Key Points
Question
Is chest dysphoria (distress about breasts) more common among transmasculine youth who have not had chest reconstruction compared with those who have undergone this surgery?
Findings
In this cohort study, chest dysphoria was significantly higher in the nonsurgical vs postsurgical cohort. Among the nonsurgical cohort, 94% perceived chest surgery as very important; among the postsurgical cohort, serious complications were rare, and 67 of 68 reported an absence of regret.
Meaning
Professional guidelines and clinical practice should recommend patients for chest surgery based on individual need rather than chronologic age.
This cohort study examines chest dysphoria in transmasculine youth who have had chest reconstruction surgery compared with those who have not.
Abstract
Importance
Transmasculine youth, who are assigned female at birth but have a gender identity along the masculine spectrum, often report considerable distress after breast development (chest dysphoria). Professional guidelines lack clarity regarding referring minors (defined as people younger than 18 years) for chest surgery because there are no data documenting the effect of chest surgery on minors.
Objective
To examine the amount of chest dysphoria in transmasculine youth who had had chest reconstruction surgery compared with those who had not undergone this surgery.
Design, Setting, and Participants
Using a novel measure of chest dysphoria, this cohort study at a large, urban, hospital-affiliated ambulatory clinic specializing in transgender youth care collected survey data about testosterone use and chest distress among transmasculine youth and young adults. Additional information about regret and adverse effects was collected from those who had undergone surgery. Eligible youth were 13 to 25 years old, had been assigned female at birth, and had an identified gender as something other than female. Recruitment occurred during clinical visits and via telephone between June 2016 and December 2016. Surveys were collected from participants who had undergone chest surgery at the time of survey collection and an equal number of youth who had not undergone surgery.
Main Outcomes and Measures
Outcomes were chest dysphoria composite score (range 0-51, with higher scores indicating greater distress) in all participants; desire for chest surgery in patients who had not had surgery; and regret about surgery and complications of surgery in patients who were postsurgical.
Results
Of 136 completed surveys, 68 (50.0%) were from postsurgical participants, and 68 (50.0%) were from nonsurgical participants. At the time of the survey, the mean (SD) age was 19 (2.5) years for postsurgical participants and 17 (2.5) years for nonsurgical participants. Chest dysphoria composite score mean (SD) was 29.6 (10.0) for participants who had not undergone chest reconstruction, which was significantly higher than mean (SD) scores in those who had undergone this procedure (3.3 [3.8]; P < .001). Among the nonsurgical cohort, 64 (94%) perceived chest surgery as very important, and chest dysphoria increased by 0.33 points each month that passed between a youth initiating testosterone therapy and undergoing surgery. Among the postsurgical cohort, the most common complication of surgery was loss of nipple sensation, whether temporary (59%) or permanent (41%). Serious complications were rare and included postoperative hematoma (10%) and complications of anesthesia (7%). Self-reported regret was near 0.
Conclusions and Relevance
Chest dysphoria was high among presurgical transmasculine youth, and surgical intervention positively affected both minors and young adults. Given these findings, professional guidelines and clinical practice should consider patients for chest surgery based on individual need rather than chronologic age.
Introduction
The last decade has seen an unprecedented number of youth presenting for care related to gender dysphoria at gender-specific clinics and centers around the United States, Canada, and Europe.1,2 Transmasculine youth (those assigned a female sex at birth who have a gender identity along the masculine spectrum) who have undergone an endogenous female puberty and subsequent breast development commonly experience significant discomfort with the presence of breasts (chest dysphoria). Many but not all of these youth desire surgical intervention to achieve a flatter chest contour. This procedure involves a double mastectomy with downsizing and regrafting of the nipple areola complex or a minimally invasive procedure that spares the nipple.3
As an interim strategy prior to chest surgery, many youth bind their chest in order to achieve a flatter, more masculine appearance. In a recent study of 1800 adults, Peitzmeier et al4 report an exhaustive list of negative health outcomes related to the practice of binding. These included pain, rib fractures, light-headedness, weakness, skin infection, and others.
There are no measures that capture the discomfort and subsequent consequences of chest dysphoria. The purpose of this study was to develop a measure that captures the distress associated with having a feminine chest contour (breasts) experienced by minors (persons younger than 18 years) and young adults (those aged 18 to 25 years) with a masculine gender identity, understand the association with chest surgery, and determine if there are differences in this association between young adults and minors. These results may serve to inform the practice of health care professionals with lingering concerns about potential complications, patient regret, and lawsuits, particularly for minors.
