Abstract
Objectives
In England, many hypertensives are not detected by primary medical care. Higher detection is associated with lower premature mortality. We aimed to summarise recent evidence on detection and interventions to improve detection in order to inform policies to improve care.
Design
Data sources: systematic review of articles published since 2000. Searches of Medline and Embase were undertaken. Eligibility criteria: published in English, any study design, the setting was general practice and studies included patients aged 18 or over. Exclusion criteria: screening schemes, studies in primary care settings other than general practice, discussion or comment pieces. Participants: adult patients of primary medical care services. Synthesis: study heterogeneity precluded a statistical synthesis, and papers were described in summary tables.
Results
Seventeen quantitative and one qualitative studies were included. Detection rates varied by gender and ethnic group, but longitudinal studies indicated an improvement in detection over time. Patient socioeconomic factors did not influence detection, but living alone was associated with lower detection. Few health system factors were associated with detection, but in two studies higher numbers of general practitioners per 1000 population were associated with higher detection. Three studies investigated interventions to improve detection, but none showed evidence of effectiveness.
Limitations
The search was limited to studies published from 2000, in English. There were few studies of interventions to improve detection, and a meta-analysis was not possible.
Conclusions and implications
Levels of detection of hypertension by general practices may be improving, but large numbers of people with hypertension remain undetected. Improvement in detection is therefore required, but guidance for primary medical care is not provided by the few studies of interventions included in this review. Primary care teams should continue to use low-cost, practical approaches to detecting hypertension until evidence from new studies of interventions to improve detection is available.
Keywords: hypertension, detection, primary care, public health
Strengths and limitations of this study.
The review employed a systematic approach to identify relevant articles and summarise the findings.
Papers published before the year 2000 and those published in languages other than English were excluded.
A meta-analysis was not undertaken because of the heterogeneity of the study questions and outcomes, the blood pressure thresholds used and patients included. There were very few studies of interventions to improve detection.
Introduction
Hypertension is a common risk factor for cardiovascular mortality. In 2015, an estimated 874 million adults worldwide had a systolic blood pressure of 140 mm Hg or more.1 As in many countries, England has a national strategy to improve the detection and management of hypertension,2 and the proportion of adults with untreated hypertension was 13% in 2011 compared with 21% in 1994.3 In the 2015 Health Survey for England, 26.1% of women and 30.8% of men aged 16 or over had evidence of hypertension,4 although only 13.8% of the population were recorded on GP hypertension registers in 2015–2016.5 Failure to detect hypertension continues to influence mortality rates, higher proportions of the population on general practice hypertension registers being associated with lower premature mortality.6 A scheme to offer health (including blood pressure) checks to people aged 40–75 without an existing cardiovascular condition was launched in primary care in 2009, but its impact has been modest,7 a finding consistent with a review of randomised trials of similar interventions that failed to find a reduction in mortality.8 Public Health England recently launched an initiative to reduce heart attacks and strokes through better detection of hypertension, raised cholesterol and atrial fibrillation,9 and National Health Service (NHS) Right Care has developed a prevention pathway that includes promotion of real-time audits for general practices to identify gaps in detection and opportunities for improvement.10
In England, GPs have for more than 35 years been encouraged to check the blood pressure of consulting patients.11 From 2004, a financial incentive scheme (the quality and outcomes framework) has rewarded GPs for the management of people with hypertension and for recording the blood pressures of people aged 45 or above at least once within the preceding 5 years.12 Data from the outcomes framework show that 90.6% of patients aged 45 or older had a blood pressure record within the last 5 years in their general practice notes in 2015–2016.5 Since a third or more of adults with hypertension are not recorded on general practice registers, this suggests that the problem in detecting hypertension may not be primarily due to failure to check and record patients’ blood pressures, but that raised blood pressure readings are not adequately followed up until a diagnosis is confirmed, an example of diagnostic inertia (defined as a failure to diagnose disease).13 The English national guidelines on hypertension in adults recommend that in people whose blood pressure is 140/90 or above in the clinic (two or more readings advised), ambulatory blood pressure monitoring or home blood pressure monitoring should be offered.14 However, evidence about the factors explaining why these recommendations have not led to higher detection rates is limited. In one review of 53 studies, different designs of health system factors influence hypertension awareness (ie, the patient has been told they have hypertension), treatment and control.15 Only seven studies investigated levels of awareness of hypertension, and they indicated that having a routine physician or usual source of care were positively associated with awareness, but lack of health insurance was associated with lower awareness. A review of barriers to hypertension awareness, treatment and follow-up found 69 qualitative or quantitative studies undertaken in various settings.16 Patient, provider and system factors were identified as potential barriers, with knowledge, beliefs about the consequences of diagnosis and treatment, social influence and lack of time in consultations being described by providers, and lack of insurance and costs of treatment being reported by patients. Neither of these reviews specifically focused on the role of primary medical care.
Our research questions were: in adult patients of primary medical care providers, what patient or system factors are associated with the detection of hypertension and what interventions improve rates of detection in comparison with current practice? We undertook a review with specific objectives to (1) describe the proportion of patients with hypertension who are detected by primary care, (2) identify factors (patient or provider) that may influence the likelihood of hypertension being detected and (3) highlight interventions to assist primary healthcare teams improve detection among their patients. We excluded non-medical primary care providers such as pharmacies since our focus was on identifying potential approaches for improving the detection of hypertension in English primary medical care.
