Key Points
Question
Is there a common threshold level above which blood pressure rise tends to accelerate in progression toward hypertension?
Findings
This community-based longitudinal cohort study found that, prior to hypertension onset, individuals generally maintained a resting systolic blood pressure of less than 120 to 125 mm Hg. Above this level, resting systolic blood pressure increased at a more rapid rate over time, a consistent trend whether hypertension manifested earlier or later in life.
Meaning
A resting systolic blood pressure that chronically exceeds approximately 120 to 125 mm Hg tends to signal incipient hypertension, irrespective of age.
This longitudinal cohort study aimed to identify a common threshold level above which blood pressure level rise tends to accelerate in progression toward hypertension.
Abstract
Importance
Given that hypertension remains a leading risk factor for chronic disease globally, there are substantial ongoing efforts to define the optimal range of blood pressure (BP).
Objective
To identify a common threshold level above which BP rise tends to accelerate in progression toward hypertension.
Design, Setting, and Participants
This longitudinal, community-based epidemiological cohort study of adults enrolled in Framingham, Massachusetts, included 1252 participants (mean [SD] age, 35.3 [2.7] years) from the Framingham Original Cohort, of whom 790 (63.1%) were women. Each participant contributed up to 28 serial examinations of standardized resting BP measurements between 1948 and 2005.
Exposures
Age and systolic BP.
Main Outcomes and Measures
Via a segmented mixed model, we identified significant change points in the association between advancing age and increasing systolic BP among individuals categorized by their age at hypertension onset.
Results
Individuals maintained a relatively stable resting systolic BP level prior to hypertension onset. Systolic BP level began to rise at a more rapid rate after reaching a level of 123.2 mm Hg (95% CI, 122.7-130.1 mm Hg) in people with onset at 40 to 49 years; 122.0 mm Hg (95% CI, 120.3-123.9 mm Hg) in those with onset between 50 and 59 years, 124.9 mm Hg (95% CI, 120.2-127.9 mm Hg) in those with onset between 60 and 69 years, and 120.5 mm Hg (95% CI, 118.0-123.2 mm Hg) in those with onset between 70 and 79 years (P = .29 for between-group heterogeneity).
Conclusions and Relevance
We observed that individuals in the community generally maintained a systolic BP of less than 120 to 125 mm Hg, above which systolic BP increased at a relatively rapid rate toward overt hypertension. This trend was consistent whether the hypertension manifested earlier or later in life. Thus, a resting systolic BP that chronically exceeds the range of approximately 120 to 125 mm Hg may represent an important threshold of underlying vascular remodeling and signal incipient hypertension irrespective of age. Further investigations are needed to unravel the sequence of hemodynamic and vascular changes occurring prior to hypertension onset.
Introduction
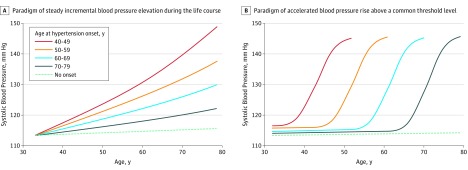
The widespread burden of hypertension and its associated risk for multisystem end-organ damage has prompted substantial ongoing efforts to define the optimal range of blood pressure (BP). The general understanding of normal BP has evolved greatly since the 1970s, when the age of a person plus 100 mm Hg was considered acceptable for systolic BP.1 Nonetheless, incremental elevations in systolic BP during the life course are still commonly believed to be a largely unavoidable feature of biological aging (Figure 1A).
Figure 1. Competing Conceptual Frameworks of Hypothetical Blood Pressure Trajectories Preceding Hypertension.
Challenging this notion are experimental data suggesting that, while many disease traits are age-related, their onset of development may be effectively delayed by biological resilience (the preservation of health despite chronic exposure to stressors) (Figure 1B).2 In this paradigm, the onset of BP elevation might occur at an earlier or a later age, at which point BP starts to rise at a relatively rapid rate. As such, then the timing and nature of the disease onset, rather than its progression, would be especially important to understand and target for intervention. In turn, more frequent clinical assessments might be warranted to monitor for a rapid progression to hypertension once BP elevation is detected at a certain threshold.
