Abstract
Purpose
Present the rationale, methods, and cohort characteristics for two complementary “big data” studies of residential environment contributions to body weight, metabolic risk, and weight management program participation and effectiveness.
Design
Retrospective cohort
Setting
Continental U.S.
Subjects
3,261,115 veterans who received Department of Veteran Affairs (VA) healthcare in 2009–2014, including 169,910 weight management program participants and a propensity-score derived comparison group.
Intervention
VA MOVE! weight management program, an evidence-based lifestyle intervention.
Measures
BMI, metabolic risk measures, MOVE! participation; residential environmental attributes (e.g., food outlet availability, walkability); MOVE! program characteristics.
Analysis
Descriptive statistics presented on cohort characteristics and environments where they live.
Results
Forty-four percent of men and 42.8% of women were obese, while 4.9% of men and 9.9% of women engaged in MOVE!. About half of the cohort had at least one supermarket within one-mile of their home, while they averaged close to 4 convenience stores (3.6 for men; 3.9 for women) and 8 fast food restaurants (7.9 for men; 8.2 for women). Forty-one percent of men and 38.6% of women did not have a park, and 35.5% of men and 31.3% of women did not have a commercial fitness facility within one-mile.
Conclusion
Drawing on a large nationwide cohort residing in diverse environments, these studies are poised to significantly inform policy and weight management program design.
Keywords: Neighborhood, Obesity, Weight Loss, Health Status Disparities, Food Environment, Built Environment
Indexing Key Words: Research Program evaluation, Relationship Testing Quasi-experimental, Biometric Clinical/health care, Local community, National Weight control, Skill building/behavior change, Built environment Adults, Seniors Education/income level, Geographic location, Race/ethnicity
Purpose
Obesity (body mass index ≥ 30 kg/m2) is a well-established contributor to cancer development and mortality, as well as other health outcomes.1–5 The age-adjusted prevalence of obesity in the U.S. is 34.9%, with disparities by gender, race/ethnicity, socioeconomic status (SES), and urbanicity.6–9 Despite tremendous investment in obesity research, weight loss treatments continue to show limited success in terms of both individual and population changes in body weight and associated chronic disease health outcomes. Even among people who successfully lose weight, only half lose a clinically significant amount of weight.10–12 Furthermore, those who do lose weight usually gain the weight back in a relatively short time period.13,14
Researchers increasingly believe that environmental pressures to eat will often override self-management skills that support intentional weight loss and maintenance.15 A growing literature now focuses on environmental contributors to obesity that are amenable to policy interventions with broad population impact.16–18 Environmental attributes such as availability of healthy foods and options for physical activity vary widely, with economically disadvantaged and segregated minority communities often having less supportive environments.19–21 Environmental interventions and policies are being proposed and occasionally implemented.22–25 However, despite the growth in geospatial research in this area,26 there is little consensus on whether environmental attributes themselves affect body weight and metabolic risk measures (e.g., blood pressure, lipids, glucose), and how much change could be expected by modifying specific environmental attributes.27–33 It is also unclear whether one’s environment is a motivating or deterring factor to weight loss and maintenance,34–38 or whether weight management interventions could be enhanced by environmental tailoring.
The Weight And Veterans’ Environments Study (WAVES) I and II are complementary retrospective cohort studies of U.S. military veterans who used U.S. Department of Veterans Affairs (VA) healthcare in 2009–2014 and who were followed to date through 2015. The VA provides integrated healthcare to over 5 million veterans each year. Once enrolled for VA care, veterans generally remain enrolled over their lifetimes. Together, the two projects examine impacts of diet- and physical activity-related attributes of residential environments on body weight, metabolic risk, and participation in and effectiveness of the VA MOVE! program, a nationwide weight management program. The studies are guided by social-ecological models of behavior change,39,40 as well as microeconomic theory of the demand for and production of health.41 Funded by the National Cancer Institute (R01CA172726), WAVES I examines environmental attributes that help individuals to maintain healthier BMI and metabolic risk status up to 7 years and also whether those attributes support MOVE! participation and weight loss at six months and 18 months, and achieve healthier BMI trajectory in the longer term (5 years). The overarching hypothesis of WAVES I is that over time individuals living in more supportive environments will have a healthier BMI and metabolic risk status and achieve better weight outcomes in MOVE!. Funded by the U.S. Department of Veterans Affairs Office of Research and Development (VA IIR 13-085), WAVES II studies whether individuals are more likely to engage in MOVE! and achieve better weight management outcomes if specific MOVE! program elements are matched to, or aligned with, environmental attributes. A key hypothesis is that the MOVE! program is more effective when program elements substitute for environmental deficiencies and complement environmental resources. We will also examine whether these relationships differ by race/ethnicity, gender, and urbanicity.
WAVES I and II are unique studies at the forefront of “big data” research linking electronic health record and health system program data, with public and proprietary data on the residential environment to understand relationships among the residential environment, weight management programs, and body weight and related health outcomes. Using VA healthcare data allows us to answer timely and important scientific questions that are otherwise impossible to address since no other U.S. population database is comparable with respect to the number of covered individuals, inclusion of measured health outcomes, diversity of residential environments due to the national scope, and longitudinal structure. While veterans using VA healthcare are different in some respects than the U.S. adult population (e.g., more likely to be men, older, and non-Hispanic black and less likely to be Hispanic), they should be similar in terms of effects of the residential environment on health outcomes and responses to weight management programs, and they live in communities throughout the U.S. In this paper, following the rationale provided above for WAVES I and II, we review methods we are using to address our study aims and provide a description of our cohort and the environments in which they live. Additionally, we share results of our analysis to construct an inverse propensity score weighted comparison group for our forthcoming analyses involving MOVE!. We conclude by discussing the strengths and weaknesses of the studies.
Methods
Design
WAVES I and II are complementary, observational retrospective longitudinal cohort studies and were both approved by the institutional review boards of the University of Illinois at Chicago and Hines VA Hospital.
Sample
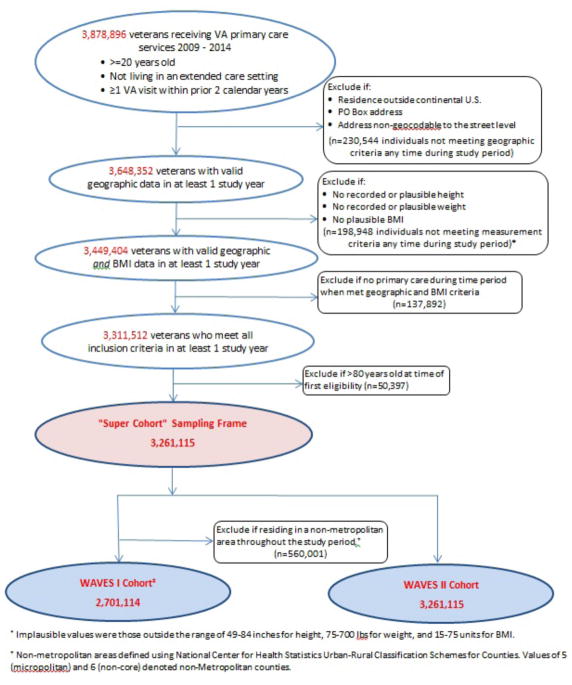
The study cohort consists of more than 3 million U.S. military veterans who received primary healthcare services in the VA between 2009 and 2014 and lived in the continental U.S. Sample inclusion criteria are: (1) aged 20–80 years and (2) at least one VA healthcare encounter in the two years prior to baseline year (2009 or first year in which the patient met study eligibility criteria). Exclusion criteria are: (1) long-stay nursing home residence at baseline; (2) no home address, PO Box address, or address that was non-geocodable to the street or ZIP+4 in all study years; and (3) absence of measured height and weight in all study years. In addition, due to resource constraints, WAVES I excluded individuals who lived exclusively in non-metropolitan areas during the study period. Patients were accrued to the study based on the earliest year (2009–2014) in which they met study inclusion criteria. To date, the cohort has been followed through 2015. Figure 1 shows the sample derivation, with the “super cohort” (sample spanning both studies) consisting of 3,261,115 patients of whom 78.2% lived in metropolitan areas. Those living in metropolitan areas formed the basis of the WAVES I cohort. For study questions related to the MOVE! program, we identified 169,910 MOVE! program participants and used propensity score analysis based on a rich set of covariates to construct matched (male and female) longitudinal comparison groups from among all non-participants who had complete data on the 120+ variables used in the propensity score analysis. For the WAVES II cohort, we included patients living in both metropolitan and non-metropolitan areas. According to VA records as of 11-18-2016, 492,999 deaths had occurred in the super cohort during the study period (through December 31, 2015).
