Abstract
Objectives
To estimate prevalence of and factors contributing to bullying among senior doctors and dentists in New Zealand’s public health system, to ascertain rates of reporting bullying behaviour, perceived barriers to reporting and the effects of bullying professionally and personally.
Design
Cross-sectional, mixed methods study.
Setting
New Zealand.
Participants
Members of the Association of Salaried Medical Specialists (40.8% response rate).
Main outcome measures
Prevalence of bullying was measured using the Negative Acts Questionnaire (revised) (NAQ-r). Workplace demands and level of peer and managerial support were measured with the Health and Safety Executive Management Standards Analysis tool. Categories of perpetrators for self-reported and witnessed bullying and barriers to reporting bullying were obtained and qualitative data detailing the consequence of bullying were analysed thematically.
Results
The overall prevalence of bullying, measured by the NAQ-r, was 38% (at least one negative act on a weekly or daily basis), 37.2% self-reported and 67.5% witnessed. There were significant differences in rates of bullying by specialty (P=0.001) with emergency medicine reporting the highest bullying prevalence (47.9%). The most commonly cited perpetrators were other senior medical or dental specialists. 69.6% declined to report their bullying. Bullying across all measures was significantly associated with increasing work demands and lower peer and managerial support (P=0.001). Consequences of bullying were wide ranging, affecting workplace environments, personal well-being and subjective quality of patient care.
Conclusions
Bullying is prevalent in New Zealand’s senior medical workforce and is associated with high workloads and low peer and managerial support. These findings help identify conditions and pressures that may encourage bullying and highlight the significant risk of bullying for individuals and their patients.
Keywords: bullying, medical specialists, New Zealand
Strengths and limitations of this study.
Strengths include being the first study to report prevalence of bullying using the Negative Acts Questionnaire (revised) in a multispecialty nationwide survey of medical specialists in any country.
It fills a gap in the otherwise scant literature on senior medical professionals as victims of bullying.
It extends the understanding of bullying as a multicausal phenomenon, demonstrating the roles of increasing work demands and low peer and managerial support, as well as suggesting opportunities for mitigation.
Limitations include a moderate participation rate and use of self-reported data.
The cross-sectional design limits the scope for causal inference.
Introduction
Workplace bullying in medicine is a cause of ongoing concern in several countries. Described as the most ‘destructive phenomenon plaguing medical culture’,1 it poses significant risks to patient safety and quality of patient care,2 staff morale and job satisfaction,3 and the physical and psychological well-being of doctors and their coworkers.4 5
Workplace bullying is defined as an escalating process where individuals repeatedly and over a period of time experience negative actions and behaviours from the people they encounter at work.6 7 Bullying behaviours may range from overt aggression and violence to subtle and indirect acts. The intent of the behaviour(s) is not the primary consideration; it is the impact on and perception of the victim that is key in determining whether or not bullying has occurred.8 9
The antecedents of workplace bullying are many and complex. The high rates of bullying experienced by junior doctors and trainees, for example, have been ascribed to the hierarchical model of medical training with bullying described as a necessary but unpleasant ‘rite of passage’.1 10 Factors known to encourage bullying include stressful and demanding work environments,11 competitive and unsupportive workplace cultures,8 and normalisation of incivility and rudeness in common conduct.12
Research commissioned by the Royal Australasian College of Surgeons in 2015 found almost half of all surgeons in New Zealand (NZ) and Australia had experienced some form of inappropriate behaviour, with trainees reporting the highest reported levels of bullying among those surveyed.13 Surgical directors or consultants were found to be the main perpetrators. Much less is known about the prevalence and consequences of bullying experienced by consultants and specialists in other specialities. In the NZ context, specialists are defined as any medical practitioner who is vocationally registered by the Medical Council of New Zealand in an approved branch of medicine. Of the known studies that have focused on senior doctors, the focus has been on bullying prevalence in specific medical specialties, for example, Australian general surgery consultants,14 Australasian fellows of the college of intensive care medicine,15 or obstetrics and gynaecology consultants working in the British National Health Service.16
To the best of the authors’ knowledge, no studies to date have specifically assessed the prevalence of bullying in medical specialists in a multispecialty, multicentre, nationwide survey. This study addresses this knowledge gap by investigating the prevalence of bullying among senior doctors and dentists of different specialties working in NZ’s public health system. The study also explores correlates of experiencing negative behaviours, including medical specialty, gender and ethnicity as well as perceived levels of workplace demands and support from peers and non-clinical managers. Finally, the study examines the nature and extent of barriers to formally reporting bullying behaviour as well as the consequences of bullying on the professional and personal lives of respondents.
Methods
Participants
Participants were members of the Association of Salaried Medical Specialists (ASMS) who are medical and dental specialists, and other non-specialist registered medical officers, employed by NZ’s 20 district health boards (DHB) and other medical employers around the country such as the national blood service and community health providers. DHBs provide inpatient and outpatient healthcare for geographically defined populations within NZ’s health system and are the main employers of health professionals working in the public sector. The ASMS is the professional association and union for senior doctors and dentists in NZ. For ease of description, these ASMS members are referred to as medical specialists or as the senior medical workforce. At the time of the survey, the ASMS represented over 90% of all senior doctors and dentists and other non-vocationally registered medical specialists employed within NZ’s DHBs and approximately 77% of non-DHB employers.
