Key Points
Question
Is individual placement and support–supported employment better than a stepwise vocational rehabilitation program that includes transitional work in helping unemployed veterans with posttraumatic stress disorder become steady workers?
Findings
In this randomized clinical trial of 541 adults with posttraumatic stress disorder, the individual placement and support intervention resulted in 38.7% of participants achieving steady employment compared with 23.3% of participants in the transitional work group—a significant difference. In addition, individual placement and support participants earned significantly more income from competitive jobs compared with transitional work participants.
Meaning
Individual placement and support is more successful than transitional work at helping unemployed veterans with posttraumatic stress disorder obtain and sustain competitive employment.
Abstract
Importance
Posttraumatic stress disorder (PTSD) often interferes with a person’s ability to obtain or sustain employment, which leads to premature exit from the labor force and reduced income.
Objective
To determine whether individual placement and support (IPS)–supported employment is more effective than stepwise vocational rehabilitation involving transitional work assignments at helping veterans with PTSD attain steady, competitive employment.
Design, Setting, and Participants
The Veterans Individual Placement and Support Toward Advancing Recovery (VIP-STAR) study was a prospective, multisite, randomized clinical trial that included 541 unemployed veterans with PTSD at 12 Veterans Affairs medical centers. Data were collected from December 23, 2013, to May 3, 2017. Intent-to-treat analysis was performed.
Interventions
Individual placement and support is a supported employment intervention that rapidly engages people with disabilities in community job development to obtain work based on their individual job preferences. Transitional work is a stepwise vocational rehabilitation intervention that assigns people temporarily to noncompetitive jobs as preparation for competitive employment in the community.
Main Outcomes and Measures
A priori hypotheses were that, compared with those in transitional work, more participants in the IPS group would become steady workers (primary) and earn more income from competitive jobs (secondary) over 18 months. Steady worker was defined as holding a competitive job for at least 50% of the 18-month follow-up period.
Results
A total of 541 participants (n = 271 IPS; n = 270 transitional work) were randomized. Mean (SD) age was 42.2 (11) years; 99 (18.3%) were women, 274 (50.6%) were white, 225 (41.6%) were African American, and 90 (16.6%) were of Hispanic, Spanish, or Latino ethnicity. More participants in the IPS group achieved steady employment than in the transitional work group (105 [38.7%] vs 63 [23.3%]; odds ratio, 2.14; 95% CI, 1.46-3.14). A higher proportion of IPS participants attained any competitive job (186 [68.6%] vs 154 [57.0%]; P = .005) and had higher cumulative earnings from competitive jobs (median [interquartile range] $7290 [$23 174] in IPS vs $1886 [$17 167] in transitional work; P = .004).
Conclusions and Relevance
This multisite trial demonstrated significantly greater effectiveness of IPS-supported employment over stepwise transitional work vocational rehabilitation for veterans living with chronic PTSD. The results provide supporting evidence for increasing access to IPS for veterans living with PTSD.
Trial Registration
clinicaltrials.gov Identifier: NCT01817712
This randomized clinical trial compares individual placement and support with transitional work vs stepwise vocational rehabilitation in helping unemployed veterans with posttraumatic stress disorder attain employment.
Introduction
Posttraumatic stress disorder (PTSD) interferes with a person’s ability to function at work and negatively affects sustained employment and income. Veterans who screen positive for PTSD are more likely to be unemployed than are those without PTSD. The co-occurrence of PTSD, depression, and mild traumatic brain injury is significantly associated with unemployment compared with mild traumatic brain injury alone. Chronic health conditions paired with PTSD significantly increase the odds of early retirement or job loss before age 60 years. A 2015 analysis found that veterans’ labor force participation declined over the previous 35 years in close correlation with growth in service-connected disability. Without effective intervention, the growing numbers of unemployed prime working-aged individuals with disabling PTSD could have a substantial economic impact for generations to come.
Vocational rehabilitation services for veterans with PTSD typically involve stepwise transitional work assignments in Veterans Administration (VA) settings rather than referral to individual placement and support (IPS)–supported employment. Individual placement and support has shown robust effectiveness in people living with serious mental illness and other conditions, including 1 small pilot study in veterans with PTSD. Veterans are significantly more likely to be employed at discharge from VA-supported employment compared with VA transitional work programs. For the past decade, as a consequence of limited resources and lack of results from large effectiveness trials in a PTSD population, the VA has prioritized IPS services for veterans with serious mental illness; as such, veterans with PTSD have limited access to IPS-supported employment.
Given the body of evidence for the effectiveness of IPS in serious mental illness populations, the promising PTSD pilot study results, and the need for improved occupational recovery in veterans with PTSD, a large study to determine the best intervention for unemployed veterans with PTSD was warranted. The objective of this randomized clinical trial was to determine whether IPS is more effective than transitional work at helping unemployed veterans with PTSD attain steady competitive employment.
Methods
Study Design
Veterans Individual Placement and Support Toward Advancing Recovery (VIP-STAR) was a VA Cooperative Studies Program (CSP) multicenter, prospective, randomized clinical trial comparing the effectiveness of IPS vs transitional work in unemployed veterans with a diagnosis of PTSD. The investigators hypothesized that more veterans in the IPS group would become steady workers (primary outcome) and earn more income from competitive jobs (secondary outcome) over the 18-month follow-up compared with the transitional work group. The trial was approved by local site institutional review boards and was monitored by a data monitoring committee (eAppendix in Supplement 1). All participants signed informed consent and privacy authorization and received financial compensation. The full protocol is available in Supplement 2. The methods with baseline characteristics of enrolled participants have been published previously.