Methods
We defined detection of hypertension as either (1) a diagnosis of hypertension has been recorded in the general practice records, or (2) the patient is on treatment for hypertension or (3) has been told by a doctor that they have hypertension.17 The latter is often referred to as awareness of hypertension, but in this paper, we incorporate this term into the idea of detection. A review protocol has not been published.
Search strategy
We undertook searches of Medline and Embase in October 2016 for publications from 2000 onwards. The strategy was first developed in Medline and then adapted for Embase. An example search strategy is shown in online supplementary appendix, the same strategy being used in amended form for the Embase search. Search terms including delay, diagnosis, underdiagnosis, detection and awareness were used along with terms including barriers and inertia to identify relevant studies. We had limited funding for completing the review and therefore did not extend the search to before the year 2000. We were also aware that electronic health records that would facilitate large studies based on medical records were not in wide use in primary care before that date. Also, changes over time in health system structures and policies (including the definition of hypertension) could affect detection levels and factors influencing detection rates. We did not undertake a search of the grey literature.
bmjopen-2017-019965supp001.pdf (338.3KB, pdf)
Inclusion/exclusion criteria
We included studies published in English, with any design (discussion and comment pieces were excluded) that were undertaken in the setting of general practice–based primary medical care services, and involving patients aged 18 years and over. Studies undertaken in community settings other than general practice such as pharmacies or work places and studies focused on evaluation of specific screening schemes such as inviting people for a ‘health check’ were excluded, as were studies undertaken in accident and emergency departments or other hospital settings. We included studies (randomised and non-randomised) of interventions to improve detection rates, if any were found.
Review procedure
The titles and abstracts of articles identified in the searches were assessed for relevance by two reviewers independently, articles being obtained in full text for further assessment if either of the reviewers considered they were potentially relevant. These papers were assessed for inclusion in the review by two reviewers independently, differences being resolved through discussion with a third reviewer. Those papers agreed to be relevant went forward for data extraction and risk of bias assessment.
Data extraction
A data extraction form was developed and piloted in order to collect information on study design, setting, population and findings. Two reviewers independently extracted data from each article, differences being resolved through discussion. The extracted data were entered into tables. Extracted data included study subjects, country and setting, objectives, design, interventions if any, and results.
Risk of bias assessment
We included studies of different designs, and an assessment tool developed to accommodate a wide range of designs was therefore selected. We used the Mixed Methods Appraisal Tool (MMAT), which was designed to be applicable for qualitative, quantitative, randomised controlled or mixed-methods studies. For each type of study design, four criteria are given against which the studies can be assessed (only three criteria are used for mixed-methods studies). Two reviewers independently assessed the included papers, and we summarised the mean of these pairs of assessments out of the possible total score of four criteria assessed as met.18
Data synthesis
In view of the variety of study designs and the degree of heterogeneity, we undertook a descriptive analysis only, presenting the papers and the findings in summary tables. Heterogeneity affected various aspects of the studies: different research questions and outcomes; differences in BP thresholds (most used <140/90, although some used a lower threshold for diabetes and chronic kidney disease, and others used > 150/90); different patient groups—older people, younger people, people with anxiety and/or depression, people with diabetes and whole populations; different measures of hypertension detection, including awareness and treatment, in addition to a record of the diagnosis; different designs—cross-sectional and longitudinal designs in the observational studies, qualitative research and intervention studies with different interventions. Consequently, a quantitative synthesis was not attempted.
Results
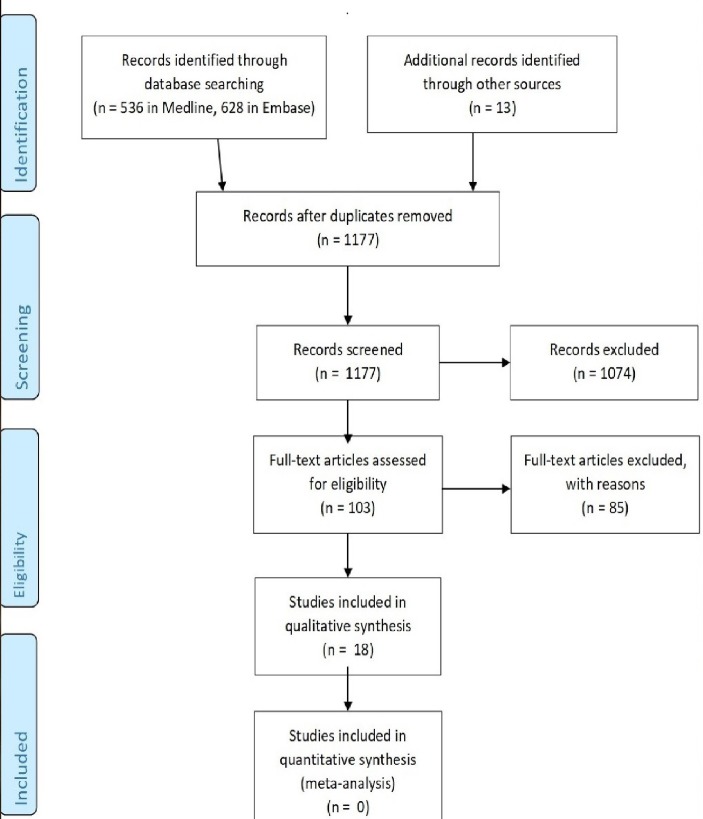
The bibliographic searches identified 1177 articles, of which 103 were assessed as potentially relevant, with 18 being included after assessment of the full-text manuscripts (see the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram, figure 1). The most common reasons for exclusion were that studies had not been undertaken in general practice settings, or that they involved assessments of health system screening schemes such as the NHS health check scheme.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2009 flow diagram.
