Abstract
Importance
Increasing value requires improving quality or decreasing costs. In surgery, estimates for the cost of 1 minute of operating room (OR) time vary widely. No benchmark exists for the cost of OR time, nor has there been a comprehensive assessment of what contributes to OR cost.
Objectives
To calculate the cost of 1 minute of OR time, assess cost by setting and facility characteristics, and ascertain the proportion of costs that are direct and indirect.
Design, Setting, and Participants
This cross-sectional and longitudinal analysis examined annual financial disclosure documents from all comparable short-term general and specialty care hospitals in California from fiscal year (FY) 2005 to FY2014 (N = 3044; FY2014, n = 302). The analysis focused on 2 revenue centers: (1) surgery and recovery and (2) ambulatory surgery.
Main Outcomes and Measures
Mean cost of 1 minute of OR time, stratified by setting (inpatient vs ambulatory), teaching status, and hospital ownership. The proportion of cost attributable to indirect and direct expenses was identified; direct expenses were further divided into salary, benefits, supplies, and other direct expenses.
Results
In FY2014, a total of 175 of 302 facilities (57.9%) were not for profit, 78 (25.8%) were for profit, and 49 (16.2%) were government owned. Thirty facilities (9.9%) were teaching hospitals. The mean (SD) cost for 1 minute of OR time across California hospitals was $37.45 ($16.04) in the inpatient setting and $36.14 ($19.53) in the ambulatory setting (P = .65). There were no differences in mean expenditures when stratifying by ownership or teaching status except that teaching hospitals had lower mean (SD) expenditures than nonteaching hospitals in the inpatient setting ($29.88 [$9.06] vs $38.29 [$16.43]; P = .006). Direct expenses accounted for 54.6% of total expenses ($20.40 of $37.37) in the inpatient setting and 59.1% of total expenses ($20.90 of $35.39) in the ambulatory setting. Wages and benefits accounted for approximately two-thirds of direct expenses (inpatient, $14.00 of $20.40; ambulatory, $14.35 of $20.90), with nonbillable supplies accounting for less than 10% of total expenses (inpatient, $2.55 of $37.37; ambulatory, $3.33 of $35.39). From FY2005 to FY2014, expenses in the OR have increased faster than the consumer price index and medical consumer price index. Teaching hospitals had slower growth in costs than nonteaching hospitals. Over time, the proportion of expenses dedicated to indirect costs has increased, while the proportion attributable to salary and supplies has decreased.
Conclusions and Relevance
The mean cost of OR time is $36 to $37 per minute, using financial data from California’s short-term general and specialty hospitals in FY2014. These statewide data provide a generalizable benchmark for the value of OR time. Furthermore, understanding the composition of costs will allow those interested in value improvement to identify high-yield targets.
This cross-sectional analysis of annual financial disclosure documents calculates the cost of 1 minute of operating room time, assesses cost by setting and facility characteristics, and ascertains the proportion of costs that are direct and indirect.
Key Points
Questions
What is the cost of 1 minute of operating room time, and what contributes to this cost?
Findings
In this cross-sectional analysis, the mean cost of operating room time in fiscal year 2014 for California’s acute care hospitals was $36 to $37 per minute; $20 to $21 of this amount is direct cost, with $13 to $14 attributable to wages and benefits and $2.50 to $3.50 attributable to surgical supplies.
Meaning
These numbers are the first standardized estimates of operating room cost; understanding the composition of costs will allow those interested in value improvement to identify high-yield targets.
Introduction
Understanding hospital costs is critical to value-based care. Hospitals charge insurers and patients at a markup, expecting a reimbursement (revenue) that is greater than their actual costs to generate a profit. Whereas in traditional fee-for-service models, more services equate to more revenue, new models, such as bundled payments, will reimburse hospitals a set amount for the surgical episode. These capitated models focus on cost control, shifting the burden of cost minimization away from insurers and onto clinicians and administrators.
There is a growing body of literature describing cost-saving interventions in surgery; however, estimates of savings vary widely, and while myriad reasons may explain this variation, such as implementation differences, hospital setting, and patient mix, these analyses are often not comparable because of variations in the type of cost data and accounting practices used. An exemplar of this variation is operating room (OR) cost, with reported values ranging widely, from $7 to more than $100 per minute, even within a surgical field or procedure. In 2010, an editorial found no standardized estimates were available and that most existing sources report hospital charges, which are confounded by contractual allowances and profit margins, and are of little use when assessing cost-saving interventions.
