Key Points
Question
What are the structural and vascular abnormalities seen in the maculas of patients with incontinentia pigmenti, and how do they correlate with the peripheral pathologies?
Findings
In this prospective cross-sectional study of 5 patients with incontinentia pigmenti, multiple structural and vascular abnormalities were observed on optical coherence tomography and optical coherence tomography angiography.
Meaning
These findings suggest that in addition to peripheral vascular changes, macular abnormalities are frequently encountered in patients with incontinentia pigmenti.
Abstract
Importance
Incontinentia pigmenti (IP) is a rare, X-linked dominant disease with potentially severe ocular complications that predominantly affect the peripheral retina. However, little is known about its effects on the macula.
Objective
To describe the structural and vascular abnormalities observed in the maculas of patients with IP and to correlate these findings with peripheral pathologies.
Design, Setting, and Participants
Prospective, cross-sectional study at Wilmer Eye Institute, Johns Hopkins University. Five participants with a clinical diagnosis of IP were included and underwent multimodal imaging with ultra–wide-field fluorescein angiography (FA), spectral-domain optical coherence tomography (OCT), and OCT angiography.
Main Outcomes and Measures
The structural and vascular abnormalities observed on spectral-domain OCT and OCT angiography and their correlation with peripheral pathologies seen on ultra–wide-field FA.
Results
A total of 9 eyes from 5 patients (median age, 20.5 years; range, 8.4-54.2 years) were included. Median Snellen visual acuity was 20/32 (range, 20/16 to 20/63). ultra–wide-field FA-identified retinal vascular abnormalities in all 7 eyes in which FA was obtained. These abnormalities included microaneurysms, areas of nonperfusion, and vascular anastomoses, most of which were peripheral to the standard view of 30° FA with peripheral sweeps. Structural abnormalities were observed in 6 eyes on spectral-domain OCT, including inner retinal thinning and irregularities in the outer plexiform layer. Optical coherence tomography angiography abnormalities were noted in all 9 eyes, including decreased vascular density, abnormal vascular loops, and flow loss in the superficial and deep plexuses, which corresponded to areas of retinal thinning on spectral-domain OCT.
Conclusions and Relevance
Although our study is limited by the small sample size, the findings suggest that multimodal imaging is useful for detecting structural and vascular abnormalities that may not be apparent on ophthalmoscopy in patients with IP. Macular pathologies, especially a decrease in vascular density on OCT angiography, are common. Further studies are needed to characterize further the association between macular and peripheral abnormalities in patients with IP.
This study uses multimodal retinal imaging to describe the structural and vascular abnormalities observed in the maculas of patients with incontinentia pigmenti and to correlate these findings with peripheral pathologies.
Introduction
Incontinentia pigmenti (IP), also known as Bloch-Sulzberger syndrome, is a rare, X-linked dominant disease, attributed to mutations in the gene encoding for NF-kB essential modulator protein at locus Xq28.1,2 Patients typically present with a characteristic neonatal vesicular skin rash and subsequently develop hyperpigmented whorls on the trunk and linear hairless patches on the extremities that follow the lines of Blaschko.3,4 In addition to the skin, IP can affect the eyes, teeth, and central nervous system.
Ophthalmic manifestations are present in about 35% of patients with IP,5 and vision-threatening diseases affect approximately 20% of patients.6,7 Pathologic posterior segment findings include ischemic optic neuropathy, retinal arterial occlusion, macular ischemia, peripheral retinal nonperfusion, preretinal neovascularization, and vitreous hemorrhage.7,8 Incontinentia pigmenti is thought to affect the peripheral retina predominantly, and peripheral retinal nonperfusion has been observed in up to 25% of patients.7 Retinal detachment (tractional and/or rhegmatogenous) is seen in up to 22% of patients.9 While previous literature has shown that visually significant macular abnormalities, such as enlargement of the foveal avascular zone, perifoveal capillary dropout, presence of abnormal vessels in the foveal avascular zone, and macular ischemia, can be seen on fluorescein angiography,8 little is known about how these macular pathologies manifest with newer imaging modalities such as optical coherence tomography (OCT) and OCT angiography.
The aims of this study are to characterize the macular findings in IP using multimodal imaging, with particular attention to structural and vascular changes, and to correlate these macular findings with the peripheral retinal pathologies.
