatment, No. (%) | 203 (27.4) |
| Patients in symptomatic remission, No. (%)a | 163 (22.0) |
Individuals with a score of mild or better on 8 core symptoms, according to standardized criteria.
Network Analysis
The adaptive LASSO network (Figure 1) showed that nodes belonging to each construct were generally strongly associated and close to each other and well separated from those belonging to different constructs. As shown in Figure 1, resilience, neurocognition, social cognition, and indices of real-life functioning formed spatially contiguous patterns, with densely interconnected nodes.
Figure 1. Adaptive Least Absolute Shrinkage and Selection Operator Network of the Overall Study Population.
The thickness of an edge reflects the magnitude of the correlation (the thickest edge representing a value of 0.61, which is the correlation between Positive and Negative Syndrome Scale [PANSS] positive [Pos] and PANSS disorganization [Dis]). Green lines represent positive correlations, whereas red lines represent negative correlations. Nodes with the same color belong to the same domain. Att indicates attention; Avl, Brief Negative Symptom Scale (BNSS) avolition; Dep, Calgary Depression Scale for Schizophrenia total score for depression; Dis, PANSS disorganization; ELS, everyday life skills; EnS, service engagement; ExD, BNSS expressive deficit domain; FC, functional capacity; FCo, family cohesion; FEI, Facial Emotion Identification Test; Inc, incentives; Int, interpersonal relationships; MSC, Measurement and Treatment Research to Improve Cognition in Schizophrenia Consensus Cognitive Battery Mayer-Salovey-Caruso Emotional Intelligence Test managing emotion section; PFu, perception of future; Pos, PANSS positive factor; PrS, problem solving; PSe, perception of self; PSp, processing speed; SCo, social competence; SLe, visuospatial learning; Stg, stigma; Ta1, The Awareness of Social Inference Test (TASIT) section 1 (see footnote a in Table 1 for a description of the sections); Ta2, TASIT section 2; Ta3, TASIT section 3; VLe, verbal learning; WMe, working memory; and Wrk, Specific Level of Functioning Scale work skills.
Only items regarding psychopathologic variables were not spatially contiguous: strong links were found between avolition and diminished expression, as well as between the positive and disorganization dimensions; however, connections between negative and positive and disorganization symptoms were weak or indirect. Still, psychopathologic variable nodes were proximal and inversely correlated with the real-life functioning nodes. Only the positive symptoms node was quite isolated, and it connected to the rest of the network only through its strong association with disorganization, which, besides its connection with everyday life skills, was linked to expressive deficit and functional capacity. Positive symptoms were also connected with service engagement (the higher the positive symptoms, the poorer the service engagement). Depression was connected with avolition, bridged avolition with resilience and stigma, was linked to the resilience node perception of self, and had no direct connection with positive and disorganization symptoms.
The neurocognition and social cognition constructs were adjacent and densely connected and interconnected. In the neurocognition domain, the working memory node showed the highest centrality: it was strongly connected to all the other neurocognition nodes and bridged them with social cognition and functional capacity and, through functional capacity, with real-life functioning nodes. Verbal learning, visuospatial learning, and attention were also directly connected with functional capacity. Visuospatial learning and processing speed were directly, although weakly, connected to The Awareness of Social Inference Test (TASIT) section 1: emotion recognition node (TASIT-1).
In the social cognition domain, the TASIT-1 node showed the highest betweenness and closeness (Figure 2) and, together with TASIT section 2: social inference minimal (TASIT-2), showed the highest strength. The TASIT-1 node was connected to all the other social cognition nodes and bridged the social cognition domain with the functional capacity node and, through the functional capacity node, with the real-life functioning nodes. The TASIT-1 node also showed an inverse association with service engagement, such that, the better the social cognition, the better the service engagement.
Figure 2. Centrality Plots for Adaptive Least Absolute Shrinkage and Selection Operator Network of the Overall Study Population Depicting the Betweenness, Closeness, and Strength of Each Node.