Surgical interventions for transgender individuals undergoing phenotypic gender transition have been considered an integral part of the transitioning process from as far back as the 1950s.5 Dissatisfaction with primary and secondary sex characteristics aligned with the chromosomes and gonads one has, rather than one’s gender of identity, is a fundamental characteristic of gender dysphoria.6 While surgical procedures are not desired by all individuals with transgender experience, these procedures are commonly sought in order to bring the physical body into better alignment with the experienced gender.7 Satisfaction rates across studies of adult transmasculine individuals undergoing chest reconstruction are 97%, and regret is present in less than 1% of transmasculine patients.8 Hormone therapy and surgery have been found to be medically necessary to diminish gender dysphoria.7,9 Few data have been published concerning the outcomes of these procedures among minors, despite the growing numbers of youth presenting for care.1
Most transmasculine youth are accessing care after or near completion of breast development, necessitating surgical intervention for those who wish to have a masculine-appearing chest contour. Because pubertal development of people who are assigned female at birth may begin as early as 8 or 9 years of age, completion of puberty is plausible even as young as 12 years.
National guidelines regarding surgical interventions for minors are outlined in the World Professional Association for Transgender Health Standards of Care, version 7.9 These guidelines recommend that adolescents defer genital surgery until the age of consent, but acknowledge that individual minors might be candidates for chest reconstruction. Despite this acknowledgment, many insurance plans continue to impose a mandatory age requirement of 18 years for chest surgery, as well as the use of testosterone for a full year prior to surgery to ensure the best results. While breast tissue does tend to atrophy with the use of testosterone, this effect is only partial.10 The adolescent section of the Standards of Care, version 7, recommends 1 year of testosterone use prior to chest surgery, but specifically states elsewhere that “hormone therapy is not a pre-requisite” for surgery.9(p59) It leaves unclear why the recommendation is in place for adolescents but not for adults. The recommendation to omit the requirement of hormone administration acknowledges that there are individuals who desire chest surgery but do not wish to undergo hormone therapy for phenotypic gender transition.9,11
This study was undertaken to determine if chest reconstruction diminishes chest dysphoria and if it should be considered a medically necessary intervention for both transmasculine minors and young adults. Additionally, in providing data on the experience of youth younger than 18 years, we hope to inform future revisions of existing guideline recommendations regarding transgender minors seeking surgical interventions to help mitigate gender dysphoria.
Methods
Practice Setting
The Center for Transyouth Health and Development at Children’s Hospital Los Angeles has been serving the medical and mental health needs of transgender adolescents and young adults since 1993. At the time of this study, the center was serving 818 gender-nonconforming and transgender youth. Of the youth in care, 384 (46.9%) were assigned the female sex at birth; 93 youth (24.2%) had undergone chest reconstruction surgery before the study commenced.
Consent Procedures
The research study was approved by the Children’s Hospital Los Angeles institutional review board. One or more parents or legal guardians provided consent for eligible minors. All participants provided verbal consent before completing the survey.
Study Eligibility
Youth in the nonsurgical group and the postsurgical group were considered eligible to complete the survey if they were 13 to 25 years old, assigned female at birth, identified their gender as something other than female, were able to read and understand English, and were able to provide consent.
Youth were included in the nonsurgical group if they had not undergone chest reconstruction surgery and had chest tissue consistent with female development. Prepubertal youth and those who had been administered puberty-blocking medications early in development were ineligible.
Youth were included in the postsurgical group if they had undergone chest reconstruction surgery. All participating youth who had undergone chest reconstruction surgery had done so after obtaining referral letters from medical and mental health professionals as required by the surgeons and insurance plans. The process by which individual mental health professionals assess readiness for surgery varies across practices. The common goal of health care professionals is to assure that patients have the capacity to provide consent and are fully informed about the mechanics, recovery, and irreversible nature of the surgery.
