Abstract
Background
Optimization of care to correct the unilateral cleft lip nasal deformity is hampered by lack of objective measures to quantify pre-operative severity and outcome.
The purpose of this study was to: develop a consensus standard of nasal appearance using 3D stereophotogrammetry; determine if anthropometric measurements could be used to quantify severity and outcome; and determine if pre-operative severity predicts post-operative outcome.
Methods
We collected facial 3D images of 100 subjects in three groups: 45 infants before cleft lip repair; the same 45 infants after cleft lip repair; and 45 children age 8–10 years with previous repairs. Five additional age-matched unaffected control subjects were included in each group.
Seven expert surgeons ranked images in each group according to nasal appearance. The rank sum score was used as consensus standard. Anthropometric analysis was performed on each image and compared to the rank sum score. Pre-operative rank and anthropometric measurements were compared to post-operative rank.
Results
Inter-rater and intra-rater reliability was excellent (ICC>0.76 and Pearson correlation >0.75 respectively) on each of the 3 image sets.
Columellar angle, nostril width ratio, and lateral lip height ratio were highly correlated with pre-operative severity and moderately correlated with post-operative nasal appearance.
Post-operative outcome was associated with pre-operative severity (rank and anthropometric measurement).
Conclusions
Consensus ranking of pre-operative severity and post-operative outcome can be achieved on 3d images. Pre-operative severity predicts post-operative outcomes. Columellar angle, nostril width ratio, and lateral lip height ratio are objective measures that correlate with consensus ratings by surgeons at multiple ages.
Introduction
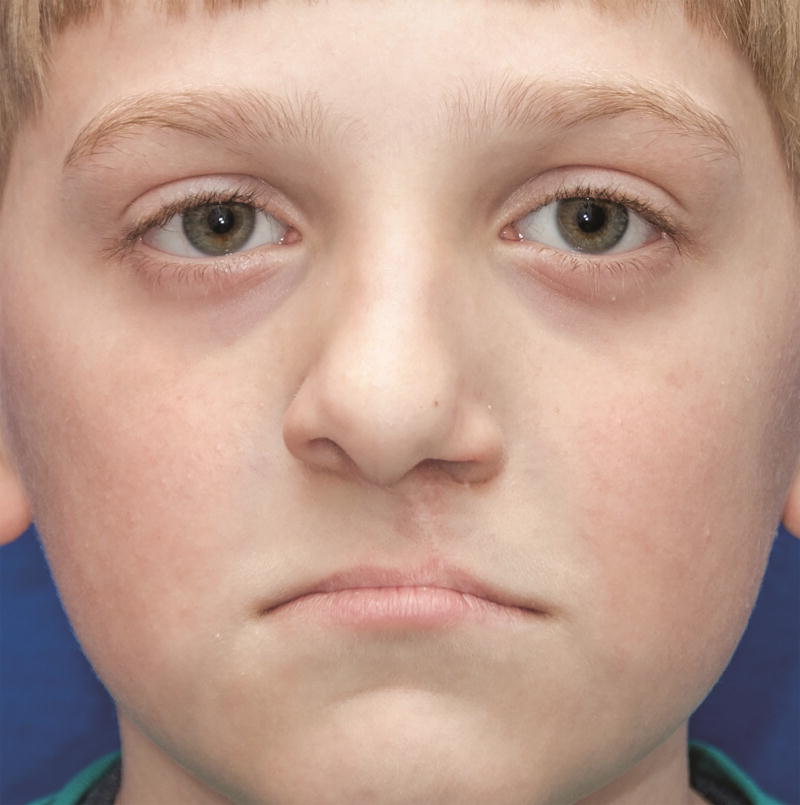
The presence of a cleft lip results in a complex 3-dimensional facial deformity that has significant functional, esthetic, and social ramifications. While favorable correction of the lip deformity can often be achieved in a single stage, correction of the nasal deformity remains a challenge and recurrence is common. To varying degrees, the cleft splays the base elements of the nose, thereby resulting in collapse of the arch structures that define the tip and ala1. In the case of the unilateral cleft lip nasal deformity (uCLND), displacement of the caudal septum results in angulation of the columella on submental view and twisting of the dorsum on frontal view (Figure 1). Significant changes can be produced surgically (Figure 2), however, residual or recurrent deformity is often present and can be accentuated with further time and growth (Figure 3)
Figure 1. Unilateral cleft lip nasal deformity.
Pre-op: Displacement of the anterior nasal spine results in twisted deformity of nose and collapse of columella and nasal arch forms.
Figure 2. Unilateral cleft lip nasal deformity.
Post-op: Significant correction has been achieved following primary cleft lip repair and primary septoplasty (same patient as in Figure 1).
Figure 3. Unilateral cleft lip nasal deformity.
Age 8–10 years: Residual or recurrent nasal deformity can become more apparent with time and growth (different patient than in Figures 1 and 2).
Correction of the uCLND occurs over multiple stages. The initial cleft lip repair may be combined with primary rhinoplasty and/or primary septoplasty. Additional treatments may include nasoalveolar molding, early tip rhinoplasty, septorhinoplasty, and secondary revisions. Other treatments that can alter the nose include alveolar bone grafting and orthognathic surgery. There is no consensus on treatment that optimizes outcomes and minimizes the burden of care. In part, this is due to a lack of objective measures to track changes through longitudinal care. Current rating scales do not take into account pre-operative deformities2 and the multitude of proposed, but unvalidated rating systems, suggests a lack of consensus in the subjective scoring of facial aesthetics3. Measurements on 2 dimensional photos are prone to error from parallax4 and direct anthropometric analysis or nasolabial casts are impractical. As a result, many decisions in care tend to be based upon experience and expert opinion, and, consequently, many controversies continue to exist.