A, Betweenness indicates the number of times a node lies on the shortest path length between any 2 other nodes. B, Closeness indicates the average distance of a node from all other nodes in the network. C, Strength quantifies the extent to which a certain node influences other nodes in the network. For each index, higher values reflect greater centrality in the network. Att indicates attention; Avl, Brief Negative Symptom Scale (BNSS) avolition; Dep, Calgary Depression Scale for Schizophrenia total score for depression; Dis, Positive and Negative Syndrome Scale (PANSS) disorganization; ELS, everyday life skills; EnS, service engagement; ExD, BNSS expressive deficit domain; FC, functional capacity; FCo, family cohesion; FEI, Facial Emotion Identification Test; Inc, incentives; Int, interpersonal relationships; MSC, Measurement and Treatment Research to Improve Cognition in Schizophrenia Consensus Cognitive Battery Mayer-Salovey-Caruso Emotional Intelligence Test managing emotion section; PFu, perception of future; Pos, PANSS positive factor; PrS, problem solving; PSe, perception of self; PSp, processing speed; SCo, social competence; SLe, visuospatial learning; Stg, stigma; Ta1, The Awareness of Social Inference Test (TASIT) section 1 (see footnote a in Table 1 for a description of the sections); Ta2, TASIT section 2; Ta3, TASIT section 3; VLe, verbal learning; WMe, working memory; and Wrk, Specific Level of Functioning Scale work skills.
In the resilience domain, social competence was the node with the highest betweenness and closeness (Figure 2). It was associated with all the other resilience nodes and bridged the resilience domain with interpersonal functioning and stigma. It was also inversely and weakly associated with avolition. Perception of self was strongly connected to social competence, perception of future, and family cohesion; it was also inversely correlated with stigma and depression.
In the real-life functioning domain, everyday life skills had the highest centrality (Figure 2). It was strongly connected with the other 2 functioning nodes (interpersonal relationships and work skills) and with functional capacity. The everyday life skills node was also inversely correlated with the expressive deficit negative symptom construct, with the disorganization dimension, and with stigma.
The functional capacity and Specific Level of Functioning Scale (SLOF) everyday life skills were the most central nodes of the whole network (highest betweenness and closeness; Figure 2). As shown in Figure 1, functional capacity bridged neurocognition and social cognition with the everyday life skills node, which, in turn, was connected to the SLOF subscales Work and Interpersonal Relationships, to the expressive deficit negative node, and to the disorganization node.
Both the interpersonal relationships node and the work skills node were inversely associated with avolition (the more severe the avolition, the poorer the functioning), but the connection was stronger between the interpersonal relationships node and avolition. Poor work functioning was also associated with the availability of incentives and poor service engagement.
The LASSO networks for male and female participants did not differ significantly at NetworkComparisonTest permutation tests of global strength (network strength, 0.557; P = .62) and structural invariance (maximum difference between edges, 0.166; P = .40).
Replicability and robustness tests demonstrated the validity of the network solution (eAppendix 2 and eFigures 2-4 in the Supplement).
Discussion
To our knowledge, this is the first study using a network approach to analyze the complex associations among psychopathologic variables, personal resources, context-related factors, and real-life functioning in a large sample of community-dwelling individuals with schizophrenia. Research studies performed to date using network analysis were focused on the interplay of symptoms in mood, anxiety, and eating disorders and only recently investigation has been extended to schizophrenia and the association of psychotic symptoms with environmental factors.
Our study confirms that social cognition, neurocognition, resilience, and real-life functioning represent robust and independent constructs, with spatially contiguous and highly interconnected nodes, regardless of the use of 1 or more measures of the same construct. Psychopathologic variable nodes are the only exception: avolition, expressive deficit, and depression form a highly interconnected pattern on 1 side of real-life functioning nodes, densely connected with them and with the area of resilience and stigma. Positive symptoms and disorganization have few connections to the other nodes, as reflected by their low betweenness and closeness. In particular, positive symptoms show no direct connection with the real-life functioning nodes.
The study clearly shows that functional capacity and everyday life skills play a key role in the network: they have the highest centrality, as shown by their location in the network and their high betweenness and closeness. Functional capacity is the node that links neurocognition and social cognition with real-life functioning nodes, in particular with everyday life skills, such as household activities, handling of personal finances, and use of the telephone or public transportation. The greater proximity of functional capacity to everyday functioning with respect to neuropsychological measures supports the choice of functional capacity as a functionally meaningful coprimary measure in clinical trials of cognition enhancement in schizophrenia.
According to the network analysis, and in line with previous reports, social cognition is highly interconnected with neurocognition, and both nodes show a strong link with functional capacity and, through functional capacity, with real-life functioning. The social cognition node directly connected to functional capacity is TASIT-1, which measures the ability to identify basic emotions in a series of brief videotaped vignettes, in which professional actors produce spontaneous emotional displays resembling those encountered in everyday social interactions.