Figure 1.
Sample derivation and sizes for WAVES I and II
Intervention
VA MOVE! is a nationwide, evidence-based weight management program, patterned after the lifestyle intervention developed for the Diabetes Prevention Program and updated based on new dietary guidelines.12,42–45 The VA implemented MOVE! in 2006 to address the high obesity prevalence among veterans.43 VA clinical guidelines recommend referrals to MOVE! for patients who are obese or who are overweight and also have obesity-related comorbidities and no contraindications to weight loss treatment.46 MOVE! participants receive an individualized treatment plan, including education and counseling strategies that support lifestyle behavior change efforts. Referred patients are offered group as well as individual sessions (in person or phone). Rather than a highly structured program, MOVE! intentionally allows for flexibility in program implementation and is a set of tools, resources, and guidelines. Thus, while each of the 136 VA healthcare facilities in the continental U.S. has a MOVE! coordinator, physician champion, and staff who address weight management, other MOVE! elements are determined locally and can be customized to fit local conditions and patient populations. As a result, specific program elements vary across the 136 healthcare facilities. This heterogeneity is captured in the MOVE! program exposures outlined below.
Measures
Patient measures
Veteran measures are obtained mainly from patient-level healthcare encounter records and other VA administrative data sources. One practical challenge for our longitudinal study design is that outcome measurements are a byproduct of healthcare utilization and are not collected according to a predefined schedule. We imposed an annual measurement structure on the data for each person and derived patients’ study measures using data from all healthcare visits in that year. Measurements are not available if a person did not utilize health services from the VA during the year. We accrued a total of 14,975,115 person-year observations, which is 87.4% of the total possible.
Health outcomes include BMI (calculated from measured height and weight) and blood pressure, obtained by healthcare personnel during clinical encounters; VA laboratory result values for glucose and cholesterol ordered by providers in the routine course of patient care (WAVES I only); and MOVE! engagement (Table 1). Covariates include demographics; clinical factors including chronic health conditions, health events, and prescribed medications; healthcare utilization; and VA facility. Using Department of Defense (DoD), Defense Manpower Data Center (DMDC) data, SES will be measured with two proxy indicators: military rank at discharge47–49 and aptitude test results.50–52
Table 1.
Patient Measures.
| Construct* | Conceptual Definition | Operational Definition | Source |
|---|---|---|---|
| Outcomes | |||
|
| |||
| BMI | Weight, controlling for height | weight (kg)/[height (m)]2, based on measured height and weight | CDW |
| Metabolic Risk (WAVES I) | Blood pressure Serum glucose Serum lipids |
Systolic and diastolic blood pressures Serum glucose Total, HDL and LDL cholesterol |
CDW |
| MOVE! Engagement/Participation (WAVES II) | Duration and/or intensity of MOVE! program participation | 2 or more visits (yes/no) MOVE! visit count “Intense and Sustained” participation as defined by MOVE! (8 or more visits in 6 months taking place over at least 4 months) |
NPCD |
|
| |||
| Covariates | |||
|
| |||
| Demographics | Age | Age: in years | NPCD |
| Gender/sex | Self-reported gender or sex | NPCD | |
| Race/ethnicity | Self-reported race and ethnicity | NPCD | |
| Marital status | Marital status | NPCD | |
| Socioeconomic status | Military rank at discharge (DoD) AFQT aptitude test score (percentile), taken at military recruitment |
DoD | |
| Clinical Factors | Health status/comorbidity burden | Modified Deyo-Charlson Comorbidity Score, based on ICD-9 and CPT procedure codes, or similar comorbidity index | NPCD, Medicare claims |
| Health events impacting diet, physical activity, or weight | Surgical procedures, based on Decision Support System (DSS) Identifiers (clinic stop codes), CPT, and ICD-9 procedure codes | NPCD, Medicare claims | |
| Medications known to influence appetite, weight | Weight loss medications (e.g., orlistat) Other medications known to influence appetite and/or weight (e.g., insulin, anti-psychotics antidepressants, oral diabetes drugs) |
DSS Pharmacy Data, Medicare Part D event data | |
| Healthcare Utilization | Inpatient stays and outpatient encounters | Count of inpatient days Count of outpatient primary and specialty care provider encounters |
NPCD, Medicare claims |
| MOVE! Program Participation (WAVES I) | Intensity, duration, and components of MOVE! program participation | MOVE! encounters (e.g., count, yes/no) MOVE! encounter type(s)—individual in-person, individual phone, group |
NPCD (DSS identifiers) |
| Veteran’s VA Facility | VA facility where veteran received the majority of his/her care | VA facility identifier | NPCD |
Abbreviations: ADR: Administrative Data Repository; AFQT: Armed Forces Qualifying Test; ASVAB: Armed Services Vocational Aptitude Battery; BMI: Body Mass Index; CDW: VA Corporate Data Warehouse; DoD: Department of Defense; DSS: VHA Decision Support System; NPCD: National Patient Care Database; NPPD: National Prosthetics Patient Database; PSSG: Planning Systems Support Group; VBA: Veterans Benefits Administration; VSF: VHA Vital Status File; VADIR: VA/DOD Identity Repository
Constructs apply to both WAVES I and II unless otherwise specified.
Residential environmental exposures
Annual residential environmental exposure measures are based on home geocodes (2009–2015) obtained from the VHA Planning Systems Support Group and based on current address information at the end of each federal fiscal year.53 In addition to urbanicity,54 ten categories of environmental attributes are of interest: healthier food outlet accessibility (e.g., supermarkets), less healthy food outlet accessibility (e.g., fast food restaurants), healthier food product prices (e.g., fruits and vegetables), less healthy food product prices and taxes (e.g., fast food), walkability (e.g., street connectivity), accessibility of recreational settings (e.g., parks), aesthetics (e.g., vacant housing), traffic safety (e.g., presence of traffic-calming features), local area socioeconomic and demographic characteristics, and VA healthcare accessibility (Table 2). These categories were selected based on conceptual frameworks of environmental influences on healthy eating18 and active living55 while precise attributes within each category were selected based on nationwide and retrospective availability of high-quality data.
Table 2.
Residential Environmental and MOVE! Weight Management Program Exposure Measures.
| Construct | Conceptual Definition | Operational Definition | Source |
|---|---|---|---|
| Residential Environmental Attributes | |||
|
| |||
| Healthier food outlet accessibilitya | Availabilityb of food outlets offering a large selection of healthier food products | Chain and non-chain supermarkets Grocery stores Supercenters and other general merchandise storesc |
InfoUSA |
| Less healthy food outlet accessibilitya | Availabilityb of food outlets primarily selling energy-dense, nutrient-poor food products | Convenience stores | InfoUSA |
| Chain and non-chain fast food restaurants | Dun & Bradstreet | ||
| Healthier food product pricesd | Prices of healthier foods and beverages | Fruit and vegetable prices: summary measure of raw potatoes (10 lb bag), bananas (per lb), lettuce (head), peas (15–15.25 oz can), tomatoes, frozen corn (16 oz), peaches (29 oz can) | C2ER Cost of Living Index |
| Food at home prices: summary measure including items such as eggs, milk, chicken, coffee, cereal, and bread | C2ER Cost of Living Index | ||
| Less healthy food product pricesd | Prices of and sales taxes on energy-dense, nutrient-poor foods and beverages | Fast food prices: summary measure of pizza (11–12 inch thin cheese), hamburger (1/4 lb), 2 piece chicken (thigh plus drumstick) | C2ER Cost of Living Index |
| Soda prices: Coke (12 oz) | |||
| Soda taxes (i.e., state-level sales taxes on soda) | http://www.bridgingthegapresearch.org/research/sodasnack_taxes/ | ||
| Walkabilitye | Availability of non- residential destinations and directness of walking routes | Street connectivity (e.g., density of street intersections, ratio of 4- way to all street) | NAVTEQ |
| Population and housing unit densities | ACS | ||
| Density of commercial destinations | InfoUSA and Dun & Bradstreet | ||
| Accessibility of recreational settingsa | Availabilityb of indoor and outdoor settings to be physically active | Parks – count and land area | NAVTEQ and TeleAtlas |
| Fitness facilities | InfoUSA | ||
| Aestheticse | Attractiveness or appeal | Vacant housing unit density | ACS |
| Traffic safetye | Road features that slow or calm traffic | Presence of (a) median/dividers, (b) roundabouts, and (c) “low mobility” features (e.g., low speeds and traffic volumes) | NAVTEQ |
| Socioeconomic and demographic characteristics | Deprivation and affluence | % below poverty Median household income % college educated |
ACS |
| VA healthcare accessibility | Proximity of VA healthcare facility | Distance from patient’s home to (a) nearest VA inpatient facility, (b) nearest VA outpatient facility, and (c) patient’s most frequently used VA facility | |
| Urbanicityf | Degree of urbanization | Urban-Rural Classification Scheme: metropolitan area (large central metro, large fringe metro, medium metro, small metro) and non-metropolitan area (micropolitan, non-core) | NCHS |
|
| |||
| MOVE! Program Characteristicsg | |||
|
| |||
| MOVE! program elements | Nutrition supports | Total nutrition specialist FTE Specific provider specialty FTE (Registered Dietician vs. Dietetic Technician) Multidisciplinary approach: Involvement of dietetic/nutrition specialist and behavioral health specialist (yes/no; FTE ratio) Includes a highly structured low-calorie diet (yes/no) |
MOVE! Annual Reporth |
| Physical activity supports | Total physical activity specialist FTE Specific provider specialty FTE (Recreational Therapist vs. Physical, Occupational, or Kinesiotherapist) Multidisciplinary approach: Involvement of physical activity specialist and behavioral health specialist (yes/no; FTE ratio) Physical activity incorporated into MOVE! group sessions (yes/no) Dedicated indoor physical activity space (yes/no) Outdoor environment for physical activity (yes/no) |
MOVE! Annual Report | |
| Behavioral health supports | Total behavioral health specialist FTE Specific provider specialty FTE (Psychologist or Social Worker vs. Mental Health Technician) “Sufficient” behavioral/mental health specialist involvement to meet needs (yes/no) Self-management support skill development:
Use of incentives/rewards (yes/no) |
MOVE! Annual Report | |
| Distance supports | Telehealth utilization (available yes/no; % of all MOVE! encounters):
|
MOVE! Annual Report | |
Abbreviations: FTE: Full time equivalent; NPCD: National Patient Care Database
Constructed for approximately 0.25, 1, 3, and 5-mile buffers from home location.