Study Recruitment and Data Collection
Participants were recruited from the youth visiting the Center for Transyouth Health and Development for routine gender-related care between June 2016 and December 2016. A total of 52 patients (13.5%) were ineligible to participate in this study because they did not have chest tissue as a result of being either prepubertal or having taken puberty-blocking medications early in development. The remaining 332 transmasculine youth in active care were considered eligible for the study. All transmasculine youth who met study inclusion criteria and came for visits during this time were approached to participate. Nonsurgical youth outnumbered postsurgical youth in active care at the clinic by a ratio of 3.5:1, and to survey as many postsurgical youth as possible, study staff attempted to contact via telephone all postsurgical youth who had not visited the clinic during the enrollment period. Two postsurgical youth refused the survey, and 24 (26%) could not be contacted. Of those who could not be contacted, 12 had no working phone number, 7 did not respond to 3 messages left, and 5 agreed to participate but could not coordinate a time. Telephone calls and clinic visits during the study period yielded 68 (72%) completed surveys from postsurgical participants.
To obtain a sample of youth without surgery, we recruited until a comparable number of surveys were completed during the window of clinical visits. None of the youth who had not undergone surgery who were approached refused to participate.
The 10-minute survey collected demographic information, characteristics of surgery, and chest dysphoria. No incentive was provided for survey completion. Study data were collected and managed using Research Electronic Data Capture electronic data capture tools, which are hosted at the Southern California Clinical and Translational Science Institute.12
Development of the Chest Dysphoria Scale
To develop the Chest Dysphoria Scale, 21 survey items were generated that queried multiple aspects of chest dysphoria based on clinical experience of the first author over the past 11 years of delivering clinical care for transgender youth in a large, urban, hospital-based gender clinic. To establish face validity from the community perspective, the scale was reviewed by a small number of transmasculine youth and transmasculine adults who evaluated whether the questions captured elements of chest dysphoria effectively, used appropriate language, and was otherwise generally acceptable. The scale includes items related to physical functioning, including hygiene and exercise, intimate partnerships and dating, being perceived as a member of a gender other than their gender of identity, and disruption of future plans. Items such as “I avoid bathing/showering in order to avoid seeing my chest,” and “I avoid seeking medical care because of my chest” were scored using a Likert scale, from 0 (never) to 3 (all the time). The complete Chest Dysphoria Scale is displayed in Table 1.
Table 1. Chest Dysphoria Scale (Final Version).
| Item | Patients Endorsing Item, No. (%)a | |
|---|---|---|
| Nonsurgical Patients (n = 68) | Postsurgical Patients (n = 68) | |
| Items included in the final scale | ||
| I like looking at my chest in the mirror | 7 (10) | 57 (84) |
| Taking a shower/bath is difficult because I have to see my chest | 40 (59) | 1 (2) |
| I avoid going to the beach and/or swimming in public places because of my chest | 55 (81) | 7 (10) |
| I get gendered as female because of my chest | 24 (35) | 1 (2) |
| Dating/forming intimate partnerships is more difficult because of my chest | 34 (50) | 1 (2) |
| Physical intimacy/sexual activity is difficult because of my chest | 41 (60) | 2 (3) |
| I have struggled to make future plans because of my chest | 39 (57) | 1 (2) |
| I avoid exercise because of my chest | 32 (47) | 1 (2) |
| I avoid shopping/buying clothing because of my chest | 21 (31) | 0 (0) |
| I avoid seeking medical care because of my chest | 9 (13) | 1 (2) |
| I feel like my life hasn’t started because of my chest | 40 (59) | 1 (2) |
| I avoid swimming in private places because of my chest | 44 (65) | 2 (3) |
| I have to buy/wear certain clothes because of my chest | 54 (79) | 0 (0) |
| I sleep with a binder on at night | 11 (16) | 0 (0) |
| I avoid using locker rooms because of my chest | 53 (78) | 5 (7) |
| I worry that people are looking at my chest | 57 (84) | 7 (10) |
| I participate in life less than others because of my chest | 41 (60) | 1 (2) |
| Additional items not included in final scale | ||
| Thinking about my chest does not get in the way of daily activities | 13 (19) | 40 (59) |
| My chest does not get in the way of attending school/work | 15 (22) | 42 (62) |
| I avoid bathing/showering in order to avoid seeing my chest | 11 (16) | 0 (0) |
| I bind my chest in the daytime | 60 (88) | 0 (0) |
Frequencies and corresponding percentages represent combine responses of “frequently” and “all the time.”