The connection between recognition of emotions and functional capacity highlights the role of social and emotional processing in general psychosocial functioning. As pointed out by Thaler et al, individuals who are able to comprehend social and emotional stimuli may have acquired better interpersonal skills required for some of the tasks incorporated in the functional capacity assessment (eg, communication skills).
Our network analysis shows that social competence, not social cognition, is directly linked to interpersonal functioning. This connection might be the result of overlapping constructs in the 2 instruments. However, social competence is self-rated, while social cognition is based on caregiver reports.
Our network analysis did not show direct connections of social cognition with real-life functioning nodes, which is at odds with some previous reports. However, those reports used structural equation models and modeled social cognition as a mediator of neurocognitive effects on functioning. Our results cannot directly address the issue of mediation effects, as network analysis does not have a consolidated procedure to test these effects; however, they suggest that functional capacity bridges social cognition and real-life functioning.
The other key variable of the network is the domain of everyday life skills. This domain shows the highest closeness and betweenness centralities: it links real-life functioning with psychopathologic variables and functional capacity, which, in turn, connects everyday life skills to the cognition nodes. The everyday life skills are also connected, although weakly, with internalized stigma.
The other 2 real-life functioning nodes (ie, interpersonal relationships and work skills) show a lower centrality in the network. As noted by Leifker et al, different domains of everyday functioning have different determinants. Although this finding could not be tested in a previous study based on a structural equation model in which the SLOF subscales were combined into a latent variable, the network approach clearly shows that cognition and functional capacity are connected to everyday life skills but not to interpersonal functioning. On the contrary, avolition is inversely connected to interpersonal functioning and weakly connected to work skills but not to everyday life skills. This is in line with previous studies showing a significant association between SLOF interpersonal relationships and avolition, both in individuals with schizophrenia and their first-degree nonaffected relatives.
Our findings also support the discriminant validity of the 2 negative symptom factors, which, although strongly connected to each other, do show a different pattern of connections. Specifically, avolition is connected to depression and social competence, as well as to SLOF interpersonal relationships and work skills, while expressive deficit is connected with disorganization, functional capacity, and everyday life skills. Interpersonal functioning is also connected to social competence, which is actually the only node bridging resilience and real-life functioning, besides the weak connection between internalized stigma and everyday life skills.
In line with studies by Galderisi et al and Strassnig et al, our results confirm that depression has no direct influence on real-life functioning. Specifically, depression is connected to resilience, self-stigma, and avolition and only indirectly connected, through self-stigma and avolition, to the 3 nodes of functioning.
Our results might have substantial implications for treatment if they are confirmed in longitudinal studies in which the direction of effects can be tested. The high centrality of functional capacity and everyday life skills in the network is in line with the recovery-oriented approaches to schizophrenia, maintaining that the ability to perform tasks relevant to everyday life should represent the primary target of rehabilitation programs. The cross-sectional nature of our findings does not allow firm conclusions, as the centrality measures may be high because the nodes strongly influence the rest of the system but also because they are influenced by other nodes.
In spite of their cross-sectional nature, our findings strongly suggest that treatment beyond antipsychotic drugs is needed for people with schizophrenia, as positive symptoms are a peripheral node in the network. Therefore, targeting positive symptoms only, as treatment with antipsychotic medication does, is unlikely to lead to recovery in adults with schizophrenia.
In addition, the pattern of connections among the network nodes indicates that, depending on the patient’s characteristics, different rehabilitation programs should be implemented. For instance, targeting the cognition area may affect functional capacity more strongly and, with cascading effects, may improve functioning in everyday life activities and, indirectly and to a minor extent, work skills and interpersonal relationships. This finding is in line with meta-analyses of rehabilitation interventions, showing that treatment of cognitive deficits should be combined with interventions aimed at ameliorating skills deficits to yield significant functional benefits.
Strengths and Limitations
The main strength of our study is the use of the network approach to investigate the pattern of connections among a wide array of cognitive, psychopathologic, and psychosocial variables from a large sample of community-dwelling individuals with schizophrenia who are stabilized on antipsychotic treatment (mainly second-generation antipsychotic medications).
The network analysis might contribute to the shift from simpler, a priori models of established causal associations between variables to the recognition of the complex interdependence between disease-related factors, personal resources, environmental variables, and real-life functioning. This shift might be instrumental in promoting a personalized and integrated approach to the treatment of schizophrenia.