The entire ASMS membership (4307 individuals) was invited by email to participate voluntarily in an anonymous electronic survey in June 2017. The invitation emphasised the anonymous nature of the survey and noted that analysis would not be undertaken on a line-by-line basis to encourage participation. The survey was open for 1 month and four reminders were sent out to encourage participation. Demographic information, including age, gender, main place of work, ethnicity and country of primary medical qualification, was requested, summarised and described.
Measures
Prevalence of workplace bullying was measured with the Negative Acts Questionnaire (revised) (NAQ-r), developed by Einarsen et al.17 The NAQ-r is accepted as a robust tool to quantify bullying in international contexts as it combines both an operational approach to establishing bullying prevalence as well as a single-item measure of perceived victimisation.17 The first part of the NAQ-r scores how often respondents have experienced 22 types of behaviours over the past 6 months (never=1, now and then=2, monthly=3, weekly=4, daily=5). Overall scores were computed with a possible range of 22 (never experienced any behaviours) to 110 (experiencing all behaviours on a daily basis). The NAQ-r comprises three inter-related subscales of bullying (work-related, person-related and physically intimidating bullying), which enables an analysis of the prevalence of the different types of negative behaviours.
After the NAQ-r questions had been answered, a definition of workplace bullying was provided: ‘bullying at work refers to situations where one or more persons feel subjected to negative and/or aggressive behaviour from others in the workplace over a period of time and in a situation where they for different reasons are unable to defend themselves against these actions’ (adapted from Einarsen and Skogstad18). On the basis of this definition, respondents were asked whether they had witnessed bullying of other staff or colleagues and whether they had been subjected to bullying over the past 6 months. Responses were on a 5-point Likert scale (never; yes, rarely; yes, now and then; yes, several times per week; and yes, almost daily).
Bullying prevalence from the NAQ-r was established according to Leymann’s criteria as experiencing at least one negative act on a daily or weekly basis over a 6-month period.19 For both witnessed and self-report responses, bullying was identified if any of the affirmative responses, that is, very rarely, now and then, several times a week and almost daily were endorsed.
Those respondents who reported either witnessing or self-reporting bullying were asked to select the main categories of perpetrators of the bullying and those who self-reported were asked whether they had reported the behaviours, what the outcomes of reporting were and if they had not reported them, the main reasons why.
Levels of workplace demand (including factors such as workload and the work environment) and support from colleagues and non-clinical managers were measured using 17 items from the Health and Safety Executive (HSE) Management Standards Analysis tool20 asking about experiences at work over the past 6 months (never=1 to always=5 and work demands never=5 to always=1). Total scores for each of these three subscales were calculated and the scores for workplace demands reversed, so that higher scores reflected higher demands.
A χ2 goodness-of-fit test was used to compare the mixture of gender and DHB groups in the respondent group with the known distributions for the full ASMS. Differences in mean scores for the individual questions in the NAQ-r and the health and safety executive management scales between demographic, specialty and country of training (NZ vs international medical graduate (IMG)) groups were tested using one-way analysis of variance (ANOVA). The differences in the percentages experiencing the different types of bullying were compared among the groups using χ2 tests. Spearman’s correlation coefficients were used to test the associations between HSE scales and the NAQ-r scales and the frequency of witnessed and respondent’s self-reporting of being bullied. ANOVA was used to test construct validity between those scoring as a victim of bullying using self-report data and those with higher total sum scores on the NAQ-r. A two-tailed P value <0.05 was used to define statistical significance.
Qualitative data were extracted from comments from respondents who self-identified as bullied. These respondents were asked to describe the impact of bullying on their personal and professional lives. Data from the comments section were imported into NVivo pro (V.11), read through in detail and open coded. This coding resulted in 23 recurring themes that were grouped into three umbrella categories pertaining to the severity of the consequences of the bullying behaviour, namely significantly, moderately and little effects/managing, consistent with a study by Shabazz et al.16 This process followed the broad tenets of grounded theory where qualitative data are organised into emergent themes through iterative coding with the resultant themes understood to reflect the perspectives of the research participants.21 Comments selected for inclusion were those that best expressed the various themes. Comments were transcribed directly, and where sections were omitted, ellipses (‘…’) signify the break. Any words replaced or altered to preserve anonymity, tense or sense are noted within square brackets (‘[]’).
Results
Responses were received from 40.8% (n=1759) of the ASMS membership. 56.8% (n=862) were male and 43.2% (n=655) were female. A total of 242 respondents did not disclose their gender and occasionally other items were not completed. The majority of respondents were NZ trained (58.1%) and identified as NZ European (Pākehā) (59.4%). Fifty-nine specialties and subspecialties were represented in the study which were grouped into 26 major specialty categories for analyses (see online supplementary appendix 1). Some comments left in open-text boxes expressed fear of identification and this was also raised in four emails despite reassurances in the invitations to participate in the research as to the anonymous nature of the survey. Analysis was undertaken on the most complete data available for each summary or comparison and the actual numbers available are specified throughout. A full demographic summary of respondents is provided in table 1.
Table 1.