Given that surgical care accounts for nearly one-third of all US health care spending, and the OR is the second most expensive part of surgical care, having a data-driven benchmark for OR cost and defining what contributes to this cost is essential. California law requires hospitals to report financial metrics to the Office of Statewide Health Planning and Development (OSHPD). This study uses these statements to calculate the mean cost of 1 minute of OR time, assess variation between hospitals, understand what contributes to cost, and evaluate how cost has changed over time.
Methods
Data Set
The data set includes 10 years (2005-2014) of California Hospital Annual Disclosure Reports (HADR) released by the OSHPD. California hospitals are required to use the OSHPD’s accounting system and to report disclosures in a comparable format. Duplicate reports occur when facilities change ownership, licensure, or the dates of their fiscal year (FY). To prevent double counting, only the longest report for a given facility was included each year. Hospitals set their own FY; for example, in FY2014, most hospitals began on either July 1, 2013, or January 1, 2014. This analysis pools these into a single fiscal year identified as FY2014. Hospitals were linked over time using the OSHPD facility number, a unique identifier based on location. The data for this study are publicly available and do not meet the definition of human participants research. As such, institutional review board review was not indicated, which we confirmed with the institutional review board of the University of California, Los Angeles, prior to starting our project.
Included Hospitals
Several hospitals in California are not required to submit all HADR pages because of a waiver granted by the OSHPD, and are excluded from this analysis. In FY2014, these hospitals included all 34 Kaiser facilities, 4 long-term care facilities, 24 psychiatric health facilities, 2 Shriner’s hospitals, and 9 state hospitals. In FY2014 additional excluded hospitals were 27 short-term psychiatric facilities, 26 long-term care facilities, and 15 facilities that did not report surgical expenditures (3 short-term general hospitals and 12 short-term specialty hospitals) (eTable 1 in the Supplement). The final database included 3044 financial statements from FY2005 to FY2014; 302 were from FY2014.
Calculating the Cost per Minute of OR Time
Descriptions of select financial terminology are included in eTable 2 in the Supplement. This study focuses on the perspective of the hospital (ie, the cost to the hospital of delivering the service). However, many financial perspectives exist including that of the patient (ie, out-of-pocket costs) or the payer (eg, the amount Medicare reimburses a hospital), as well as the societal perspective, which would include both patient and payer costs along with the opportunity cost of patient and caregiver time, transportation costs, and effects on future productivity.
Each HADR is organized in a series of sequentially more granular details (eFigure in the Supplement). The income statement lists total expenses for a year. As a contrived example, total expenses may be $1 billion. Expenses are divided into smaller bins, culminating with individual revenue centers. This study focuses on 2 revenue centers: (1) surgery and recovery and (2) ambulatory surgery. To extend our example, the former may have expenses of $10 million and the latter may have expenses of $5 million. As defined by the OSHPD, the surgery and recovery center includes all costs associated with “the performance of surgical and related procedures during and immediately following surgery”(p2420.3[Cont.1]) and the ambulatory surgery center includes costs associated with a “separately identifiable outpatient surgery room.”(p2420.3[Cont.3]) These costs include intraoperative costs (eg, salaries and supplies), the cost of services to maintain the OR (eg, environmental services and cleaning and repair of instruments), and the cost of the recovery room. Immediate preoperative expenses are not detailed by the OSHPD, but they are likely included. Operating rooms used for both inpatient and outpatient operations are classified under surgery and recovery.
To compare costs across facilities, each revenue center has a unit or denominator. For surgical revenue centers, the unit is minutes of operating time, which is the sum of OR time for the year. Time is measured from the beginning to end of anesthesia or, when no anesthesia is provided, the start and stop of surgery. Hospitals report these units for each revenue center (continuing our example, 200 000 minutes for each). To calculate the cost per minute, the facility divides expenses in that revenue center (ie, $10 million and $5 million) by the number of minutes (ie, 200 000) to produce a cost per minute (ie, $50 per minute or $25 per minute). Each facility reports expenses, the number of minutes, and the cost per minute in their HADR.
For each revenue center, costs are further divided into direct (costs attributable to the revenue center, such as staff salaries or supplies [eTable 2 in the Supplement]), and indirect costs (costs allocated from nonrevenue centers, such as security, that are required for patient care but cannot be attributed to a single department [eTable 2 in the Supplement]). Direct costs are split into wages, benefits, professional fees, supplies, purchased services, depreciation, leases and rentals, and other direct expenses (eFigure in the Supplement).