The studies had been undertaken in a narrow range of countries: UK eight, USA six, Spain two, and one each in Australia and San Marino. Fifteen were observational, of which one was a qualitative study of barriers to hypertension detection19–33 (table 1). Three studies were evaluations of interventions to improve detection, two of these being randomised trials34–36 (table 2). The mean MMAT rating of the observational studies was 3.5 and the mean MMAT rating of the intervention studies was 2.7 (see table 3). Of the 17 quantitative studies, 9 used data from electronic health records, 2 used administrative data, 3 involved secondary analyses of existing health surveys and 3 used other sources of data (tables 4 and 5).
Table 1.
Studies of levels of detection and factors associated with detection
| Paper | Country | Setting | Design | Sample |
| Banerjee et al 19 | USA | Primary care clinics | Cross-sectional analysis of electronic health records | 251 590 adults with at least two clinic visits in a 3-year period |
| Bankart et al 20 | England | 8052 general practices | Cross-sectional analysis of routinely collected administrative data about practices | 13.3% of patients on general practice hypertension registers |
| de Burgos-Lunar et al 21 |
Spain | 21 health centres in Madrid | Retrospective cohort study, using electronic health records | 8074 adults with diabetes who, during the study period, met the criteria for hypertension |
| Byrd et al 22 | USA | 3 HMOs | Longitudinal analysis, using a hypertension registry derived from electronic health records, of time to detection of hypertension | 168 630 patients |
| Howes et al 23 | Australia | General practice | Qualitative study of barriers to diagnosing hypertension | 30 clinicians in six focus groups |
| Johnson et al 24 | USA | Multidisciplinary academic group practice | Using electronic medical records, a retrospective analysis of time from meeting hypertension diagnosis criteria to antihypertensive treatment | 10 022 patients aged >18 years with incident hypertension |
| MacDonald and Morant25 | UK | 326 general practices | Cross-sectional analyses for three separate years of electronic health records | Up to 2.58 million patients aged >16 years |
| Mancia et al 26 | San Marino | Nine general practitioners | Cross-sectional phase identifying people with raised BP followed by 2 years of longitudinal follow-up, using an ad hoc designed database | Patients aged 40–75 years consulting over an 8-month period |
| Nazroo et al 27 | England | The general population | Analysis of 4 years’ data from a national household survey (Health Survey for England) | 23 987 adults |
| Pallares-Carratalá et al 28 | Spain | Primary care health centres in one region | Cross-sectional observational study, using electronic health records | 48 605 patients without hypertension |
| Patel et al 29 | UK | Patients registered with general practices in 24 British towns | Cross-sectional study of people randomly selected from general practice lists, patients undergoing an examination including BP measurement | 3059 women and 3007 men aged 60–79 years |
| Shah and Cook30 | England | The general population | Analysis of 2 year’s data from a national household survey (Health Survey for England) | Aged over 25, with raised BP or on antihypertensive treatment (2208 men, 2811 women) |
| Soljak et al 31 | England | 351 local authorities and 8372 general practices | Cross-sectional observational study, using routinely available administrative data on general practices and local government | The English population |
| Wallace et al 32 | USA | A large primary care academic group practice | Retrospective analysis of 4 years’ electronic health record data | Aged >18 with diabetes and incident hypertension |
| Zhao et al 33 | USA | Ambulatory care organisation (same place as Banerjee et al 19) | Cross-sectional study, using electronic health records | Patients aged >18 with at least two consultations in a 3-year period |
BP, blood pressure; HMO, health maintenance organisation.
Table 2.
Interventions to improve detection
| Paper | Country | Setting | Intervention | Design |
| Bonds et al 34 |
USA | 61 primary care practices in North Carolina | Multifaceted, targeting providers, involving an educational session, academic detailing, written educational materials, tools for patients, audit and feedback | RCT, data being extracted from medical charts |
| Cottrell et al 35 |
England | 425 general practices | Hypertension protocol on diagnosis implemented using telehealth: participants asked to text at least five further BP readings within a week | Uncontrolled descriptive analysis, data being extracted from the telehealth software |
| Hemming et al 36 |
England | 26 general practices | Nurse-led targeted case finding: patients at high risk invited to attend for assessment | Cluster RCT with stepped wedge design, data being extracted from electronic health records |
BP, blood pressure; RCT, randomised controlled trial.
Table 3.