Recent advances in 3D stereophotogrammetry have made rapid and convenient capture of 3D form widely available. Measurements using this technology have been found to be accurate5 and anthropometric analysis has been used to study to children who have previously undergone cleft lip repair6–16. However, a system of meaningful objective analysis of uCLND is still lacking. Many dimensions can be measured on a 3D image, but which one of the many measurements is actually useful in determining pre-operative severity and post-operative success? Even more fundamental is how we might define severity and outcome and whether pre-operative severity influences post-operative outcome.
The first part of this study was designed to determine if a qualitative consensus of pre-operative severity, post-cheiloplasty outcome, and late outcome of CLND could be obtained on 3D images. No such consensus has previously been obtained. The second part was to determine if quantitative anthropometric measurements were predictive of the qualitative consensus. If so, these measurements could be used as valid objective measures. The third part was to determine if pre-operative severity was predictive of post-operative outcome. While varying hypotheses have been proposed, little evidence to link the two exists. Together, these would be significant strides in objectifying esthetic outcome and progressing our field to evidence-based practice.
Methods
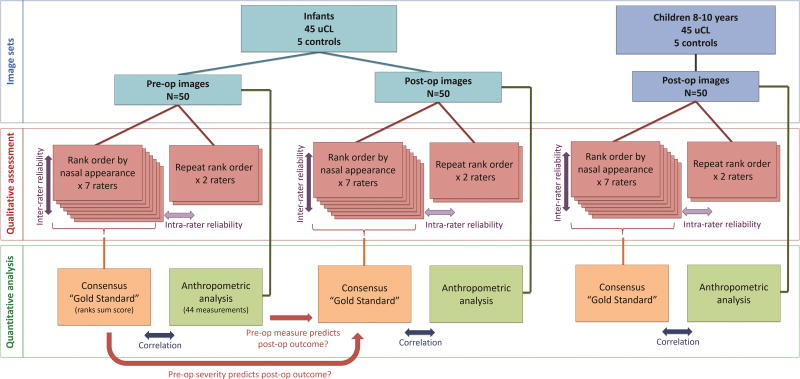
Our Institutional Review Board approved this study. Written informed consent was obtained for each subject enrolled. Overall study design is summarized in Figure 4.
Figure 4. Study Design.
The purposes of this study were to determine if expert cleft surgeons could reliably rank nasal appearance of infants before cleft lip repair, after cleft lip repair and at 8–10 years of age; to determine if objective anthropometric were predictive of the consensus rankings; to determine if pre-operative severity or objective measures of pre-op severity predicted post-operative outcome.
Subjects and image acquisition
We recruited 45 infants undergoing unilateral cleft lip repair and 5 age-matched unaffected control subjects (Group A). To assess the post-operative changes that may occur with further time and growth, we also recruited 45 children aged 8–10 years with previously repaired unilateral cleft lip as well as 5 age-matched unaffected controls (Group B). Consecutive eligible patients presenting to our center were invited to participate. Of 104 families approached, 100 agreed to participate.
Subject images were captured by a professional image technologist using the 3dMDCranial system (3dMD, Atlanta, Ga.), according to standard guidelines17. 3D images were collected before and after primary cleft lip repair for Group A, and at the time of recruitment for Group B (prior 3D images were not available for Group B participants). We therefore produced 3 image sets, each containing 50 subject images (Figure 4): Group A Infants pre-op, Group A Infants post-op, Group B Children 8–10 years old.
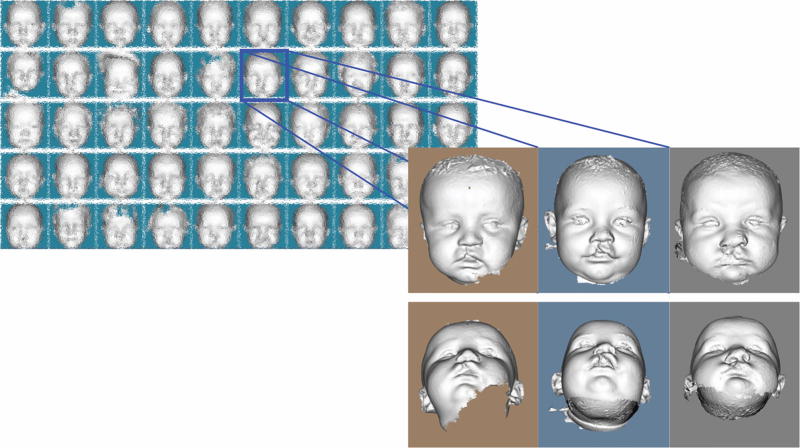
The 3D images were processed using previously developed software18 that extracts the face (removing body, neck, clothing, etc. from the image) and aligns them to a standard facial frontal plane.
Assessment of CLND
We recruited 7 expert full-time cleft surgeons (the Americleft Task Force Surgeon Subgroup), who were from different high-volume North American cleft centers, to provide expert assessments. Each expert individually ranked the 50 images contained within an image set, in the order of best to worst nasal appearance. We used software that presented the rater with a randomized initial order of 3D images on a “sorting board” and allowed 3D rendering of each mesh and its neighbors (Figure 5). Raters viewed full-face mesh only images.
Figure 5. Ranking interface for 3D.
(a) The main screen allowed users to change the order of the images by dragging and dropping any image to desired location. (b) To enable a detailed comparison of the nasal shape, 3D rendering of an image with two neighboring images was provided when it was selected.
Each of the 3 image sets (each containing 50 images) was assessed by each of the 7 surgeons thereby producing 1050 rank scores. Rankings by each surgeon were compared to determine inter-rater reliability. Two surgeons repeated the rankings for each of the 3 image sets after a 2-month washout period to produce another 300 rank scores so that an estimate of intra-rater reliability could also be obtained.