Some services physically performed in the OR are counted in revenue centers outside of surgery and recovery. Notable examples include anesthesia, supplies sold to patients (eg, implants and tissue factors), radiologic procedures, pathologic tests, and the blood bank. We report these costs separately from the OR costs per minute. Cost estimates for these revenue centers are not specific to the OR; for example, the cost of a unit of blood is averaged over the OR, intensive care unit, and ambulatory settings.
Statistical Analysis
All costs were winsorized to the fifth and 95th percentiles to account for outliers. Facilities with very low ambulatory surgery volumes (<10% of total operative minutes) had necessarily high costs per minute and were excluded from ambulatory analysis (this excluded 8 of 60 facilities in FY2014). Each HADR provided a cost per minute for each revenue center. We calculated the median and mean (grand mean) across facilities and stratified by setting (inpatient vs ambulatory), teaching status, and hospital ownership. Comparisons were made within and between categories using rank sum and Kruskal-Wallis tests. Ambulatory and inpatient costs were paired for a given facility using the ratio of inpatient to ambulatory costs. To assess whether covariates (eg, teaching status) had different cost trajectories over time, we conducted a difference-in-difference analysis using mixed-effects linear regression models. Two-sided tests with P < .05 were used for statistical significance.
Results
Sample and Hospital Characteristics, FY2014
Of 445 California facilities providing HADR files in FY2014, 302 were included in this analysis. Seventy-five facilities were excluded because of lack of comparability in financial statements and an additional 68 were excluded because they were the wrong type of hospital (eg, psychiatric care) or because surgical expenditure data were not available. Of the included hospitals, 78 (25.8%) were for profit, 175 (57.9%) were not for profit, and 49 (16.2%) were government owned. Thirty facilities (9.9%) were teaching hospitals (Table 1). Median annual discharge volume was 7069 patients, with 59 of 302 hospitals (19.5%) reporting less than 1000 or more than 20 000 discharges. The median number of ORs (inpatient or combined inpatient and outpatient ORs) was 6, and for the 60 hospitals reporting ambulatory surgery data, the median number of ambulatory ORs was 5.
Table 1. Characteristics of Included Short-term Hospitals in California for Fiscal Year 2014.
| Characteristic | Value (N = 302)a |
|---|---|
| Ownership, No. (%) | |
| Governmentb | 49 (16.2) |
| Investor (for profit) | 78 (25.8) |
| Not-for-profit | 175 (57.9) |
| Teaching, No. (%) | 30 (9.9) |
| Discharges, median (IQR), No. | 7069 (3298-14 471) |
| Licensed beds, median (IQR), No. | 195 (104-358) |
| Nurse FTE, median (IQR), No. | 303 (132-559) |
| Operating rooms, median (IQR), No. | |
| Inpatient | 6 (3-10) |
| Ambulatoryc | 5 (3-7) |
Abbreviations: FTE, full time equivalent; IQR, interquartile range.
Medians and IQRs presented given skewed distributions.
Including state, city, and district owned.
For a reduced sample size of 60.
Cost per Minute of OR Time, Stratified by Setting and Hospital Characteristic, FY 2014
The mean (SD) cost for 1 minute of OR time across California hospitals was $37.45 ($16.04) in the inpatient setting (Table 2) and $36.14 ($19.53) in the ambulatory setting (Table 3), which was not statistically different (P = .65). On paired analysis, however, the ratio of inpatient to ambulatory costs per minute was 1.31 (95% CI, 1.10-1.51) (Table 3). There was no difference in the mean (SD) cost of 1 minute of OR time between for-profit, not-for-profit, and government-owned facilities, in either setting (inpatient: for-profit facilities, $35.72 [$18.11]; not-for-profit facilities, $38.09 [$14.55]; and government-owned facilities, $37.94 [$17.71]; P = .08; and ambulatory: not-for-profit facilities, $35.98 [$18.92]; and government-owned facilities, $38.01 [$29.45]; P = .66 [there were no for-profit facilities with ORs in the ambulatory setting]). Teaching hospitals had lower mean (SD) expenditures than nonteaching hospitals in the inpatient setting ($29.88 [$9.06] vs $38.29 [$16.43]; P = .006), but these costs were not significantly different in the ambulatory setting ($32.78 [$15.98] vs $37.15 [$20.55]; P = .73).