Methods
This prospective, cross-sectional study was approved by the Johns Hopkins University institutional review board (Baltimore, Maryland). Only individuals with a clinical diagnosis of IP were included, and the diagnosis of IP was based on previously published criteria.3 Our group previously published a retrospective study on a cohort of patients with IP with extended follow-up.9 Using the same database, individual patients were contacted for a clinic visit. Written informed consent was obtained from all participants and/or their legal guardians. Each patient received a comprehensive dilated fundus examination by the authors (T.Y.A.L., M.F.G., and A.W.S.) and underwent multimodal imaging with spectral-domain OCT (SD-OCT; Spectralis; Heidelberg Engineering), OCT angiography (OCTA; RTVue XR Avanti; Optovue), ultra–wide-field color fundus photography (200Tx; Optos), and ultra–wide-field fluorescein angiography (FA; 200Tx; Optos), with the exception of 1 patient who declined FA. Optical coherence tomography angiography scan protocols included 3 × 3–mm and 6 × 6–mm scans centered on the fovea. The foveal and parafoveal vascular density was computed by a preset, automated, commercial algorithm, ReVue, version 2016.2.0.36, identical to the method described by Ghassemi et al.10
Results
A total of 9 eyes from 5 patients were included because retinal examination could not be performed in 1 eye owing to phthisis bulbi. The median age was 20.5 years (range, 8.4-54.2 years). The median vision was LogMAR 0.20 (Snellen 20/32), with a range of logMAR −0.10 to LogMAR 0.50 (Snellen, 20/16 to 20/63). Patient characteristics, ocular history, and multimodal imaging findings are summarized in the Table. Additional results for each imaging modality are reported in the following paragraphs.
Table. Patient Characteristics, Ocular History, and Multimodal Imaging Findings.
| Patient, Age at Visit | Snellen Visual Acuity | Prior Ocular History | Ultra–Wide-Field FA (Peripheral Findings) | SD-OCT | OCTA (Qualitative Findings) |
|---|---|---|---|---|---|
| Patient 1, early 20s, right eye | No light perception | Retinal detachment by age 1 y; phthisis bulbi | NA | NA | NA |
| Patient 1, early 20s, left eye | 20/16 | None | Nasal anastomoses; temporal nonperfusion and anastomoses; irregular contour of distal superotemporal branch vein | Irregular OPL temporal to fovea | Abnormal vessels temporal to fovea (SCN) |
| Patient 2, mid-30s, right eye | 20/20 | None | Temporal MAs, nonperfusion and anastomoses | Irregular OPL nasal to fovea | Normal |
| Patient 2, mid-30s, left eye | 20/32 | None | Nasal anastomoses; temporal MAs, nonperfusion and anastomoses | Normal | Small area of flow loss and anastomotic loops temporal to the fovea (SCN) |
| Patient 3, child, right eye | 20/40 | None | Nasal nonperfusion and anastomoses; inferotemporal nonperfusion with an anomalous loop | Irregular OPL inferonasal to fovea | Normal |
| Patient 3, child, left eye | 20/32 | None | Temporal nonperfusion and anastomoses | Normal | Normal |
| Patient 4, preteen, right eye | 20/63 | Temporal cryotherapy and nasal laser photocoagulation (at 2 mo of age); ERM s/p PPV, MP (at age 7 y) | Not available | Inner retinal thinning in inferotemporal macula | Flow loss in inferotemporal macula (SCN and DCN) |
| Patient 4, preteen, left eye | 20/20 | Inferotemporal cryotherapy (at age 2 mo) | Not available | Normal | Normal |
| Patient , mid-50s, right eye | 20/50 | Inferotemporal scattered laser photocoagulation for atrophic holes and nonperfused retina (at age 49 and 50 y) | Nasal anastomoses; temporal nonperfusion and anastomoses | Inner retinal thinning in superotemporal macula; schisis-like changes centrally | Abnormal loops temporal to the fovea (SCN); multiple areas of flow loss in temporal macula (SCN and DCN) |
| Patient 5, mid-50s, left eye | 20/20 | Scleral buckle, cyrotherapy for macula-sparing retinal detachment (at 47 y of age) | Nasal nonperfusion, anastomoses, and abnormally straightened vessels; temporal anastomoses | OPL irregularity inferonasal to fovea | Normal |
Abbreviations: DCN, deep capillary network; ERM, epiretinal membrane; FA, fluorescein angiography; MA, microaneurysm; MP, membrane peeling; NA, not applicable; OCTA, optical coherence tomography angiography; OPL, outer plexiform layer; PPV, pars plana vitrectomy; SCN, superficial capillary network; SD-OCT, spectral-domain optical coherence tomography.