Demographic composition of survey respondents
| Gender | n | % |
| Female | 862 | 56.8 |
| Male | 655 | 43.2 |
| Not disclosed | 242 | |
| Age bracket | ||
| 30–39 | 182 | 11.6 |
| 40–49 | 577 | 36.8 |
| 50–59 | 545 | 34.8 |
| 60–69 | 235 | 15.0 |
| 70 and over | 29 | 1.8 |
| Not disclosed | 191 | |
| Ethnicity categories | ||
| NZ European/Pākehā | 919 | 59.4 |
| Māori/Pasifika (Samoan, Cook Island Māori, Tongan, Fijian) | 31 | 2.0 |
| Asian/Indian (Southeast Asian, Chinese, Indian, other Asian) | 165 | 10.7 |
| European/other European | 315 | 20.4 |
| Other (Middle Eastern, Latin American/Hispanic, African, ‘other’) | 117 | 7.6 |
| Not disclosed | 212 | |
| Country of primary medical qualification | ||
| New Zealand | 888 | 58.1 |
| International medical graduate | 638 | 41.9 |
| Not disclosed | 230 | |
| Medical specialty | ||
| Anaesthesia | 199 | 14.3 |
| Cardiology | 30 | 2.1 |
| Dentistry | 31 | 2.2 |
| Emergency medicine | 94 | 6.7 |
| General medicine | 73 | 5.2 |
| General practice | 35 | 2.5 |
| General surgery | 48 | 3.4 |
| Geriatric medicine | 38 | 2.7 |
| Intensive care medicine | 31 | 2.2 |
| Nephrology | 18 | 1.3 |
| Obstetrics/gynaecology | 56 | 4.0 |
| Occupational and public health medicine | 18 | 1.3 |
| Oncology | 28 | 2.0 |
| Ophthalmology | 27 | 1.9 |
| Orthopaedic surgery | 48 | 3.4 |
| Other | 30 | 2.1 |
| Otolaryngology | 21 | 1.5 |
| Paediatrics | 113 | 8.1 |
| Palliative medicine | 24 | 1.7 |
| Pathology | 29 | 2.1 |
| Psychiatry | 178 | 12.8 |
| Radiology | 75 | 5.4 |
| Respiratory medicine | 19 | 1.4 |
| Rural hospital medicine | 18 | 1.3 |
| Specialist internal medicine other | 71 | 5.1 |
| Specialist surgery other | 44 | 3.2 |
| Not disclosed | 363 |
NZ, New Zealand.
bmjopen-2017-020158supp001.pdf (41KB, pdf)
The χ2 goodness-of-fit tests indicated a slight over-representation of women in the sample (43% compared with 38% in the ASMS) and the over-representation of a single DHB in the sample (6% compared with 4%). Apart from these two examples, the respondents were generally representative of the full ASMS membership
Prevalence of negative behaviours
The overall mean NAQ-r score was 31.4, with a maximum score of 102. Based on the NAQ-r, 93% (n=1575) of respondents had experienced at least one negative behaviour at least once over the last 6 months and 38.1% (n=645) had experienced at least one negative behaviour on a daily or weekly basis. 24.9% had experienced two negative behaviours on a weekly or daily basis and 6.7% (n=114) had experienced at least five on a daily or weekly basis.
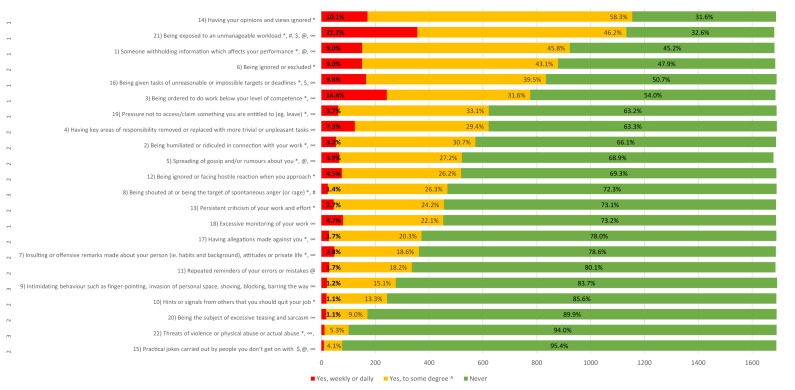
Analysis of the NAQ-r subscales revealed negative work-related behaviours (49.9%) were more prevalent and occurred on a more regular basis than negative person-related (25.3%) or physically intimidating behaviours (16.7%). The most prevalent work-related behaviours experienced on a daily or weekly basis were being exposed to an unmanageable workload (21.2%) and being ordered to do work below your level of competence (14.4%). Being ignored or excluded and having key areas of responsibility removed or replaced with more trivial or unpleasant tasks were the most frequently experienced negative person-related behaviours occurring on a weekly or daily basis (9% and 7.3%, respectively). While infrequent, 24 respondents (1.4%) had experienced being shouted at or spontaneous anger on a weekly or daily basis and 11 (0.7%) had experienced threats of violence or actual abuse at the same frequency. Detailed scores for all 22 NAQ-r behaviours are presented in figure 1.
Figure 1.
Frequency and percentage of respondents experiencing negative behaviours over the past 6 months (Negative Acts Questionnaire (revised) (NAQ-r)). Subscale questions: 1=work related bullying, 2=person-related bullying, 3=physically intimidating bullying. ^Collapsed frequencies of ‘now and then’ and monthly. *Behaviours with significant variance by age group. #Behaviours with a significantly higher prevalence for female respondents compared with male respondents. $Behaviours with significant variance by ethnicity. @Behaviours with significantly higher prevalence for IMG respondents compared with New Zealand (NZ)-trained respondents. ∞Behaviours with significant variance by medical specialty. Red colour indicates yes, weekly or daily; yellow colour indicates yes, to some degree; green colour indicates never.