A principal components extraction method by an oblique (oblimin) rotation yielded a single factor comprised of 17 items (eigenvalue, 11.1). The same factor structure emerged when analyses were conducted with nonsurgical and postsurgical cohorts separately. After imputing the mean of all completed items in place of missing values, the 17 items yielded a composite score ranging from 0 to 51, with higher scores indicating greater chest dysphoria. Missing data were minimal (<5%) for all items. Data with mean imputations were used to calculate the α and also for subsequent analyses involving the Chest Dysphoria Scale. Results of tests for internal consistency suggest high reliability (Cronbach α for postsurgical patients, .79; Cronbach α for nonsurgical patients, .89). See Table 1 for information about the 4 items dropped from the scale.
Statistical Analysis
Descriptive characteristics for both nonsurgical and postsurgical cohorts were summarized. The ages of respondents were stratified by age for binary analyses (<18 years and ≥18 years). In the nonsurgical cohort, the analysis was dichotomized based on age at the time of survey, and in the postsurgical cohort, the analysis was based on age at time of chest surgery. To examine the utility of the 1 year taking testosterone prior to surgery recommended by insurance plans, a simple linear regression model was used to evaluate the relationship between duration of time taking testosterone and chest dysphoria scores in nonsurgical cohort respondents. Results were expressed as regression coefficients with 95% confidence intervals. Analyses were conducted using IBM SPSS Statistics, version 17.0 (IBM Corporation).
Results
Descriptive Characteristics
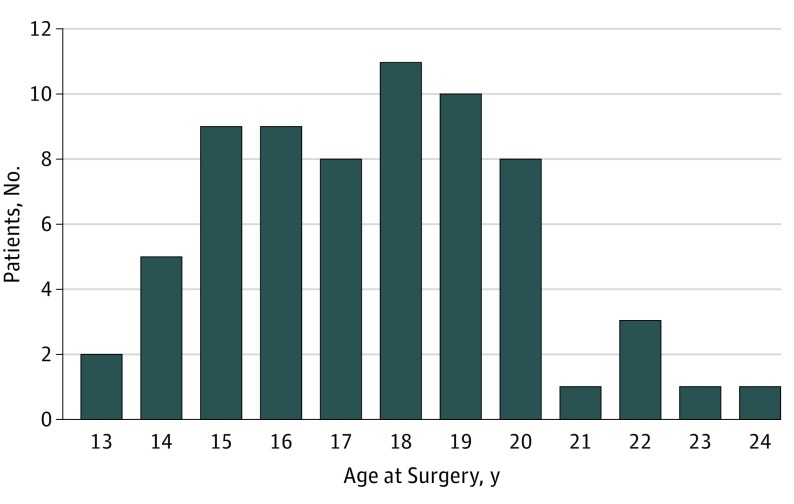
At the time of survey, the mean (SD) age of postsurgical participants was 19 (2.5) years (range, 14-25 years). The length of time between survey and chest surgery varied from less than 1 year to 5 years (Table 2). The mean (SD) age at chest surgery in this cohort was 17.5 (2.4) years (range, 13-24 years), with 33 (49%) being younger than 18 years. Of the 33 postsurgical participants younger than 18 years at surgery, 16 (48%) were 15 years or younger (Figure). At the time of survey, the mean (SD) age of participants without surgery was 17 (2.5) years (range, 13-23 years), with 39 (57%) being younger than 18 years.
Table 2. Descriptive Characteristics of Nonsurgical and Postsurgical Cohorts.
| Characteristic | No. (%) | |
|---|---|---|
| Postsurgical Patients (n = 68) | Nonsurgical Patients (n = 68) | |
| Age range (at time of survey), y | 14-25 | 13-23 |
| Age, mean (SD), y | 18.9 (2.5) | 16.9 (2.5) |
| Length of time since surgery, y | ||
| <1 | 20 (29) | NA |
| 1 | 20 (29) | NA |
| 2 | 19 (28) | NA |
| 3 | 4 (6) | NA |
| 4 | 4 (6) | NA |
| 5 | 1 (2) | NA |
| Hormone related descriptive characteristics | ||
| Currently taking testosterone? | 66 (97) | 59 (87) |
| Age at start of testosterone, mean (SD), y | 16.3 (2.1) | 16.4 (2.0) |
| Length of time taking testosterone, y | ||
| <0.5 | 6 (9) | 27 (46) |
| 0.50-1 | 3 (4) | 11 (19) |
| 1-2 | 19 (29) | 15 (25) |
| >2 | 38 (58) | 6 (10) |
Abbreviation: NA, not applicable.
Figure. Age at Chest Surgery in the Postsurgical Cohort.
Graph includes all study participants who had undergone chest reconstruction (n = 68).