Table 2. Cost per Minute for Inpatient Operating Rooms, Stratified by Ownership and Teaching Statusa.
| Characteristic | Sample Size | Cost per Minute, $ | P Valueb | |
|---|---|---|---|---|
| Mean (SD) | Median (IQR) | |||
| All inpatient operating rooms | 302 | 37.45 (16.04) | 33.78 (26.12-45.19) | NA |
| Ownership | ||||
| Governmentc | 49 | 37.94 (17.71) | 33.17 (27.76-46.68) | .08 |
| Investor (for profit) | 78 | 35.72 (18.11) | 30.26 (23.56-39.72) | |
| Not-for-profit | 175 | 38.09 (14.55) | 35.42 (27.75-45.89) | |
| Nonteaching | 272 | 38.29 (16.43) | 34.69 (27.44-46.40) | .006 |
| Teaching | 30 | 29.88 (9.06) | 27.86 (22.95-36.61) | |
Abbreviations: IQR, interquartile range, NA, not applicable.
Inpatient refers to physical location of operating rooms and can include inpatient and outpatient operations.
Nonparametric comparisons (rank sum and Kruskal-Wallis tests).
Including state, city, and district owned.
Table 3. Cost per Minute for Ambulatory Operating Rooms, Stratified by Ownership and Teaching Status, Including Paired Analysis.
| Characteristic | Sample Sizea | Cost per Minute, $ | P Valueb | |
|---|---|---|---|---|
| Mean (SD) | Median (IQR) | |||
| All ambulatory operating rooms | 52 | 36.14 (19.53) | 32.68 (20.30-46.51) | NA |
| Ownership | ||||
| Governmentc | 4 | 38.01 (29.45) | 31.63 (14.90-61.12) | .66 |
| Investor (for profit) | 0 | NA | NA | |
| Not-for-profit | 48 | 35.98 (18.92) | 32.68 (20.64-46.51) | |
| Nonteaching | 40 | 37.15 (20.55) | 32.68 (20.64-46.51) | .73 |
| Teaching | 12 | 32.78 (15.98) | 34.19 (16.84-45.82) | |
| Paired analysisd | Mean (95% CI) | |||
| Ratio (inpatient/ambulatory) | 52 | 1.31 (1.10-1.51) | NA | |
Abbreviations: IQR, interquartile range, NA, not applicable.
Reduced sample size owing to exclusion of 8 facilities with very low proportions (<10%) of ambulatory surgery.
Nonparametric comparisons (rank sum and Kruskal-Wallis tests).
Including state, city, and district owned.
Paired analysis answers the question “For hospitals with both inpatient and ambulatory surgery operating rooms, how much more does an inpatient operating room cost?”
Cost per Minute, Including Direct and Indirect Components, FY 2014
Direct expenses accounted for 54.6% of total expenses ($20.40 of $37.37) in the inpatient setting and 59.1% of total expenses ($20.90 of $35.39) in the ambulatory setting (Table 4). Wages and benefits accounted for approximately two-thirds of direct expenses (inpatient, $14.00 of $20.40; ambulatory, $14.35 of $20.90), with nonbillable supplies accounting for less than 10% of total expenses (inpatient, $2.55 of $37.37; ambulatory, $3.33 of $35.39).
Table 4. Cost per Minute Including Direct and Indirect Components, by Setting.
| Component | Inpatient Cost (n = 294)a,b | Ambulatory Cost (n = 51)b | ||||
|---|---|---|---|---|---|---|
| Mean (SD), $ | Median (IQR), $ | Proportion of Total, %c | Mean (SD), $ | Median (IQR), $ | Proportion of Total, %c | |
| Total | 37.37 (15.97) | 33.78 (26.12-44.92) | 100 | 35.39 (18.95) | 32.66 (20.02-46.47) | 100 |
| Direct | 20.40 (8.32) | 19.04 (14.11-24.61) | 54.6 | 20.90 (12.54) | 18.37 (11.53-27.06) | 59.1 |
| Wagesd | 10.00 (3.63) | 9.56 (7.29-11.81) | 26.8 | 10.07 (5.93) | 9.34 (5.87-13.36) | 28.5 |
| Benefitse | 4.00 (2.00) | 3.67 (2.35-5.18) | 10.7 | 4.28 (2.68) | 4.01 (2.39-5.23) | 12.1 |
| Suppliesf | 2.55 (2.67) | 1.44 (0.73-3.48) | 6.8 | 3.33 (3.85) | 1.73 (0.70-4.34) | 9.4 |
| Otherg | 3.37 (2.13) | 2.85 (1.81-4.50) | 9.0 | 3.09 (3.28) | 1.84 (0.85-4.06) | 8.7 |
| Indirect | 16.43 (7.99) | 14.66 (10.52-19.94) | 44.0 | 14.34 (7.82) | 13.71 (7.43-20.52) | 40.5 |
Inpatient refers to physical location of operating rooms and can include inpatient and outpatient operations.
Reduced sample size owing to missing data; the data presented are based on complete case analysis.