We anticipated some variability in rankings provided by the experts and planned to obtain consensus by pooling their assessments. Individual rankings from surgeons were summed for each image to produce a rank sum score that would serve as the “gold standard”
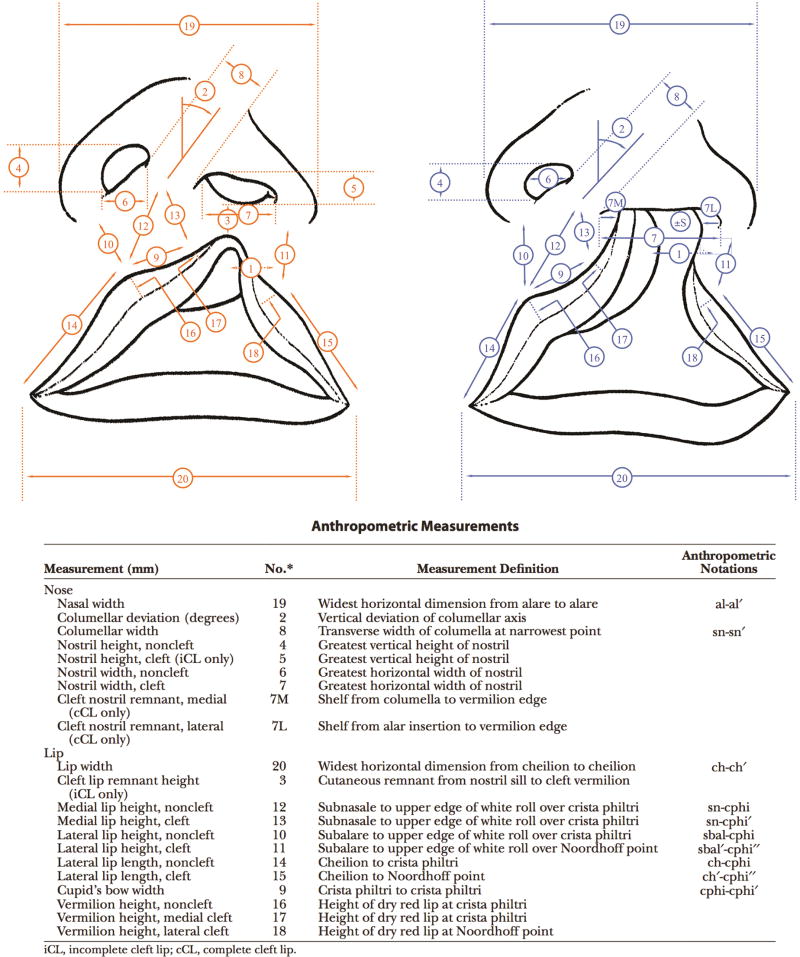
Anthropometric Measurements
We performed conventional indirect anthropometric analysis (Figure 6) on each of the 145 images5,19 to obtain objective measures of form. Forty-four anthropometric landmarks were placed and inter-landmark distances or angles were calculated on the images using 3dMDvultus software. In order to control for variation amongst individuals and to focus on aberrations of form, anthropometric distances were translated to ratios of cleft side to non-cleft side for further analysis.
Figure 6. Anthropometric measurements.
(Adapted from Tse R, Booth L, Keys K, Saltzman B, Stuhaug E, Kapadia H, Heike C. Reliability of Nasolabial Anthropometric Measures Using Three-Dimensional Stereophotogrammetry in Infants with Unrepaired Unilateral Cleft Lip. Plast Reconstr Surg. 2014; 133(4):530e-42e)
The level of importance of each objective measure was determined by calculating the correlation with the rank sum “gold standard”.
Statistical Analysis
Reliability of expert rank assessments of nasal form was assessed using intra-class correlation coefficient for inter-rater reliability and Pearson’s correlation for intra-rater reliability. The correlation of anthropometric measurements to the ranked severity standard was determined using Pearson’s correlation. The relationship between pre-operative severity and post-operative outcome was determined using Pearson’s correlation.
Results
Subjects
Demographics of the 100 subjects are summarized in Table 1. The types of cleft lip and cleft extent were consistent with the presentation normally seen at our center. The majority of children 8–10 years old had complete cleft lip and palate and only one child had an incomplete cleft lip. Although the distribution for these children does not match that seen at initial presentation, it is consistent with the demographics of children who are returning to our center at age 8–10 years for ongoing care.
Table 1.
Subject demographics, cleft type and extent.