There was no significant difference in the overall mean NAQ-r score by gender (female mean=32.7, male mean=32.3) although women (mean 3.72) had a significantly higher mean NAQ-r subscale score for physically intimidating behaviour than men (mean 3.55), P=0.011. A higher proportion of female respondents experienced at least one or more negative behaviours than their male counterparts (94.8% vs 91%, P=0.004). Specific questions in the NAQ-r for which women had a higher mean score are noted with # in figure 1.
There were significant differences in mean scores by age group (P<0.001). Respondents aged 40–49 and 50–59 had higher than average NAQ-r scores and further analysis of frequency scores found respondents aged 40–49 and 50–59 also experienced significantly higher prevalence of bullying behaviours than other age groups. Specific questions in the NAQ-r for which there was significant variance by age group are noted with * in figure 1.
Ethnicity was significantly associated with experiencing one or more negative behaviours (P=0.037) with Asian ethnicities reporting the lowest prevalence (89.1%) overall. There were no significant associations of ethnicity with overall or subscale mean scores but some ethnicities experienced higher levels of some behaviours noted by $ in figure 1. IMGs reported significantly higher mean scores for person-related bullying than NZ-trained specialists (16.7 vs 15.9, P=0.012) and reported higher levels of experiencing five behaviours (noted with @ in figure 1) than NZ-trained specialists.
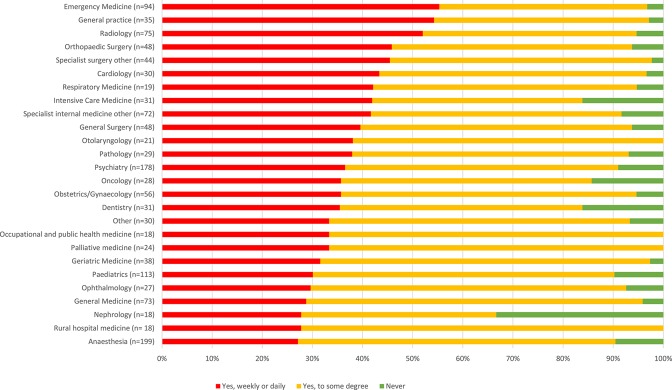
There were significant differences among the medical specialties in the NAQ-r overall mean (P=0.032) and subscale scores as well as prevalence of negative behaviours (P=0.006). Specialists in emergency medicine and general surgery reported the two highest mean overall NAQ-r scores (35.8 and 35.7, respectively). Respondents from emergency medicine had the highest mean subscale scores for work-related and physically intimidating bullying behaviours (14.4 and 4.2, respectively) as well as the highest prevalence of bullying behaviours experienced on a weekly or daily basis (55.7%). Behaviours with significant effects of medical specialty are noted with ∞ in figure 1. Prevalence of experiencing at least one negative behaviour (NAQ-r) by medical specialty is summarised in figure 2.
Figure 2.
Prevalence of experiencing at least one negative behaviour (Negative Acts Questionnaire (revised) (NAQ-r)) by medical specialty. Red colour indicates yes, weekly or daily; yellow colour indicates yes, to some degree; green colour indicates never.
Overall prevalence of self-report and witnessed bullying
37.2% (n=606) self-reported having been bullied ‘to some degree’ (ie, from very rarely to almost daily) over the last 6 months. 2.5% (n=40) reported that they had been bullied either several times a week or almost daily. The corresponding figures for witnessing bullying were almost twice as high with 67.5% (n=1109) reporting that they had witnessed colleagues being bullied to some degree (ie, from very rarely to almost daily) over the last 6 months. 4.7% (n=78) reported that they had witnessed bullying either several times a week or almost daily. Women were significantly more likely to self-report bullying compared with their male counterparts (39.9% vs 32.3%, P=0.002). There were also significant differences in rates of self-report ‘to some degree’ (P=0.033) and significant differences in frequency of witnessing bullying (P=0.001 ‘to some degree’ and ‘weekly or daily’) by medical specialty (online supplementary figures a and b). There were no other significant differences in rates of self-report or witnessed bullying rates by other demographic variables. Prevalence data for self-report and witnessed bullying are summarised overall and by gender in table 2.
Table 2.
Prevalence of self-report and witnessed bullying with significant variance by demographic variable
| Self-report as bullied | Witnessed bullying of other staff or colleagues | |||||||||||
| No | Yes, to some degree | Yes, weekly or daily | No | Yes, to some degree | Yes, weekly or daily | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Overall | 1022 | 62.8 | 606 | 37.2 | 40 | 2.5 | 535 | 32.5 | 1109 | 67.5 | 78 | 4.7 |
| Female | 392 | 60.1 | 260 | 39.9* | 17 | 2.6 | 199 | 30.4 | 455 | 69.6 | 34 | 5.2 |
| Male | 583 | 67.7 | 278 | 32.3* | 21 | 2.4 | 299 | 34.8 | 561 | 65.2 | 40 | 4.7 |
Totals for each block differ because of missing data.
*P<0.001.