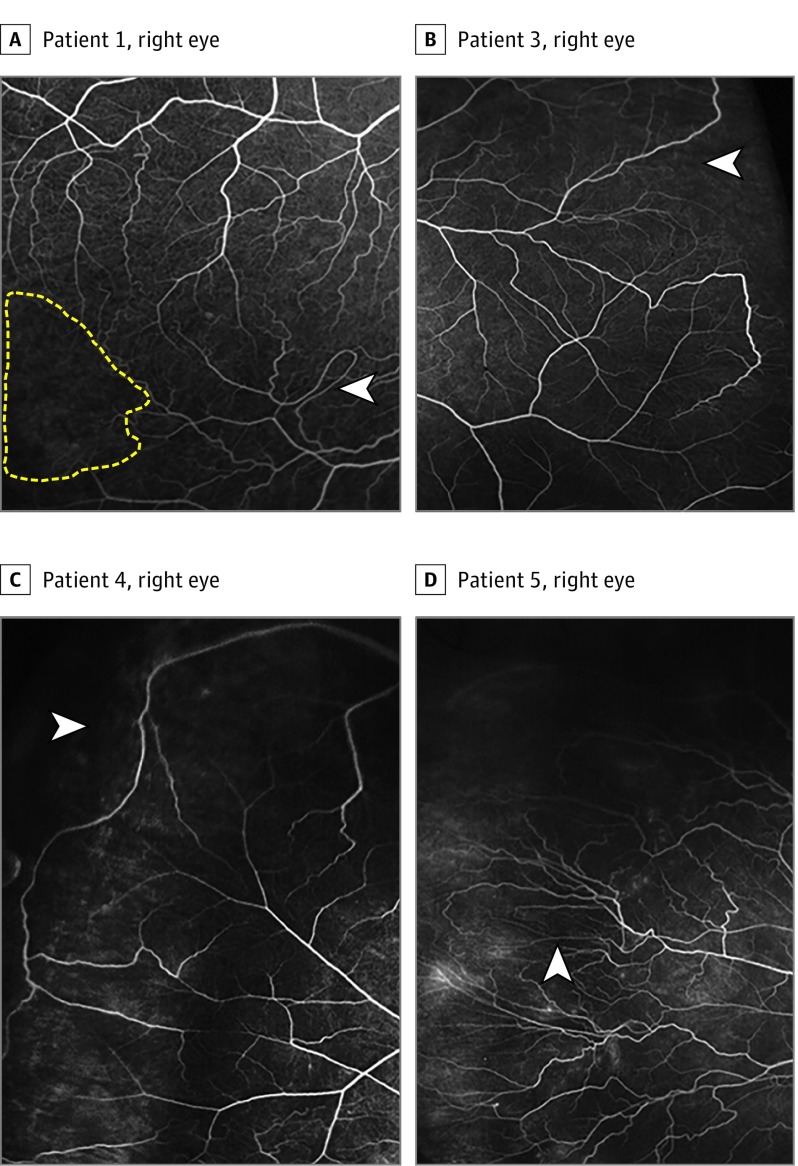
Ultra–Wide-Field FA
Four of 5 patients (7 eyes total) underwent ultra–wide-field FA because 1 patient declined FA. All 7 eyes showed pathologic changes on FA. In 3 of 7 eyes, these far peripheral changes were primarily captured by ultra–wide-field imaging; ie, no pathologic changes would likely have been seen had these 3 eyes undergone only traditional 30° FA with peripheral sweeps. Peripheral abnormal vascular anastomoses were observed in all eyes, with varying degrees of nonperfusion. Only 2 eyes showed pathologic changes within the macula on FA: 1 had parafoveal microaneurysms, and 1 had vascular anastomoses temporal to the fovea. Representative FA images are shown in Figure 1.
Figure 1. Representative Ultra–Wide-Field Fluorescein Angiographic Findings.
A, Patient 3, right eye. An anomalous vascular loop (arrowhead) and large areas of nonperfusion (yellow dotted lines) are seen in the inferotemporal quadrant. B, Patient 3, left eye. Broad, vascular anastomoses (arrowhead) and extensive nonperfusion peripheral to the anastomoses are seen temporally. C, Patient 5, right eye. Broad vascular anastomoses (arrowhead) and extensive nonperfusion are seen in the superotemporal quadrant. D, Patient 5, left eye. Multiple vascular anastomotic loops and pathologically straightened vessels (arrowhead) are seen nasally.