Assessment of risk of bias of the included papers, using the MMAT risk assessment tool18
| Study design and studies | Assessment criteria | Total score | |||
| Qualitative | Relevant to research question | Analysis relevant for objective | Findings related to context | Findings related to researcher’s influence | |
| Howes et al 23 | y/n | y | y/n | y/n | 2.5 |
| Quantitative randomised (randomised controlled trials) | Clear description of randomisation | Clear description of allocation concealment | 80% or more outcome data | Withdrawal/drop-out less than 20% | |
| Bonds et al 34 | n | n | y | y | 2 |
| Hemming et al 36 | y | y | y | y | 4 |
| Quantitative non-randomised | Selection bias minimised | Measurements appropriate | Study groups comparable or differences accounted for | Outcome data 80% or above, or response rate 60% or above, or acceptable follow-up rate | |
| Cottrell et al 35 | n | y | n | y | 2 |
| Quantitative descriptive | Sampling strategy relevant to research question | Sample representative of the population | Measurements appropriate | Response rates 60% or above | |
| Bannerjee et al 19 | y | y | y | y | 4 |
| Bankart et al 20 | y | y | y | y | 4 |
| de Burgos-Lunar et al 21 | y | y | y | y | 4 |
| Byrd et al 22 | 3 | ||||
| Johnson et al 24 | y | y | y | y | 4 |
| MacDonald and Morant25 | y/n | y | y | y | 3.5 |
| Mancia et al 26 | n | y | y | y | 3 |
| Nazroo et al 27 | y | y | y | y/n | 3.5 |
| Pallares-Carratalá et al 28 | y/n | y | y | y | 3.5 |
| Patel et al 29 | y/n | y/n | y | y | 3 |
| Shah and Cook30 | y | y/n | y | y | 3.5 |
| Soljak et al 31 | y | y | y | y | 4 |
| Wallace et al 32 | y | y | y | y | 4 |
| Zhao et al 33 | y/n | y | y | y | 3.5 |
MMAT, Mixed Methods Appraisal Tool; n, criterion not met; y, criterion met; y/n, one assessor assigned criterion as met, the second assessor as not met.
Table 4.
Findings of observational studies of detection rates and factors associated with detection
| Paper | Thresholds for hypertension diagnosis | Outcome of interest | Detection rates | Factors associated with detection (findings with significant P values or outside 95% CIs) |
| Banerjee et al 19 | At least 2 BP readings >140/90 | % of adults (aged >18) with hypertension who had a record of the diagnosis. Two groups investigated: (1) prevalent (those with raised readings and/or on antihypertensives) and (2) incident (new cases during the study period) | 62.9% of hypertensives had a recorded diagnosis (45 365/72 206) among the prevalent group; 19.9% among the incident group (figures not given) | ORs: Prevalent hypertension: age 1.046, women 0.760, Asian 1.67, black/African American 1.979, BMI 1.064, no of BP readings >160/100 1.716Incident hypertension: age 1.030, Asian 1.577, black/African American 2.420, BMI 1.039, no of BP readings >140/90 1.195, no of BP readings >160/100 2.273. |
| Bankart et al 20 | BP >150/90 | Numbers (%) of patients on general practice hypertension registers | 13.3% of the population were on practice hypertension registers, a mean of 750 patients per practice | Predictors of numbers on registers (IRRs): deprivation 1.001, aged >65 10.04, white ethnicity 1.000007, poor health 1.013, practice list size 0.999992, GPs/1000 population 1.06, performance points for hypertension 1.006 |
| de Burgos-Lunar et al 21 | > 140/90 and >130/80 | Correct diagnosis of hypertension defined as the recording of the diagnosis during the first 6 months after the diagnostic criteria were met. Patients had type 2 diabetes; those with hypertension at the time of diagnosis of diabetes were excluded | For those meeting the diagnostic threshold of >140/90 during follow-up, 42.4% remained undiagnosed after a median follow-up of 3.6 years. Mean delay in those diagnosed 8.9 months | OR for correct diagnosis: women 1.288, age 1.006, BMI 25 to 30 1.460, >30 10.696, prior MI 0.448, not depressed 1.630, on antiplatelet treatment 1.469, BP above 140/90 2.770 |
| Byrd et al 22 | > 140/90, or >130/80 in diabetes or chronic kidney disease | Time to recognition of hypertension in patients with an inpatient or outpatient diagnosis for anxiety or depression before first elevated BP | Hypertension recognised within 12 months of second BP reading in 30.1% of those with depression and anxiety, 34.4% of those without | Median days to recognition longer among patients with anxiety and depression (45 days vs 56 days), adjusted HR 1.30 |
| Howes et al 23 | – | Barriers to detection of hypertension in general practice, as perceived by general practitioners | Barriers included: clinical uncertainty about the true BP values, mistrust of the evidence on BP management, patient age, gender and comorbidity, perceived patient attitude, clinical inertia, patient centred care, system issues | |
| Johnson et al 24 | > 140/90 | Patient and provider explanatory variables to identify barriers to hypertension management were based on a model for clinical inertia | Among 10 022 patients with hypertension, 4149 commenced medication or achieved control (41.4%); of the 2606 young adults, 451 (17.3%) received medication before receiving medication | Adjusted HRs of predictors of medication initiation included younger age 0.56, BMI 1.014, stage of hypertension 0.63, diabetes 1.44, having a low prevalence condition 1.26, adjusted clinical risk group score 1.06, no of primary care visits 1.06 |
| MacDonald and Morant25 | > 140/90 | Outcomes were the prevalence and treatment of hypertension (data for 1998, 2003 and 2006) | Among those with hypertension, treatment rates increased from 45.2% (1998), 54.4% (2003), 60.3% (2006) | The likelihood of hypertension being diagnosed and recorded was 2.0 times greater in patients who also had hypercholesterolaemia |