|
|
|
|||||
|---|---|---|---|---|---|---|
| Group A | Group B* | |||||
|
|
|
|||||
| Infant Pre- Repair |
Infant Post- repair |
Infant Control |
8–10 y Post-repair |
8–10 y Control |
||
| Mean age at photo | 7.5 months | 10 months | 5.5 months | 9.5 years | 9 years | |
| Standard deviation | 7 months | 10 months | 1 month | 1.5 years | 0.7 years | |
| Sex | ||||||
| Male | 32 (71%) | 32 (71%) | 4 (80%) | 27 (61%) | 2 (40%) | |
| Female | 13 (29%) | 13 (29%) | 1 (20%) | 17 (39%) | 3 (60%) | |
| Ethnicity | ||||||
| Caucasian | 27 (60%) | 27 (60%) | 2 (40%) | 17 (39%) | 4 (80%) | |
| Asian | 4 (9%) | 4 (9%) | 1 (20%) | 19 (43%) | 0 (0%) | |
| Latino | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (20%) | |
| Native American | 0 (0%) | 0 (0%) | 0 (0%) | 1 (2%) | 0 (0%) | |
| Mixed Caucasian | ||||||
| Caucasian/Asian | 1 (2%) | 1 (2%) | 1 (20%) | 2 (5%) | 0 (0%) | |
| Caucasian/Indian | 1 (2%) | 1 (2%) | 1 (20%) | 0 (0%) | 0 (0%) | |
| Caucasian/Hawaiian | 1 (2%) | 1 (2%) | 0 (0%) | 1 (2%) | 0 (0%) | |
| Caucasian/Other | 1 (2%) | 1 (2%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Other | 7 (16%) | 7 (16%) | 0 (0%) | 2 (5%) | 0 (0%) | |
| Did not indicate | 3 (7%) | 3 (7%) | 0 (0%) | 2 (5%) | 0 (0%) | |
| Cleft Side | ||||||
| Left | 25 (56%) | 25 (56%) | NA | 33 (75%) | NA | |
| Right | 20 (44%) | 20 (44%) | NA | 11 (25%) | NA | |
| Cleft Type | ||||||
| Complete | 15 (31%) | 15 (31%) | NA | 41 (93%) | NA | |
| Complete + band** | 6 (13%) | 6 (13%) | NA | 2 (5%) | NA | |
| Incomplete | 24 (53%) | 24 (53%) | NA | 1 (2%) | NA | |
| Cleft Extent | ||||||
| Cleft Lip | 15 (33%) | 15 (33%) | NA | 6 (14%) | NA | |
| Cleft Lip and Alveolus | 5 (11%) | 5 (11%) | NA | 2 (5%) | NA | |
| Cleft Lip and Palate | 25 (56%) | 25 (56%) | NA | 36 (82%) | NA | |
| Associated Syndrome | 4† (9%) | 4 (9%) | NA | 2‡ (5%) | NA | |
Pre-repair images for Group B were not available for analysis. One subject was excluded from the study due to an image quality problem, resulting in a final set of 44 8–10y subjects post-repair.
Band (a.k.a. Simonart band) was defined as any soft tissue found across the cleft in the presence of a complete cleft of alveolus.
Popliteal pterygium syndrome, bilateral hand and foot syndactyly, cardiac anomalies, EEC.
Van der Woode syndrome.
Image set rankings
Each rater required approximately one hour to rank each set of 50 images. Subjectively, each rater found the Infants pre-op easiest to compare followed by the Children 8–10 years old. All raters found the Infants post-op the most difficult to compare due to the similarities in appearance. For each image set, the control subjects were assessed to have the best nasal appearance.
1. Reliability of image set assessments
Infants Pre-op
For pre-operative severity of the cleft nasal deformity, the inter-rater reliability of individual raters was consistently excellent with correlation coefficients of >0.9 when individual raters were compared (Table 2). The Intra-class correlation incorporating rankings performed by all of the raters was extremely high at 0.93. Intra-rater reliability on repeat assessment was also extremely high with correlation coefficients of 0.91 and 0.95.
Table 2.
Rater Reliability assessing nasal appearance for each of three image sets (Pearson correlation coefficients, p < 0.01)
| Infant Pre-op (n=50) | Infant Post-op (n=50) | 8–10yo Post-op (n=50) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| Surgeon | S2 | S3 | S4 | S5 | S6 | S7 | S2 | S3 | S4 | S5 | S6 | S7 | S2 | S3 | S4 | S5 | S6 | S7 |
| S1 | .95 | .95 | .94 | .93 | .95 | .95 | .72 | .57 | .71 | .55 | .75 | .75 | .83 | .85 | .83 | .86 | .88 | .83 |
| S2 | .92 | .91 | .88 | .94 | .92 | .65 | .74 | .68 | .76 | .76 | .77 | .79 | .80 | .82 | .85 | |||
| S3 | .92 | .93 | .94 | .95 | .60 | .54 | .70 | .71 | .70 | .81 | .88 | .78 | ||||||
| S4 | .91 | .91 | .94 | .66 | .77 | .79 | .79 | .83 | .83 | |||||||||
| S5 | .92 | .92 | .63 | .64 | .83 | .80 | ||||||||||||
| S6 | .93 | .87 | .87 | |||||||||||||||
|
|
|
|
||||||||||||||||
| Repeat | .91 | .95 | .76 | .94 | .80 | .88 | ||||||||||||
s=surgeon
Infants Post-op
The agreement on assessment post-op was not as strong but was nonetheless consistently very good (Table 2) with correlation coefficients ranging from 0.55 to 0.79 and with an Intra-class correlation of 0.70. Intra-rater reliability was also very good with correlation coefficient of 0.76 and 0.94.
Children 8–10 years old
The inter-rater reliability on assessment was consistently excellent (Table 2) with correlation coefficients ranging from 0.70 to 0.88 and with an Intra-class correlation of 0.82. Intra-rater reliability was also excellent with correlation coefficients of 0.80 and 0.88.
2. Anthropometric Measurements
Table 3 summarizes the correlation of anthropometric measurements on individual images with the rank sum score. Columellar angle, nostril width ratio, and lateral lip height ratio were the strongest predictors of the expert rankings.
Table 3.
Correlation of anthropometric measurements and the expert consensus (rank sum score) of nasal appearance using Pearson correlation coefficient
| Infants Pre-op |
Infants Post-op |
8–10 yo Post-op |
|
|---|---|---|---|
| Columellar angle | −0.72* | −0.22 | −0.51* |
| Cleft/Non-Cleft Nostril Width Ratio | −0.80* | −0.34* | −0.41* |
| Cleft/Non-Cleft Nostril Height Ratio† | 0.41* | −0.20 | 0.15 |
| Cleft/Non-Cleft Nostril Height Ratio (NNCL method) | 0.40* | −0.23 | 0.12 |
| Cleft/Non-Cleft Medial Lip Height Ratio | 0.41* | −0.29 | −0.20 |
| Cleft/Non-Cleft Lateral Lip Length Ratio | −0.06 | −0.12 | 0.02 |
| Cleft/Non-Cleft Lateral Lip Height Ratio | 0.79* | 0.42* | 0.16 |
| Lip/Nasal Width Ratio | 0.04 | −0.05 | 0.18 |
Each image set included 45 subjects with unilateral cleft lip and 5 unaffected controls
N=34.