Participants
Veterans were recruited between December 23, 2013, and April 24, 2015, from 12 VA medical centers, and data were collected to May 3, 2017. Veterans with a lifetime diagnosis of PTSD according to DSM-IV criteria who were aged 65 years or younger, currently unemployed, interested in seeking competitive employment, eligible for transitional work (based on local programmatic restrictions, such as physical limitations), likely to complete the study (based on participant’s plans to remain in the catchment area for 18 months), and willing to be randomized were included. Veterans with a lifetime diagnosis of schizophrenia, schizoaffective disorder, bipolar I disorder, dementia, severe cognitive disorder, or current suicidal or homicidal ideation were excluded.
Interventions
Participants were randomized to either IPS or transitional work and followed up for 18 months, regardless of their adherence to the intervention; the participant could decline vocational services, transitional work assignments, job interviews, and/or job offers at any time and opt to remain in the study for follow-up assessments. The transitional work professionals were existing employees of the VA medical centers embedded in fully operational vocational teams. The IPS specialists were hired and trained specifically for the study. Most of the IPS specialists had experience with or exposure to evidence-based supported employment serving other populations. On-site and remote IPS training and technical assistance were provided by experienced IPS trainers who guided the IPS service delivery and implementation as an integral part of the local sites’ existing IPS teams.
Individual Placement and Support
Individual placement and support involves job development to rapidly obtain competitive work in the community that aligns with the participant’s preferences, skills, and abilities. Although a member of a larger IPS team within the vocational rehabilitation department, the IPS specialist is colocated within the PTSD or mental health clinic to provide integrated services to an active caseload of 25 veterans. The IPS specialist provides all phases of person-centered employment services that include vocational assessment; individualized job search consistent with the participant’s preferences, skills, and abilities; job coaching and advocacy; care coordination within the treatment team; disability benefits counseling; and open-ended follow-along supports. The IPS model bypasses time-limited, pre-employment, sheltered, transitional work assignments and focuses on rapidly searching and finding competitive employment in the community setting for each participant. The IPS specialists spend most of their time in job development activities that include learning the needs of and developing a personal relationship with potential employers, building employer networks based on participants’ interests, cultivating relationships between veterans and employers, advocating for a person with a disability, matching the veteran’s skills with the demands of a job, and maintaining close follow-up with the veteran and employer after job placement.
Transitional Work
Transitional work is part of a stepwise vocational intervention in the VA that involves vocational assessment followed by a set-aside, pre-employment, brokered, time-limited assignment in a noncompetitive, minimum-wage activity, such as maintenance, housekeeping, or laundry services. The transitional work assignments differ from a competitive job in that there is no job application or competitive selection process, the incumbent does not have ownership of the position, and the work assignment is temporary and has no provision for advancement. The transitional work assignments are prearranged with contracted employers, most often the VA itself, and the veteran is paid a stipend by the transitional work program. The transitional work specialist serves 30 to 40 participants, which is a larger caseload than the IPS specialists. Unlike IPS, transitional work is not integrated or colocated within the PTSD or mental health treatment team. During the transitional work assignment, the vocational rehabilitation specialist provides the participant with some guidance for competitive job searches, but the specialist neither engages in community-based job development activities nor provides long-term follow-up after the first competitive job is obtained or transitional work ends.
Fidelity Monitoring
The study’s IPS fidelity monitor (R.T.) performed a biannual, on-site IPS fidelity review using the Supported Employment Fidelity Scale. This scale is scored from 15 to 75, with higher scores indicating better implementation (score of >66 is good implementation, 56-65 is fair implementation, and <55 indicates not IPS).
At baseline, a research coordinator assessed participants for a lifetime diagnosis of PTSD using the Clinician Administered PTSD Scale for DSM-IV (CAPS-IV) (possible range, 0-136; higher level is worse), current severity of PTSD using the PTSD Checklist for DSM-5 (PCL-5) (very mild, 0-18; mild, 19-37; moderate, 38-59; and severe, 60-80), and concurrent mental disorders using the Mini-International Neuropsychiatric Interview for DSM-IV. Participants were instructed to maintain a study-formatted employment calendar diary and bring this employment diary with copies of paystub and/or tax forms to follow-up visits. The coordinator recorded the following for each week: whether the participant worked for pay (yes/no/unknown), work type (transitional work/competitive/other), job(s) type per Hollingshead job classification, number of days and hours worked, and gross income earned and sources. Hollingshead job classification levels are 1, higher executive, major professional, owner of large business; 2, manager of medium-sized business, lesser professions (ie, nurse, optician, pharmacist, social worker, teacher); 3, administrative personnel, manager, minor professional, owner/proprietor of small business; 4, clerical, sales, technician, small business, bank teller, bookkeeper, clerk, timekeeper, secretary; 5, skilled labor (ie, baker, barber, chef, electrician, fireman, machinist, mechanic, painter, repairman, tailor, welder, police, plumber); 6, semiskilled labor (ie, hospital aide, bartender, bus driver, cutter, cook, garage guard, checker, waiter, spot welder, machine operator); and 7, unskilled labor (ie, attendant, janitor, construction helper, laborer, porter).
In advance of study initiation and based on the consensus of the study planning committee’s desire to have a rigorous threshold of success, the investigators declared the primary outcome as steady worker, defined as holding a competitive job for at least 50% of the weeks during the 18-month follow-up (ie, ≥39 of the 78 weeks). Competitive employment was defined as a nonsheltered job earning salary, wages, or commission, excluding military drill and transient cash-based jobs, such as yard work, babysitting, and manual day labor. The participant did not have to hold the same job during consecutive weeks to be counted toward meeting the threshold of steady worker.