Proportions do not sum perfectly owing to winsorization.
Wages includes all remuneration for management, technicians, registered and licensed vocational nurses, aides, clerical and administrative staff, environment and food (if applicable), and, depending on the financial arrangement, physician and nonphysician (eg, physician assistant and nurse practitioner) salaries.
Benefits include Federal Insurance Contributions Act taxes, vacation and sick leave, insurance, and other payroll and nonpayroll benefits.
Supplies include nonbillable items such as sutures and needles and packs.
Other includes purchased services (ie, repairs and maintenance) as well as depreciation, leases, utilities, insurance, and travel.
Trends Over Time, Including Comparisons With Common Inflation Indices
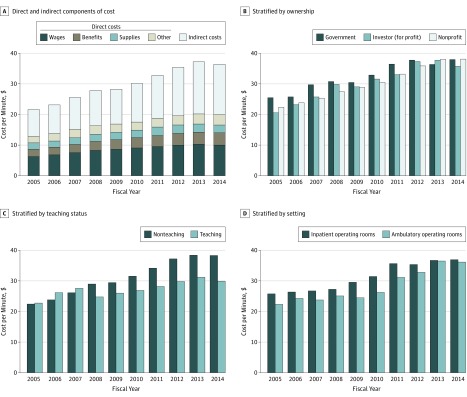
The Figure presents data over time. Figure, A shows the components of cost (direct, indirect, and subcomponents of direct) for inpatient ORs. The proportion of cost attributable to indirect expenses has increased from 39.5% to 44.3% (P < .001), with commensurate decreases in salary (29.8% to 28.1%; P = .01) and supplies (6.5% to 4.2%; P < .001). Figure, B shows inpatient costs, stratified by ownership; Figure, C shows inpatient costs, stratified by teaching status; and Figure, D shows inpatient and ambulatory costs for hospitals with both inpatient and ambulatory ORs. There was no statistical difference in trends when stratified by ownership or setting (inpatient vs ambulatory). However, teaching hospital costs increased more slowly than nonteaching hospital costs during the study (difference-in-difference coefficient, –1.098, P < .001). Costs of OR time have increased significantly faster than the medical component of the consumer price index and urban consumer price index (eTable 3 in the Supplement).
Figure. Cost per Minute, Fiscal Years 2005-2014.
A, Breakdown of direct and indirect components and direct subcomponents of cost per minute for inpatient operating rooms; total sample size for each year ranges from 291 to 309. B, Cost per minute for inpatient operating rooms stratified by ownership; total sample size for each year ranges from 295 to 311. C, Cost per minute for inpatient operating rooms stratified by teaching status; total sample size for each year ranges from 295 to 311. D, Cost per minute stratified by setting; sample includes only facilities with both inpatient and ambulatory operating rooms with at least 10% of operative minutes in the ambulatory setting; sample size for each year ranges from 46 to 58.
Miscellaneous Expenses, FY2014
Some expenses that physically occur in the OR are included in separate revenue centers (eTable 4 in the Supplement). Mean (SD) costs in FY2014 were $3.42 ($2.94) per minute for anesthesia, $305.18 ($230.81) per unit for medical supplies sold to patients, $167.89 ($68.80) per unit for radiologic procedures, $78.36 ($42.98) per unit for pathologic tests, and $294.07 ($146.88) per unit for blood products.
Discussion
The mean cost of OR time was $36 to $37 per minute using financial data from California’s short-term general and specialty hospitals in FY2014. Although small differences exist by setting, payer, and teaching status, mean costs of OR time were all between $30 and $38 per minute. Of the $36 to $37 per minute, $20 to $21 is direct costs, with $13 to $14 attributable to wages and benefits and $2.50 to $3.50 attributable to nonbillable surgical supplies.
Previous estimates of cost per minute have been limited to single-site studies with marked variation and scarce accounting details. For example, 2 studies on joint replacements estimated costs per minute at $51 for a “fully staffed rate”(p1258.e1) and $113 for “staff and instrumentation” costs.(p1785) A study in laparoscopic hysterectomy found a cost per minute of $94.14 for “support staff salaries, drapes, room maintenance, and…nonchargeable items,”(p74) while a study in pediatric hernia repair found a cost per minute of $6.67. This variation likely reflects incorporation of different cost categories. Our study, on the other hand, uses consistent resources (ie, salaries and benefits), across hundreds of California facilities, and benefits from well-defined accounting principles mandated by the OSHPD.