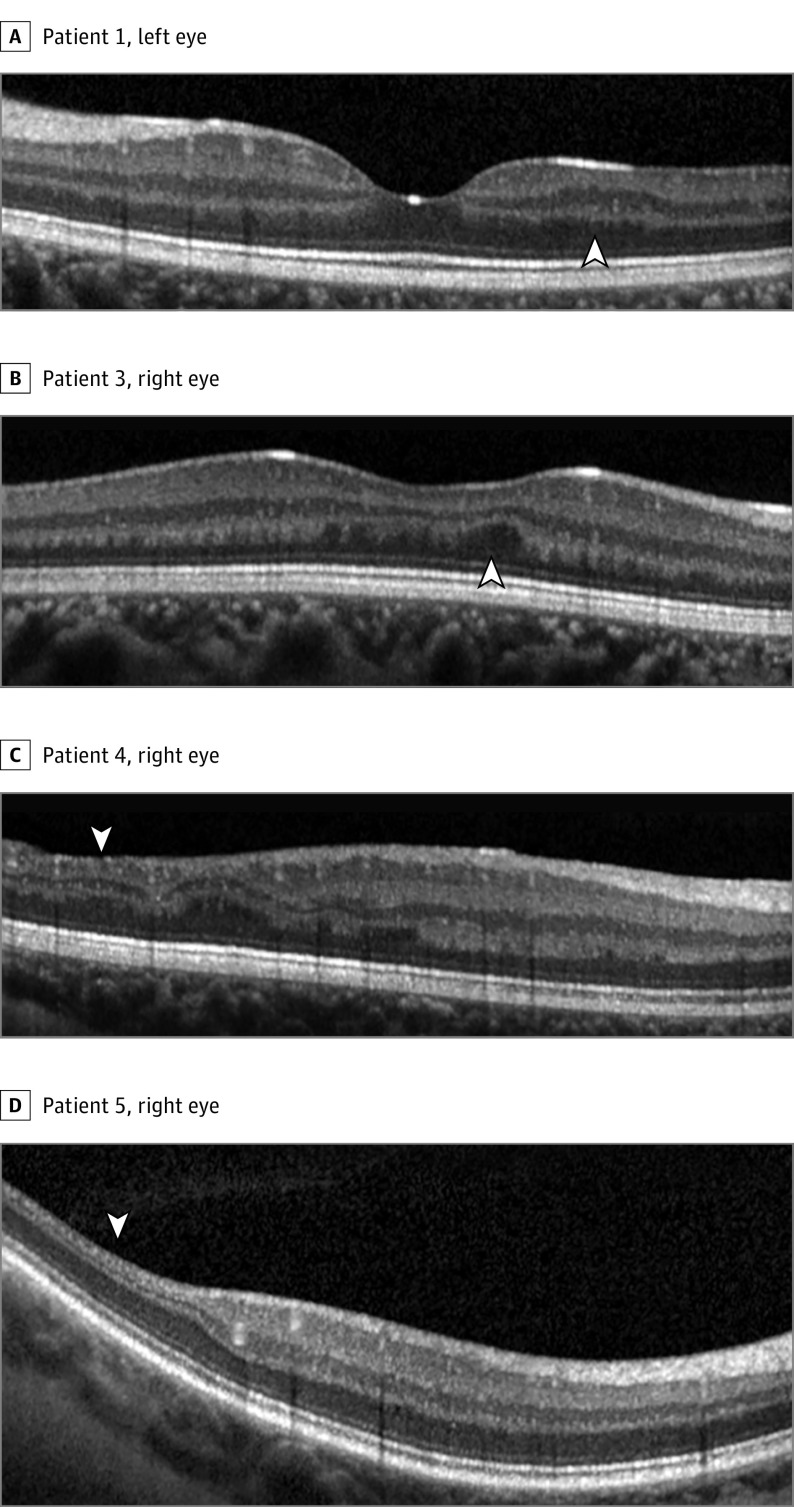
Spectral-Domain Optical Coherence Tomography
All patients (9 eyes total) underwent SD-OCT. Pathologic changes were seen in 6 of 9 eyes and included irregularities in the outer plexiform layer (Figure 2A-B) and inner retinal thinning (Figure 2C-D). In addition to inner retinal thinning, Patient 5’s right eye also showed progressive lamellar hole formation and schisis-like changes over several years, after spontaneous release of vitreomacular traction had occurred and in the absence of any vascular leakage on FA (eFigure 1 in the Supplement).
Figure 2. Representative Spectral-Domain Optical Coherence Tomography Findings.
A, Patient 1, left eye. Irregular outer plexiform layer in the temporal juxtafoveal area (arrowhead). B, Patient 3, right eye. Irregular outer plexiform layer in the inferonasal juxtafoveal area (arrowhead). C, Patient 4, right eye. Inner retinal thinning in the inferotemporal macula (arrowhead). D, Patient 5, right eye. Inner retinal thinning in the superotemporal macula (arrowhead).