Associations with bullying, workplace demands, peer and non-clinical manager support
Non-parametric Spearman’s correlations revealed significant associations between the three HSE subscales, with levels of workplace demands increasing with decreasing levels of peer and managerial support (all correlations >0.28). There was a strong association between being exposed to higher workplace demands and increasing overall NAQ-r and NAQ-r subscale scores. Low levels of peer support were also strongly associated with higher overall NAQ-r and person-related bullying scores. Similarly, high levels of workplace demands were associated with higher levels of work-related bullying. Witnessing and self-reporting bullying were also associated with high workplace demands, low levels of peer support and low levels of managerial support as detailed in table 3.
Table 3.
Correlations between bullying measures and levels of workplace demands, peer and managerial support
| Correlations (Pearson correlation) | Level of workplace demands | Level of peer support | Level of non-clinical managers’ support |
| NAQ-r score | 0.464* | −0.574* | −0.463* |
| Physically intimidating bullying subscale score | 0.246* | −0.319* | −0.214* |
| Person-related bullying subscale score | 0.284* | −0.565* | −0.408* |
| Work-related bullying subscale score | 0.608* | −0.491* | −0.464* |
| Frequency of witnessing bullying | 0.229* | −0.315* | −0.253* |
| Frequency of self-reporting as bullied | 0.379* | −0.461* | −0.379* |
*All correlations are statistically significant at P<0.001.
NAQ-r, Negative Acts Questionnaire (revised).
Perpetrators and reporting of bullying behaviour
Of the 606 respondents who self-reported as bullied, other senior medical or dental staff were the most commonly cited perpetrators (52.5%) followed by non-clinical managers (31.8%) and clinical leaders (24.9%). The largest share of respondents reported that perpetrators were mainly male (36.8%) followed by those reporting equal numbers of men and women (35.5%).
30.4% (n=182) of those who self-reported as bullied formally reported the behaviour experienced. Of the 415 who did not report it, 407 provided reasons why. Table 4 details the most common reasons for not reporting. Notably, 43.5% felt that they would not be supported and 42% felt that reporting would make the situation worse.
Table 4.
Summary of reasons for not reporting bullying behaviour
| Why did you not report this behaviour?* | n | % |
| I was concerned that reporting the issue would make the situation worse. | 171 | 42.0 |
| I did not know who to report the issue to. | 45 | 11.1 |
| I felt I would not be supported if I reported the issue. | 177 | 43.5 |
| I was concerned about the impact that reporting the issue would have on my career. | 112 | 27.5 |
| The behaviour stopped and has not recurred. | 26 | 6.4 |
| The person I would normally report the issue to is the perpetrator. | 115 | 28.3 |
| Other (please specify) | 127 | 31.2 |
*Respondents could select more than one reason.
Explanations in the ‘other’ section expressed choosing not to report due to the behaviours being normalised: ‘I have come to accept this as the culture of the institution I feel I cannot trust the people who I could report.’ Others noted that the behaviour was something that they accepted as simply part of the job, ‘[aggressive] behaviour from upset parents has always been part of my job. It makes me feel shaken and I generally would have a cup of tea with a colleague afterwards. Never considered a formal report.’ Some simply stated that ‘I have more important things to worry about.’
Of the 182 who reported their bullying experience, 30.8% noted that the issue was not addressed and the behaviour continued, while 20.9% stated that the issue was addressed but not resolved and the behaviour continued. ‘Other’ outcomes (28.6%) included the issue being currently under review as well as people noting either a dismissal of the reporting, “I mentioned to head of department and he said, ‘yes they can be difficult sometimes’” as well as extreme consequences such as resigning or changing roles, ‘[eventually] I resigned and moved to be as far away from possible from the person. Restructuring later occurred and that person has now left. The service has been traumatised and is still healing from his 2 years of reign.’
Consequences of bullying on professional and personal lives
The effects of bullying, as reported by those who self-identified as having been bullied and chose to leave comments (n=563), were many and varied with ‘moderate’ consequences the most frequently reported. Respondents described feeling disillusioned, isolated, fearful and lacking in trust. Others detailed the significant personal and professional costs of bullying including depressive episodes and feelings of burnout. Some detailed feelings of distress and upset when their stress and frustration spilled over from work into their interactions with partners or children. Thirty-one comments described bullying as significantly circumscribing their ability to innovate or improve clinical service delivery due to poor communication and a tendency to resort to defensive medical practice. Some felt that this ultimately affected the timeliness and quality of patient care: ‘[it] makes you reluctant to engage a second time to discuss patient management. A delay in or wrong decision to discharge is then made. Over-monitoring by a non-clinical [manager] then has you working defensively. Add abuse from patients for not meeting expectations and weekly passive aggressive reminders that targets are not being met….’ A full summary of themes and illustrative comments is detailed in table 5.
Table 5.