Sample Size
The power analysis was based on the results of a 12-month PTSD study comparing IPS with transitional work. The planned sample size of 540 was projected to provide 90% power to detect a 12.5% absolute difference in the percentage of participants achieving steady worker status between treatment groups (27.5% in the IPS group vs 15% in the transitional work group; odds ratio [OR], 2.15) adjusted for an estimated 13% attrition.
Randomization
The randomization scheme was generated by the VA CSP Coordinating Center with SAS, version 9.3 (SAS Institute Inc) using a permuted block design of randomly varying block sizes and stratified by site. Upon confirming eligibility, the research coordinator logged on to a secure website and retrieved the randomization certificate assigning the participant to IPS or transitional work. The coordinator did not have advance notice of the randomized assignment, but after randomization, the treatment assignment was not concealed.
Missing Data
To adhere to intent-to-treat principles, participants who declined the intervention were encouraged to continue in the study for the outcome assessments. For purposes of primary outcome analysis, missing data for employment status were counted as “not worked.”
Statistical Analysis
The primary steady worker outcome was analyzed using a logistic regression model to calculate an OR adjusted by site. Additional analyses of total time worked (days or weeks) compared the 2 groups using an analysis of variance adjusted for site or the Kruskal-Wallis test if the data were not normally distributed. The cumulative gross income from competitive employment was compared between the 2 groups using a nonparametric test because the income data were not normally distributed. To control for testing of multiple hypotheses, the sequentially rejective procedure of Hochberg was used to determine statistical significance for the treatment comparisons for secondary outcomes using an overall type I error of 5% (2-sided). All statistical analyses were performed with the use of SAS, version 9.3.
Results
Participant Flow
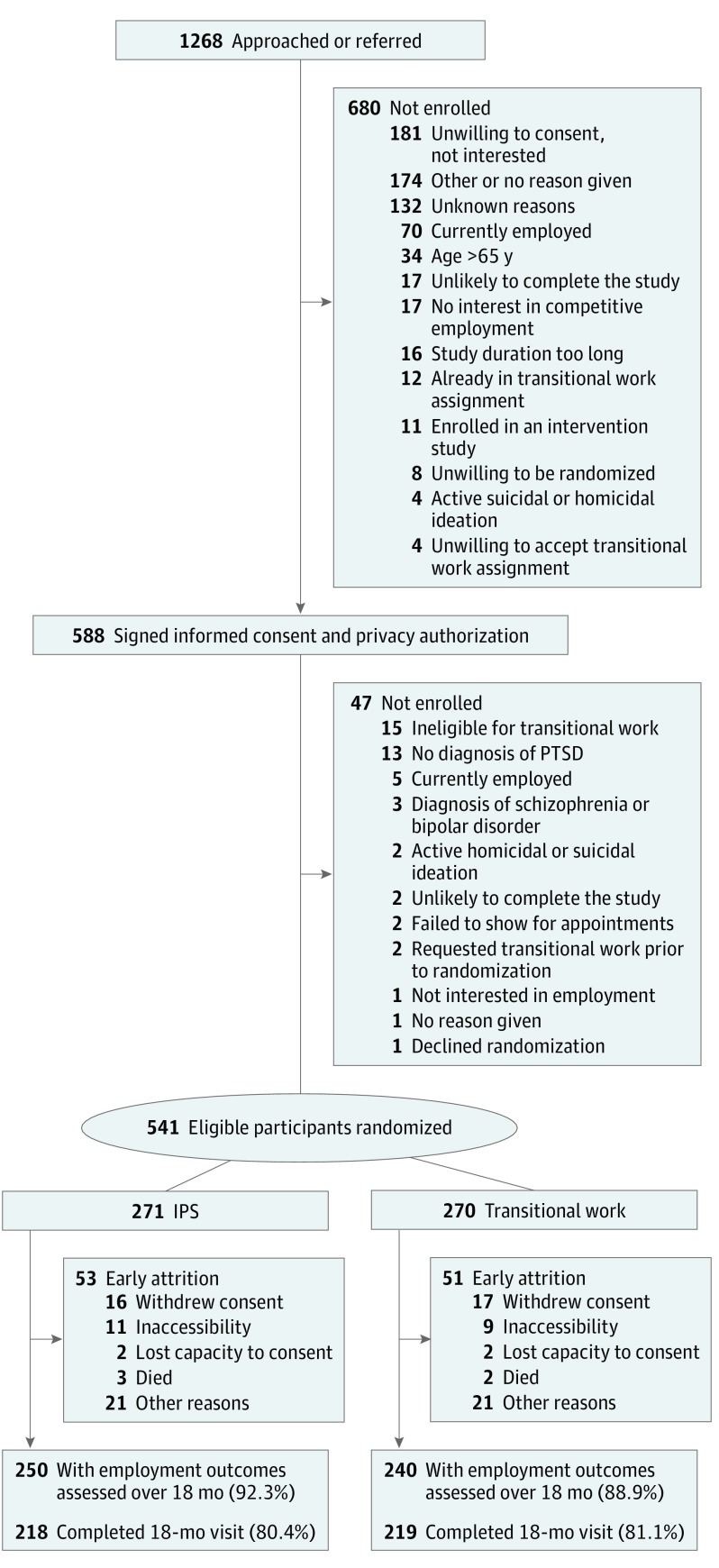
Of the 1268 veterans who were approached or referred, 588 consented to participate, 541 were randomized (IPS, 271; transitional work, 270), 490 (90.6%) had employment outcomes ascertained up to and including their last assessment time, and 437 (80.8%) completed the 18-month study visit (Figure 1). Participants remained in the study for a mean (SD) of 77.2 (17.0) weeks, with no significant difference between groups (IPS, 76.9 [17.7] vs transitional work, 77.4 [16.4] weeks). All 541 randomized participants were included in the analyses regardless of adherence to the intervention.