(p<0.05).
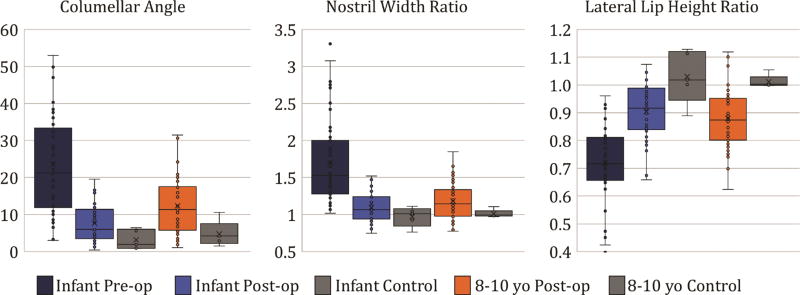
Given that variation in correlation amongst the image sets may be related to the magnitude of differences amongst subjects. The mean, range, and variation of anthropometric measurements for subjects in each image set are summarized in Figure 7.
Figure 7. Distribution of anthropometric measurements in groups.
Box-and-whisker plots for the most predictive anthropometric measurements of the 3 image sets. The bottom and top of the boxes mark the first and third quartiles, the bands inside the boxes mark the median (second quartile) and whiskers mark local minimum and maximum (1.5 × interquartile range). Each data point is shown with a filled circle and mean point is marked with an X. Data points lying outside the whiskers are outliers. Red dashed lines show the perfect symmetry. The distribution of measurements was different for each of the 3 image sets. The Infant pre-op group had the widest variation (size of the box), while the Infant post-op group had the smallest variation. The smaller variation suggests more similar appearances, and thus greater difficulty making side-by-side comparisons to rank appearances.
Infants pre-op
Columellar angle, nostril width ratio, and lateral lip height ratio were highly correlated with the rank sum score (coefficients of 0.72 to 0.80). The nostril height ratio and medial lip height ratio were moderate predictors of the rank sum score (coefficients of 0.4 to 0.41).
Infants post-op
Following primary cleft lip repair, only the nostril width ratio and the lateral lip height ratio were correlated with the rank sum score. Correlation was moderate for both measures (coefficients of 0.34 and 0.42 respectively).
Children 8–10 years old
Columellar angle and nostril width ratio had moderate or good correlation with the rank sum score (coefficients of 0.51 and 0.41 respectively).
3. Predictors of early post-operative outcome
The pre-operative rank sum score of an individual infant subject was predictive of the immediate post-operative rank sum score: R = 0.65 (p = <0.01).
Several objective pre-operative measures were also found to be predictive of the immediate post-operative rank (Table 4) including columellar angle, nostril width ratio, nostril height ratio, and lateral lip height ratio (correlations coefficients 0.36 to 0.42)
Table 4.
Correlation of pre-operative anthropometric measurements with post-operative expert consensus (ranks sum score) of nasal appearance using Pearson correlation coefficient
| Infants | |
|---|---|
| Columellar angle | −0.42* |
| Cleft/Non-Cleft Nostril Width Ratio | −0.36* |
| Cleft/Non-Cleft Nostril Height Ratio† | 0.32 |
| Cleft/Non-Cleft Nostril Height Ratio (NNCL method) | 0.31* |
| Cleft/Non-Cleft Medial Lip Height Ratio | 0.24 |
| Cleft/Non-Cleft Lateral Lip Length Ratio | 0.06 |
| Cleft/Non-Cleft Lateral Lip Height Ratio | 0.43* |
| Lip/Nasal Width Ratio | 0.13 |
Subjects included 45 infants with unilateral cleft lip and 5 unaffected controls
N=34.
(p<0.05).
Discussion
Can we agree on the esthetics of appearance? Can we use objective measurements to reflect subjective appraisals? Does the initial severity influence the post-operative result? These 3 questions are common conundrums encountered in many areas of plastic surgery. This study addresses all three in the treatment of the unilateral cleft lip nasal deformity.
1. Experts agree on qualitative assessment of appearance
In our study expert cleft surgeons could reliably rank pre-operative severity and post-operative outcome of the unilateral cleft lip nasal deformity on 3D images. The raters were from different institutions in different cities across North America and thus the consensus is not limited to a single region. Tight agreement in assessments at each of these stages in treatment has not previously been attained. Most previous attempts to assess appearance use absolute ratings, which are prone to variations in interpretation and appraisal by different individuals who have varying backgrounds and experiences. “Beauty is in the eye of the beholder” and for different individuals, there will be a different ideal and value placed on that ideal. Not surprisingly, in Sharma’s systematic review, a large number of ratings systems were identified suggesting a lack of consensus on valid and reproducible methods3. We used a different and more inductive approach. By asking individuals to place images in rank order, the relative appearance was evaluated without imposing a set of criteria or parameters on which to make judgments. Amongst raters recruited from different centers across Canada and the United States we found extremely high agreement and excellent consistency. Fisher has previously used this approach, however, that study involved 2D photos, which are prone to error from parallax, and only assessed pre-operative severity (i.e. no evaluation of post-operative outcome)19.