Our objective was therefore to elucidate the natural history of BP elevation in individuals with varying ages at hypertension onset. We focused particularly on discovering distinct change points in BP trajectories, defined as a level of BP beyond which the rate of BP rise accelerates.
Methods
We studied first-generation participants of the Framingham Heart Study, who compose 1 of the few existing cohorts with standardized BP measurements performed at frequent intervals (approximately every 2 years) during an extended period (1948 to 2005). In this setting, serial BP measurements collected across up to 28 examination cycles per participant allowed for precise estimates of long-term BP trajectories. The characteristics and study protocol of this original cohort (n = 5209) have been published previously.3,4 To reduce the potential effects of age, time, and birth cohort, we excluded individuals from analyses per the following criteria: participants who were older than 40 years at baseline, who had existing hypertension at baseline, who attended fewer than 3 examinations before hypertension onset, and/or who had hypertension onset before age 40 years or at or after age 80 years. The last criteria was applied because of the low number of individuals in these categories.
The institutional review board of Boston University Medical Center approved all protocols. Each participant provided informed consent.
At each examination, a physician used a mercury sphygmomanometer to perform 2 sequential BP measurements according to a standardized protocol; we calculated the mean of the 2 measurements as the final BP value.3,4 Hypertension onset was defined as a BP level greater than or equal to 140/90 mm Hg or use of antihypertensive medication at 2 or more consecutive examinations. This approach was meant to reduce misclassification and represent a durable change in BP. Consistent with methods used in prior studies of disease onset,5,6,7 we also defined hypertension onset as the first examination at which hypertension criteria was met. For each participant meeting hypertension criteria, we truncated data at the time of hypertension onset. If a person was treated for hypertension at a given examination, we imputed systolic BP to be 10 mm Hg greater as an estimate of the expected BP if antihypertensive therapy were discontinued.8
We categorized participants based on their age at hypertension onset (40-49 years, 50-59 years, 60-69 years, 70-79 years, or no onset), and compared baseline characteristics across these categories using 1-way analysis of variance and χ2 tests. The associations between the predictor variable (age) and the response variable (systolic BP) were nonlinear, with associations demonstrating values at which the association of the predictor with the response changes abruptly (manifesting a change point). Therefore, for each age-based category of hypertension onset, we used an unadjusted segmented mixed model to fit the longitudinal systolic BP data collected to estimate change points in the association between advancing age and progressively increasing systolic BP leading up to hypertension onset.9,10 This method extends from simple segmented regression to permit application within a mixed-model framework; accordingly, the method includes random effects to accommodate longitudinal, repeated-measures data. The segmented mixed regression provides estimates and confidence intervals for the slopes before and after hypertension onset and the change point identified by age. To estimate confidence limits for the corresponding systolic BP for each change point, we performed 1000 bootstraps for each category and reported percentile limits to accommodate for non-parametric data distributions. We used the Cochran Q test to assess between-group heterogeneity in the estimates. We also plotted the systolic BP trajectories using restricted cubic splines.
All statistical analyses were performed using R version 3.3.1 (R Foundation for Statistical Computing). We considered a 2-sided P value of less than .05 statistically significant.
Results
Applying the study inclusion criteria to the 5209 individuals in the Framingham Original Cohort resulted in the exclusion of 3325 individuals who were older than 40 years at baseline, 471 with hypertension at baseline, 91 with fewer than 3 examinations attended before hypertension onset, and 70 who experienced hypertension onset either before age 40 years or at or after age 80 years. The final sample of 1252 individuals contributed 16 072 BP measurements collected once every 2 years.