Some limitations of the study must be acknowledged. First, the cross-sectional nature of the study does not allow appropriate testing of the direction of the effects. Second, owing to the inclusion of only patients with established schizophrenia who are clinically stable, in whom the effect of positive symptoms and disorganization on functioning might be less central than in patients with a first episode of schizophrenia, our results might not generalize to the latter patient population. Third, a further limitation is represented by the fact that the effects of antipsychotics and of self-report vs interview-based instruments on the network structure cannot be estimated. Finally, the network analysis, at odds with the structural equation model, cannot address the issue of mediation effects, as it does not have a consolidated procedure to test these effects.
Conclusions
The high centrality of functional capacity and everyday life skills in the network suggests that improving the ability to perform tasks relevant to everyday life is critical for any therapeutic intervention in individuals with schizophrenia. The pattern of network node connections supports the implementation of personalized interventions.
eAppendix 1. Methods
eAppendix 2. Analysis of Network Robustness and Stability
eTable. Zero-Order Correlation Matrix of the Variables Selected for the Network Analysis
eFigure 1. Example of a Network with 5 Nodes and 6 Edges
eFigure 2. Node Strength Centrality Estimates of the 27 Nodes Obtained by the Bootstrap Sampling Procedure
eFigure 3. Results of Case-Dropping Subset Bootstrap Procedure to Assess Stability of Network Centrality Indices
eFigure 4. Bootstrapped 95% Confidence Intervals of Edge Weights for the Network of 27 Variables
eReferences.
References
- 1.Murray CJ, Lopez AD. Evidence-based health policy—lessons from the Global Burden of Disease Study. Science. 1996;274(5288):740-743. [DOI] [PubMed] [Google Scholar]
- 2.Fleischhacker WW, Arango C, Arteel P, et al. Schizophrenia—time to commit to policy change. Schizophr Bull. 2014;40(suppl 3):S165-S194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jääskeläinen E, Juola P, Hirvonen N, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull. 2013;39(6):1296-1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sergi MJ, Rassovsky Y, Nuechterlein KH, Green MF. Social perception as a mediator of the influence of early visual processing on functional status in schizophrenia. Am J Psychiatry. 2006;163(3):448-454. [DOI] [PubMed] [Google Scholar]
- 5.Couture SM, Granholm EL, Fish SC. A path model investigation of neurocognition, theory of mind, social competence, negative symptoms and real-world functioning in schizophrenia. Schizophr Res. 2011;125(2-3):152-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bowie CR, Leung WW, Reichenberg A, et al. Predicting schizophrenia patients’ real-world behavior with specific neuropsychological and functional capacity measures. Biol Psychiatry. 2008;63(5):505-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71(12):2150-2161. [DOI] [PubMed] [Google Scholar]
- 8.Galderisi S, Rossi A, Rocca P, et al. ; Italian Network For Research on Psychoses . The influence of illness-related variables, personal resources and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry. 2014;13(3):275-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bell MD, Fiszdon JM, Greig TC, Bryson GJ. Can older people with schizophrenia benefit from work rehabilitation? J Nerv Ment Dis. 2005;193(5):293-301. [DOI] [PubMed] [Google Scholar]
- 10.Bio DS, Gattaz WF. Vocational rehabilitation improves cognition and negative symptoms in schizophrenia. Schizophr Res. 2011;126(1-3):265-269. [DOI] [PubMed] [Google Scholar]
- 11.Collip D, Wigman JT, Lin A, et al. Dynamic association between interpersonal functioning and positive symptom dimensions of psychosis over time: a longitudinal study of healthy adolescents. Schizophr Bull. 2013;39(1):179-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kline RB. Assumptions of structural equation modeling In: Hoyle R, ed. Handbook of Structural Equation Modeling. New York, NY: Guilford Press; 2012:111-125. [Google Scholar]
- 13.Beard C, Millner AJ, Forgeard MJ, et al. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol Med. 2016;46(16):3359-3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Costantini G, Epskamp S, Borsboom D, et al. State of the aRt personality research: a tutorial on network analysis of personality data in R. J Res Pers. 2015;54(1):13-29. doi: 10.1016/j.jrp.2014.07.003 [DOI] [Google Scholar]