Figure 1. Veterans Individual Placement and Support Toward Advancing Recovery (VA CSP #589) Flowchart.
IPS indicates individual placement and support; and PTSD, posttraumatic stress disorder.
Study Population
All baseline demographics and characteristics were balanced between groups (Table 1). Participants were unemployed for a median of 1.4 years (mean [SD], 2.8 [3.8]), and 47.0% had not held a job in the preceding 18 months. Mean (SD) age was 42.2 (11) years; 99 (18.3%) were women; 274 (50.6%) were white, 225 (41.6%) were African American, and 90 (16.6%) were of Hispanic, Spanish, or Latino ethnicity. Half (50.8%) were receiving VA service-connected disability income, and 246 (45.5%) were receiving disability income specifically for PTSD. For those receiving VA disability income, the mean total percentage of the disability rating was 55.6% (31.8%), with PTSD representing the highest percentage category.
Table 1. Demographics, Clinical Characteristics, and Adverse Eventsa.
| Characteristic | IPS (n = 271) | Transitional Work (n = 270) |
|---|---|---|
| Baseline Demographics and Clinical Characteristics | ||
| Age, mean (SD), y | 42.5 (10.7) | 41.9 (11.2) |
| Male, No. (%) | 224 (82.7) | 218 (80.7) |
| Female, No. (%) | 47 (17.3) | 52 (19.3) |
| Race/ethnicity, No. (%)b | ||
| White | 138 (50.9) | 136 (50.4) |
| African American | 115 (42.4) | 110 (40.7) |
| All other, No. (%) | 32 (11.8) | 36 (13.3) |
| Hispanic, Spanish, or Latino, No. (%) | 43 (15.9) | 47 (17.4) |
| Never married, No. (%) | 68 (25.1) | 67 (24.8) |
| Married, No. (%) | 89 (32.8) | 84 (31.1) |
| Divorced, No. (%) | 82 (30.3) | 79 (29.3) |
| Educational level, No. (%) | ||
| Less than college | 54 (19.9) | 43 (15.9) |
| College credit/degree | 201 (74.2) | 210 (77.8) |
| Graduate credit/degree | 16 (5.9) | 17 (6.3) |
| Length of current unemployment, mean (SD), y | 2.7 (3.5) | 2.9 (4.1) |
| Length of current unemployment, median (IQR), wk | 73.7 (164.7) | 78.0 (156.0) |
| Duration of longest job in lifetime, mean (SD), y | 8.3 (5.8) | 8.7 (6.4) |
| Current major depressive episode, No. (%) | 87 (32.1) | 83 (30.7) |
| Past major depressive episode, No. (%) | 183 (67.5) | 173 (64.1) |
| Current agoraphobia, No. (%) | 64 (23.6) | 59 (21.9) |
| Current panic disorder, No. (%) | 37 (13.7) | 33 (12.2) |
| Social anxiety disorder (generalized), No. (%) | 35 (12.9) | 28 (10.4) |
| Alcohol use disorder, past 12 mo, No. (%) | 54 (19.9) | 78 (28.9) |
| Non-alcohol use disorder, past 12 mo, No. (%) | 47 (17.3) | 40 (14.8) |
| Duration of PTSD, mean (SD), y | 13.3 (11.6) | 13.4 (11.3) |
| Total CAPS-IV lifetime, mean (SD)c | 84.1 (18.9) | 84.8 (18.3) |
| PCL-5, mean (SD)d | 46.2 (15.8) | 45.1 (17.0) |
| PCL-5 positive for current PTSD (≥33), No. (%) | 209 (77.1) | 204 (75.6) |
| PCL-5 very mild (0-18), No. (%) | 14 (5.2) | 20 (7.4) |
| PCL-5 mild (19-37), No. (%) | 64 (23.6) | 60 (22.2) |
| PCL-5 moderate (38-59), No. (%) | 128 (47.2) | 138 (51.1) |
| PCL-5 severe (60-80), No. (%) | 63 (23.2) | 49 (18.1) |
| Serious or Reportable AEs, No. (%) | ||
| Participants with SAEs | 63 (23.2) | 64 (23.7) |
| No. of SAEs | 129 | 94 |
| Participants with AEs | 36 (13.3) | 40 (14.8) |
| No. of reportable AEs | 52 | 51 |
| AEs attributed to PTSD (yes/possibly), No. (% of events) | 50 (38.8) | 28 (29.8) |
| AEs possibly attributed to occupation (yes/possibly), No. (% of events) | 5 (3.9) | 3 (3.2) |
| AEs attributed to study intervention, No. (% of events) | 3 (2.3) | 2 (2.1) |
| Discontinuation from study due to SAE, No. (% of events) | 3 (2.3) | 4 (4.3) |
| Deaths, No. (% of participants) | 3 (1.1) | 2 (0.7) |
Abbreviations: AE, adverse event; CAPS-IV, Clinician Administered Posttraumatic Stress Disorder (PTSD) Scale for DSM-IV for lifetime; IPS, individual placement and support; IQR, interquartile range; PCL-5, PTSD Checklist for DSM-5 for the previous month; PTSD, posttraumatic stress disorder; SAE, serious AE.
Denominators vary for some factors due to missing data.
Participants were permitted to indicate more than 1 race.
Possible range, 0 to 136 (higher score is worse).