Count, count per capita, and count per land area, as well as distance to the nearest
Supercenters and other mass merchandisers may be considered a less healthy food outlet due to marketing of unhealthy food products
Food price data are available nationwide for core-based statistical areas (CBSAs). Therefore, price data are assigned according to the CBSA in which the home is located or the nearest CBSA. Food sales tax data are available nationwide at the state level. Therefore, tax data are assigned according to the state in which home is located.
Constructed for 0.25 and 1-mile buffers from home address
Constructed based on county in which home is located
All measures to be derived from data contained in MOVE! Annual Reports, FY2008–2013 (excluding 2012 when data were not collected)
Data recollected via electronic survey from each medical center with a MOVE! Program; no survey conducted in 2012 or 2014
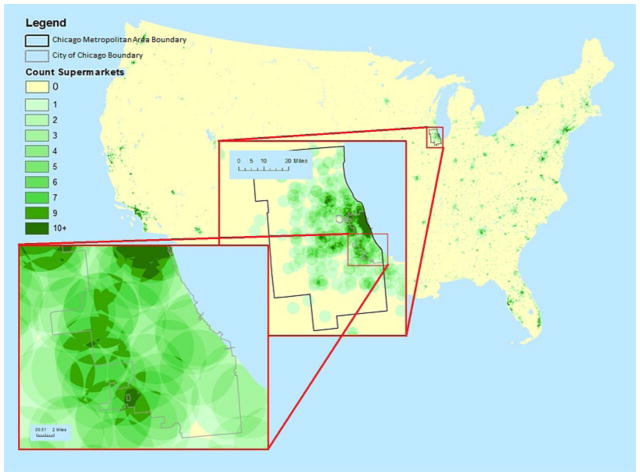
The geographic precision of the veteran residential location information allows us analytic flexibility to examine any level of geography we choose. With the exception of food prices and taxes (for which data are available at the core-based statistical area or state level), environmental measures are constructed using a “SmartMap” approach.49 Specifically, using geographic information system (GIS) software, we divided the continental U.S. into 30m × 30m cells, totaling approximately 8.98 billion cells. Environmental measures are based on each grid cell’s centroid for up to four small spatial scales (circular buffers with radii ranging from 0.25 mile to 5 miles). Time-varying, annual values for the environmental measures are assigned to each veteran based on the cell in which his or her home is located. Figure 2 shows an example of a supermarket SmartMap.
Figure 2.
Accessibility of supermarkets within 3 miles for the continental U.S.
MOVE! engagement and participation
Measures of MOVE! engagement and participation reflect duration and frequency of contact. Two or more in-person visits within a 6-month period will comprise our minimum criterion for MOVE! engagement. Among those who engage in MOVE!, we will measure extent of participation through counts of visits over specified periods of time (e.g., number of days with a MOVE! encounter over a 6-month period) and encounter type (e.g., individual in-person, individual phone, group). Additionally, we will measure and examine the impact of type or quality of participation using a measure of “intense and sustained” participation, that is, 8 or more visits in 6 months spanning 4 months or longer.56
MOVE! program exposures
We will examine single measures and four constructed composite measures of MOVE! program elements that we conceptualize as providing nutrition, physical activity, behavioral health, or distance-related support for weight management (Table 2). Annual data are available from each of the 136 VA facilities in the continental U.S. where MOVE! programs are administratively housed. Site-specific implementations of the MOVE! program use different combinations of program elements.
Data analysis
As the general analytic strategy, WAVES I and II will employ panel data statistical models that are robust to a broad class of potential sources of bias. For WAVES I (where outcomes modeled will be body weight, blood pressure, serum glucose, and serum lipids and the independent variables of primary interest will be environmental attributes), the panel data models will include individual and time fixed effects in order to account for unobserved characteristics of individuals or time period that might be associated with both environmental attributes and body weight. In these models, environmental effects are identified by within-person variation in environmental attributes that arises when people migrate between geographical areas and when people stay in place but environmental attributes change over time. To assess the sensitivity of our results to the possibility that migrants have different health trajectories than non-migrants, we will also fit the same regression models to samples of non-migrants. In analyses involving MOVE!, we also face the problem of non-random selection into the MOVE! program. In that work, we use propensity score methods to construct a comparison group of non-participants that resembles the program participant sample with respect to a vector of pre-treatment covariates and then estimate panel data regression models on the matched sample to study how participants and non-participants respond differently to environmental attributes. WAVES II (where the outcome modeled will be body weight and the independent variables of primary interest will be interactions between MOVE! program elements and environmental attributes) will use the same approach but will also employ regression discontinuity methods to add further confidence to our findings.
In this paper, we describe the study sample at baseline using descriptive statistics. In addition, we present information on environmental attributes based on where subjects lived at study accrual. Finally, we present results from our propensity score analysis involving 120+ covariates including veteran demographics, clinical factors, healthcare utilization, residential environmental attributes, and VA healthcare facility characteristics. (A complete list of covariates is available in Supplemental Table 1.) We sought to achieve a matched sample in which the standardized difference in means (Cohen’s D) between the matched participant and non-participant was less than 0.1 for each baseline covariate.57
Results
Cohort characteristics
Table 3 shows descriptive statistics at baseline for veteran demographics, clinical factors, healthcare utilization, and residential environmental attributes within one mile of home locations for the super cohort comprising 3,035,525 men and 225,590 women. Among men, the majority (61.5%) were 60–80 years of age; about 20% were non-Hispanic black (15.9%) or Hispanic (4.3%); the most common medical diagnoses were hypertension, hyperlipidemia, and diabetes; and 43.6% were obese. Among women, half (50.6%) were 40–59; over 30% were non-Hispanic black (28.4%) or Hispanic (5.3%); the most common medical diagnoses were depression, hypertension, and hyperlipidemia; and 42.8% were obese.
Table 3.