Across most covariates (eg, setting and ownership), costs per minute were stable, perhaps suggesting an optimized efficiency with little room for improvement. The exception, however, is in teaching hospitals, which have achieved slower growth in OR costs during the study. In FY2014, teaching hospitals spent approximately $8 per minute less than nonteaching hospitals. Although this amount is seemingly small, the hospitals with the highest volume in this study perform more than 4 million minutes of surgery per year; therefore, the potential cost savings when extrapolated to the state or national level could be considerable.
If we save 1 minute of OR time, how much does that actually save the hospital? At $37 per minute, OR time appears expensive; however, using this number without understanding its components may be misleading.
Almost half this cost is indirect—expenses generated by nonrevenue centers such as security and parking. These costs are allocated to the department based on statistical factors such as square footage. These costs are outside the control of the clinician and often beyond the control of the departments’ managers. Saving 5 minutes will have little effect on these expenses and are unlikely to be realized savings for the hospital.
Of the $20 to $21 direct costs, more than two-thirds ($13-$14) goes toward salaries and benefits—a potentially high-value target. These wages include both the staff in the OR (eg, scrub nurses and circulating nurses) as well as technicians, aides, managers, and administrators. It is important to consider which employees are affected by time-saving interventions. For example, in a group of studies that estimated cost savings by comparing wound closure techniques, all found small changes in the wound closure time, but found no difference in total procedure time. Staff that cannot leave the room after wound closure (ie, nurses and anesthesiologists) would, therefore, not be realized savings. Nevertheless, finding ways to reduce labor costs, for example, through decreased overtime and per diem pay, may be beneficial.
A total of $2.50 to $3.50 per minute is attributed to nonbillable supplies—items that cannot be charged to the patient such as gloves, packs, and sutures. Although this component is small, it is potentially mutable, and recent work has shown that cost feedback to surgeons may reduce supply costs. The final few dollars are attributed to purchased services (eg, repair services), depreciation (of equipment), leases and rentals, utilities, licenses, and insurance.
As a result of the revenue center structure, some costs are not included in the estimated cost of $37 per minute, including supplies billed to patients (eg, implants), anesthesia, radiologic procedures, pathologic tests, and the blood bank. The estimated cost of $37 per minute reflects a base rate including the resources (eg, personnel and supplies) that are essential to running an OR. This number can be useful when evaluating the effect of reducing OR time, although with the caveats listed above (ie, indirect costs are unlikely to change). Previous studies have described much higher costs per minute (>$100) through the addition of other revenue centers, such as the inclusion of an expensive implant. However, unlike the base rate, these additional costs cannot be saved through time alone; therefore, these estimates may be deceiving. Instead, these additional costs must be targeted directly by using less-expensive implants, performing fewer radiologic procedures, or sending fewer specimens for pathologic testing.
The above analysis is based on a cost-center approach—a “top-down” strategy in which total expenses are sequentially divided into smaller units. An alternative, time-driven activity-based costing (TDABC [eTable 1 in the Supplement]), starts from the bottom up. By mapping the steps of a patient’s care, the cost of each step can be calculated using the smallest unit possible (eg, 1 minute of a nurse’s time). These estimates are likely to be more accurate and actionable, and previous studies have demonstrated their feasibility in a variety of fields. But, TDABC has not been widely adopted, likely owing to the significant upfront investment. However, by dividing cost-center estimates into their smallest components, as is illustrated in our study, future research can approximate TDABC estimates. A recent TDABC study in laparoscopic appendectomy estimated personnel costs at approximately $10 per minute, similar to the numbers presented here.
Finally, opportunity cost in surgery refers to the loss of revenue from inefficiency. If saving time allows the OR to schedule an additional case, this potential revenue should be included as a cost. Opportunity costs vary and are likely to be highest for short operations (ie, myringotomy or cataract surgery), where scheduling additional cases is more likely. However, opportunity cost requires a case to be profitable, which, in many circumstances, depends primarily on payer mix.
Future work analyzing intraoperative costs should consider several details. First, the numbers presented here can be referenced as a benchmark for the average procedure performed at the average hospital. Studies using local estimates can incorporate these statewide numbers, allowing for comparisons as well as improved generalizability. Second, the resources included in cost estimates (eg, salaries and supplies) should be well described and, ideally, itemized; it is important to consider how interventions actually affect these individual categories, if at all. Value analysis committees should be wary of device manufacturers promising large cost savings based on OR time alone. Finally, the consumer price index and medical component of the consumer price index are likely not appropriate when adjusting cost data for a single revenue center.