Summary of themes and illustrative comments
| Themes (Note: Comments could reference multiple themes simultaneously.) |
Illustrative comments |
Minor consequence/coping:
|
‘Recognise the behaviour and dismiss it and remain calm… Does not affect me and I do not try to defend against allegations made. Have had many years of practice.’ |
Moderate consequences:
|
‘For the first time in 19 years working as a doctor, I dislike coming to work. I am anxious and sleep poorly. I am struggling in my personal relationships because I feel like I should be able to cope but don’t seem to be able to…I often feel unsafe now at work, and I worry that my experience here will have a negative impact on future positions I apply for. I am considering leaving the field of medicine because of my experience at this particular DHB.’ |
| ‘As the person doesn’t speak, communicate or interact with [me] and hasn’t for 2.5 years. I am at a loss as to how to fulfil my role…[I’m] basically guessing what to do. Plus [I] have been undermined and humiliated and disenfranchised and the staff I give clinical guidance to know it. I have lost confidence in myself and in my professional abilities.’ | |
| ‘… Bullying wrecks a whole week. It leads to self-doubt and second guessing. It takes a long time to recover from. It is poorly recognised. It is difficult as an SMO to call out on bullying as it is a sign of weakness. Therefore, many of us put up with it especially in a system where we are overworked with unrealistic schedules and no hope of making an improvement.’ | |
| ‘You pull back and do the bare minimum to keep a service running. Bringing the behaviour to the attention of managers further up the pecking order has made no difference. Patient health is at risk.’ | |
| ‘Professionally it has affected my enjoyment of my job and I am considering moving to another DHB as I feel that I am so intimidated at times that I am unable to do my job to the best of my abilities. At times it is intolerable. The behaviour has caused me stress which has spilled over into my personal life too.’ | |
Significant consequences:
|
‘I fear going to work. I feel as if I am being watched the whole time. I feel as though it doesn’t matter how good my clinical work is, that my manager and [clinical director] will find a way to put a negative spin on it… I have lost confidence in myself as a doctor and a person. I feel disempowered… I am very anxious about work. This affects my sleep, which makes me worry more… I find it harder to trust people in general, and am more defensive…I am less patient with my children, as I feel so stressed. It feels like being trapped in an abusive relationship… I often dream of leaving. I often feel I have wasted my life, investing so much of myself in my work, when it is not valued by my seniors, even though patients value what I do.…I see patient care compromised, and the quality of the service being eroded. …I feel ethically compromised every day.’ |
Discussion
This study reports the first multicentre multispecialty study into the prevalence of workplace bullying in a senior medical workforce across an entire country, including the sources of such behaviour and rates of and barriers to reporting. It extends existing research by examining associations between bullying prevalence and perceptions of workload and peer and managerial support. It addresses the extensive methodological debate about how to measure workplace bullying, including both ‘inside’, or self-report measures and ‘outside’, or peer report methods.22 It also combines quantitative and qualitative data, with analysis of the latter, describing personal and professional impacts of bullying, further adding to the strengths of this study. Other approaches, such as focus group discussions, or critical incident analysis would not be feasible on a large scale.
Over a third of this sample of senior doctors and dentists working in NZ’s public health system are regularly exposed to a wide range of negative behaviours at work. Over a third self-report as being bullied and over two-thirds report witnessing bullying of colleagues. The results overall suggest exposure to some degree of negative behaviour is ubiquitous in this senior medical workforce, with work-related bullying especially common.
The strong associations between decreasing peer and managerial support, increasing workplace demands and increasing frequencies of all measures of bullying are of note. These findings contribute to the literature which views bullying as a phenomenon with multiple antecedents, and emphasise the impact of stressful workplaces with poor organisational cultures where bullying may be normalised as a coping strategy.6 9 23 Conversely, these associations suggest that having good relationships with peers and those in managerial positions might act as a buffer against bullying. It is also worth noting that even in workplaces with high stress and demands, bullying is not always an inevitable consequence.12
The application of the NAQ-r enables both an assessment of the types of behaviours most commonly experienced as well as the frequency of the bullying experienced in a manner that provides for international comparisons as well as highlighting specific issues requiring action. Overall NAQ-r prevalence in this study is higher than the rates of bullying reported in Australasian studies applying the same methodology.14 24 The NAQ-r mean score and 37% self-report prevalence scores were also higher than in other international studies using the NAQ-r such as Carter et al.23 The difference in the rates of self-reported (37%) and witnessed bullying rates (67.5%) is consistent with trends reported in other studies.3 25 This differential may be ascribed to a reluctance by individuals to self-identify as a ‘victim’,26 but it is equally possible that some respondents may witness the same person being bullied thus potentially over-reporting bullying prevalence.
The statistically significant differences in NAQ-r mean scores and self-report bullying rates by age, medical specialty, and for some of the subscale scores, gender, ethnicity, medical specialty and country of medical training, are concerning. They suggest that while bullying is experienced across the board, there are pockets of higher prevalence of certain behaviours for specific groups of individuals that warrant further investigation and organisational action. For example, the finding that IMGs are more likely to experience person-related bullying should be of concern given NZ’s high reliance on IMGs.27
The findings from this study confirm the impression given by the existing literature that certain medical specialties experience higher prevalence of bullying than others. The high self-report prevalence (47.9%) and NAQ-r scores for specialists in emergency medicine are, methodological differences notwithstanding, higher than the 34.5% bullying prevalence reported by the Australasian College of Emergency Medicine which surveyed all fellows of the college, including trainees.28 At the time of both surveys, many emergency departments around the country were reporting higher than usual demands on their services over the winter period.29 In light of broader workforce pressures including poor resourcing, staffing shortages and high levels of burnout in this workforce,30 it is not hard to conceive that negative interpersonal interactions, particularly if they are already normalised in the workplace, may escalate as a way to ‘get things done’ in times of significant stress.31
Also consistent with studies was the finding that other senior medical staff were the main perpetrators of self-reported and witnessed bullying behaviour (52.5% overall). These findings highlight the significant problem of peer-to-peer bullying in this section of the medical workforce. Little research to date has revealed the extent to which other senior medical and dental staff bullying each other and this finding is, while not entirely unexpected, of great concern.