Baseline Characteristics of the Weight And Veterans’ Environments Study (WAVES) I and II Super Cohort, Including MOVE! Weight Management Program Participanta and Control Comparison With and Without Application of Inverse Propensity Score Weights.
| N | Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Overall | MOVE! Participants |
Comparison Group | Overall | MOVE! Participants |
Comparison Group | ||||||
|
|
|
||||||||||
| Unweighted | Weighted | Unweighted | Weighted | ||||||||
|
| |||||||||||
| 3,035,525 | 147,646 | 2,887,879b | 225,590 | 22,264 | 203,326b | ||||||
|
| |||||||||||
| Patient Demographics | % (unless otherwise noted) | Cohen’s D | % (unless otherwise noted) | Cohen’s D | |||||||
| Age - 10 year groups | |||||||||||
| 20–29 | 4.4 | 1.6 | 4.6 | 1.6 | .001 | 14.9 | 6.4 | 15.9 | 6.3 | .003 | |
| 30–39 | 5.3 | 4.1 | 5.4 | 4.1 | .003 | 19.1 | 15.7 | 19.4 | 15.7 | .001 | |
| 40–49 | 9.4 | 12.0 | 9.3 | 11.9 | .003 | 24.2 | 29.5 | 23.7 | 29.5 | −.001 | |
| 50–59 | 19.4 | 27.0 | 19.0 | 27.0 | −.001 | 26.4 | 34.9 | 25.4 | 35.0 | −.002 | |
| 60–69 | 36.3 | 47.1 | 35.7 | 47.3 | −.004 | 10.6 | 11.9 | 10.4 | 11.9 | .001 | |
| 70–80 | 25.2 | 8.1 | 26.1 | 8.1 | .002 | 4.8 | 1.6 | 5.2 | 1.6 | .002 | |
| Race/Ethnicity | |||||||||||
| Non-Hispanic white | 67.9 | 65.4 | 68.0 | 65.2 | .004 | 54.7 | 51.8 | 55.0 | 51.9 | −.001 | |
| Non-Hispanic black | 15.9 | 22.0 | 15.6 | 22.2 | −.005 | 28.4 | 36.1 | 27.5 | 36.2 | −.001 | |
| Hispanic | 4.3 | 5.1 | 4.2 | 5.2 | −.002 | 5.3 | 4.3 | 5.4 | 4.3 | .002 | |
| Other | 2.1 | 2.2 | 2.1 | 2.1 | .000 | 3.1 | 2.8 | 3.2 | 2.7 | .002 | |
| Unknown | 10.0 | 5.4 | 10.2 | 5.3 | .003 | 8.5 | 5.0 | 8.9 | 5.0 | .002 | |
| Marital status | |||||||||||
| Married | 57.7 | 56.3 | 57.7 | 56.2 | .004 | 34.3 | 32.7 | 34.5 | 32.6 | .002 | |
| Separated or divorced | 22.6 | 24.3 | 22.5 | 24.4 | −.001 | 31.4 | 35.2 | 30.9 | 35.2 | .001 | |
| Widowed | 3.9 | 2.8 | 4.0 | 2.8 | −.000 | 3.7 | 3.5 | 3.7 | 3.5 | −.000 | |
| Single | 14.8 | 15.8 | 14.8 | 15.9 | −.004 | 28.7 | 27.3 | 28.8 | 27.5 | −.002 | |
| Unknown | 1.1 | 0.7 | 1.1 | 0.7 | −.000 | 2.0 | 1.3 | 2.1 | 1.3 | −.001 | |
|
| |||||||||||
| Clinical Factors | |||||||||||
|
| |||||||||||
| Health conditions | |||||||||||
| Cancer | 8.9 | 6.1 | 9.1 | 7.0 | −.039 | 3.5 | 3.4 | 3.5 | 3.7 | −.018 | |
| Cerebrovascular disease | 5.5 | 3.6 | 5.6 | 3.6 | .001 | 1.8 | 1.9 | 1.7 | 1.9 | .004 | |
| COPD (not asthma) | 13.2 | 11.9 | 13.3 | 13.6 | −.055 | 10.3 | 13.3 | 10.0 | 14.4 | −.032 | |
| Congestive heart failure | 5.8 | 5.0 | 5.9 | 5.1 | −.000 | 1.3 | 1.2 | 1.3 | 1.2 | .002 | |
| Depression | 16.1 | 25.2 | 15.6 | 25.4 | −.005 | 28.2 | 40.3 | 26.8 | 40.5 | −.003 | |
| Diabetes mellitus | 25.1 | 35.7 | 24.6 | 36.0 | −.005 | 9.7 | 15.3 | 9.0 | 15.3 | −.000 | |
| Hyperlipidemia | 43.7 | 49.2 | 43.5 | 49.4 | −.002 | 20.6 | 28.4 | 19.8 | 28.6 | −.004 | |
| Hypertension | 54.3 | 61.8 | 54.0 | 62.0 | −.004 | 25.8 | 35.3 | 24.8 | 35.3 | −.001 | |
| Osteoarthritis | 14.5 | 18.3 | 14.3 | 17.8 | .012 | 10.2 | 15.8 | 9.5 | 14.9 | .024 | |
| Body mass index: Mean (SD) | 29.9 (5.8) | 35.3 (6.6) | 29.6 (5.6) | 35.4 (6.6) | −.006 | 29.6 (6.5) | 34.4 (6.5) | 29.0 (6.3) | 34.4 (6.5) | −.004 | |
| Body weight status | |||||||||||
| Normal or underweight | 18.7 | 2.4 | 19.5 | 2.4 | .002 | 26.2 | 4.4 | 28.5 | 4.3 | .002 | |
| Overweight | 37.8 | 17.7 | 38.8 | 17.5 | .005 | 31.1 | 22.0 | 32.0 | 21.8 | .005 | |
| Obese | 43.6 | 79.9 | 41.7 | 80.1 | −.005 | 42.8 | 73.6 | 39.4 | 73.9 | −.006 | |
|
| |||||||||||
| Healthcare Utilization | |||||||||||
|
| |||||||||||
| Healthcare utilization: Mean (SD) | |||||||||||
| Primary care encounters, annual number | 3.0 (2.7) | 4.1 (3.5) | 3.0 (2.6) | 4.1(4.2) | .003 | 3.3 (2.8) | 4.4 (3.6) | 3.2 (2.6) | 4.4 (3.8) | .016 | |
| Hospital admissions, annual number | 0.2 (.6) | 0.2 (.6) | 0.2 (.6) | 0.2 (.6) | −.003 | 0.1 (.5) | 0.2 (.6) | 0.1 (.5) | 0.2 (.6) | −.005 | |
| Days in hospital, annual number | 1.2 (6.6) | 1.3 (6.4) | 1.2 (6.6) | 1.3 (6.3) | −.004 | 0.8 (5.6) | 1.2 (6.3) | 0.8 (5.6) | 1.2 (6.6) | −.005 | |
| Migration | |||||||||||
| Moved at least once in 5 years | 30.6 | 37.1 | 30.1 | 34.6 | .052 | 40.5 | 47.0 | 39.8 | 44.3 | .053 | |
|
| |||||||||||
| Residential Environmental Attributes | |||||||||||
|
| |||||||||||
| Census division | |||||||||||
| New England | 4.4 | 4.7 | 4.3 | 4.4 | .009 | 3.0 | 3.0 | 3.0 | 2.9 | .010 | |
| Middle Atlantic | 10.2 | 10.0 | 10.2 | 10.2 | −.006 | 7.5 | 7.8 | 7.4 | 7.7 | .004 | |
| East North Central | 14.6 | 18.3 | 14.4 | 18.6 | −.007 | 11.2 | 14.1 | 10.9 | 14.5 | −.010 | |
| West North Central | 7.6 | 7.4 | 7.7 | 7.3 | .004 | 5.9 | 6.8 | 5.8 | 6.2 | .025 | |
| South Atlantic | 23.2 | 20.7 | 23.3 | 20.9 | −.004 | 28.8 | 26.5 | 29.0 | 27.1 | −.013 | |
| East South Central | 8.0 | 5.5 | 8.1 | 5.4 | .005 | 7.9 | 7.0 | 8.0 | 6.8 | .007 | |
| West South Central | 12.9 | 12.4 | 12.9 | 11.9 | .015 | 15.0 | 15.1 | 15.0 | 14.9 | .004 | |
| Mountain | 8.1 | 10.1 | 8.0 | 10.0 | .002 | 9.3 | 9.8 | 9.2 | 9.9 | −.002 | |
| Pacific | 11.1 | 11.0 | 11.1 | 11.3 | −.01 | 11.5 | 9.9 | 11.7 | 10.1 | −.009 | |
| Urbanicity | |||||||||||
| Large central metro | 22.4 | 26.9 | 22.2 | 26.9 | −.001 | 26.0 | 27.1 | 25.9 | 27.4 | −.007 | |
| Large fringe metro | 19.6 | 18.9 | 19.6 | 18.9 | .001 | 20.5 | 18.7 | 20.7 | 18.7 | .002 | |
| Medium metro | 23.5 | 24.4 | 23.4 | 24.3 | .002 | 26.1 | 27.6 | 25.9 | 27.6 | −.000 | |
| Small metro | 12.3 | 12.0 | 12.3 | 12.1 | −.002 | 11.9 | 11.6 | 11.9 | 11.8 | −.004 | |
| Micropolitan | 13.9 | 11.7 | 14.0 | 11.5 | .008 | 10.5 | 10.2 | 10.6 | 9.8 | .012 | |
| Non-core | 8.4 | 6.1 | 8.5 | 6.4 | −.011 | 5.1 | 4.8 | 5.1 | 4.8 | −.001 | |
| Census tract demographics: Mean (SD) | |||||||||||
| Percent below poverty | 14.4 (10.6) | 14.8 (11.3) | 14.4 (10.6) | 14.8 (11.3) | −.004 | 14.7 (10.5) | 15.4 (11.0) | 14.6 (10.4) | 15.4 (11.0) | −.002 | |
| Median household income ($) | 50,907 (20,796) | 50,529 (20,411) | 50,926 (20,815) | 50,504 (20,414) | .001 | 51,416 (20,106) | 49,403 (19,160) | 51,636 (20,194) | 49,357 (19,177) | .002 | |