- 15.Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9(2):91-121. [DOI] [PubMed] [Google Scholar]
- 16.Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirkpatrick B, Strauss GP, Nguyen L, et al. The Brief Negative Symptom Scale: psychometric properties. Schizophr Bull. 2011;37(2):300-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mucci A, Galderisi S, Merlotti E, et al. ; Italian Network for Research on Psychoses . The Brief Negative Symptom Scale (BNSS): independent validation in a large sample of Italian patients with schizophrenia. Eur Psychiatry. 2015;30(5):641-647. [DOI] [PubMed] [Google Scholar]
- 19.Addington D, Addington J, Maticka-Tyndale E. Assessing depression in schizophrenia: the Calgary Depression Scale. Br J Psychiatry Suppl. 1993;(22):39-44. [PubMed] [Google Scholar]
- 20.Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-276. [DOI] [PubMed] [Google Scholar]
- 21.Nuechterlein KH, Green MF, Kern RS, et al. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry. 2008;165(2):203-213. [DOI] [PubMed] [Google Scholar]
- 22.Kern RS, Nuechterlein KH, Green MF, et al. The MATRICS Consensus Cognitive Battery, part 2: co-norming and standardization. Am J Psychiatry. 2008;165(2):214-220. [DOI] [PubMed] [Google Scholar]
- 23.Kerr SL, Neale JM. Emotion perception in schizophrenia: specific deficit or further evidence of generalized poor performance? J Abnorm Psychol. 1993;102(2):312-318. [DOI] [PubMed] [Google Scholar]
- 24.McDonald S, Bornhofen C, Shum D, Long E, Saunders C, Neulinger K. Reliability and validity of The Awareness of Social Inference Test (TASIT): a clinical test of social perception. Disabil Rehabil. 2006;28(24):1529-1542. [DOI] [PubMed] [Google Scholar]
- 25.Mucci A, Rucci P, Rocca P, et al. ; Italian Network for Research on Psychoses . The Specific Level of Functioning Scale: construct validity, internal consistency and factor structure in a large Italian sample of people with schizophrenia living in the community. Schizophr Res. 2014;159(1):144-150. [DOI] [PubMed] [Google Scholar]
- 26.Mausbach BT, Harvey PD, Goldman SR, Jeste DV, Patterson TL. Development of a brief scale of everyday functioning in persons with serious mental illness. Schizophr Bull. 2007;33(6):1364-1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tait L, Birchwood M, Trower P. A new scale (SES) to measure engagement with community mental health services. J Ment Health. 2002;11(2):191-198. [DOI] [PubMed] [Google Scholar]
- 28.Brohan E, Elgie R, Sartorius N, Thornicroft G; GAMIAN-Europe Study Group . Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: the GAMIAN-Europe study. Schizophr Res. 2010;122(1-3):232-238. [DOI] [PubMed] [Google Scholar]
- 29.Friborg O, Hjemdal O, Rosenvinge JH, Martinussen M. A new rating scale for adult resilience: what are the central protective resources behind healthy adjustment? Int J Methods Psychiatr Res. 2003;12(2):65-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cox DR, Wermuth N. Linear dependencies represented by chain graphs. Stat Sci. 1993;8(3):204-218. doi: 10.1214/ss/1177010887 [DOI] [Google Scholar]
- 31.Liu H, Han F, Yuan M, Lafferty J, Wasserman L. High-dimensional semiparametric Gaussian copula graphical models. Ann Stat. 2012;40(4):2293-2326. doi: 10.1214/12-AOS1037 [DOI] [Google Scholar]
- 32.Fruchterman TMJ, Reingold EM. Graph drawing by force-directed placement. Softw Pract Exper. 1991;21(11):1129-1164. doi: 10.1002/spe.4380211102 [DOI] [Google Scholar]
- 33.Freeman LC. Centrality in social networks conceptual clarification. Soc Networks. 1978;1(3):215-239. doi: 10.1016/0378-8733(78)90021-7 [DOI] [Google Scholar]
- 34.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper [published online March 24, 2017]. Behav Res Methods. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Epskamp S, Cramer AOJ, Waldorp LJ, et al. qgraph: network visualizations of relationships in psychometric data. J Stat Softw. 2012;48(4):1-18. doi: 10.18637/jss.v048.i04 [DOI] [Google Scholar]
- 36.Van Borkulo C, Boschloo L, Kossakowski J, et al. Comparing network structures on three aspects: a permutation test. https://www.researchgate.net/publication/314750838_Comparing_network_structures_on_three_aspects_A_permutation_test. Accessed December 30, 2017. [DOI] [PubMed]