The low rates of reporting, largely due to the fear of exacerbating the situation or not receiving support, suggest that considerable effort is still required to facilitate better reporting systems and procedures for handling bullying complaints. It is of further concern that, for the majority of those who did formally report bullying behaviour, the issue was not addressed and the behaviour continued. This suggests that despite the rhetoric, much work remains to be done to improve the outcomes for those who do choose to report.
These findings have considerable relevance for those charged with improving the working conditions of this vital component of the medical workforce. Previous research has revealed a correlation with sickness absence, although the direction of causation is unclear.32 A Finnish study found that those who experienced bullying were more likely to use sedatives and hypnotics, with potential consequences for their performance.33 The same study found greater levels of stress in those who were the victims of bullying and those who observed it, compared with those in workplaces without bullying. However, they also have implications for those concerned for the quality of patient care.34 As explicated in grim detail in the qualitative data, bullying has far-reaching consequences that do not stop at the individual. Working in an environment where bullying is both witnessed and experienced has clear consequences for the manner in which medical teams are able to function16 35 and deliver the services on which public health systems depend.2 36
The results of this survey indicate a need for a comprehensive series of interventions to address problematic behaviours and to consider the broader implications of growing workloads, under-resourcing and understaffing for the health and well-being of this medical workforce and their patients.
It is possible that the topic of the survey may have motivated those who have experienced bullying to respond, resulting in responder bias. Nevertheless, the primary author received a number of emails from individuals who self-identified as bullied who chose not to participate in the study for a variety of reasons including fear of identification. Thus, research in this area may contradict the common conception that responder bias favours those affected by the issue at hand. Regardless, given the moderate response rate, this study cannot be presumed to be representative of the views or experiences of the senior medical workforce in NZ as a whole. The cross-sectional design of the survey also means that causal relationships cannot be inferred and any discussion of the associations between demographic and other factors is not meant to imply causality or direction.
bmjopen-2017-020158supp002.jpg (564.4KB, jpg)
bmjopen-2017-020158supp003.jpg (516.5KB, jpg)
Supplementary Material
Acknowledgments
Thanks to the members of the ASMS who participated in this research.
Footnotes
Contributors: The research was designed and conducted by CNLC, statistical analysis was performed by CMAF, and analysis and contributions were received from MB and MM. All authors edited and revised the final submission and signed off on the final version.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: The survey was deemed outside of scope for ethical review by the New Zealand Health and Disability Ethics Committee (HDEC) due to the anonymous nature of the survey and the type of data requested.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Jamieson J, Mitchell R, Le Fevre J, et al. Bullying and harassment of trainees: an unspoken emergency? Emerg Med Australas 2015;27:464–7. 10.1111/1742-6723.12465 [DOI] [PubMed] [Google Scholar]
- 2. Paice E, Smith D. Bullying of trainee doctors is a patient safety issue. Clin Teach 2009;6:13–17. 10.1111/j.1743-498X.2008.00251.x [DOI] [Google Scholar]
- 3. Quine L. Workplace bullying in NHS community trust: staff questionnaire survey. BMJ 1999;318:228–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hogh A, Conway PM, Grynderup MB, et al. Negative acts at work as potential bullying behavior and depression: examining the direction of the association in a 2-year follow-up study. J Occup Environ Med 2016;58:e72–9. 10.1097/JOM.0000000000000622 [DOI] [PubMed] [Google Scholar]
- 5. Kivimäki M, Virtanen M, Vartia M, et al. Workplace bullying and the risk of cardiovascular disease and depression. Occup Environ Med 2003;60:779–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Einarsen S. Harassment and bullying at work: a review of the scandinavian approach. Aggress Violent Behav 2000;5:379–401. 10.1108/IJOTB-13-02-2010-B004 [DOI] [Google Scholar]
- 7. Einarsen S, Raknes BI. Harassment in the workplace and the victimization of men. Violence Vict 1997;12:247. [PubMed] [Google Scholar]
- 8. Matthiesen SB, Einarsen S. Bullying in the workplace: definition, prevalence, antecedents and consequences. Int J Org Theory Behav 2010;13:202 10.1108/IJOTB-13-02-2010-B004 [DOI] [Google Scholar]
- 9. Salin D. Ways of explaining workplace bullying: a review of enabling, motivating and precipitating structures and processes in the work environment. Human Relations 2003;56:1213–32. [Google Scholar]
- 10. Fink-Samnick E. The new age of bullying and violence in health care: part 2: advancing professional education, practice culture, and advocacy. Prof Case Manag 2016;21:114–26. quiz E1-2 doi 10.1097/NCM.0000000000000146 [DOI] [PubMed] [Google Scholar]
- 11. Hoel H, Salin D. 10 organisational antecedents of workplace bullying. Bullying and emotional abuse in the workplace. 2003;203. [Google Scholar]
- 12. Bradley V, Liddle S, Shaw R, et al. Sticks and stones: investigating rude, dismissive and aggressive communication between doctors. Clin Med 2015;15:541–5. 10.7861/clinmedicine.15-6-541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Knowles R, Szoke H, Campbell G, et al. Expert advisory group on discrimination, bullying and sexual harassment advising the royal australasian college of surgeons report to the Royal Australasian College of Surgeons. 2015.