| Population density | 3,240 (8,071) | 4,053 (9,446) | 3,198 (7,992) | 4,108 (9,503) | −.006 | 3,543 (7,777) | 3,823 (8,221) | 3,503 (7,729) | 3,831 (8,170) | −.001 | |
| (Dis)amenities – count within 1 mile | |||||||||||
| Supermarket: Mean (SD) | 1.0 (1.8) | 1.1 (1.9) | .95 (1.8) | 1.1 (2.0) | −.008 | 1.0 (1.7) | 1.1 (1.8) | 1.0 (1.7) | 1.1 (1.7) | .004 | |
| Supermarket: 1+ | 47.1 | 51.4 | 46.8 | 51.9 | −.006 | 50.1 | 52.5 | 49.8 | 52.8 | .001 | |
| Convenience store: Mean (SD) | 3.6 (4.6) | 4.1 (5.1) | 3.6 (4.6) | 4.2 (5.1) | −.007 | 3.9 (4.5) | 4.2 (4.7) | 3.8 (4.5) | 4.2 (4.7) | −.003 | |
| Convenience store: 1+ | 69.5 | 74.0 | 69.2 | 74.5 | −.006 | 74.7 | 77.3 | 74.4 | 77.6 | −.003 | |
| Fast food restaurant: Mean (SD) | 7.9 (16.3) | 9.3 (18.0) | 7.8 (16.2) | 9.5 (18.6) | −.007 | 8.2 (14.7) | 8.8 (15.6) | 8.2 (14.6) | 8.8 (15.5) | −.005 | |
| Fast food restaurant: 1+ | 70.9 | 75.7 | 70.6 | 75.9 | −.004 | 75.9 | 77.7 | 75.7 | 77.8 | −.003 | |
| Park: Mean (SD) | 2.0 (2.7) | 2.3 (2.9) | 1.9 (2.7) | 2.3 (2.9) | −.004 | 2.0 (2.6) | 2.2 (2.8) | 2.0 (2.7) | 2.2 (2.8) | −.004 | |
| Park: 1+ | 59.0 | 64.9 | 58.7 | 65.1 | −.004 | 61.4 | 64.0 | 61.1 | 64.3 | −.007 | |
| Park area (in acres): Mean (SD) | 67.8 (205.1) | 68.5 (183.6) | 67.7 (206.2) | 68.4 (181.6) | .004 | 62.8 (176.7) | 63.3 (170.7) | 62.7 (177.4) | 62.7 (163.0) | .006 | |
| Commercial fitness facility: Mean (SD) | 3.1 (7.0) | 3.4 (6.8) | 3.1 (7.0) | 3.5 (7.0) | −.005 | 3.1 (5.7) | 3.3 (6.0) | 3.1 (5.6) | 3.3 (5.7) | −.004 | |
| Commercial fitness facility: 1+ | 64.5 | 69.1 | 64.3 | 69.6 | −.006 | 68.7 | 70.7 | 68.4 | 71.1 | −.003 | |
Based on MOVE! engagement in any of 6 years (2009–2014)
A total of 1,249 individuals (n=1,168 men and n=81 women) were excluded from the comparison group because they were missing data on census tract poverty rate and/or median household income.
The super cohort lived throughout the continental U.S., as evidenced by their distribution across census divisions, and 77.8% of men and 84.5% of women lived in a metropolitan area (Table 3). Compared to the U.S. population, super cohort members were less likely to live in census tracts that fall in the very lowest decile and two highest deciles of both poverty and median household income (Table 4). About half of the super cohort had at least one supermarket within one mile, while they averaged close to 4 convenience stores (3.6, SD=4.6 for men and 3.9, SD=4.5 for women) and 8 fast food restaurants (7.9, SD=16.3 for men and 8.2, SD=14.7 for women). On average, 2.0 parks (SD=2.7, 2.6 for men and women, respectively) and 3.1 commercial fitness facilities (SD=7.0, 5.7 for men and women, respectively) were available within one mile. Still, 41.0% of men and 38.6% of women did not have a park and 35.5% of men and 31.3% of women did not have a commercial fitness facility within one mile.
Table 4.
Percentage of Super Cohort Members by Gender Who Fall Within General U.S. Population Deciles for Census Tract Poverty Rate and Median Household Income.
| General U.S. Population Census Tract Deciles | Percentage (%) of Cohort Within Each Decile | |||
|---|---|---|---|---|
|
| ||||
| Percent Below Poverty | Median Household Income | |||
|
| ||||
| Men | Women | Men | Women | |
| 1 | 7.7 | 6.9 | 8.6 | 8.2 |
| 2 | 10.2 | 9.9 | 11.4 | 10.5 |
| 3 | 10.9 | 10.6 | 12.3 | 11.8 |
| 4 | 11.8 | 11.8 | 12.0 | 11.7 |
| 5 | 11.5 | 11.5 | 12.2 | 12.2 |
| 6 | 11.6 | 11.9 | 11.2 | 12.0 |
| 7 | 11.1 | 11.7 | 10.3 | 11.0 |
| 8 | 10.4 | 10.6 | 9.6 | 10.4 |
| 9 | 8.5 | 8.7 | 7.7 | 8.2 |
| 10 | 6.3 | 6.4 | 4.5 | 4.2 |
MOVE! engagement and propensity score matching
Approximately 5% of men (n=147,646) and 10% of women (n=22,264) participated in MOVE!. Comparisons of MOVE! participants and those not engaged in MOVE! on select demographics, clinical factors, healthcare utilization, and residential environmental attributes within one mile of home locations before and after matching are also shown in Table 3. The unweighted comparisons reveal that MOVE! participants and non-participants differed on several factors before matching. For example, men who participated in MOVE! were more likely to be midlife (40–69 years of age); non-Hispanic black; have a diagnosis of diabetes, hypertension, hyperlipidemia, and depression; have higher BMI; and meet criteria for obesity. In contrast, after inverse propensity score weighting, descriptive statistics are nearly identical across the variables in the two groups, with all standardized differences well below the commonly accepted criterion of 0.1 indicating an excellent match between the intervention and comparison groups.
Discussion
In response to growing interest in the use of “big data” involving electronic health records to address pressing public health questions,58 this paper provides an overview of the rationale, methods, and cohort characteristics of WAVES I and II, which are exploiting big data to address questions with important implications for policy and weight management programs. This study is being conducted in a cohort of over 3 million U.S. military veterans who used VA healthcare between 2009 and 2014 and who were followed to date through 2015. As evidenced by the descriptive statistics, most of the cohort is men (93.1%) and they tend to be older (men only) with relatively few Hispanics. These demographic patterns reflect veterans as a whole.59,60 However, veterans using VA healthcare are disproportionately non-Hispanic black (especially women) as shown by our summary statistics and tend to be lower income.61 Nonetheless, the cohort does include 1,359,463 persons under age 60, 225,590 women, 546,142 non-Hispanic blacks, and 140,798 Hispanics. Given that 46 million Americans, including disproportionate numbers of African Americans are living in poverty, veterans using VA healthcare represent an important segment of the U.S. population, which is disproportionately at risk for obesity.