- 37.Fried EI, van Borkulo CD, Cramer AO, Boschloo L, Schoevers RA, Borsboom D. Mental disorders as networks of problems: a review of recent insights. Soc Psychiatry Psychiatr Epidemiol. 2017;52(1):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Rooijen G, Isvoranu AM, Kruijt OH, et al. ; GROUP investigators . A state-independent network of depressive, negative and positive symptoms in male patients with schizophrenia spectrum disorders [published online August 22, 2017]. Schizophr Res. doi: 10.1016/j.schres.2017.07.035 [DOI] [PubMed] [Google Scholar]
- 39.Isvoranu AM, Borsboom D, van Os J, Guloksuz S. A network approach to environmental impact in psychotic disorder: brief theoretical framework. Schizophr Bull. 2016;42(4):870-873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bowie CR, Depp C, McGrath JA, et al. Prediction of real-world functional disability in chronic mental disorders: a comparison of schizophrenia and bipolar disorder. Am J Psychiatry. 2010;167(9):1116-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Strassnig MT, Raykov T, O’Gorman C, et al. Determinants of different aspects of everyday outcome in schizophrenia: the roles of negative symptoms, cognition, and functional capacity. Schizophr Res. 2015;165(1):76-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Green MF, Schooler NR, Kern RS, et al. Evaluation of functionally meaningful measures for clinical trials of cognition enhancement in schizophrenia. Am J Psychiatry. 2011;168(4):400-407. [DOI] [PubMed] [Google Scholar]
- 43.Mancuso F, Horan WP, Kern RS, Green MF. Social cognition in psychosis: multidimensional structure, clinical correlates, and relationship with functional outcome. Schizophr Res. 2011;125(2-3):143-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thaler NS, Sutton GP, Allen DN. Social cognition and functional capacity in bipolar disorder and schizophrenia. Psychiatry Res. 2014;220(1-2):309-314. [DOI] [PubMed] [Google Scholar]
- 45.Green MF, Hellemann G, Horan WP, Lee J, Wynn JK. From perception to functional outcome in schizophrenia: modeling the role of ability and motivation. Arch Gen Psychiatry. 2012;69(12):1216-1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Leifker FR, Bowie CR, Harvey PD. Determinants of everyday outcomes in schizophrenia: the influences of cognitive impairment, functional capacity, and symptoms. Schizophr Res. 2009;115(1):82-87. [DOI] [PubMed] [Google Scholar]
- 47.Galderisi S, Bucci P, Mucci A, et al. Categorical and dimensional approaches to negative symptoms of schizophrenia: focus on long-term stability and functional outcome. Schizophr Res. 2013;147(1):157-162. [DOI] [PubMed] [Google Scholar]
- 48.Galderisi S, Rossi A, Rocca P, et al. ; Italian Network for Research on Psychoses . Pathways to functional outcome in subjects with schizophrenia living in the community and their unaffected first-degree relatives. Schizophr Res. 2016;175(1-3):154-160. [DOI] [PubMed] [Google Scholar]
- 49.Farkas M. The vision of recovery today: what it is and what it means for services. World Psychiatry. 2007;6(2):68-74. [PMC free article] [PubMed] [Google Scholar]
- 50.Slade M, Amering M, Oades L. Recovery: an international perspective. Epidemiol Psichiatr Soc. 2008;17(2):128-137. [DOI] [PubMed] [Google Scholar]
- 51.Slade M, Amering M, Farkas M, et al. Uses and abuses of recovery: implementing recovery-oriented practices in mental health systems. World Psychiatry. 2014;13(1):12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Charzyńska K, Kucharska K, Mortimer A. Does employment promote the process of recovery from schizophrenia? a review of the existing evidence. Int J Occup Med Environ Health. 2015;28(3):407-418. [DOI] [PubMed] [Google Scholar]
- 53.Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168(5):472-485. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Methods
eAppendix 2. Analysis of Network Robustness and Stability
eTable. Zero-Order Correlation Matrix of the Variables Selected for the Network Analysis
eFigure 1. Example of a Network with 5 Nodes and 6 Edges
eFigure 2. Node Strength Centrality Estimates of the 27 Nodes Obtained by the Bootstrap Sampling Procedure
eFigure 3. Results of Case-Dropping Subset Bootstrap Procedure to Assess Stability of Network Centrality Indices
eFigure 4. Bootstrapped 95% Confidence Intervals of Edge Weights for the Network of 27 Variables
eReferences.