In this study, we examined 2 groups of subjects in 3 distinct image sets: Group A Infants pre-op, Group A Infants post-op, and Group B Children 8–10 years old. We found that the reliability of assessments on each image set excellent but that the reliability was different in each scenario. These differences followed clinical expectations. Prior to cleft lip repair, there is a wide spectrum of nasal deformity and thus a large range in terms of the magnitude of visible differences. At the same time, all of these differences are on the same continuum or dimension of initial cleft severity, making linear rank ordering of subjects relatively simple. Ranking of pre-operative severity was extremely reliable (ICC of 0.93). After repair, all subjects have a similar appearance with a narrow range in terms of magnitude of visible difference. At the same time, aberrations in appearance are far more complex because the nasal shape not only reflects the initial cleft severity, but also some degree of under-correction, over-correction, and iatrogenic change. With small visible differences but multiple dimensions along which these could occur, comparisons are more difficult and differences may be less perceptible. Raters subjectively found Infants post-op difficult to compare and the reliability, although still excellent (ICC of 0.70), was not as good as before surgery. With further growth and at 8–10 years of age, differences in nasal form continue to be complex but the range in magnitude of visible differences is greater. The Children 8–10 years old were easier to rank and the reliability of rankings (ICC of 0.82) were better than the Infants post-op. Ultimately, rater reliability was excellent for all 3 image-sets and the final consensus of the Americleft Surgeon Subgroup via rank sum score could be used as a valid and granular standard against which objective measures could be assessed.
2. Objective measures correlate with qualitative assessments of severity and outcome
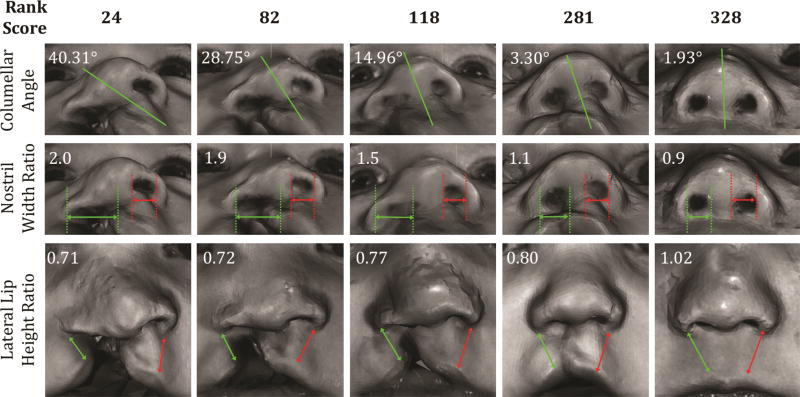
Although anthropometric analysis provides objective and quantitative measurement of form, the clinical relevance of the various dimensions may or may not be of any clinical significance. In our study, columellar angle, nostril width ratio, and lateral lip height ratio were strongly correlated with pre-operative severity (Figure 8) and moderate predictors of post-operative appearance. As with rater reliability, the smaller range in magnitude of differences and the greater complexity of post-operative nasal deformity are likely contributed to the lower correlations after cleft lip repair. Similar to our previous study20, anthropometric measures after surgery tend to normalize (Figure 5), but with further time and growth, those differences become greater. Taken together, these three measurements may be used to quantify severity and outcome and could be used to follow longitudinal changes with time.
Figure 8. Objective measurement of uCLND.
The columellar angle, nostril width ratio and lateral lip height ratio (top left corner of each image) were tightly correlated with the pre-operative rank sum score (top row).
Fisher has previously found that columellar angle and nostril width ratio correlate with expert surgeon appraisals of pre-operative cleft severity19. Meltzer21 and Vathulya22 have also reported that angulation of the columella is an important proxy of cleft severity however, these studies used conventional photography, which is prone to error from parallax, and only examined pre-operative severity. Our study validates these prior studies using 3D imaging and also supports the use of these measurements post-operatively.
In addition to columellar angle and nostril width ratio, we also found that the discrepancy in lateral lip height ratio was an important measure of pre-operative CLND severity. While such a measure of lip deficiency may not intuitively make sense when evaluating nose deformity, deficiencies of the lateral lip have been associated with hypoplasia. Measured deficiencies of lateral lip have been associated with dental agenesis23,24, dental arch deficiencies25, and maxillary hypoplasia24. The lateral lip ratio may therefore be a surrogate objective measure of cleft related hypoplasia when assessing cleft severity and the associated nasal deformity.
3. Initial severity predicts outcome
We are not aware of other studies with appraisals of pre-op severity and post-op appearance as robust as in our study. All of the infants in this study underwent cleft lip repair by the same surgeon (RT) using the same approach and as a result of measuring correlations in the absence of surgeon variability - we may have been more able to evaluate the connection between post-operative outcomes with pre-operative factors. We found that both the pre-operative rank severity and pre-operative anthropometric measures were predictive of the immediate post-operative appearance as determined by expert surgeon consensus rank. While the post-operative differences may be minor, they are detectable by surgeons who are highly trained and capable of detecting subtle abnormalities. What we can’t directly answer in our study is how relevant those abnormalities are to patients. Surgeons tend to rate postoperative deformities more severely when asked to assess appearance on photos when compared to individuals with clefts, lay people or parents26,27. Nonetheless, in one of our previous studies, lay people could detect post-operative differences in appearance that seemed to be related to initial cleft severity. In that study, de-identified photographs of children 8–10 years old were assessed by lay people via Crowdsourcing28. It makes intuitive sense that the more severe a deformity is, the more difficult it is to correct, and thus the worse the outcome. Our findings also reaffirm the importance of taking into account pre-operative severity with post-operative outcome when assessing surgical outcomes.
Future work
While much of what cleft surgeons do is based upon experience and expert opinion, in this era of evidence-based medicine, there is a role for more objective assessment of outcome. Quantification of an esthetic ideal remains elusive, however, based on this study, several objective anthropometric measurements can and should be used to report outcomes. Quantitative measures would reduce our reliance on subjective descriptors. In the short term, these measurements would be helpful in incorporating measures of severity with reports of treatment outcome. In the long term, these measurements could serve as the basis to develop quantitative measurements of treatment success. By linking pre-operative severity and post-operative success in a quantitative manner, we will be better able to understand the relative effects of treatments, techniques, and protocols over time. Although conventional photography is less costly and more readily available, 3D images provide new opportunities for analysis. The ranked image sets are the consensus of the Americleft Task Force Surgeon Subgroup and can potentially be used for other investigations. Our future work will focus on leveraging the rich surface data on 3D images to produce more sensitive objective measures of nasal deformity29–31.