We found that the environments where the cohort lived vary. Like all veterans,62 those using VA healthcare,63 particularly men, are more likely to live in rural areas than non-veterans. About 78% of men in the cohort lived in a metropolitan area, as compared to 85% for the U.S. resident population.64 Moreover, cohort members are less likely to live in communities with extreme median household income or poverty rates. Nonetheless, our results show they live in communities that span the urban-rural and economic continuum. Moreover, like the general U.S. population,20,65–69 their environments vary considerably with respect to the geographic accessibility of food and physical activity settings. Many live in areas without environmental resources potentially important for achieving or maintaining a healthy body weight. The environmental variation in the cohort provides ample opportunity to identify how variations in the residential environment is related to BMI, metabolic risk, and weight management program outcomes.
It is noteworthy that 43.6% of men and 42.8% of women in our cohort were obese. Similar to the general U.S. population, obesity rates have climbed among military service members and veterans alike.70 Obesity prevalence among veterans and particularly veterans using VA healthcare may even exceed that of non-veterans.71–74 Obesity-related behaviors (i.e., poor diet, physical inactivity) are thought to contribute to poorer health status observed among veterans and especially veterans using VA health care compared to non-veterans.70,74–78
Despite the high prevalence of obesity, we found less than 5% of men and 10% of women engaged in MOVE! (i.e., completed at least two in-person MOVE! visits within a 6-month period), even though the program is available at no cost to VA healthcare users, available across the 136 healthcare facilities in the continental U.S., and offers in-person and phone sessions. Thus, innovative strategies are needed to positively influence MOVE! program engagement, which our study will address.
Our results suggest our propensity score analysis created a well-matched comparison group for MOVE! participants. Applying the generated propensity score weights in future analyses involving MOVE! will allow us to address innovative questions about whether the environment where people live affects weight management program outcomes, as well as whether specific MOVE! program characteristics can substitute for environmental deficiencies and complement environmental resources to achieve better weight outcomes.
Study strengths
WAVES I and II’s strengths in addressing their aims include research designs and analytic approaches that address potential threats to internal validity. First, because the VA provides continuous integrated healthcare to veterans, many veterans receive care in the VA over most of their adult life. These long-term relationships and VA’s electronic health record have resulted in healthcare data stores that are unparalleled in the U.S. We know of no other nationwide U.S. data source that supports follow-up on millions of adults over this extended period with repeated clinical (rather than self-reported) and environmental measures. Using these longitudinal data, together with our study design, our WAVES I research will overcome many limitations present in the preponderance of prior research on environment-obesity relationships. Within-person repeated measures over 7 years (WAVES I), repeated observations of veterans’ environments, and use of panel data statistical models will allow us to address an often-cited criticism of the extant research: selection bias stemming from the non-random placement of individuals in residential environments. The WAVES I and II data will allow us to use quasi-experimental research designs that account for a broad class of measured and unmeasured individual and environmental factors that may generate bias in simpler research designs. In addition, we will be able to carefully compare the results from study designs that exploit environmental variation that arises from individual migration decisions (following people as they move around the country) and also from processes of environmental change (following non-migrants as the environment changes around them). Research designs based on migration and neighborhood change may be subject to different sources of bias. Together, the two designs may shed important light on the connection between the residential environment and health. Relatedly, these VA healthcare services are provided to veterans at no cost. Thus, we are able to address our study questions in a population for which differential healthcare access is not a likely confounder.
Another strength is the great diversity in residential environments afforded by the study’s nationwide coverage, precise residential location information, and thus the precision of the environmental measures. We are characterizing the environment based on grid-cells (30m × 30m) that are at a fine spatial resolution and time constant for the entire continental U.S. for 7 years. Centering the environmental measures so precisely on individuals’ home locations is still unusual as national U.S. studies typically must rely on administrative units.79 Our study can also simultaneously account for multiple environmental attributes and identify the relative and joint effects of each.
Among the few studies that have examined whether the environment moderates weight management or behavioral (i.e., diet, physical activity) intervention engagement or effectiveness, sample sizes are small, follow-up periods are generally short, there is little variation in intervention characteristics,80 and studies have not been able to control for differences in healthcare access and utilization.34–38 Small sample sizes do not provide the statistical power required to measure such effects. In contrast, WAVES I will determine whether success in the MOVE! weight management program depends on environmental attributes in 169,910 participants plus matched controls. The relatively long follow-up period will also allow us to observe long-term (up to 5 years) moderating effects of environmental exposures on weight management program effectiveness (WAVES I), another unique contribution of the study. Exploiting variation in MOVE! program elements across facilities, WAVES II moves beyond what has been possible to date by examining which specific program elements may substitute for or complement environmental attributes to improve patients’ responses to MOVE!. In the WAVES cohort, there is universal healthcare access, VA imposes no copayment on MOVE! participation, and we will incorporate information on quantity and type (inpatient, outpatient, primary care, specialty care) of care received.
Study limitations
Despite these considerable strengths, WAVES I and II also have several limitations. First, while we have carefully selected a strong research design and analytic approach to promote causal inference, the study remains observational. Randomized control trials, which are practicably quite difficult in neighborhood research, would be needed to test our hypotheses more definitively. Second, we do not have measures of our assumed behavioral mediators (dietary intake, physical activity) of environmental effects on health or weight management program outcomes. We also do not have measures that capture individual-level SES shifts over time such as annual household income. As a result, residual confounding related to within- and between-person differences in SES changes will be a possibility, which we will try to address by controlling for multiple, time-varying local area-level SES measures. Fourth, as discussed above, veterans using VA healthcare are not representative of the U.S. adult population and tend to be male, non-Hispanic and non-Hispanic black (especially women), and of lower income, although there is variation. Fifth, our environmental measures do not capture the “quality” of the environmental settings (e.g., healthy food availability and marketing, park features and upkeep), which may be more influential than their geographic accessibility. Unfortunately, nationwide data on these qualitative features are not available.
Finally, our large sample is a considerable strength, providing ample statistical power to detect small effects common in research on the residential environment including in important subgroups. However, our sample size can lead to statistically significant associations that are not substantively important. Thus, we will interpret our findings in terms of both clinical and policy relevance. With respect to clinical relevance, we will compare our effects to a 5% weight change, which is considered clinically significant.81 With respect to the policy relevance, prior research can help place our results in context. For example, a recent study found that one-third of U.S. adults consumed fast food on a given day and that fast food consumption was associated with consumption of 194 additional calories on these days.82 Simple calculations imply that consuming an extra 194 calories per day could annually lead to a 6.7-pound weight gain, which is about 1 BMI unit for an average person. This suggests that a policy that reduced fast food consumption by about 10% (which would be quite a substantial economic effect) would reduce a person’s BMI by about 0.1 BMI units over the course of a year. While these calculations are crude, they can help put forthcoming findings in perspective. We should expect most environmental attributes to generate relatively small absolute effects on BMI; however, comprehensive changes across the environment may cumulatively contribute to large reductions in BMI.
Conclusion
Despite these limitations, drawing on a sample of over 3 million adults with clinically-measured outcomes and nationwide geographic coverage, WAVES I and II have tremendous potential to produce vital evidence to select the most promising targets of policy and environmental interventions and to enhance the design of behavioral weight management programs to achieve healthier body weights nationwide in the U.S.
Supplementary Material
SO WHAT?
What is already known on this topic?
Despite tremendous investment in obesity research, weight loss treatments have had limited success in terms of individual and population improvements in body weight. Moreover, the role of the environment in body weight and weight loss remains unclear.
What does this article add?
This article describes the rationale, methods, and cohort characteristics for two complementary cohort studies at the forefront of “big data” research linking electronic health record data with public and proprietary environmental data to determine impacts of residential environmental attributes on body weight, metabolic risk, and participation in and effectiveness of a nationwide weight management program.
What are the implications for health promotion practice or research?
These studies have tremendous potential to produce vital evidence to select the most promising targets of policy and environmental interventions and to enhance the design of behavioral weight management programs to achieve healthier body weights nationwide in the U.S.
Acknowledgments
This research was funded by the National Cancer Institute (R01CA172726) and the U.S. Department of Veterans Affairs (HSR&D IIR 13-085).
Contributor Information
Shannon N. Zenk, University of Illinois at Chicago College of Nursing, 845 S. Damen Ave., Chicago, IL 60612 USA; Phone: (312) 355-2790; Fax: (312) 996-7725.
Elizabeth Tarlov, Center of Innovation for Complex Chronic Healthcare (CINCCH), Hines VA Hospital, 5000 S. 5th Ave., Hines, IL 60141 USA; University of Illinois at Chicago College of Nursing, 845 S. Damen Ave., Chicago, IL 60612 USA; Phone: (708) 202-2254; Fax: (708) 202-2316.
