A healthy 42-year-old woman presented proteinuria and hematuria on regular medical check-up two years ago. Her other laboratory examinations did not show any abnormal findings, including renal function, anti-neutrophil antibody, anti-neutrophil cytoplasmic antibody, C3, C4, or immunoglobulin. Her blood pressure was also normal. Because flank pain had developed, color Doppler ultrasound of the kidney was performed. There was a 2-cm-sized renal cyst with blood flow in the right kidney (Fig. 1). Computed tomography angiography and renal angiography demonstrated it to be a renal arteriovenous malformation (RAVM) (Fig. 1, 2). Based on the size of the malformation, its location, and symptoms of the patient, we planned elective endovascular treatment. Successful selective embolization with 5 coils was done, and she was discharged the day after without any complications.
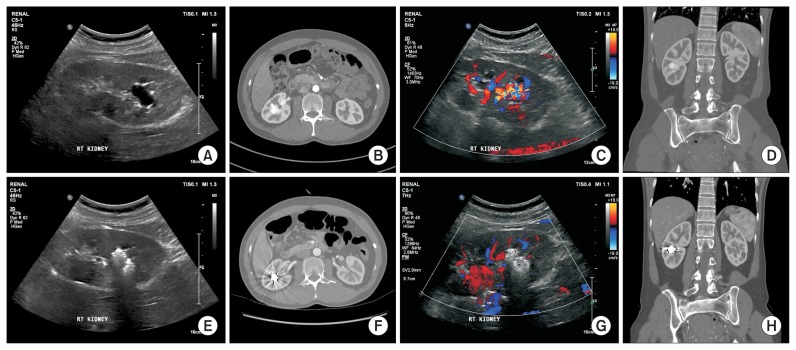
Figure 1. Ultrasound and computed tomography angiography.
Left column shows ultrasound images, and right column shows computed tomography angiography images. (A–D) Before endovascular treatment. (E–F) After endovascular treatment.
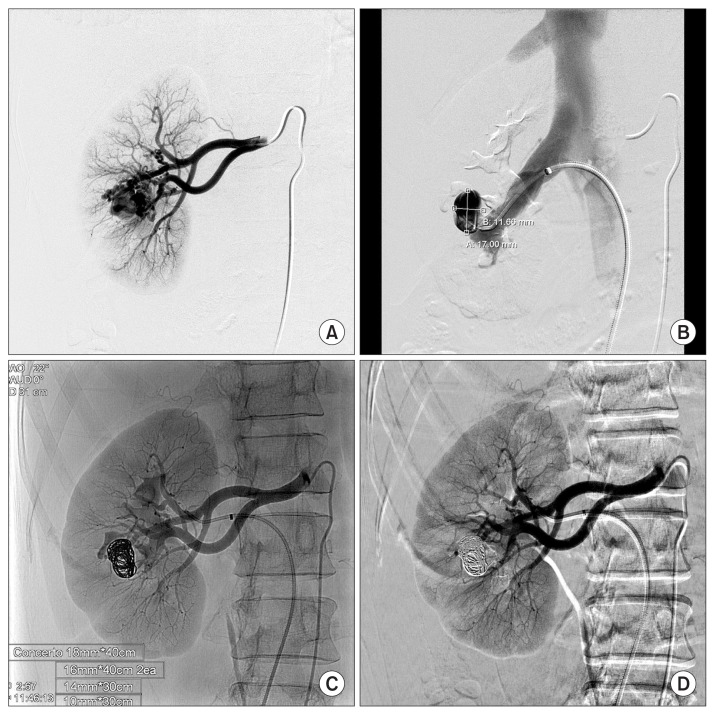
Figure 2. Angiography of the right renal artery.
(A, B) Before endovascular treatment. (C, D) After endovascular treatment.
RAVMs are an unusual disease with a prevalence less than 0.04%. It may or may not manifest symptoms, such as flank pain, hematuria, hypertension, and flank bruit. When patients show these kinds of symptoms, RAVMs should be considered, and image studies should be performed. Compared with surgical treatment, transcatheter arterial embolization can reduce complications and length of hospital stay and could be considered as the treatment of choice for RAVMs.
Footnotes
Conflicts of interest
All authors have no conflicts of interest to declare.