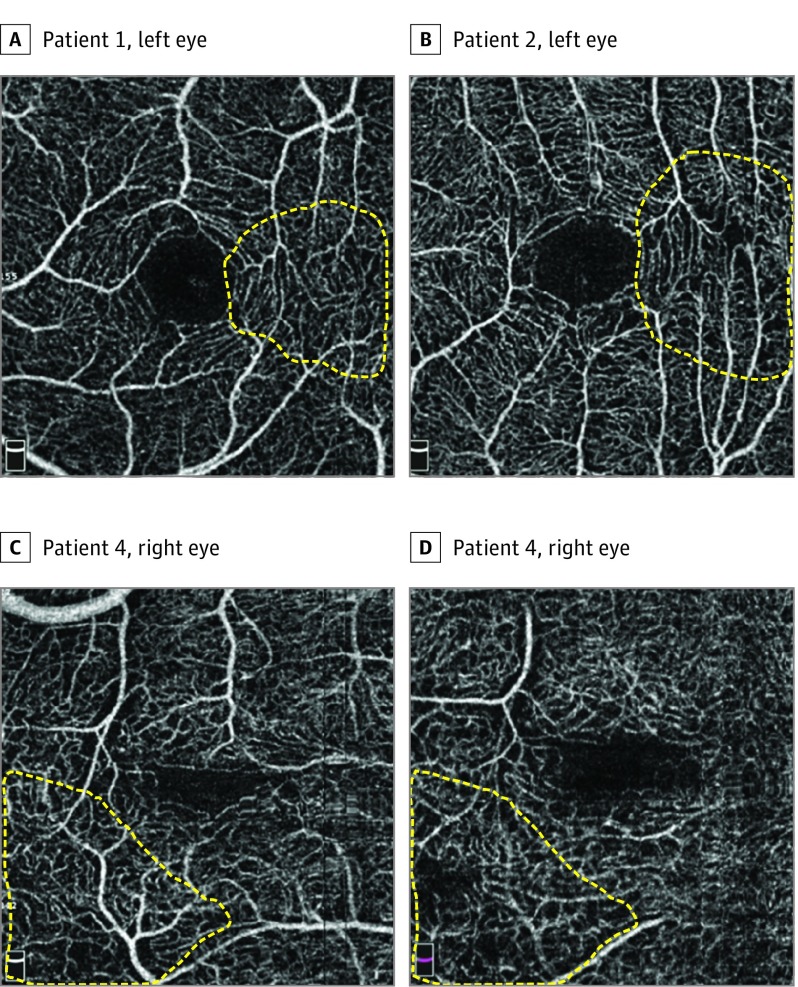
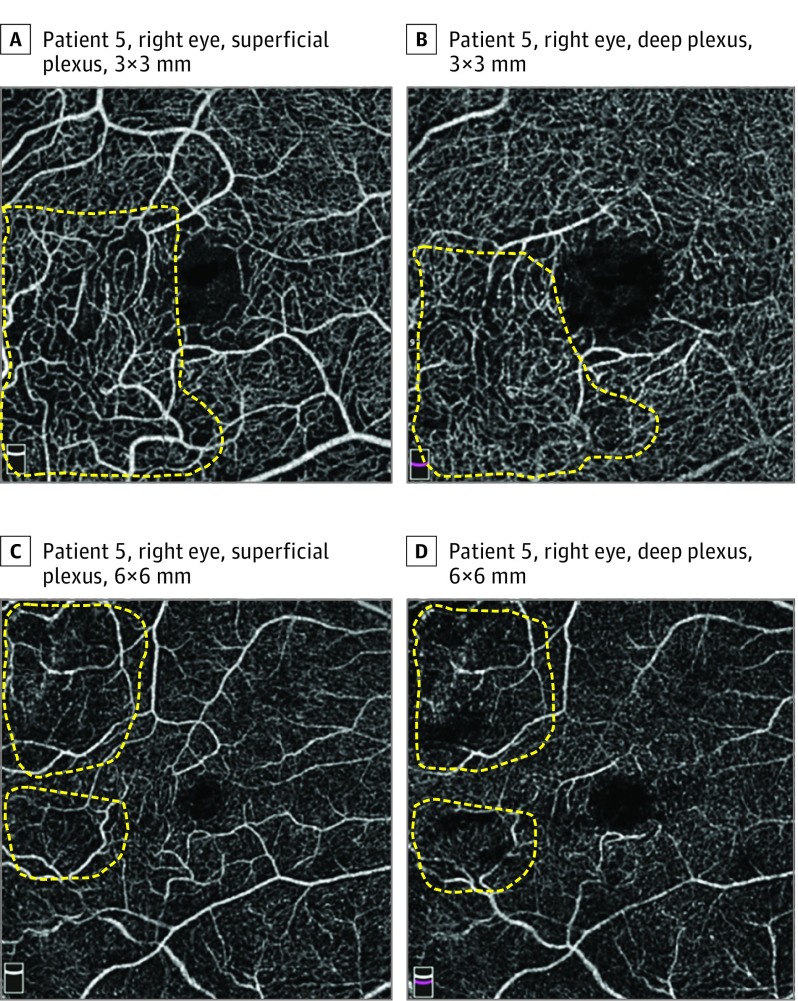
Optical Coherence Tomography Angiography
All patients (9 eyes total) underwent OCTA. Pathologic changes were seen in all 9 eyes and included decreased vascular density, abnormal vascular loops, and regions of flow loss in the superficial and deep retinal plexuses. No distinct flow loss was observed in the choriocapillaris or choroid layer in any of the eyes. Figures 3 and 4 highlight the various vascular abnormalities detected by OCTA. Patient 1’s left eye showed qualitatively abnormal vessels in the superficial plexus temporal to the fovea (Figure 3A). Patient 2’s left eye showed a small area of flow loss and anastomotic loops in the superficial plexus temporal to the fovea (Figure 3B). Patient 4’s right eye showed an area of flow loss in the superficial and deep plexuses inferotemporal to the fovea (Figure 3C and D). Patient 5’s right eye showed abnormal anastomoses in the superficial plexus inferotemporal to the fovea and flow loss in the superficial and deep plexuses in the same area (Figure 4A and B). Additional areas of flow loss were seen in the superficial and deep plexuses at the temporal aspect of the macula (Figure 4C and D). The vascular densities measured within a 3-mm–diameter circle centered on the fovea in each eye were recorded. These values were compared with age-matched normative data, and all 9 eyes showed varying degrees of pathologic decrease in vascular density (more than 2 standard deviations less than the age-matched mean)10 (eTable 1 in the Supplement).