Lisa M. Powell, University of Illinois at Chicago School of Public Health, 1603 W. Taylor St., Chicago, IL 60612 USA; Phone: (312) 413-8468; Fax: (312) 996-2703.
Coady Wing, Indiana University-Bloomington School of Public and Environmental Affairs, 1315 E. 10th St., Bloomington, IN 47405 USA; Phone: (812) 855-0563; Fax: (812) 855-7802.
Stephen A. Matthews, The Pennsylvania State University, Department of Sociology, Anthropology, and Demography, 211 Oswald Tower, University Park, PA 16802 USA; Phone: (814) 863-9721; Fax: (814) 863-7216.
Sandy Slater, University of Illinois at Chicago School of Public Health, 1603 W. Taylor St., Chicago, IL 60612 USA; Phone: (312) 413-0475; Fax: (312) 996-2703.
Howard S. Gordon, Jesse Brown VA Medical Center, 820 S. Damen Ave., Chicago, IL 60612 USA; University of Illinois at Chicago Department of Medicine, 1747 W. Roosevelt Ave., Chicago, IL 60608 USA; Phone: (312) 569-7473; Fax: (312) 569-8114.
Michael Berbaum, University of Illinois at Chicago Institute for Health Research and Policy, 1747 W. Roosevelt Rd., Chicago, IL 60608 USA; Phone: (312) 413-0476; Fax: (312) 413-1221.
Marian L. Fitzgibbon, University of Illinois at Chicago Institute for Health Research and Policy, 1747 W. Roosevelt Rd., Chicago, IL 60608 USA; Phone: (312) 996-0146; Fax: (312) 413-8950.
References
- 1.Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012;31(1):219–230. doi: 10.1016/j.jhealeco.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Preston SH, Stokes A. Contribution of obesity to international differences in life expectancy. Am J Public Health. 2011;101(11):2137–43. doi: 10.2105/AJPH.2011.300219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med. 2003;348(17):1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 4.Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. Body fatness and cancer—Viewpoint of the IARC working group. N Engl J Med. 2016;375(8):794–798. doi: 10.1056/NEJMsr1606602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.di Angelantonio E, Bhupathiraju SN, Wormser D, et al. Body mass index and all-cause mortality: individual participant data meta-analysis of 239 prospective studies in four continents. The Lancet. 2016 doi: 10.1016/S0140-6736(16)30175-1. online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005–2008) J Rural Health. 2012;28(4):392–397. doi: 10.1111/j.1748-0361.2012.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 8.Ljungvall Å, Zimmerman FJ. Bigger bodies: long-term trends and disparities in obesity and body-mass index among US adults, 1960–2008. Soc Sci Med. 2012;75(1):109–119. doi: 10.1016/j.socscimed.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Franz MJ, Boucher JL, Rutten-Ramos S, VanWormer JJ. Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. J Acad Nutr Diet. 2015;115(9):1447–1463. doi: 10.1016/j.jand.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 11.Wadden TA, West DS, Neiberg RH, et al. One-year weight losses in the look AHEAD study: factors associated with success. Obesity. 2009;17(4):713–722. doi: 10.1038/oby.2008.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wing RR, Hamman RF, Bray GA, et al. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obesity. 2004;12(9):1426–1434. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Middleton KM, Patidar SM, Perri MG. The impact of extended care on the long-term maintenance of weight loss: a systematic review and meta-analysis. Obes Rev. 2012;13(6):509–517. doi: 10.1111/j.1467-789X.2011.00972.x. 1467–789. [DOI] [PubMed] [Google Scholar]
- 14.Barte J, Ter Bogt N, Bogers R, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obes Rev. 2010 doi: 10.1111/j.1467-789X.2010.00740.x. [DOI] [PubMed] [Google Scholar]
- 15.MacLean PS, Wing RR, Davidson T, et al. NIH working group report: Innovative research to improve maintenance of weight loss. Obesity. 2015;23(1):7–15. doi: 10.1002/oby.20967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100(4):590–95. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. Milbank Q. 2009;87(1):123–154. doi: 10.1111/j.1468-0009.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 19.Zenk SN, Powell LM, Rimkus L, et al. Relative and absolute availability of healthier food and beverage alternatives across communities in the United States. Am J Public Health. 2014;104(11):2170–2178. doi: 10.2105/AJPH.2014.302113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007;44(3):189–195. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 21.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the US. Am J Prev Med. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 22.Bowen DJ, Barrington WE, Beresford SA. Identifying the effects of environmental and policy change interventions on healthy eating. Annu Rev Public Health. 2015;36(1):289–306. doi: 10.1146/annurev-publhealth-032013-182516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mozaffarian D, Afshin A, Benowitz NL, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126(12):1514–1563. doi: 10.1161/CIR.0b013e318260a20b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shulaker BD, Isacoff JW, Cohen DA, Marsh T, Wier M, Bhatia R. Partnerships for parks and physical activity. Am J Health Promot. 2014;28(3):S97–S99. doi: 10.4278/ajhp.130430-ARB-215. [DOI] [PubMed] [Google Scholar]
- 25.Steeves EA, Martins PA, Gittelsohn J. Changing the food environment for obesity prevention: Key gaps and future directions. Curr Obes Rep. 2014;3:451–458. doi: 10.1007/s13679-014-0120-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berrigan D, Hipp JA, Hurvitz PM, et al. Geospatial and contextual approaches to energy balance and health. Annals of GIS. 2015;21(2):157–168. doi: 10.1080/19475683.2015.1019925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bancroft C, Joshi S, Rundle A, et al. Association of proximity and density of parks and objectively measured physical activity in the United States: a systematic review. Soc Sci Med. 2015;138:22–30. doi: 10.1016/j.socscimed.2015.05.034. [DOI] [PubMed] [Google Scholar]
- 28.Cobb LK, Appel LJ, Franco M, Jones-Smith JC, Nur A, Anderson CA. The relationship of the local food environment with obesity: a systematic review of methods, study quality, and results. Obesity. 2015;23(7):1331–1344. doi: 10.1002/oby.21118. 1930–739; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff. 2014;33(2):283–201. doi: 10.1377/hlthaff.2013.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferdinand AO, Sen B, Rahurkar S, Engler S, Menachemi N. The relationship between built environments and physical activity: A systematic review. Am J Public Health. 2012;102(10):e7–e13. doi: 10.2105/AJPH.2012.300740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes Rev. 2011;12(3):217–230. doi: 10.1111/j.1467-789X.2010.00726.x. [DOI] [PubMed] [Google Scholar]
- 32.Mackenbach JD, Rutter H, Compernolle S, et al. Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health. 2014;14:233. doi: 10.1186/1471-2458-14-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zenk SN, Thatcher E, Reina M, Odoms-Young A. 6 local food environments and diet-related health outcomes. In: Morland K, editor. Local Food Environments: Food Access in America. Baton Rouge, FL: CRC Press; 2014. pp. 167–204. [Google Scholar]
- 34.Feathers A, Aycinena AC, Lovasi GS, et al. Food environments are relevant to recruitment and adherence in dietary modification trials. Nutr Res. 2015;35(6):480–488. doi: 10.1016/j.nutres.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gustafson AA, Sharkey J, Samuel-Hodge CD, Jones-Smith JC, Cai J, Ammerman AS. Food store environment modifies intervention effect on fruit and vegetable intake among low-income women in North Carolina. J Nutr Metab. 2012 doi: 10.1155/2012/932653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kerr J, Norman GJ, Adams MA, et al. Do neighborhood environments moderate the effect of physical activity lifestyle interventions in adults? Health Place. 2010;16(5):903–908. doi: 10.1016/j.healthplace.2010.05.002. doi: http://dx.doi.org/10.1016/j.healthplace.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wedick NM, Ma Y, Olendzki BC, et al. Access to healthy food stores modifies effect of a dietary intervention. Am J Prev Med. 2015;48(3):309–317. doi: 10.1016/j.amepre.2014.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zenk SN, Wilbur J, Wang E, et al. Neighborhood environment and adherence to a walking intervention in African American women. Health Educ Behav. 2009;36(1):167–181. doi: 10.1177/1090198108321249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. Vol. 4. John Wiley & Sons; 2008. pp. 465–486. [Google Scholar]
- 40.Stokols D. Establishing and maintaining healthy environments. toward a social ecology of health promotion. Am Psychol. 1992;47(1):6–22. doi: 10.1037//0003-066x.47.1.6. 0003-066; 0003-066. [DOI] [PubMed] [Google Scholar]
- 41.Grossman M. On the concept of health capital and the demand for health. J Polit Economy. 1972;80(2):223–255. [Google Scholar]
- 42.Hamman RF, Wing RR, Edelstein SL, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29(9):2102–07. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jones K. MOVE! weight management program for veterans. National MOVE! Education Meeting presentation; 2012. [Google Scholar]
- 44.Kinsinger LS, Jones KR, Kahwati L, et al. Design and dissemination of the MOVE! weight-management program for veterans. Prev Chronic Dis. 2009;6(3):A98. [PMC free article] [PubMed] [Google Scholar]
- 45.United States Department of Agriculture. [Accessed 12/12, 2016];Choose My Plate. https://www.choosemyplate.gov/. Updated 2016.