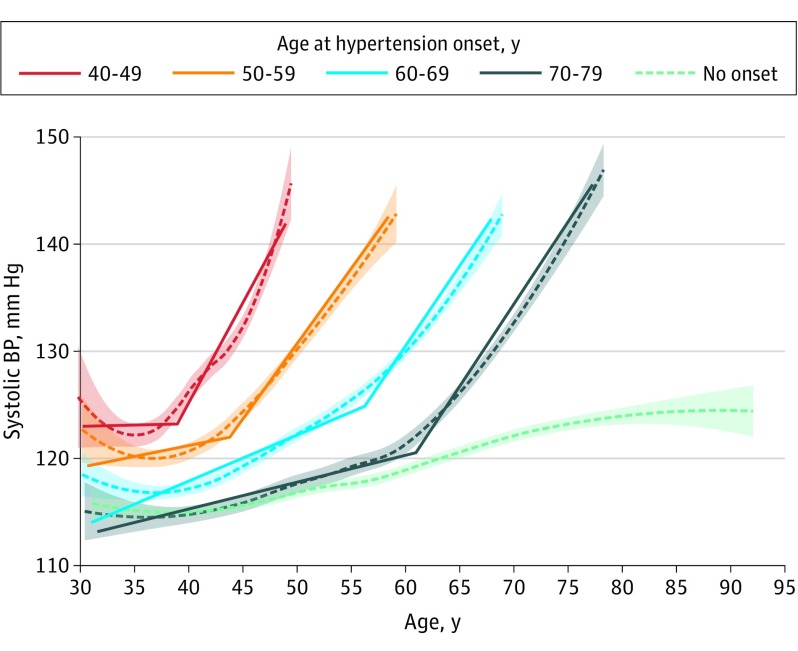
The mean (SD) age of the total sample at baseline was 35.3 (2.7) years; 790 participants (63.1%) were women. Characteristics were similar across individuals categorized by age of hypertension onset (Table). We observed that individuals in each category generally maintained systolic BP measures below 120 to 125 mm Hg, above which systolic BP increased at a relatively rapid rate leading to overt hypertension (Figure 2). Systolic BP began to rise at a more rapid rate after reaching a mean level of 123.2 mm Hg (95% CI, 122.7-130.1 mm Hg) in people with hypertension onset at 40 to 49 years, 122.0 mm Hg (95% CI, 120.3-123.9 mm Hg) in those with onset between 50 and 59 years, 124.9 mm Hg (95% CI, 120.2-127.9 mm Hg) in those with onset between 60 and 69 years, and 120.5 mm Hg (95% CI, 118.0-123.2 mm Hg) in individuals with onset between 70 and 79 years (P = .29 across all comparisons). This trend was consistent whether hypertension manifested earlier or later in life.
Table. Baseline and Change Point Characteristics by Age-Decade of Hypertension Onset.
| Characteristics | Age at Hypertension Onset | P Value | ||||
|---|---|---|---|---|---|---|
| 40-49 Years | 50-59 Years | 60-69 Years | 70-79 Years | No Onset | ||
| Baseline characteristica | ||||||
| No. | 218 | 228 | 240 | 130 | 436 | |
| Age at enrollment, mean (SD), y | 35.2 (2.5) | 35.5 (2.7) | 34.7 (2.6) | 35.4 (2.7) | 35.5 (2.7) | .004 |
| Women, No. (%) | 134 (61.5) | 155 (68.0) | 163 (67.9) | 78 (60.0) | 260 (59.6) | .22 |
| BMI, mean (SD) | 24.4 (3.8) | 23.9 (3.5) | 23.3 (3.2) | 23.6 (3.1) | 23.6 (3.1) | .01 |
| Current smoker, No. (%)b | 142 (67) | 135 (63) | 137 (60) | 77 (63) | 304 (74) | .52 |
| Serum cholesterol (total), mean (SD), mg/dLc | 211 (41) | 207 (37) | 202 (36) | 203 (39) | 205 (37) | .12 |
| Systolic BP, mean (SD), mm Hg | 124 (8) | 122 (8) | 119 (9) | 117 (9) | 118 (10) | <.001 |
| Diastolic BP, mean (SD), mm Hg | 79 (6) | 77 (6) | 76 (7) | 75 (7) | 75 (7) | <.001 |
| Change point characteristic, estimate (95% CI)d | ||||||
| Age at change point, y | 39.0 (37.9 to 40.0) |
43.8 (42.5 to 45.0) |
56.2 (55.0 to 57.5) |
61.0 (59.7 to 62.2) |
NA | <.001 |
| Systolic BP at change point, mm Hg | 123.2 (122.7 to 130.1) |
122.0 (120.3 to 123.9) |
124.9 (120.2 to 127.9) |
120.5 (118.0 to 123.2) |
NA | .29 |