- 14. Ling M, Young CJ, Shepherd HL, et al. Workplace bullying in surgery. World J Surg 2016;40:2560–6. 10.1007/s00268-016-3642-7 [DOI] [PubMed] [Google Scholar]
- 15. Venkatesh B, Corke C, Raper R, et al. Prevalence of bullying, discrimination and sexual harassment among trainees and Fellows of the College of Intensive Care Medicine of Australia and New Zealand. Crit Care Resusc 2016;18:230. [PubMed] [Google Scholar]
- 16. Shabazz T, Parry-Smith W, Oates S, et al. Consultants as victims of bullying and undermining: a survey of Royal College of Obstetricians and Gynaecologists consultant experiences. BMJ Open 2016;6:e011462 10.1136/bmjopen-2016-011462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Einarsen S, Hoel H, Notelaers G. Measuring exposure to bullying and harassment at work: validity, factor structure and psychometric properties of the negative acts questionnaire-revised. Work Stress 2009;23:24–44. 10.1080/02678370902815673 [DOI] [Google Scholar]
- 18. Einarsen S, Skogstad A. Bullying at work: epidemiological findings in public and private organizations. Eur J Work Organ Psy 1996;5:185–201. 10.1080/13594329608414854 [DOI] [Google Scholar]
- 19. Leymann H. Mobbing and psychological terror at workplaces. Violence Vict 1990;5:119–26. [PubMed] [Google Scholar]
- 20. HSE. Health and safety executive management standards tool. Secondary Health and safety executive management standards tool. 2017. http://www.hse.gov.uk/stress/standards/index.htm.
- 21. Charmaz K. Grounded theory as an emergent method : Hesse-Biber SN, Leavy P, Handbook of emergent methods. New York: The Guilford Press, 2008:155–72. [Google Scholar]
- 22. Cowie H, Naylor P, Rivers I, et al. Measuring workplace bullying. Aggression and Violent Behavior 2002;7:33–51 https://doi.org/. [Google Scholar]
- 23. Carter M, Thompson N, Crampton P, et al. Workplace bullying in the uk nhs: a questionnaire and interview study on prevalence, impact and barriers to reporting. BMJ open 2013;3:e002628. [Google Scholar]
- 24. Bentley T, Catley B, Cooper-Thomas H, et al. Understanding stress and bullying in new zealand workplaces: final report to oh&s steering committee. Wellington, New Zealand, 2009. [Google Scholar]
- 25. Steadman L, Quine L, Jack K, et al. Experience of workplace bullying behaviours in postgraduate hospital dentists: questionnaire survey. Br Dent J 2009;207:379–80. 10.1038/sj.bdj.2009.901 [DOI] [PubMed] [Google Scholar]
- 26. Mikkelsen EG, Einarsen S. Bullying in danish work-life: prevalence and health correlates. Eur J Work Organ Psy 2001;10:393–413. [Google Scholar]
- 27. Zealand MCoN. The new zealand medical workforce in 2013 and 2014. Wellington, New Zealand: Medical Council of New Zealand, 2016. [Google Scholar]
- 28. ACEM. Acem membership consultation paper on discrimination, bullying and sexual harassment. Australia: Australasian College for Emergency Medicine, 2017. [Google Scholar]
- 29. Weber A. Winter ills fill hospitals: ’we simply haven’t got the space'. Secondary winter ills fill hospitals: ’we simply haven’t got the space'. 2017. http://www.radionz.co.nz/news/national/335368/winter-ills-fill-hospitals-we-simply-haven-t-got-the-space.
- 30. Chambers CN, Frampton CM, Barclay M, et al. Burnout prevalence in New Zealand’s public hospital senior medical workforce: a cross-sectional mixed methods study. BMJ Open 2016;6:e013947 10.1136/bmjopen-2016-013947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bentley TA, Catley B, Cooper-Thomas H, et al. Perceptions of workplace bullying in the New Zealand travel industry: prevalence and management strategies. Tourism Management 2012;33:351–60. 10.1016/j.tourman.2011.04.004 [DOI] [Google Scholar]
- 32. Kivimäki M, Elovainio M, Vahtera J. Workplace bullying and sickness absence in hospital staff. Occup Environ Med 2000;57:656–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vartia MA. Consequences of workplace bullying with respect to the well-being of its targets and the observers of bullying. Scand J Work Environ Health 2001;27:63–9. [DOI] [PubMed] [Google Scholar]
- 34. Rosenstein AH, O’Daniel M. Impact and implications of disruptive behavior in the perioperative arena. J Am Coll Surg 2006;203:96–105. 10.1016/j.jamcollsurg.2006.03.027 [DOI] [PubMed] [Google Scholar]
- 35. Roche M, Diers D, Duffield C, et al. Violence toward nurses, the work environment, and patient outcomes. J Nurs Scholarsh 2010;42:13–22. 10.1111/j.1547-5069.2009.01321.x [DOI] [PubMed] [Google Scholar]
- 36. Wild JR, Ferguson HJ, McDermott FD, et al. Undermining and bullying in surgical training: a review and recommendations by the association of surgeons in training. Int J Surg 2015;23 Suppl 1:S5–9. 10.1016/j.ijsu.2015.09.017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-020158supp001.pdf (41KB, pdf)
bmjopen-2017-020158supp002.jpg (564.4KB, jpg)
bmjopen-2017-020158supp003.jpg (516.5KB, jpg)