Figure 3. Pathological Changes on Optical Coherence Tomography Angiography, Highlighted by Yellow Dotted Lines.
A, Patient 1, left eye, 3 × 3 mm, superficial plexus. Qualitatively abnormal vessels temporal to fovea. B, Patient 2, left eye, 3 × 3 mm, superficial plexus. Small area of flow loss and vascular loops temporal to fovea. C and D, Patient 4, right eye, 3 × 3 mm. Flow loss in the superficial (C) and deep (D) plexus inferotemporal to the fovea, corresponding to an area of inner retinal thinning.
Figure 4. Pathological Changes on Optical Coherence Tomography Angiography, Highlighted by Yellow Dotted Lines.
A and B, Patient 5, right eye, 3 × 3 mm. Flow loss in the superficial (A) and deep (B) plexus inferotemporal to the fovea. C and D, Patient 5, right eye, 6 × 6 mm. Multiple areas of flow loss in the superficial (C) and deep (D) plexus in the temporal macula, corresponding to an area of inner retinal thinning.
Discussion
To our knowledge, this is the first study in the literature to describe OCTA findings in IP. This study is also the first to compare pathologic findings seen on multimodal imaging, including SD-OCT, OCTA, and ultra–wide-field FA, in patients with IP. Although our sample size is limited by the rare nature of the disease, we have made the following observations.
First, ultra–wide-field FA is useful for detecting peripheral pathologies in IP. All 7 eyes that underwent ultra–wide-field FA showed pathologic changes, a portion of which were likely to have been peripheral to standard views of 30° FA with peripheral sweeps. In 3 of these eyes, the only pathologies present were likely to be peripheral to the view with standard FA. Greater detection of peripheral pathology with ultra–wide-field imaging has been demonstrated in other conditions, including diabetic retinopathy, sickle cell retinopathy, and posterior uveitis.11,12,13,14,15,16 This study highlights the fact that ultra–wide-field imaging (ultra–wide-field FA in particular) is useful in detecting and monitoring peripheral pathologies in IP that may be missed on standard field FA.
Second, SD-OCT can detect structural macular abnormalities, including areas of inner retinal thinning and irregularities of the outer plexiform layer. Limited literature exists on SD-OCT findings in patients with IP. Two eyes in our study (patient 4’s right eye and patient 5’s right eye) were found to have inner retinal thinning, a finding that has been reported previously by Basilius et al17 and Mangalesh et al.18 However, both of the eyes in our study had prior treatment for peripheral retinopathy. Patient 5’s right eye underwent laser retinopexy in the peripheral retina (during the patient’s late 40s and early 50s). The area of inner retinal thinning in the macula was associated with flow loss on OCTA in the same area, an association that will be further discussed in the following paragraph. Patient 4’s right eye underwent cryopexy and ablative photocoagulation laser as an infant or peripheral retinopathy, as well as pars plana vitrectomy with membrane peeling for epiretinal membrane as a child, so it is difficult to know whether the retinal thinning seen on SD-OCT is related to IP or related to treatment including surgery. Irregularities in the outer plexiform layer were identified in 4 eyes in our study (patient 1’s left eye, patient 2’s right eye, patient 3’s right eye, and patient 5’s left eye). Areas of outer retinal irregularity on SD-OCT have also been reported previously by Mangalesh et al.18
Patient 5’s right eye was found to have macular lamellar hole and schisis-like changes predominantly in the outer nuclear layer in the setting of prior vitreoretinal traction observed on SD-OCT. Despite spontaneous release of the vitreomacular traction, these schitic changes progressed during a span of 3 years, while her left eye remained stable without similar changes during the same time. Little is known about vitreomacular interface abnormalities in IP, and it is unclear whether the vitreomacular traction was related to prior peripheral laser, intrinsic to IP, or owing to natural history of progressive idiopathic vitreomacular interface abnormality. In addition, we did not encounter any retinal pigment epithelium or ellipsoid zone abnormalities in the patients, which is in agreement with the reports by Basilius et al17 and Mangalesh et al.18
Third, multiple abnormalities were observed on OCTA in the patients, including distinct areas of vascular flow loss and quantitative decreases in vascular density. Distinct areas of flow loss were seen in the superficial and deep plexuses, but not in the choriocapillaris or choroid. In patient 4’s right eye and patient 5’s right eye, these areas of flow loss were associated with inner retinal thinning in the same locations. This observation, together with the lack of retinal pigment epithelium abnormalities, is in agreement with Goldberg19 and Mangalesh et al,18 who suggested that neural tissue changes in the retina in IP are likely secondary to retinal vascular insults and not secondary to RPE abnormalities, as postulated by Mensheha-Manhart et al.20 Also, we observed in patient 5’s left eye that the area of outer plexiform layer irregularity corresponded to a focal zone of decreased vascular density (without a distinct area of flow loss) in the deep plexus on OCTA, again demonstrating that structural retinal changes in IP are associated with vascular insufficiency.