| Mancia et al 26 | > 140/90 | Detection and treatment of hypertension among a sample of patients undergoing a GP check-up | 62.3% of hypertensives were aware of their condition and 58.6% were on drug treatment | Awareness more common in women (67.1% vs 56.9%) and older people (74.3% aged 66 to 75, 43.7% aged 40 to 50). Treatment more common in women (63.6% vs 53.0%) and older people (71.5% aged 66 to 75 vs 39.1% aged 40 to 50) |
| Nazroo et al 27 | >140/90 | The result of BP readings related to the patient reporting they had been diagnosed as having hypertension, or were on antihypertensive medication | Undiagnosed hypertension was present in 12.6% of whites, 12.7% Irish, 9.4% Caribbeans, 9.7% Indians, 6.7% Pakistanis, 5.6% Bangladeshis, 8.2% Chinese | ORs for undiagnosed hypertension: compared with whites, Caribbean 0.43 |
| Pallares-Carratalá et al 28 | > 140/90 | New diagnoses of hypertension in a population without a diagnosis of hypertension who had at least 3 BP readings | Of 48 605 people without a diagnosis of hypertension, 6450 (13.3%) presented diagnostic inertia (raised BP without the diagnosis being made) | Variables associated with diagnostic inertia (ORs): male gender 1.46, atrial fibrillation 0.73, having a health professional 0.88, diabetes 0.93, cardiovascular disease 0.77 and older age 20.4 |
| Patel et al 29 | > 150/90 | High BP on examination, related to recall of a doctor diagnosis of hypertension, or on antihypertensive medication | Of those with raised BP on examination (949), 54.5% (517) recalled being told by a doctor they had high BP, and 35.4% (336) were on antihypertensive treatment | Socioeconomic factors, area of residence, behavioural risk factors not associated with good BP control in either sex, apart from alcohol in men (OR 0.67) |
| Shah and Cook30 | > 160/100 | Antihypertensive medication and control of hypertension among adults found to have raised BP on examination | 1119/2208 (50.7%) hypertensive men and 1620/2811 (57.6%) hypertensive women were receiving antihypertensive medication | In a fully adjusted model, ORs for treatment were as follows: men—younger age 0.39, housing tenure 0.75, living alone 0.49, smoker 0.61, heavy alcohol consumption 0.49, overweight 1.41, family history of heart disease 1.83, lack social support 1.33; women—older age 1.36, family history of heart disease 1.30, obese 1.43, lack social support 1.48 |
| Soljak et al 31 | >150/90 and >140/90 | Numbers of patients on GP hypertension registers (observed prevalence) compared with the modelled (expected) prevalence | The observed prevalence for England was 4 530 369 (8.95%), the expected was 12 356 995 (24.7%) | Regression of expected prevalence plus GP supply gave adjusted correlation coefficient of 0.407 |
| Wallace et al 32 | > 130/80 and >140/90 | The probability of receiving a diagnosis and antihypertensive medication at specific time points | Of 771 people with diabetes and incident hypertension included in the study, 315 (40.9%) received a hypertension diagnosis and 286 (37.1%) received antihypertensives. The median time to diagnosis was 1.9 months | Associations with diagnosis rates (HRs): atrial fibrillation 2.18, peripheral vascular disease 0.18, fewer primary care visits 0.93 |
| Zhao et al 33 | > 140/90 | Age-adjusted prevalence, treatment and control of hypertension | In nine ethnic groups, prevalence varied in women from 30.0% to 59.1%, treatment rates varying from 64.6% to 77.8% Figures for men: prevalence 35.9%–59.9%, treatment 57.0%–70.9% | Compared with whites, hypertension treatment was more likely in Asian Indians (women/men) OR 1.25, 1.17; Chinese 1.38, 1.34; Filipinos 1.97, 1.64; Japanese 1.32, 1.29; Vietnamese 1.40, n.s.; and Non-Hispanic Black 1.92, 1.72 |
BMI, body mass index; BP, blood pressure; GP, general practitioner; IRR, incident rate ratio; MI, myocardial infarction; n.s., not significant.
Table 5.
Findings of intervention studies
| Paper | BP thresholds | Outcome | Results | Significance |
| Bonds et al 34 | > 140/90 (> 130/90 with diabetes or renal disease) | Rates of undiagnosed hypertension | 18.1% in the intervention group, 13.6% in the controls | P=0.12 |
| Cottrell et al 35 | > 140/90 or >130/90 in diabetes or CKD | % of patients with an initial raised BP who have hypertension confirmed or not | 1166 of 1468 (79%) submitted further BP readings | – |
| Hemming et al 36 | Not stated | Measurement of BP; treatment with antihypertensives | BP was measured in 27.8% of control and 43.9% of intervention group patients 7.5% of control and 11.4% of intervention group patients started on antihypertensives |
BP measurement—P=0.022; starting antihypertensives—time-adjusted OR 7.7 (−0.1–15.5) P=0.054 |
BP, blood pressure; CKD, chronic kidney disease.
Proportion of patients with hypertension who are detected by primary care
Seven articles19 21 22 24 25 28 33 reported studies using primary care electronic health records to investigate whether people with raised blood pressure readings were followed up to confirm or refute a diagnosis of hypertension. They were undertaken in various years, and investigated different outcomes, including the proportions with evidence of hypertension (ie, consistently raised blood pressure readings) who were diagnosed (62.9% in one study19 and varying between nine ethnic groups from 57.0% in men and 64.6% in women among whites to 70.9% (men) and 77.8% (women) among Filipinos in another33).