Very mild, 0 to 18; mild, 19 to 37; moderate, 38 to 59; and severe, 60 to 80.
Participants served in the Army (329 [60.8%]), Navy (99 [18.3%]), Marine Corps (84 [15.5%]), Air Force (47 [8.7%]), or Coast Guard or National Guard (39 [7.2%]) for 8.3 (6.5) years; 324 (59.9%) served in Iraq and/or Afghanistan; and 389 (71.9%) served in a combat zone. Participants’ primary trauma resulting in PTSD was identified as nonsexual combat-related (319 [59.0%]), military sexual (93 [17.2%]), or other military-related (71 [13.1%]) events. Table 1 reports the mean length and severity of PTSD; 413 (76.3%) of the participants scored above the PCL-5 threshold (≥33) for current PTSD diagnosis at baseline.
Steady Employment: Primary Outcome
Compared with the transitional work group, significantly more participants in the IPS group achieved steady worker status (OR, 2.14; 95% CI, 1.46-3.14; P < .001) over the 18-month follow-up (Table 2). Specifically, 105 (38.7%) of IPS participants compared with 63 (23.3%) of the transitional work group became steady workers.
Table 2. Outcomes During 18-Month Follow-up.
| Outcome | IPS (n = 271) | Transitional Work (n = 270) | P Value |
|---|---|---|---|
| Primary outcome | |||
| Steady worker (held competitive job ≥39 of 78 wk), No. (%)a | 105 (38.7) | 63 (23.3) | <.001a |
| Secondary outcome | |||
| Income from competitive sources for all participants, $ | .004 | ||
| Mean (SD) | 14 642 (19 308) | 10 989 (17 097) | |
| Median (IQR) | 7290 (23 174) | 1886 (17 167) | |
| Other employment outcome | |||
| Obtained a competitive job within 18 mo, No. (%) | 186 (68.6) | 154 (57.0) | .005 |
| Obtained a competitive job within 12 mo, No. (%) | 179 (66.1) | 127 (47.0) | <.001 |
| Obtained a competitive job within 6 mo, No. (%) | 145 (53.5) | 86 (31.9) | <.001 |
| Weeks employed in competitive jobs, mean (SD) | 17.5 (17.7) | 12.1 (15.5) | <.001 |
| Proportion of weeks unencumbered by transitional work assignment in which competitive jobs were held | .006 | ||
| Mean (SD) | 0.4 (0.3) | 0.3 (0.3) | |
| Median (IQR) | 0.3 (0.7) | 0.1 (0.6) | |
| Days employed in competitive jobs, mean (SD) | 122.3 (124.2) | 84.9 (108.1) | <.001 |
| Held full-time (≥30 h/wk) competitive job, No. (%) | 161 (59.4) | 128 (47.4) | .01 |
| Weeks employed in full-time competitive job, mean (SD) | 14 (17.0) | 10.4 (14.9) | .01 |
| Time to first competitive job, mean (SD), wk | 18.4 (15.1) | 28.2 (20.0) | <.001 |
| Competitive jobs/person employed | <.001 | ||
| Mean (SD) | 40.6 (22.8) | 32.5 (21.6) | |
| Median (IQR) | 44 (40) | 30 (34) | |
| Hollingshead job classification, No. (%) competitively employedb | |||
| 1, 2, and 3 | 37 (19.9) | 29 (18.7) | .30 |
| 4 and 5 | 84 (45.2) | 77 (49.7) | .53 |
| 6 | 102 (54.8) | 57 (36.8) | <.001 |
| 7 | 53 (28.5) | 48 (31.0) | .60 |
| Income from competitive job(s) in steady workers, mean (SD), $ | 12 603 (10 126) | 8461 (17 569) | .01 |
| Income from all sources including transitional work and excluding disability income, mean (SD), $ | 15 354 (19 661) | 14 467 (17 497) | .50 |
| Employment outcomes from transitional work assignments | |||
| Worked in a transitional work assignment, No. (%) | 11 (4.1)c | 142 (52.6) | <.001 |
| Weeks in transitional work assignment, mean (SD) | 0.2 (1.7) | 6.9 (9.8) | <.001 |
| Income from transitional work sources for participants who held a transitional work assignment, $ | <.001 | ||
| Mean (SD) | 205 (1506) | 2986 (4715) | |
| Median (IQR) | 0 | 177 (4903) | |
| PTSD outcome, (95% CI) | |||
| PCL-5, LS mean estimate, 95%CId | −3.66 (−6.09 to 1.23) | −0.82 (−3.24 to 1.59) | .07 |
Abbreviations: IPS, individual placement and support; IQR, interquartile range; LS, least squares; PCL-5, PTSD Checklist for DSM-5 for the previous month; PTSD, posttraumatic stress disorder.
Odds ratio, 2.14 (95% CI, 1.46-3.14).
Hollingshead job classification: 1, higher executive, major professional, owner of large business; 2, manager of medium-sized business, lesser professions (ie, nurse, optician, pharmacist, social worker, teacher); 3, administrative personnel, manager, minor professional, owner/proprietor of small business; 4, clerical, sales, technician, small business, bank teller, bookkeeper, clerk, timekeeper, secretary; 5, skilled labor (ie, baker, barber, chef, electrician, fireman, machinist, mechanic, painter, repairman, tailor, welder, police, plumber); 6, semiskilled labor (ie, hospital aide, bartender, bus driver, cutter, cook, garage guard, checker, waiter, spot welder, machine operator); 7, unskilled labor (ie, attendant, janitor, construction helper, laborer, porter).
After randomization, on their own volition, 11 IPS participants crossed over to transitional work during the follow-up period.