Fourth, although only 4 of 9 eyes showed definite qualitative changes on OCTA, all 9 eyes showed some degree of decreased vascular density when compared with age-matched normal eyes (defined as more than 2 standard deviations less than the mean).10 This suggests that macular perfusion abnormalities in IP, although sometimes subtle, may be common. Optical coherence tomography angiography detected qualitative abnormalities in the superficial plexus in 4 of 9 eyes and qualitative abnormalities in the deep plexus in 2 of 9 eyes. These findings suggest that vascular insufficiency may be more common in the superficial plexus in IP, in contrast to other peripheral retinopathies such as sickle cell retinopathy, where the deep plexus seems to be preferentially affected.21,22,23 Also, in comparing all parafoveal quadrants, an abnormal decrease in vascular density was most commonly noted temporally (7 of 9 eyes). This can perhaps be explained by the fact that the retinal vascular watershed zone is located along the temporal horizontal raphe, making this area more vulnerable to any kind of ischemic insult. A study with a larger sample size is needed to confirm these observations.
Fifth, in comparing the findings of FA, OCT, and OCTA, we observed that some patients with severe peripheral vascular pathologies had near-normal macular structure and vasculature (patient 3’s left eye and patient 5’s left eye). This highlights the potential difference in susceptibility of the macula and peripheral retina to vascular insult and suggests that the severity of central and peripheral vascular abnormalities in patients with IP may not necessarily be correlated. Further studies with a larger sample size are needed to determine the association between macular and peripheral pathologies in IP.
Limitations
The limitations of this study include its small sample size and lack of serial imaging in most eyes to demonstrate the evolution of pathologic findings over time. For example, Basilius et al17 reported disorganization of inner retinal layers and foveal avascular zone irregularities prior to the development of inner retinal thinning in IP, suggesting that vascular abnormalities precede inner retinal thinning. With longitudinal follow-up, serial OCTAs will be able to demonstrate whether flow loss on OCTA precedes inner retinal thinning or vice versa. Also, with a larger cohort, if a quantitative or chronologic correlation between decreased OCTA flow and peripheral nonperfusion can be established, then OCTA can perhaps be used as a surrogate modality to suggest the need for close follow-up and possible peripheral laser ablation treatment (if FA cannot be performed). Compared with the reported literature, our cohort was older and generally had milder phenotypes. The older age of our cohort provides insight into the chronic effects of IP on the retina. These effects are important to document and monitor because late complications, such as rhegmatogenous retinal detachments, tend to happen more frequently in adults with IP compared with children with IP.9 However, the older age of our cohort also raises the possibility that some of the abnormalities detected, eg, decrease in vascular density on OCTA, represent chronic secondary remodeling rather than direct effects of the underlying disease process. Some of our patients had already received retinal procedures, such as laser photocoagulation or cryotherapy, prior to being imaged. Hence, we cannot state with absolute certainty that all the pathologies demonstrated here are exclusively caused by IP rather than by secondary responses to prior treatment.
Conclusions
Our study is limited by its small sample size, but the findings suggest that multimodal imaging is useful for detecting structural and vascular abnormalities that may not be apparent on ophthalmoscopy in patients with IP. Although IP is classically thought to predominantly affect the peripheral retina, our study demonstrates that structural and vascular changes are frequently seen in the macula as well. Longitudinal studies are needed to establish the temporal association between macular structural changes and vascular insufficiency. Further studies with a larger sample size are also needed to characterize the association between macular and peripheral abnormalities in patients with IP.
eTable. Vascular Density (%) Measured Within a 3 mm-Diameter Circle Centered on the Fovea in Each Eye.