Two other studies used different sources of data, one of which investigated people aged 40–75 years consulting general practitioners, of whom 62.3% of hypertensives were aware of their condition and 58.6% were treated.26 Another study used a national survey of a random sample of adults, reporting that 50.7% of men and 57.6% of women with hypertension were receiving antihypertensive medication.30
Changes in detection rates over time
In one study, changes in detection rates were shown to have increased from 45.2% to 60.3% over 9 years in one study.25
Diagnostic delay
Some studies also investigated diagnostic delay, that is, the first time between defined criteria for hypertension being met and a diagnosis being made. Among those whose hypertension had been diagnosed, the delay was 8.9 months in one study21 and 1.9 months in another,32 although 60% or more of hypertensive patients in these studies had not been detected during the period of follow-up. In a third study of delay, 34% of adults aged 18–39 years meeting criteria for hypertension were detected after 20 months of follow-up (44% among those 40–59 years old and 56% among those aged 60 or older).24
Factors (patient or provider) that may influence the likelihood of hypertension being detected
Of patient-related factors, the quantitative studies indicated a greater likelihood of detection in older people19 21 26 and women.21 26 28 30 33 Patient socioeconomic factors did not appear to influence detection,29 but living alone was associated with lower detection,30 and the presence of some physical health conditions was associated with higher detection rates.21 24 25 28 32 There were few differences by ethnic group, Caribbeans in a study in England being more likely to be diagnosed than whites27 and Asian Americans and non-Hispanic blacks being more likely to be treated than whites in a US study.33
Of the health system factors investigated, few were associated with detection rates, but a greater number of general practitioners per 1000 population were associated with higher detection.20 28 In the only qualitative study of barriers to detection,23 general practitioners reported several factors influencing their decisions on detecting hypertension, including uncertainty about the true blood pressure level, patient characteristics such as the age, the limited time available in consultations and distrust of the evidence on hypertension management.
Interventions to assist primary healthcare teams improve detection among their patients
Three studies investigated interventions to improve detection rates. An uncontrolled evaluation of a protocol implemented using telehealth to encourage people with isolated high blood pressure to submit further readings by text suggested this could have potential in the diagnosis of hypertension, although the study design precluded firm conclusions.35 A randomised trial of a multifaceted intervention was not effective34 and another randomised trial of targeted nurse-led case finding found an increase in blood pressure measurement, although the improvement in starting patients on antihypertensive treatment just failed to reach statistical significance.36
Discussion
In this review of studies published since 2000 on the detection of hypertension in primary medical care, we found only 18 studies from a limited range of countries. The available evidence suggests that levels of detection are around 60% and also that detection rates have improved in recent years. Delays in detection remain common, however. Several patient factors are associated with detection rates, with women, older people and those with higher levels of blood pressure and those with coexisting cardiovascular and some other conditions being more likely to be detected. There is some reassurance, therefore, in that people at greater risk of cardiovascular events are more likely to have their hypertension diagnosed. Ethnicity and socioeconomic factors are not major influences on detection, but social isolation may be associated with lower detection. The number of general practitioners per 1000 population was found in two studies from one country (England) to be associated with detection, but consistent evidence on other provider factors was limited. There was limited evidence on the potential of interventions such as use of telehealth and proactive case-finding to improve detection rates. Qualitative evidence on the barriers to detection faced by providers was likewise very limited.
We found only three studies that evaluated interventions to improve detection rates, and none of these reported a significant improvement in detection.
Strengths and limitations
This is a systematic review of recent literature on the detection of hypertension including several large studies using a range of methodologies. Although the quantitative studies were too heterogeneous to allow meta-analysis, a number of consistent findings emerged. However, our study also has a number of limitations. The search was restricted to studies published in English since 2000, and it is likely that earlier studies and those in other languages could contribute useful evidence on improving detection rates. However, the studies we did include did not draw on many references to older studies and those not published in English. Furthermore, the studies were undertaken in only a limited number of countries, and some caution is needed in assuming the findings would be replicated in other developed countries. We also acknowledge that interventions undertaken outside primary medical care, such as screening programmes, the offer of blood pressure checks to people attending pharmacies or optometrists, or in emergency departments, may improve detection rates for hypertension, but our focus was on the contribution that routine primary care itself can make. In most countries, primary medical care is the setting for the management of people with hypertension. We have not assessed the risk of publication bias, but given the descriptive nature of the majority of studies in the review, the probability of publication bias is likely to be low.
Implications
Reducing the fatal and non-fatal consequences of untreated hypertension is a priority for many countries, and detection is a key element of strategies to achieve this. Over several decades, policies and systems have aimed to improve detection, and although detection rates have gradually improved, it is notable that a third or more of people with hypertension are still not detected and therefore offered appropriate management. In England, practice nurses and healthcare assistants are increasingly involved in the detection and management of hypertension, and it is important they are involved in developing policies and local initiatives to improve detection rates.10 The pay-for-performance scheme in England, the quality and outcomes framework, may have encouraged the offer of blood pressure checks to patients, but it has not ensured that people with raised readings are followed up to reach a diagnosis.5 Policy-makers should continue to give attention to the development and implementation of initiatives to improve detection, and should note the finding that the numbers of general practitioners per 1000 population is associated with detection rates. Both the qualitative study included in this review16 and a previous review of barriers to hypertension awareness and treatment23 highlighted the limited time in consultations to adequately investigate raised blood pressures. Primary care services that are under-resourced appear to be at risk of failing to detect a proportion of people with hypertension. Our study suggests a need in particular to increase attention to the follow-up of patients found to have an elevated blood pressure reading, until a diagnosis is confirmed or refuted. Practices need to detect hypertension more consistently. They should consider their arrangements for following up patients until a diagnosis is confirmed or ruled out, including how they will make use of home blood pressure monitoring or ambulatory blood pressure monitoring.37
Further research is also needed. New studies should aim to improve understanding of the barriers to detecting hypertension in primary medical care, and qualitative and ethnographic research could have valuable roles to play. We were able to identify only one relevant qualitative study for this review, although a review including settings other than primary medical care identified barriers among professionals that included knowledge and beliefs about the consequences of treatment.16 Investigation of such issues among primary medical care teams is required. The perceptions of medical and nursing primary care practitioners of the priority that hypertension detection merits and the processes involved in detecting hypertension in large numbers of patients need to be understood. It is also important to understand patients’ perceptions of systematic case-finding by practices. There is also a need for studies to develop and evaluate interventions to improve detection. Few intervention studies were found in our review. Interventions that include coordination with screening schemes both in practices and other settings such as pharmacies or the workplace are particularly needed.