Emotional and Physical Features of Postsurgical Cohort
All postsurgical participants (68 of 68; 100%) affirmed the statement, “It was a good decision to undergo chest reconstruction.” Sixty-seven of 68 postsurgical respondents reported no regret about undergoing the procedure. Only 1 participant (who was older than 18 years at the time of surgery) reported experiencing regret “sometimes.” The most common complications reported following chest surgery were temporary and permanent loss of nipple sensation (40 of 68, or 59%, and 22 of 68, or 32%, respectively; permanency was assessed as continuation of the condition from surgery to the time of survey collection), loss of sensation in other areas of the chest (28 of 68; 41%), and unequal chest appearance (9 of 68; 13%) (Table 3). There were no statistically significant differences in complication rates reported between those younger than 18 years vs those 18 years or older at the time of surgery. Mean (SD) chest dysphoria scores among postsurgical participants were 3.3 (3.8) and were not significantly associated with length of time between surgery and survey, complication rates, or age group (minors vs those 18 years or older). Items from the Chest Dysphoria Scale indicating functional limitations were rarely endorsed (Table 1).
Table 3. Complications of Chest Reconstruction Surgery.
| Complication | Participants, No. (%) (n = 68) |
|---|---|
| Temporary loss of nipple sensation | 40 (59) |
| Loss of sensation of other areas of the chest | 29 (41) |
| Long-term loss of nipple sensation | 22 (32) |
| Keloid (excessive) scarring | 10 (15) |
| Unequal chest appearance | 9 (13) |
| Postoperative hematoma | 7 (10) |
| Postoperative pain beyond normal healing time | 6 (9) |
| Nipple/areola(s) too large | 5 (7) |
| Complications related to anesthesia | 5 (7) |
Nonsurgical Cohort
Interest in chest reconstruction among respondents was high, with nearly 70% responding to the question, “How important is having chest surgery to you?” with the description, “one of the most important things for [them] right now”; another 17 (25%) described it as “very important.” The majority (59 of 68; 87%) were using testosterone at the time of survey (Table 2). Chest dysphoria was higher for those who had been taking testosterone longer, increasing by 0.33 points for each month taking testosterone. There were no statistically significant differences in levels of chest dysphoria by age group (minors vs those 18 years and older). For items denoting functional limitations, nearly half (32 of 68; 47%) of participants avoided exercise, 11 of 68 (16%) avoided bathing, 11 of 68 (16%) slept with a chest binder at night, and 10 of 68 (13%) avoided seeking medical care because of their chest (Table 1). Half of the participants (34 of 68) found intimate partnerships more difficult because of their chest, and 40 of 68 (59%) reported feeling that their chest interfered with making future plans for their life.
Comparison of Chest Dysphoria Scale Scores by Cohort
Possible chest dysphoria composite scores ranged from 0 to 51, with higher scores indicating greater distress. Chest dysphoria composite mean (SD) scores differed significantly between those who had not undergone chest reconstruction (29.6 [10.0]; n = 68) and those who had (3.3 [3.8]; n = 68; P < .001). There was no significant difference in mean chest dysphoria score between those who had surgery at ages younger than 18 years vs those who had surgery at 18 years or older.
Discussion
Concern exists among parents and professionals about surgical interventions for transgender youth, particularly those of minority age status. Professionals harbor concerns about liability in performing transgender-related surgeries that patients may potentially regret after the procedure. This study demonstrated very low rates of regret among postsurgical youth among minors as well as those 18 years and older at the time of surgery. Reported adverse effects in the postsurgical cohort were also relatively minimal.
Chest dysphoria can negatively affect the health of young transmasculine individuals. Within our cohort of youth who had not undergone surgery, substantial numbers of youth were avoiding seeking medical care because of their chests and were binding their chests frequently or all the time, including during sleep. Youth feeling that their chest impeded life plans is an indicator of the negative effect of having an internal masculine gender identity that is at odds with the outward appearance of a female chest contour. Comparison of postsurgical and nonsurgical youth suggests that chest reconstruction had a positive effect both transmasculine minors and young adults.