eFigure. Registered Spectral Domain Optical Coherence Tomography Line Scans of Patient 5’s Right Eye
References
- 1.Sefiani A, Abel L, Heuertz S, et al. The gene for incontinentia pigmenti is assigned to Xq28. Genomics. 1989;4(3):427-429. [DOI] [PubMed] [Google Scholar]
- 2.Smahi A, Courtois G, Vabres P, et al. ; The International Incontinentia Pigmenti (IP) Consortium . Genomic rearrangement in NEMO impairs NF-kappaB activation and is a cause of incontinentia pigmenti. Nature. 2000;405(6785):466-472. [DOI] [PubMed] [Google Scholar]
- 3.Landy SJ, Donnai D. Incontinentia pigmenti (Bloch-Sulzberger syndrome). J Med Genet. 1993;30(1):53-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hadj-Rabia S, Froidevaux D, Bodak N, et al. Clinical study of 40 cases of incontinentia pigmenti. Arch Dermatol. 2003;139(9):1163-1170. [DOI] [PubMed] [Google Scholar]
- 5.Carney RG. Incontinentia pigmenti: a world statistical analysis. Arch Dermatol. 1976;112(4):535-542. [PubMed] [Google Scholar]
- 6.Rosenfeld SI, Smith ME. Ocular findings in incontinentia pigmenti. Ophthalmology. 1985;92(4):543-546. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg MF, Custis PH. Retinal and other manifestations of incontinentia pigmenti (Bloch-Sulzberger syndrome). Ophthalmology. 1993;100(11):1645-1654. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg MF. Macular vasculopathy and its evolution in incontinentia pigmenti. Ophthalmic Genet. 1998;19(3):141-148. [PubMed] [Google Scholar]
- 9.Chen CJ, Han IC, Tian J, Muñoz B, Goldberg MF. Extended follow-up of treated and untreated retinopathy in incontinentia pigmenti: analysis of peripheral vascular changes and incidence of retinal detachment. JAMA Ophthalmol. 2015;133(5):542-548. [DOI] [PubMed] [Google Scholar]
- 10.Ghassemi F, Fadakar K, Bazvand F, Mirshahi R, Mohebbi M, Sabour S. The quantitative measurements of vascular density and flow areas of macula using optical coherence tomography angiography in normal volunteers. Ophthalmic Surg Lasers Imaging Retina. 2017;48(6):478-486. [DOI] [PubMed] [Google Scholar]
- 11.Campbell JP, Leder HA, Sepah YJ, et al. Wide-field retinal imaging in the management of noninfectious posterior uveitis. Am J Ophthalmol. 2012;154(5):908-911.e2. [DOI] [PubMed] [Google Scholar]
- 12.Leder HA, Campbell JP, Sepah YJ, et al. Ultra-wide-field retinal imaging in the management of non-infectious retinal vasculitis. J Ophthalmic Inflamm Infect. 2013;3(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silva PS, Cavallerano JD, Haddad NM, et al. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years. Ophthalmology. 2015;122(5):949-956. [DOI] [PubMed] [Google Scholar]
- 14.Silva PS, Cavallerano JD, Sun JK, Soliman AZ, Aiello LM, Aiello LP. Peripheral lesions identified by mydriatic ultrawide field imaging: distribution and potential impact on diabetic retinopathy severity. Ophthalmology. 2013;120(12):2587-2595. [DOI] [PubMed] [Google Scholar]
- 15.Soliman AZ, Silva PS, Aiello LP, Sun JK. Ultra-wide field retinal imaging in detection, classification, and management of diabetic retinopathy. Semin Ophthalmol. 2012;27(5-6):221-227. [DOI] [PubMed] [Google Scholar]
- 16.Wessel MM, Aaker GD, Parlitsis G, Cho M, D’Amico DJ, Kiss S. Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina. 2012;32(4):785-791. [DOI] [PubMed] [Google Scholar]
- 17.Basilius J, Young MP, Michaelis TC, Hobbs R, Jenkins G, Hartnett ME. Structural abnormalities of the inner macula in incontinentia pigmenti. JAMA Ophthalmol. 2015;133(9):1067-1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mangalesh S, Chen X, Tran-Viet D, Viehland C, Freedman SF, Toth CA. Assessment of the retinal structure in children with incontinentia pigmenti. Retina. 2017;37(8):1568-1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldberg MF. The blinding mechanisms of incontinentia pigmenti. Trans Am Ophthalmol Soc. 1994;92:167-176. [PMC free article] [PubMed] [Google Scholar]
- 20.Mensheha-Manhart O, Rodrigues MM, Shields JA, Shannon GM, Mirabelli RP. Retinal pigment epithelium in incontinentia pigmenti. Am J Ophthalmol. 1975;79(4):571-577. [DOI] [PubMed] [Google Scholar]
- 21.Han IC, Tadarati M, Pacheco KD, Scott AW. Evaluation of macular vascular abnormalities identified by optical coherence tomography angiography in sickle cell disease. Am J Ophthalmol. 2017;177:90-99. [DOI] [PubMed] [Google Scholar]
- 22.Han IC, Tadarati M, Scott AW. Macular vascular abnormalities identified by optical coherence tomographic angiography in patients with sickle cell disease. JAMA Ophthalmol. 2015;133(11):1337-1340. [DOI] [PubMed] [Google Scholar]
- 23.Minvielle W, Caillaux V, Cohen SY, et al. Macular microangiopathy in sickle cell disease using optical coherence tomography angiography. Am J Ophthalmol. 2016;164:137-44.e1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Vascular Density (%) Measured Within a 3 mm-Diameter Circle Centered on the Fovea in Each Eye.
eFigure. Registered Spectral Domain Optical Coherence Tomography Line Scans of Patient 5’s Right Eye