Conclusions
In the studies included in the review, around 60% of people with hypertension have been detected, but although levels of detection have tended to improve in recent years, general practices need to improve detection, particularly the follow-up of people with a raised blood pressure reading until a diagnosis is confirmed. People who are older, women or have existing medical conditions appear more likely to have their hypertension detected. Greater numbers of general practitioners per 1000 patients were associated with higher detection. There is insufficient evidence to enable any conclusion on the effectiveness of interventions to improve detection rates.
Supplementary Material
Footnotes
Contributors: RB: conceived the study, contributed to study design, data extraction and interpretation of the results, and prepared the first draft of the paper. AW: contributed to study design, data extraction and interpretation of the results, and revised drafts of the paper. KN: planned and conducted the literature searches, and revised drafts of the paper. SA: contributed to data extraction and interpretation of the results, and revised drafts of the paper. PM: contributed to study design, data extraction and interpretation of the results, and revised drafts of the paper. JB: advised on the potential for meta-analyses, contributed to interpretation of the results and revised drafts of the paper.
Funding: This work was supported by a small grant from NHS Leicester City Clinical Commissioning Group.
Disclaimer: The funders had no role in the design, conduct, analysis or reporting of the study.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: This article reports a review; all the data summarised in the review are reported in published studies and are therefore already in the public domain.
References
- 1. Forouzanfar MH, Liu P, Roth GA, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115mmHg, 1990–2015. JAMA 2017;317:165–82. 10.1001/jama.2016.19043 [DOI] [PubMed] [Google Scholar]
- 2. England PH. Tackling high blood pressure. From evidence into action. Public Health England 2014. [Google Scholar]
- 3. Falaschetti E, Mindell J, Knott C, et al. Hypertension management in England: a serial cross-sectional study from 1994 to 2011. Lancet 2014;383:1912–9. 10.1016/S0140-6736(14)60688-7 [DOI] [PubMed] [Google Scholar]
- 4. Health Survey for England 2015. Methods, NHS digital. 2016. http://content.digital.nhs.uk/searchcatalogue?productid=23711&q=title%3a%22Health+Survey+for+England%22&sort=Relevance&size=10&page=1#top
- 5. Quality and Outcomes Framework 2015-16. Recorded disease prevalence, achievements and exceptions: NHS Digital, 2016. http://www.content.digital.nhs.uk/catalogue/PUB22266. [Google Scholar]
- 6. Baker R, Honeyford K, Levene LS, et al. Population characteristics, mechanisms of primary care and premature mortality in England: a cross-sectional study. BMJ Open 2016;6:e009981 10.1136/bmjopen-2015-009981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chang KC, Lee JT, Vamos EP, et al. Impact of the National Health Service Health Check on cardiovascular disease risk: a difference-in-differences matching analysis. CMAJ 2016;188:E228–E238. 10.1503/cmaj.151201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Krogsbøll LT, Jørgensen KJ, Grønhøj Larsen C, et al. General health checks in adults for reducing morbidity and mortality from disease. Cochrane Database Syst Rev 2012;10:CD009009 10.1002/14651858.CD009009.pub2 [DOI] [PubMed] [Google Scholar]
- 9. Public Health England. New approach to preventing heart attacks and strokes. 2017. www.gov.uk/government/news/new-approach-to-preventing-heart-attacks-and-strokes
- 10. NHS England, NHS Right Care. Tackling blood pressure: the size of the prize. 2017. www.england.nhs.uk/rightcare.2017/01/24/matt-kearney-huon-gray/
- 11. Royal College of General Practitioners. Report from general practice 19. Prevention of arterial disease in general practice. London, RCGP: Sub-committee chair Hart JT, 1981. [Google Scholar]
- 12. NHS Employers, British Medical Association, NHS England. 2014/15 General Medical Services (GMS) Contract Quality and Outcomes Framework (QOF). Guidance for GMS contract 2014/15. London: NHS Employers, 2014. http://www.nhsemployers.org/~/media/Employers/Documents/Primary%20care%20contracts/QOF/2014-15/2014-15%20General%20Medical%20Services%20contract%20-%20Quality%20and%20Outcomes%20Framework.pdf [Google Scholar]
- 13. Martínez-St John DR, Palazón-Bru A, Gil-Guillén VF, et al. Diagnostic inertia in obesity and the impact on cardiovascular risk in primary care: a cross-sectional study. Br J Gen Pract 2015;65:e454–e459. 10.3399/bjgp15X685669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. National Institute for Health and Care Excellence (NICE). Hypertension in adults: diagnosis and management. Clinical guideline [CG127], 2011. https://www.nice.org.uk/guidance/CG127/chapter/1-Guidance#diagnosing-hypertension-2