Many insurance companies require continuous 12 months of testosterone use prior to undergoing chest surgery. The nonsurgical cohort in this study had been taking testosterone for periods ranging from less than 1 month to 52 months, with chest dysphoria increasing the longer their time on hormones. This finding should not be construed as an endorsement to withhold or delay testosterone initiation to avoid chest dysphoria intensity. It is unclear if the chest dysphoria increase is specific to the length of time taking testosterone or simply because of a longer waiting period between initiation of physical gender transition and surgery. The increasing chest dysphoria after testosterone treatment begins does reflect a common clinical phenomenon: a honeymoon period after testosterone initiation that quickly becomes eclipsed by the greater disparity between a more masculine presentation and a female chest contour. Clinicians should advise patients and families that chest dysphoria may increase over time after starting hormone therapy. In addition, the recommendation of many insurance companies that individuals take hormones for 12 months prior to chest surgery may create additional barriers to chest surgery and cause additional harm.
Limitations
Despite our participants being recruited from a single site, these data are likely generalizable to youth receiving care at clinic sites in similar settings: large, urban, academically affiliated clinics serving multiethnic youth. This investigation was limited by the cross-sectional research design; a prospective design collecting data on the same participants before and after surgical intervention would likely yield results more specific to the intervention of chest reconstruction.
An additional limitation of the study was the small sample size. The nonsurgical cohort was a convenience sample, recruited from those with appointments during the data collection period. There could be unknown imbalances between the nonsurgical and postsurgical cohorts that could have confounded the study findings.
Finally, the Chest Dysphoria Scale is not yet validated, and may not represent distress or correlate with validated measures of quality of life, depression, anxiety, or functioning. Our intent is to move forward with the process of validation, so that it might be useful in clinical practice.
Conclusions
In future studies, it would be informative to determine whether the outcome of either chest dysphoria or chest surgery varies with race/ethnicity, type of surgery, or gender identity (nonbinary vs masculine). Future studies should consider investigating the outcome of chest dysphoria on participation and functioning in school, work, and family activities.
Given the numerous complications associated with chest binding, the negative emotional and mental effects of chest dysphoria, and the positive outcome of chest surgery demonstrated in this study, changes in clinical practice and in insurance plans’ requirements for youth with gender dysphoria who are seeking surgery seem essential. Youth should be referred for chest surgery based on their individual needs, rather than their age or time spent taking medication. Individualized, patient-centered care plans should be considered the standard of care for all transgender adolescents, and referrals should be made accordingly.
References
- 1.Spack NP, Edwards-Leeper L, Feldman HA, et al. Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics. 2012;129(3):418-425. [DOI] [PubMed] [Google Scholar]
- 2.Khatchadourian K, Amed S, Metzger DL. Clinical management of youth with gender dysphoria in Vancouver. J Pediatr. 2014;164(4):906-911. [DOI] [PubMed] [Google Scholar]
- 3.Frederick MJ, Berhanu AE, Bartlett R. Chest surgery in female to male transgender individuals. Ann Plast Surg. 2017;78(3):249-253. [DOI] [PubMed] [Google Scholar]
- 4.Peitzmeier S, Gardner I, Weinand J, Corbet A, Acevedo K. Health impact of chest binding among transgender adults: a community-engaged, cross-sectional study. Cult Health Sex. 2017;19(1):64-75. [DOI] [PubMed] [Google Scholar]
- 5.Benjamin H. The Transsexual Phenomenon. New York, NY: Julian Press; 1966. [DOI] [PubMed] [Google Scholar]
- 6.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 5th ed Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 7.Davis SA, Melter SC. Effects of testosterone treatment and chest reconstruction surgery on mental health and sexuality in female-to-male transgender people. Int J Sex Health. 2013;26(2):113-128. [Google Scholar]
- 8.Gijs L, Braeways A. Surgical treatment of gender dysphoria in adults and adolescents: recent developments, effectiveness, and challenges. Annu Rev Sex Rsch. 2007;18(1):178-224. [Google Scholar]
- 9.World Professional Association for Transgender Health Standards of care for the health of transsexual, transgender, and gender nonconforming people, version 7. https://s3.amazonaws.com/amo_hub_content/Association140/files/Standards%20of%20Care%20V7%20-%202011%20WPATH%20(2)(1).pdf. Accessed February 14, 2012.
- 10.Berry MG, Curtis R, Davies D. Female-to-male transgender chest reconstruction: a large consecutive, single-surgeon experience. J Plast Reconstr Aesthet Surg. 2012;65(6):711-719. [DOI] [PubMed] [Google Scholar]
- 11.Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, et al. ; Endocrine Society . Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2009;94(9):3132-3154. [DOI] [PubMed] [Google Scholar]
- 12.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]