- 46.U.S. Department of Veteran Affairs. [Accessed 12/12, 2016];Management of obesity and overweight. http://www.healthquality.va.gov/guidelines/CD/obesity/. Updated 2014.
- 47.Loughran DS. Wage growth in the civilian careers of military retirees. Santa Monica, CA: Rand Corp; 2002. [Google Scholar]
- 48.MacLean A, Edwards RD. The pervasive role of rank in the health of US veterans. Armed Forces Soc. 2010;36(5):765–785. doi: 10.1177/0095327X09356166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.MacLean A. The privileges of rank. Armed Forces & Society. 2008;34(4):682–713. doi: 10.1177/0095327X07310336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.U.S. Department of Defense. [Accessed 05/19, 2016];Official site of the ASVAB testing program. http://official-asvab.com/index.htm. Updated 2012.
- 51.U.S. Department of Defense. [Accessed 01/28, 2012];ASVAB validity information. http://official-asvab.com/validity_res.htm. Updated 2012.
- 52.Welsh JR, Kucinkas SK, Curran LT. Armed services vocational aptitude battery (ASVAB): Integrative review of validity studies. Brooks AFB, TX: Air Force Human Resources Laboratory, Air Force Systems Command; 1990. [Google Scholar]
- 53.US Department of Veterans Affairs Information Resource Center. VIReC research user guide: PSSG geocoded enrollee files, 2015 edition. 2016. [Google Scholar]
- 54.Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat. 2014;2(166):1–73. [PubMed] [Google Scholar]
- 55.Sallis JF, Cervero R, Ascher W, Henderson K, Kraft M, Kerr J. An ecological approach to creating active living communities. Annu Rev Public Health. 2006;27:297–322. doi: 10.1146/annurev.publhealth.27.021405.102100. [DOI] [PubMed] [Google Scholar]
- 56.Kahwati LC, Lance T, Jones KR, Kinsinger LS. RE-AIM evaluation of the Veterans Health Administration’s MOVE! weight management program. Transl Behav Med. 2011;1(4):550–560. doi: 10.1007/s13142-011-0077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Casey JA, Schwartz BS, Stewart WF, Adler NE. Using electronic health records for population health research: a review of methods and applications. Annu Rev Public Health. 2016;37:61–81. doi: 10.1146/annurev-publhealth-032315-021353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.United States Census Bureau/American FactFinder. B21001I: SEX BY AGE BY VETERAN STATUS FOR THE CIVILIAN POPULATION 18 YEARS AND OVER (HISPANIC OR LATINO) [Accessed December, 2016];2015 American Community Survey 1-year estimates. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_1YR_B21001I&prodType=table. Updated 2015.
- 60.United States Census Bureau/American FactFinder. B21001: SEX BY AGE BY VETERAN STATUS FOR THE CIVILIAN POPULATION 18 YEARS AND OVER. [Accessed December, 2016];2015 American Community Survey 1-year estimates. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_1YR_B21001&prodType=table. Updated 2015.
- 61.Wilson NJ, Kizer KW. The VA health care system: An unrecognized national safety net. Health Aff (Millwood) 1997;16(4):200–204. doi: 10.1377/hlthaff.16.4.200. [DOI] [PubMed] [Google Scholar]
- 62.U.S. Department of Veteran Affairs: National Center for Veterans Analysis and Statistics. [Accessed August, 2016];Profile of veterans: 2014 data from the American Community Survey. https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2014.pdf. Updated 2016.
- 63.US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. 2013 NCHS urban-rural classification scheme for counties. 2014. [Google Scholar]
- 64.Centers for Disease Control and Prevention. [Accessed 12/12, 2016];NCHS urban-rural classification scheme for counties. http://www.cdc.gov/nchs/data_access/urban_rural.htm. Updated 2014.
- 65.Powell LM, Slater S, Chaloupka FJ, Harper D. Availability of physical activity-related facilities and neighborhood demographic and socieconomic characteristics: a national study. Am J Public Health. 2006;96(9):1676–1680. doi: 10.2105/AJPH.2005.065573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Powell LM, Chaloupka FJ, Bao Y. The availability of fast-food and full-service restaurants in the United States: associations with neighborhood characteristics. Am J Prev Med. 2007;33(4 Suppl):S240–5. doi: 10.1016/j.amepre.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 67.Wen M, Zhang X, Harris CD, Holt JB, Croft JB. Spatial disparities in the distribution of parks and green spaces in the USA. Ann Behav Med. 2013;45(S1):18–27. doi: 10.1007/s12160-012-9426-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Richardson AS, Boone-Heinonen J, Popkin BM, Gordon-Larsen P. Are neighbourhood food resources distributed inequitably by income and race in the USA? Epidemiological findings across the urban spectrum. BMJ Open. 2012;2(2) doi: 10.1136/bmjopen-2011-000698. e000698-2011-000698. Print 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bower KM, Thorpe RJ, Rohde C, Gaskin DJ. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Prev Med. 2014;58:33–39. doi: 10.1016/j.ypmed.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rush T, LeardMann CA, Crum-Cianflone NF. Obesity and associated adverse health outcomes among US military members and veterans: findings from the Millennium Cohort Study. Obesity. 2016;24(7):1582–1589. doi: 10.1002/oby.21513. [DOI] [PubMed] [Google Scholar]
- 71.Koepsell TD, Littman AJ, Forsberg CW. Obesity, overweight, and their life course trajectories in veterans and non-veterans. Obesity. 2012;20(2):434–439. doi: 10.1038/oby.2011.2. [DOI] [PubMed] [Google Scholar]
- 72.Lehavot K, Hoerster KD, Nelson KM, Jakupcak M, Simpson TL. Health indicators for military, veteran, and civilian women. Am J Prev Med. 2012;42(5):473–480. doi: 10.1016/j.amepre.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 73.Hoerster KD, Lehavot K, Simpson T, McFall M, Reiber G, Nelson KM. Health and health behavior differences: US military, veteran, and civilian men. Am J Prev Med. 2012;43(5):483–489. doi: 10.1016/j.amepre.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 74.Nelson KM. The burden of obesity among a national probability sample of veterans. J Gen Intern Med. 2006;21(9):915–919. doi: 10.1111/j.1525-1497.2006.00526.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kazis LE, Ren XS, Lee A, et al. Health status in VA patients: Results from the Veterans’ Health Study. Am J Med Qual. 1999;14(1):28–38. doi: 10.1177/106286069901400105. [DOI] [PubMed] [Google Scholar]
- 76.Selim AJ, Berlowitz DR, Fincke G, et al. The health status of elderly veteran enrollees in the Veterans Health Administration. J Am Geriatr Soc. 2004;52(8):1271–1276. doi: 10.1111/j.1532-5415.2004.52355.x. [DOI] [PubMed] [Google Scholar]
- 77.Kramarow EA, Pastor PN. The health of male veterans and non-veterans aged 25–64, United States, 2007–2010. Citeseer: 2012. [PubMed] [Google Scholar]
- 78.Haibach JP, Haibach MA, Hall KS, et al. Military and veteran health behavior research and practice: challenges and opportunities. J Behav Med. 2016:1–19. doi: 10.1007/s10865-016-9794-y. [DOI] [PubMed] [Google Scholar]
- 79.Martin D. Geographic information systems: Socioeconomic applications. Psychology Press; 1996. [Google Scholar]
- 80.Mendez DD, Gary-Webb TL, Goode R, et al. Neighborhood factors and six-month weight change among overweight individuals in a weight loss intervention. Prev Med Rep. 2016;4:569–573. doi: 10.1016/j.pmedr.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25_PA) doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 82.Powell LM, Nguyen BT, Han E. Energy intake from restaurants: demographics and socioeconomics, 2003–2008. Am J Prev Med. 2012;43(5):498–504. doi: 10.1016/j.amepre.2012.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.