- 15. Maimaris W, Paty J, Perel P, et al. The influence of health systems on hypertension awareness, treatment, and control: a systematic literature review. PLoS Med 2013;10:e1001490 10.1371/journal.pmed.1001490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Khatib R, Schwalm JD, Yusuf S, et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studies. PLoS One 2014;9:e84238 10.1371/journal.pone.0084238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Muntner P, Gu D, Wu X, et al. Factors associated with hypertension awareness, treatment, and control in a representative sample of the Chinese population. Hypertension 2004;43:578–85. 10.1161/01.HYP.0000116302.08484.14 [DOI] [PubMed] [Google Scholar]
- 18. Pace R, Pluye P, Bartlett G, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud 2012;49:47–53. 10.1016/j.ijnurstu.2011.07.002 [DOI] [PubMed] [Google Scholar]
- 19. Banerjee D, Chung S, Wong EC, et al. Underdiagnosis of hypertension using electronic health records. Am J Hypertens 2012;25:97–102. 10.1038/ajh.2011.179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bankart MJ, Anwar MS, Walker N, et al. Are there enough GPs in England to detect hypertension and maintain access? A cross-sectional study. Br J Gen Pract 2013;63:339–44. 10.3399/bjgp13X667204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. de Burgos-Lunar C, del Cura-González I, Salinero-Fort MA, et al. Delayed diagnosis of hypertension in diabetic patients monitored in primary care. Rev Esp Cardiol 2013;66:700–6. 10.1016/j.rec.2013.01.019 [DOI] [PubMed] [Google Scholar]
- 22. Byrd JB, Powers JD, Magid DJ, et al. Detection and recognition of hypertension in anxious and depressed patients. J Hypertens 2012;30:2293–8. 10.1097/HJH.0b013e328359b6e6 [DOI] [PubMed] [Google Scholar]
- 23. Howes F, Hansen E, Williams D, et al. Barriers to diagnosing and managing hypertension. Australian Family Physician 2010;39:511–6. [PubMed] [Google Scholar]
- 24. Johnson HM, Thorpe CT, Bartels CM, et al. Antihypertensive medication initiation among young adults with regular primary care use. J Gen Intern Med 2014;29:723–31. 10.1007/s11606-014-2790-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. MacDonald TM, Morant SV. Prevalence and treatment of isolated and concurrent hypertension and hypercholesterolaemia in the United Kingdom. Br J Clin Pharmacol 2008;65:775–86. 10.1111/j.1365-2125.2007.03072.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mancia G, Parati G, Borghi C, et al. Hypertension prevalence, awareness, control and association with metabolic abnormalities in the San Marino population: the SMOOTH study. J Hypertens 2006;24:837–43. 10.1097/01.hjh.0000222752.67572.61 [DOI] [PubMed] [Google Scholar]
- 27. Nazroo JY, Falaschetti E, Pierce M, et al. Ethnic inequalities in access to and outcomes of healthcare: analysis of the Health Survey for England. J Epidemiol Community Health 2009;63:1022–7. 10.1136/jech.2009.089409 [DOI] [PubMed] [Google Scholar]
- 28. Pallares-Carratalá V, Bonig-Triguerros I, Palazón-Bru A, et al. Steering Committee ESCARVAL study. Int J Clin Pract 2016;70:619–24. [DOI] [PubMed] [Google Scholar]
- 29. Patel R, Lawlor DA, Whincup P, et al. The detection, treatment and control of high blood pressure in older British adults: cross-sectional findings from the British Women’s Heart and Health Study and the British Regional Heart Study. J Hum Hypertens 2006;20:733–41. 10.1038/sj.jhh.1002064 [DOI] [PubMed] [Google Scholar]
- 30. Shah S, Cook DG. Inequalities in the treatment and control of hypertension: age, social isolation and lifestyle are more important than economic circumstances. J Hypertens 2001;19:1333–40. 10.1097/00004872-200107000-00020 [DOI] [PubMed] [Google Scholar]
- 31. Soljak M, Samarasundera E, Indulkar T, et al. Variations in cardiovascular disease under-diagnosis in England: national cross-sectional spatial analysis. BMC Cardiovasc Disord 2011;11:12 10.1186/1471-2261-11-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wallace ML, Magnan EM, Thorpe CT, et al. Diagnosis and treatment of incident hypertension among patients with diabetes: a U.S. multi-disciplinary group practice observational study. J Gen Intern Med 2015;30:768–76. 10.1007/s11606-015-3202-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zhao B, Jose PO, Pu J, et al. Racial/ethnic differences in hypertension prevalence, treatment, and control for outpatients in northern California 2010–2012. Am J Hypertens 2015;28:631–9. 10.1093/ajh/hpu189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bonds DE, Hogan PE, Bertoni AG, et al. A multifaceted intervention to improve blood pressure control: The Guideline Adherence for Heart Health (GLAD) study. Am Heart J 2009;157:278–84. 10.1016/j.ahj.2008.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cottrell E, Cox T, O’Connell P, et al. Implementation of simple telehealth to manage hypertension in general practice: a service evaluation. BMC Fam Pract 2015;16:83 10.1186/s12875-015-0301-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hemming K, Ryan R, Gill P, et al. Targeted case finding in the prevention of cardiovascular disease: a stepped wedge cluster randomised controlled trial. Br J Gen Pract 2016;66:e758–e767. 10.3399/bjgp16X686629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mejzner N, Clark CE, Smith LF, et al. Trends in the diagnosis and management of hypertension: repeated primary care survey in South West England. Br J Gen Pract 2017;67:e306–e313. 10.3399/bjgp17X690461 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-019965supp001.pdf (338.3KB, pdf)