Posttraumatic Stress Disorder Checklist for DSM-5 (decrease in scores translates to improvement); longitudinal analysis least squares mean difference, −1.9; 95% CI, −3.91 to 0.12; P = .07.
Income Earned: Secondary Outcome
The IPS group had significantly higher earnings from competitive jobs than the transitional work group (Table 2). Group differences in earned income from all sources other than disability income were nonsignificant.
Other Employment Outcomes
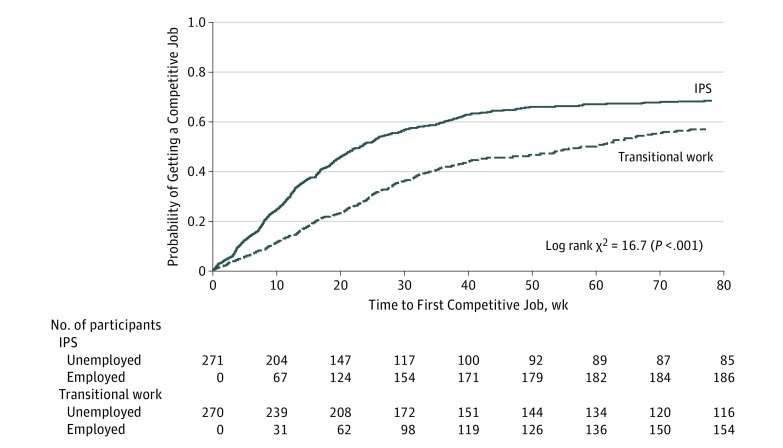
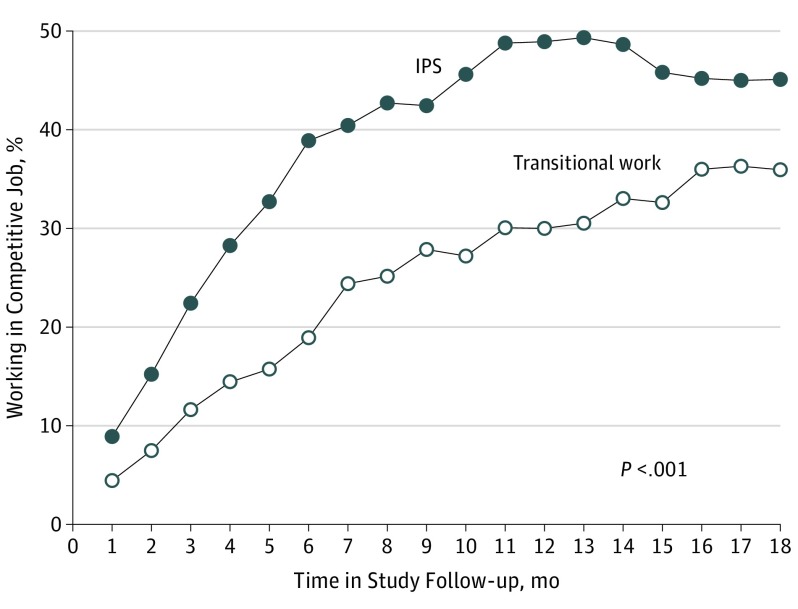
The IPS participants gained competitive employment more rapidly than transitional work participants (Table 2; Figure 2). Compared with those in the transitional work group, IPS participants were significantly more likely to obtain a competitive job, to be working competitively during any month of the study (Figure 3), to obtain full-time (≥30 h/wk) competitive employment, to work more weeks and more days, and to work more weeks in full-time competitive employment.
Figure 2. Time to First Competitive Job in Veterans With Posttraumatic Stress Disorder Randomized to Individual Placement and Support (IPS) vs Transitional Work.
Participants randomized to IPS gain a competitive job more quickly than those randomized to transitional work.
Figure 3. Percentage of Participants Holding a Competitive Job Over 18 Months Comparing Individual Placement and Support (IPS) With Transitional Work.
Participants randomized to IPS are more likely to be competitively employed at any time during the 18-month follow-up compared with those randomized to transitional work.
Consistent with the randomization, transitional work participants (52.6%) were more likely than IPS participants (4.1%) to work in a transitional work assignment (P < .001). Of those randomized to transitional work, 52.6% of participants began a transitional work assignment, with a mean wait of 9.7 (10.3) (median [interquartile range], 6.5 [10]) weeks before transitional work initiation. The transitional work assignments lasted a mean of 21 (15.2) (median [interquartile range], 21 [20]) weeks. To control for transitional work assignments, the proportion of weeks unencumbered by transitional work assignment in which participants held a competitive job was calculated. The IPS participants worked proportionally more unencumbered weeks in a competitive job (40% [30%]) than those randomized to transitional work (30% [30%]; P = .006).
Per Hollingshead job classification, the number of participants and competitive jobs in each category was similar between groups, except for significantly more IPS participants working in semiskilled jobs (code 6).
Fidelity
The mean Supported Employment Fidelity Scale score was 55 within the first 3 months and subsequently ranged between 63 and 69. Most sites maintained good or higher implementation. Two sites had difficulties with IPS implementation; however, corrective actions yielded improvement attaining fair to good implementation. The transitional work services were rated as not IPS (ie, mean, 26-32 [range, 18-41]) on the Supported Employment Fidelity Scale, indicating that transitional work did not drift toward IPS.
Adverse Events
In addition to tracking all serious adverse events, the investigators tracked adverse events that could be possibly attributed to symptoms of PTSD, occupation, or study intervention. There were no significant between-group differences on reported serious or nonserious adverse events (Table 1).