| Slope before change point, mm Hg/y | 0.02 (−0.43 to 0.40) |
0.20 (0.02 to 0.39) |
0.43 (0.36 to 0.48) |
0.25 (0.18 to 0.31) |
NA | <.001 |
| Slope after change point, mm Hg/y | 1.87 (1.62 to 2.09) |
1.41 (1.27 to 1.54) |
1.50 (1.30 to 1.62) |
1.53 (1.30 to 1.62) |
NA | .01 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); BP, blood pressure; NA, not applicable.
SI conversion factor: To convert cholesterol to mmol/L, multiply by 0.0259.
Baseline characteristics between groups were compared using 1-way analysis of variance for continuous variables and χ2 tests for categorical variables.
Data are missing for 71 individuals.
Data are missing for 40 individuals.
Change point estimates were derived using the mixed segmented model. Empirical confidence limits were derived from bootstrapping. Percentile limits are reported to accommodate for potentially non-normal sampling distributions of parameter estimates. We used the Cochran Q test to assess heterogeneity in the change point characteristics.
Figure 2. Observed Blood Pressure Trajectories Preceding Hypertension in the Framingham Heart Study Original Cohort.
Longitudinal analyses, including a piecewise segmented linear model (solid lines), identified systolic blood pressure change points (labeled) for participants across categories of hypertension onset age. Also shown are restricted cubic splines (dashed lines), with 95% confidence intervals derived from associating age with systolic blood pressure, without modeling to identify change points; all splines and regression lines are truncated at the 2.5th and 97.5th percentiles of the age distribution for each hypertension age of onset category.
We observed some between-group heterogeneity in the slopes preceding the change point (age group 40-49 years: estimate [95% CI], 0.02 mm Hg [−0.43 to 0.40 mm Hg]; 50-59 years: 0.20 mm Hg [0.02 to 0.39 mm Hg]; 60-69 years: 0.43 mm Hg [0.36 to 0.48 mm Hg]; 70-79 years: 0.25 mm Hg [0.18 to 0.31 mm Hg]; P < .001) and in the difference in slopes before and after the change point (age group 40-49 years: estimate [95% CI], 1.87 mm Hg [1.62 to 2.09 mm Hg]; 50-59 years: 1.41 mm Hg [1.27 to 1.54 mm Hg]; 60-69 years: 1.50 mm Hg [1.30 to 1.62 mm Hg]; 70-79 years: 1.53 mm Hg [1.30 to 1.62 mm Hg]; P = .01; Table). Segmented regression lines fitting the data are shown in Figure 2.