Limitations
This study has some limitations. First, while the OSHPD provides detailed guidelines for cost allocation, differences across facilities may exist—for example, depending on compensation contracts, physician remuneration may be included under salary or professional fees or may not be included at all. How facilities account for immediate preoperative care is not stated, nor is there an explicit auditing process for time measurements. However, given the similarity in estimates across facilities, the effect of these accounting differences is likely small. Furthermore, our primary interest was creating a generalizable estimate for the cost per minute of surgery regardless of the accounting process. Second, this study provides only a mean price for an average procedure. As mentioned above, for some procedures, additional revenue centers (eg, radiologic procedures) will be involved. Although no less important to target, we believe these costs should be considered outside of the base rate of OR cost. The costs that are included in our estimates (eg, salary, benefits, and nonbillable supplies) may vary between operations, especially if additional staff are required, such as perfusionists. Finally, the results are limited to short-term hospitals in California, and because of an exemption, Kaiser hospitals are not included, limiting generalizability.
Conclusions
Assessing value relies on precise estimates of cost. The cost of 1 minute of OR time is often used with little regard to how the value was calculated. This study of California hospital financial statements found the mean cost of OR time is $36 to $37 per minute, with minimal variation by setting or institutional characteristic. More than half this cost is not modifiable in the short term, including indirect costs and depreciation of equipment, and therefore will not be realized savings unless specifically targeted. These statewide numbers can serve as a benchmark when evaluating intraoperative cost-savings efforts. Finally, understanding the composition of costs will allow those interested in value improvement to identify high-value targets.
eTable 1. Short-term Facilities With no Surgical Expenditure Information
eTable 2. Definitions of Select Financial Terminology
eTable 3. Median Operating Room Cost per Minute Versus The Consumer Price Index and Medical Component of the Consumer Price Index, as Ratios, Using 2005 as the Base Year
eTable 4. Miscellaneous Expenses not Included in OR Cost per Minute Estimates, FY2014
eFigure. Hierarchy of Hospital Expenses
References
- 1.Bai G, Anderson GF. Extreme markup: the fifty US hospitals with the highest charge-to-cost ratios. Health Aff (Millwood). 2015;34(6):922-928. [DOI] [PubMed] [Google Scholar]
- 2.Nathan H, Dimick JB. Medicare’s shift to mandatory alternative payment models: why surgeons should care. JAMA Surg. 2017;152(2):125-126. [DOI] [PubMed] [Google Scholar]
- 3.Gitelis M, Vigneswaran Y, Ujiki MB, et al. . Educating surgeons on intraoperative disposable supply costs during laparoscopic cholecystectomy: a regional health system’s experience. Am J Surg. 2015;209(3):488-492. [DOI] [PubMed] [Google Scholar]
- 4.Guzman MJ, Gitelis ME, Linn JG, et al. . A Model of cost reduction and standardization: improved cost savings while maintaining the quality of care. Dis Colon Rectum. 2015;58(11):1104-1107. [DOI] [PubMed] [Google Scholar]
- 5.Krpata DM, Haskins IN, Rosenblatt S, Grundfest S, Prabhu A, Rosen MJ. Development of a disease-based hernia program and the impact on cost for a hospital system. Ann Surg. 2018;267(2):370-374. [DOI] [PubMed] [Google Scholar]
- 6.Zygourakis CC, Valencia V, Moriates C, et al. . Association between surgeon scorecard use and operating room costs. JAMA Surg. 2017;152(3):284-291. [DOI] [PubMed] [Google Scholar]
- 7.Brodsky JB. Cost savings in the operating room. Anesthesiology. 1998;88(3):834. [DOI] [PubMed] [Google Scholar]
- 8.Tsai M. The true cost of operating room time. Arch Surg. 2011;146(7):886. [DOI] [PubMed] [Google Scholar]
- 9.Brown JK, Campbell BT, Drongowski RA, et al. . A prospective, randomized comparison of skin adhesive and subcuticular suture for closure of pediatric hernia incisions: cost and cosmetic considerations. J Pediatr Surg. 2009;44(7):1418-1422. [DOI] [PubMed] [Google Scholar]