Conclusions
Expert cleft surgeons can reliably rank subjects according to nasal appearance before cleft lip repair, after cleft lip repair, and at 8–10 years of age. Based upon those rankings, we found that pre-operative severity predicts post-operative appearance and thus studies that report outcomes need to pre-operative measures. We found that columellar angle, nostril width ratio, and lateral lip height are important anthropometric dimensions that can be used for longitudinal assessment of treatment of the unilateral cleft lip nasal deformity and should be included as objective measures when reporting results.
Acknowledgments
This project was funded by Seattle Children’s Hospital CCTR Translational Research Ignition Projects Program and Seattle Children’s Hospital CCTR Pediatric Pilot Fund.
Thanks to Linda Peters, CRA and Kate Nickel, CRA for subject recruitment, and Jerrie Bishop and Karina Martinez-Lopez for their administrative support.
Footnotes
Conflicts of interest: none.
Financial Disclosure: The authors have no financial interest to disclose.
Presented at: American Cleft Palate – Craniofacial Association’s (ACPA) 74th Annual Meeting (2017) in Colorado Springs, Colorado.
References
- 1.Fisher DM, Mann RJ. A model for the cleft lip nasal deformity. Plast Reconstr Surg. 1998 May;101:1448–1456. doi: 10.1097/00006534-199805000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Asher-McDade C, Roberts C, C Shaw W, Gallager C. Development of a Method for Rating Nasolabial Appearance in Patients with Clefts of the Lip and Palate. Cleft Palate-Craniofacial J. 1991;28(4):385–391. doi: 10.1597/1545-1569(1991)028<0385:DOAMFR>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Sharma VP, Bella H, Cadier MM, Pigott RW, Goodacre TEE, Richard BM. Outcomes in facial aesthetics in cleft lip and palate surgery: A systematic review. J Plast Reconstr Aesthetic Surg. 2012;65(9):1233–1245. doi: 10.1016/j.bjps.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Oh TS, Choi JW, Koh KS. Upper Lip Asymmetry Perception Using Three-Dimensional Anthropometry in Patients With Unilateral Cleft Lip Deformity. J Craniofac Surg. 2011;22(6):2080–2083. doi: 10.1097/SCS.0b013e3182319971. [DOI] [PubMed] [Google Scholar]
- 5.Tse R, Booth L, Keys K, et al. Reliability of Nasolabial Anthropometric Measures Using Three-Dimensional Stereophotogrammetry in Infants with Unrepaired Unilateral Cleft Lip. Plast Reconstr Surg. 2014;133(4):530e–542e. doi: 10.1097/PRS.0000000000000014. [DOI] [PubMed] [Google Scholar]
- 6.Ayoub A, Garrahy A, Millett D, et al. Three-Dimensional Assessment of Early Surgical Outcome in Repaired Unilateral Cleft Lip and Palate: Part 1. Nasal Changes. Cleft Palate-Craniofacial J. 2011;48(5):571–577. doi: 10.1597/09-147. [DOI] [PubMed] [Google Scholar]
- 7.Ayoub A, Garrahy A, Millett D, et al. Three-Dimensional Assessment of Early Surgical Outcome in Repaired Unilateral Cleft Lip and Palate: Part 2. Lip Changes. Cleft Palate-Craniofacial J. 2011;48(5):578–583. doi: 10.1597/09-148. [DOI] [PubMed] [Google Scholar]
- 8.Hood CA, Hosey MT, Bock M, White J, Ray A, Ayoub AF. Facial Characterization of Infants With Cleft Lip and Palate Using a Three-Dimensional Capture Technique. Cleft Palate-Craniofacial J. 2004;41(1):27–35. doi: 10.1597/02-143. [DOI] [PubMed] [Google Scholar]
- 9.Hood CA, Bock M, Hosey MT, Bowman A, Ayoub AF. Facial asymmetry - 3D assessment of infants with cleft lip & palate. Int J Paediatr Dent. 2003;13(6):404–410. doi: 10.1046/j.1365-263X.2003.00496.x. [DOI] [PubMed] [Google Scholar]
- 10.Singh GD, Levy-Bercowski D, Santiago PE. Three-Dimensional Nasal Changes Following Nasoalveolar Molding in Patients With Unilateral Cleft Lip and Palate: Geometric Morphometrics. Cleft Palate-Craniofacial J. 2005;42(4):403–409. doi: 10.1597/04-063.1. [DOI] [PubMed] [Google Scholar]
- 11.Singh G, Levy-Bercowski D, Yáñez M, Santiago P. Three-dimensional facial morphology following surgical repair of unilateral cleft lip and palate in patients after nasoalveolar molding. Orthod Craniofac Res. 2007;10(3):161–166. doi: 10.1111/j.1601-6343.2007.00390.x. [DOI] [PubMed] [Google Scholar]
- 12.van Loon B, Reddy SG, van Heerbeek N, et al. 3D stereophotogrammetric analysis of lip and nasal symmetry after primary cheiloseptoplasty in complete unilateral cleft lip repair. Rhinology. 2011;49(5):546–553. doi: 10.4193/Rhino11.092. [DOI] [PubMed] [Google Scholar]
- 13.Krimmel M, Kluba S, Breidt M, et al. Three-Dimensional Assessment of Facial Development in Children With Unilateral Cleft Lip With and Without Alveolar Cleft. J Craniofac Surg. 2013;24(1):313–316. doi: 10.1097/SCS.0b013e318275ed60. [DOI] [PubMed] [Google Scholar]