Discussion
Participants randomized to IPS were significantly more likely than those in the transitional work group to achieve steady employment and earn more income from competitive jobs during the 18-month follow-up. Of veterans with a diagnosis of PTSD randomized to IPS, 38.7% became steady workers compared with 23.3% of those randomized to transitional work. Compared with transitional work, the IPS intervention resulted in significantly earlier competitive job acquisition and longer job tenure. Significantly more IPS participants obtained a competitive job and held full-time employment compared with transitional work participants. The types of jobs were broadly distributed across classification domains, with higher proportions in the IPS group working in semiskilled jobs than in the transitional work group. The PTSD symptoms improved over the 18-month study period without significant group differences, with the main point being that PTSD symptoms did not worsen for either group.
The outcomes in this study are consistent with previous studies. A meta-analysis of 21 randomized clinical trials found that the pooled mean risk ratio comparing the probability of competitive employment in IPS arms with alternative vocational services was 2.31 (95% CI, 1.99-2.69). Compared with the 12-month PTSD pilot study in which 76% IPS and 28% transitional work participants gained competitive employment; this sample showed slightly lower rates of employment in the IPS group (67%) and much higher rates of employment in the transitional work group (57%). The differences are likely due to the incremental success for the transitional work group during the additional 6 months of follow-up in the VIP-STAR study reported herein. Our results exceeded the naturalistic outcomes of veterans with mixed diagnoses reported by the VA that found that 35% in supported employment and 30% in VA-based transitional work were competitively employed at discharge (S.G. Resnick; October 30, 2017). Per internal VA reports of those enrolled in transitional work, the mean length of transitional work assignment was 19 weeks, and 34% were competitively employed at discharge in fiscal year 2016. These differences may be attributable to procedures in VA reporting of point-in-time outcomes, in which veterans are classified as employed or unemployed at the time of transitional work or IPS program discharge, which fails to capture the longitudinal accomplishments of either service. Our results for the transitional work group align with those reported in a small study comparing VA transitional work with state vocational rehabilitation, in which 60% of participants with mixed diagnoses in transitional work obtained a competitive job and earned a mean (SD) of $6803 ($9931) during the 12-month follow-up.
Strengths of the study include its multisite randomized trial design with adequate power to test the hypotheses, salience of determining optimized vocational rehabilitation for veterans with PTSD, IPS fidelity monitoring, inclusion of both dichotomous and continuous work outcomes, and high participant retention. We intentionally used broad eligibility criteria to match real-world clinical settings: veterans at varied levels of PTSD severity and/or active substance use were included.
A nuance of the study was that IPS service implementation was not a mature program when randomization began. Although most IPS specialists were experienced with some type of vocational rehabilitation delivery, all IPS specialists received training on high-fidelity IPS practices at the study initiation. Both IPS and transitional work programs had some turnover in staff at several sites during the study, which adds to the real-world circumstances of the research setting.
Limitations
Our study is limited by its confined generalizability to mostly male veterans. However, compared with the demographics of the veteran population, more women and minorities were represented in this sample. We used the CAPS-IV to confirm lifetime diagnosis of PTSD and the self-report PCL-5 to assess baseline current severity of PTSD. Employment outcomes were not collected by a blinded assessor; however, if the research coordinator had any doubt verifying the type of employment, an adjudication process was invoked that provided an independent evaluation by a blinded assessor. The 18-month duration may not have been long enough to evaluate the full effect of steady employment. A recent report of a 5-year follow-up among people with serious mental illness found that the effectiveness of IPS to reduce days of hospitalization and improve quality-of-life measures was mediated by IPS’ effects on increasing sustained competitive employment. We are planning analyses of nonvocational, health utilization, and cost-efficacy outcomes. Another limitation is that we did not systematically assess the participants’ job satisfaction, although a qualitative exit survey about their satisfaction with the intervention is under analysis.
Conclusions
This study provides evidence for the effectiveness of IPS for veterans living with PTSD. Recovery from PTSD requires a multifaceted treatment approach of which employment should be a central consideration. Individual placement and support can play an important role in an integrated treatment plan. Our results indicate that pre-employment transitional work delays competitive job acquisition without benefit of better rates of sustained competitive employment achieved by IPS. Based on these results, the VA should provide greater access to IPS for veterans with PTSD.