- 10.Tillmanns TD, Mabe A, Ulm MA, Lee D, Lowe P, Kumar S. Vaginal cuff closure in robotic hysterectomy: a randomized controlled trial comparing barbed versus standard suture. J Gynecol Surg. 2016;32(4):215-219. doi: 10.1089/gyn.2015.0139 [DOI] [Google Scholar]
- 11.Ting NT, Moric MM, Della Valle CJ, Levine BR. Use of knotless suture for closure of total hip and knee arthroplasties: a prospective, randomized clinical trial. J Arthroplasty. 2012;27(10):1783-1788. [DOI] [PubMed] [Google Scholar]
- 12.Eggers MD, Fang L, Lionberger DR. A comparison of wound closure techniques for total knee arthroplasty. J Arthroplasty. 2011;26(8):1251-8.e1, 4. [DOI] [PubMed] [Google Scholar]
- 13.Lukish J, Powell D, Morrow S, Cruess D, Guzzetta P. Laparoscopic appendectomy in children: use of the endoloop vs the endostapler. Arch Surg. 2007;142(1):58-61. [DOI] [PubMed] [Google Scholar]
- 14.Macario A. What does one minute of operating room time cost? J Clin Anesth. 2010;22(4):233-236. [DOI] [PubMed] [Google Scholar]
- 15.Muñoz E, Muñoz W III, Wise L. National and surgical health care expenditures, 2005-2025. Ann Surg. 2010;251(2):195-200. [DOI] [PubMed] [Google Scholar]
- 16.Stey AM, Brook RH, Needleman J, et al. . Hospital costs by cost center of inpatient hospitalization for Medicare patients undergoing major abdominal surgery. J Am Coll Surg. 2015;220(2):207-17.e11. [DOI] [PubMed] [Google Scholar]
- 17.Office of Statewide Health Planning and Development Accounting and reporting manual for California hospitals, second edition. https://www.oshpd.ca.gov/documents/HID/HospitalFormsInstructions/ch2000.pdf. Accessed June 20, 2017.
- 18.Baker JJ, Baker RW. Health Care Finance: Basic Tools for Nonfinancial Managers. 4th ed Burlington, Massachusetts: Jones & Bartlett Learning; 2014. [Google Scholar]
- 19.Sanders GD, Neumann PJ, Basu A, et al. . Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093-1103. [DOI] [PubMed] [Google Scholar]
- 20.Joynt KE, Orav EJ, Jha AK. Association between hospital conversions to for-profit status and clinical and economic outcomes. JAMA. 2014;312(16):1644-1652. [DOI] [PubMed] [Google Scholar]
- 21.Holloran-Schwartz MB, Gavard JA, Martin JC, Blaskiewicz RJ, Yeung PP Jr. Single-use energy sources and operating room time for laparoscopic hysterectomy: a randomized controlled trial. J Minim Invasive Gynecol. 2016;23(1):72-77. [DOI] [PubMed] [Google Scholar]
- 22.Sah AP. Is there an advantage to knotless barbed suture in TKA wound closure? a randomized trial in simultaneous bilateral TKAs. Clin Orthop Relat Res. 2015;473(6):2019-2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sebesta MJ, Bishoff JT. Octylcyanoacrylate skin closure in laparoscopy. J Endourol. 2003;17(10):899-903. [DOI] [PubMed] [Google Scholar]
- 24.Najjar PA, Strickland M, Kaplan RS. Time-driven activity-based costing for surgical episodes. JAMA Surg. 2017;152(1):96-97. [DOI] [PubMed] [Google Scholar]
- 25.Kaplan RS, Porter ME. How to solve the cost crisis in health care. Harv Bus Rev. 2011;89(9):46-52, 54, 56-61 passim. [PubMed] [Google Scholar]
- 26.DiGioia AM III, Greenhouse PK, Giarrusso ML, Kress JM. Determining the true cost to deliver total hip and knee arthroplasty over the full cycle of care: preparing for bundling and reference-based pricing. J Arthroplasty. 2016;31(1):1-6. [DOI] [PubMed] [Google Scholar]
- 27.McLaughlin N, Burke MA, Setlur NP, et al. . Time-driven activity-based costing: a driver for provider engagement in costing activities and redesign initiatives. Neurosurg Focus. 2014;37(5):E3. [DOI] [PubMed] [Google Scholar]
- 28.Yu YR, Abbas PI, Smith CM, et al. . Time-driven activity-based costing to identify opportunities for cost reduction in pediatric appendectomy. J Pediatr Surg. 2016;51(12):1962-1966. [DOI] [PubMed] [Google Scholar]
- 29.Chatterjee A, Payette MJ, Demas CP, Finlayson SR. Opportunity cost: a systematic application to surgery. Surgery. 2009;146(1):18-22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Short-term Facilities With no Surgical Expenditure Information
eTable 2. Definitions of Select Financial Terminology
eTable 3. Median Operating Room Cost per Minute Versus The Consumer Price Index and Medical Component of the Consumer Price Index, as Ratios, Using 2005 as the Base Year
eTable 4. Miscellaneous Expenses not Included in OR Cost per Minute Estimates, FY2014
eFigure. Hierarchy of Hospital Expenses