- 14.Bell A, Lo T-WR, Brown D, et al. Three-Dimensional Assessment of Facial Appearance Following Surgical Repair of Unilateral Cleft Lip and Palate. Cleft Palate-Craniofacial J. 2014;51(4):462–471. doi: 10.1597/12-140. [DOI] [PubMed] [Google Scholar]
- 15.Bugaighis I, Mattick CR, Tiddeman B, Hobson R. 3D Facial Morphometry in Children With Oral Clefts. Cleft Palate-Craniofacial J. 2014;51(4):452–461. doi: 10.1597/12-217. [DOI] [PubMed] [Google Scholar]
- 16.Bugaighis I, O’Higgins P, Tiddeman B, Mattick C, Ben Ali O, Hobson R. Three-dimensional geometric morphometrics applied to the study of children with cleft lip and/or palate from the North East of England. Eur J Orthod. 2010;32(5):514–521. doi: 10.1093/ejo/cjp140. [DOI] [PubMed] [Google Scholar]
- 17.Heike CL, Upson K, Stuhaug E, Weinberg SM. 3D digital stereophotogrammetry: a practical guide to facial image acquisition. Head Face Med. 2010;6(1):18. doi: 10.1186/1746-160X-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jia Wu, Tse R, Shapiro LG. Automated face extraction and normalization of 3D Mesh Data. 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; IEEE; 2014. pp. 750–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fisher DM, Tse R, Marcus JR. Objective measurements for grading the primary unilateral cleft lip nasal deformity. Plast Reconstr Surg. 2008;122(3):874–880. doi: 10.1097/PRS.0b013e3181811a52. [DOI] [PubMed] [Google Scholar]
- 20.Tse R, Lien S. Unilateral Cleft Lip Repair Using the Anatomical Subunit Approximation. Plast Reconstr Surg. 2015;136(1):119–130. doi: 10.1097/PRS.0000000000001369. [DOI] [PubMed] [Google Scholar]
- 21.Meltzer NE, Vaidya D, Capone RB. The Cleft-Columellar Angle: A Useful Variable to Describe the Unilateral Cleft Lip-Associated Nasal Deformity. Cleft Palate-Craniofacial J. 2013;50(1):82–87. doi: 10.1597/10-176. [DOI] [PubMed] [Google Scholar]
- 22.Vathulya M, Jain P. Columellar-Frenulum Angle – A Significant Clinical Parameter in Assessing the Degree of Severity in Unilateral Cleft Lip. Cleft Palate-Craniofacial J. 2016;53(3):290–297. doi: 10.1597/13-273. [DOI] [PubMed] [Google Scholar]
- 23.Antonarakis GS, Fisher DM. Presurgical unilateral cleft lip anthropometrics and the presence of dental anomalies. Cleft Palate-Craniofacial J. 2015;52(4):395–405. doi: 10.1597/13-145. [DOI] [PubMed] [Google Scholar]
- 24.Antonarakis GS, Tompson BD, Fisher DM. Preoperative Cleft Lip Measurements and Maxillary Growth in Patients With Unilateral Cleft Lip and Palate. Cleft Palate-Craniofacial J. 2015;00(00):150204130143000. doi: 10.1597/14-274R1. [DOI] [PubMed] [Google Scholar]
- 25.Antonarakis GS, Adibfar A, Tompson BD, Paedo D, Daskalogiannakis J, Fisher DM. Presurgical Cleft Lip Anthropometrics and Dental Arch Relationships in Patients With Complete Unilateral Cleft Lip and Palate. Cleft Palate-Craniofacial J. 2015;52(3):269–276. doi: 10.1597/13-272. [DOI] [PubMed] [Google Scholar]
- 26.Zhu S, Jayaraman J, Khambay B. Evaluation of Facial Appearance in Patients With Cleft Lip and Palate by Laypeople and Professionals: A Systematic Literature Review. Cleft Palate-Craniofacial J. 2016;53(2):187–196. doi: 10.1597/14-177. [DOI] [PubMed] [Google Scholar]
- 27.Ritter K, Trotman C-A, Phillips C. Validity of Subjective Evaluations for the Assessment of Lip Scarring and Impairment. Cleft Palate-Craniofacial J. 2002;39(6):587–596. doi: 10.1597/1545-1569(2002)039<0587:VOSEFT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Tse RW, Oh E, Gruss JS, Hopper RA, Birgfeld CB. Crowdsourcing as a Novel Method to Evaluate Aesthetic Outcomes of Treatment for Unilateral Cleft Lip. Plast Reconstr Surg. 2016;138(4):864–874. doi: 10.1097/PRS.0000000000002545. [DOI] [PubMed] [Google Scholar]
- 29.Liang S, Shapiro L, Tse R. Measuring Symmetry in Children With Cleft Lip. Part 3: Quantifying Nasal Symmetry and Nasal Normalcy Before and After Unilateral Cleft Lip Repair. Cleft Palate-Craniofacial J. 2016;00(00):16–035. doi: 10.1597/16-035. [DOI] [PubMed] [Google Scholar]
- 30.Wu J, Heike C, Birgfeld C, et al. Measuring Symmetry in Children With Unrepaired Cleft Lip: Defining a Standard for the Three-Dimensional Midfacial Reference Plane. Cleft Palate-Craniofacial J. 2016;53(6):695–704. doi: 10.1597/15-053. [DOI] [PubMed] [Google Scholar]
- 31.Wu J, Liang S, Shapiro L, Tse R. Measuring Symmetry in Children With Cleft Lip. Part 2: Quantification of Nasolabial Symmetry Before and After Cleft Lip Repair. Cleft Palate-Craniofacial J. 2016;53(6):705–713. doi: 10.1597/15-220. [DOI] [PubMed] [Google Scholar]