Discussion
Life-course BP trajectories in the general population are heterogeneous,11 with some individuals developing hypertension earlier or later in life or never at all.7,12 Nonetheless, we observed that among persons who develop hypertension during adulthood, systolic BP trajectories leading up to the onset of hypertension appear similar in pattern but variable in timing. In particular, systolic BP levels are generally stable until they approach approximately 120 to 125 mm Hg, after which systolic BP rises at a relatively rapid rate toward overt hypertension. This transitional systolic BP range was consistent whether hypertension developed in middle age or older age and could represent a critical threshold of extant vascular remodeling.13 Interestingly, this systolic BP range is concordant with recently published guidelines advocating use of the 130 mm Hg value for defining presence of hypertension.14
Limitations
Notwithstanding strengths of the current study, including the availability of frequent standardized BP measurements performed in the same individuals serially throughout decades, certain limitations merit consideration. The mixed segmented model may not perform optimally for extremely noisy data or when the covariate effect is markedly linear or nonlinear, and the model cannot be approximated by a piecewise association.10 As with any statistical modeling, this approach may also lead to some oversimplification of data interpretation. Although the segmented regression lines fit our BP data reasonably well, BP trajectories throughout the entire life course are often highly variable, particularly at the individual level. Further studies are needed to validate and assess the generalizability of our findings, ideally in larger cohorts with serial BP measures performed beginning early in life.
Conclusions
Overall, our findings outline a possible framework for understanding life-course trends in arterial aging, which may have implications for managing BP in practice (Figure 1). In particular, our results suggest that the onset of clinically important BP elevation may be delayed despite aging. However, further investigations are still needed to unravel the sequence of hemodynamic and vascular changes occurring before hypertension onset. In addition, investigation is needed to determine the potential benefit of interventions aimed at preventing the onset of systolic BP rise, even within the normal systolic BP range, as part of efforts to reduce the overall burden of hypertension.
References
- 1.Najjar SS, Scuteri A, Lakatta EG. Arterial aging: is it an immutable cardiovascular risk factor? Hypertension. 2005;46(3):454-462. [DOI] [PubMed] [Google Scholar]
- 2.Stroustrup N, Anthony WE, Nash ZM, et al. . The temporal scaling of Caenorhabditis elegans ageing. Nature. 2016;530(7588):103-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dawber TR, Meadors GF, Moore FE Jr. Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health Nations Health. 1951;41(3):279-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsao CW, Vasan RS. Cohort profile: the Framingham Heart Study (FHS): overview of milestones in cardiovascular epidemiology. Int J Epidemiol. 2015;44(6):1800-1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang NY, Young JH, Meoni LA, Ford DE, Erlinger TP, Klag MJ. Blood pressure change and risk of hypertension associated with parental hypertension: the Johns Hopkins Precursors Study. Arch Intern Med. 2008;168(6):643-648. [DOI] [PubMed] [Google Scholar]
- 6.Niiranen TJ, McCabe EL, Larson MG, et al. . Risk for hypertension crosses generations in the community: a multi-generational cohort study. Eur Heart J. 2017;38(29):2300-2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Niiranen TJ, McCabe EL, Larson MG, et al. . Heritability and risks associated with early onset hypertension: multigenerational, prospective analysis in the Framingham Heart Study. BMJ. 2017;357:j1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tobin MD, Sheehan NA, Scurrah KJ, Burton PR. Adjusting for treatment effects in studies of quantitative traits: antihypertensive therapy and systolic blood pressure. Stat Med. 2005;24(19):2911-2935. [DOI] [PubMed] [Google Scholar]
- 9.Muggeo VMR. Estimating regression models with unknown break-points. Stat Med. 2003;22(19):3055-3071. [DOI] [PubMed] [Google Scholar]
- 10.Muggeo VMR, Atkins DC, Gallop RJ, Dimidjan S. Segmented mixed models with random change points: a maximum likelihood approach with application to treatment for depression study. Stat Model. 2014;14(4):293-313. [Google Scholar]
- 11.Allen NB, Siddique J, Wilkins JT, et al. . Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. JAMA. 2014;311(5):490-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension. 2017;70(4):736-742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.AlGhatrif M, Strait JB, Morrell CH, et al. . Longitudinal trajectories of arterial stiffness and the role of blood pressure: the Baltimore Longitudinal Study of Aging. Hypertension. 2013;62(5):934-941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whelton PK, Carey RM, Aronow WS, et al. . 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2017; pii: HYP.0000000000000066. [Google Scholar]