eAppendix. Institutional Review Boards
Protocol
References
- 1.Erbes CR, Kaler ME, Schult T, Polusny MA, Arbisi PA. Mental health diagnosis and occupational functioning in National Guard/Reserve veterans returning from Iraq. J Rehabil Res Dev. 2011;48(10):1159-1170. [DOI] [PubMed] [Google Scholar]
- 2.Adler DA, Possemato K, Mavandadi S, et al. . Psychiatric status and work performance of veterans of Operations Enduring Freedom and Iraqi Freedom. Psychiatr Serv. 2011;62(1):39-46. [DOI] [PubMed] [Google Scholar]
- 3.Amick MM, Meterko M, Fortier CB, Fonda JR, Milberg WP, McGlinchey RE. The deployment trauma phenotype and employment status in veterans of the wars in Iraq and Afghanistan [published online April 18, 2017]. J Head Trauma Rehabil. doi:10.1097/HTR.0000000000000308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pabayo R, Fuller D, Goldstein RB, Kawachi I, Gilman SE. Income inequality among American states and the conditional risk of post-traumatic stress disorder. Soc Psychiatry Psychiatr Epidemiol. 2017;52(9):1195-1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sripada RK, Henry J, Yosef M, et al. . Occupational functioning and employment services use among VA primary care patients with posttraumatic stress disorder [published online December 12, 2016]. Psychol Trauma. doi: 10.1037/tra0000241 [DOI] [PubMed] [Google Scholar]
- 6.Yu S, Brackbill RM, Locke S, Stellman SD, Gargano LM. Impact of 9/11-related chronic conditions and PTSD comorbidity on early retirement and job loss among World Trade Center disaster rescue and recovery workers. Am J Ind Med. 2016;59(9):731-741. [DOI] [PubMed] [Google Scholar]
- 7.Coile C, Duggan M, Guo A. Veterans’ labor force participation: what role does the VA’s disability compensation program play? Am Econ Rev. 2015;105(5):131-136. [DOI] [PubMed] [Google Scholar]
- 8.Twamley EW, Baker DG, Norman SB, Pittman JO, Lohr JB, Resnick SG. Veterans Health Administration vocational services for Operation Iraqi Freedom/Operation Enduring Freedom veterans with mental health conditions. J Rehabil Res Dev. 2013;50(5):663-670. [DOI] [PubMed] [Google Scholar]
- 9.Drake RE, Frey W, Bond GR, et al. . Assisting Social Security Disability Insurance beneficiaries with schizophrenia, bipolar disorder, or major depression in returning to work. Am J Psychiatry. 2013;170(12):1433-1441. [DOI] [PubMed] [Google Scholar]
- 10.Drake RE, McHugo GJ, Bebout RR, et al. . A randomized clinical trial of supported employment for inner-city patients with severe mental disorders. Arch Gen Psychiatry. 1999;56(7):627-633. [DOI] [PubMed] [Google Scholar]
- 11.Lehman AF, Goldberg R, Dixon LB, et al. . Improving employment outcomes for persons with severe mental illnesses. Arch Gen Psychiatry. 2002;59(2):165-172. [DOI] [PubMed] [Google Scholar]
- 12.Cook JA, Leff HS, Blyler CR, et al. . Results of a multisite randomized trial of supported employment interventions for individuals with severe mental illness. Arch Gen Psychiatry. 2005;62(5):505-512. [DOI] [PubMed] [Google Scholar]
- 13.Mueser KT, Drake RE, Bond GR. Recent advances in supported employment for people with serious mental illness. Curr Opin Psychiatry. 2016;29(3):196-201. [DOI] [PubMed] [Google Scholar]
- 14.Salyers MP, Becker DR, Drake RE, Torrey WC, Wyzik PF. A ten-year follow-up of a supported employment program. Psychiatr Serv. 2004;55(3):302-308. [DOI] [PubMed] [Google Scholar]
- 15.Davis LL, Leon AC, Toscano R, et al. . A randomized controlled trial of supported employment among veterans with posttraumatic stress disorder. Psychiatr Serv. 2012;63(5):464-470. [DOI] [PubMed] [Google Scholar]
- 16.Abraham KM, Yosef M, Resnick SG, Zivin K. Competitive employment outcomes among veterans in VHA therapeutic and supported employment services programs. Psychiatr Serv. 2017;68(9):938-946. [DOI] [PubMed] [Google Scholar]
- 17.Abraham KM, Ganoczy D, Yosef M, Resnick SG, Zivin K. Receipt of employment services among Veterans Health Administration users with psychiatric diagnoses. J Rehabil Res Dev. 2014;51(3):401-414. [DOI] [PubMed] [Google Scholar]
- 18.Davis LL, Kyriakides TC, Suris A, et al. . Veterans Individual Placement and Support Towards Advancing Recovery: methods and baseline clinical characteristics of a multisite study [published online March 30, 2017]. Psychiatr Rehabil J. doi: 10.1037/prj0000250 [DOI] [PubMed] [Google Scholar]
- 19.Bond GR, Becker DR, Drake RE, et al. . A fidelity scale for the individual placement and support model of supported employment. Rehabil Couns Bull. 1997;40:265-284. [Google Scholar]
- 20.Blake DD, Weathers FW, Nagy LM, et al. . The development of a clinician-administered PTSD scale. J Trauma Stress. 1995;8(1):75-90. [DOI] [PubMed] [Google Scholar]
- 21.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489-498. [DOI] [PubMed] [Google Scholar]
- 22.Sheehan DV, Lecrubier Y, Sheehan KH, et al. . The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(S20)(suppl 20):22-33. [PubMed] [Google Scholar]
- 23.Hollingshead AB. Four factor index of social status. Yale J Sociol. 2011;8:21-52. [Google Scholar]
- 24.Metcalfe JD, Drake RE, Bond GR. Economic, labor, and regulatory moderators of the effect of individual placement and support among people with severe mental illness: a systematic review and meta-analysis [published online September 28, 2017]. Schizophr Bull. doi: 10.1093/schbul/sbx132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Resnick SG, Kaczynski R, Sieffert D, Porter E, Hoff RA. Northeast Program Evaluation Center Fiscal Year 2016 Annual Report for the Therapeutic and Supported Employment Program. West Haven, CT: Veterans Administration; 2017. [Google Scholar]
- 26.Penk W, Drebing CE, Rosenheck RA, Krebs C, Van Ormer A, Mueller L. Veterans Health Administration transitional work experience vs. job placement in veterans with co-morbid substance use and non-psychotic psychiatric disorders. Psychiatr Rehabil J. 2010;33(4):297-307. [DOI] [PubMed] [Google Scholar]
- 27.Jäckel D, Kupper Z, Glauser S, Mueser KT, Hoffmann H. Effects of sustained competitive employment on psychiatric hospitalizations and quality of life. Psychiatr Serv. 2017;68(6):603-609. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Institutional Review Boards
Protocol