Key Points
Question
What is the association of visual impairment (visual acuity worse than 6/12) with mortality risk among indigenous Australian individuals in remote central Australia, who experience the worst social disadvantage and morbidity in the country?
Findings
In this cohort study of 1347 remote indigenous Australian individuals, vision impairment was associated with 40% higher 10-year mortality after adjusting for age, sex, hypertension, and diabetes compared with normal vision.
Meaning
Visual impairment is associated with an increased mortality among remote indigenous Australian individuals, which is 3 times higher than that of the general population; efforts must be made to improve the ocular health of this highly disadvantaged group.
Abstract
Importance
It is well established from different population-based studies that visual impairment is associated with increased mortality rate. However, to our knowledge, the association of visual impairment with increased mortality rate has not been reported among indigenous Australian individuals.
Objective
To assess the association between visual impairment and 10-year mortality risk among the remote indigenous Australian population.
Design, Setting, and Participants
Prospective cohort study recruiting indigenous Australian individuals from 30 remote communities located within the central Australian statistical local area over a 36-month period between July 2005 and June 2008. The data were analyzed in January 2017.
Exposures
Visual acuity, slitlamp biomicroscopy, and fundus examination were performed on all patients at recruitment. Visual impairment was defined as a visual acuity of less than 6/12 in the better eye.
Main Outcomes and Measures
Mortality rate and mortality cause were obtained at 10 years, and statistical analyses were performed. Hazard ratios for 10-year mortality with 95% confidence intervals are presented.
Results
One thousand three hundred forty-seven patients were recruited from a total target population number of 2014. The mean (SD) age was 56 (11) years, and 62% were women. The total all-cause mortality was found to be 29.3% at 10 years. This varied from 21.1% among those without visual impairment to 48.5% among those with visual impairment. After adjustment for age, sex, and the presence of diabetes and hypertension, those with visual impairment were 40% more likely to die (hazard ratio, 1.40; 95% CI, 1.16-1.70; P = .001) during the 10-year follow-up period compared with those with normal vision.
Conclusions and Relevance
Bilateral visual impairment among remote indigenous Australian individuals was associated with 40% higher 10-year mortality risk compared with those who were not visually impaired. Resource allocation toward improving visual acuity may therefore aid in closing the gap in mortality outcomes between indigenous and nonindigenous Australian individuals.
This cohort study assesses the association between visual impairment and 10-year mortality risk among the remote indigenous Australian population
Introduction
Indigenous Australian individuals have lower life expectancy compared with the Australian population as a whole,1 especially in remote central Australia, where they experience the worst social disadvantage2 and morbidity in the country. Health care professionals in these areas struggle to deliver adequate services owing to the logistics involved. As a result, increased resources are always required but not always received. It is therefore important to highlight the needs of this underrepresented population by drawing the attention of policy makers to the adverse outcomes experienced in remote regions of Australia.
The association of visual impairment (VI) with increased mortality rate has been reported in many places across the world including Australia.3,4 However, to our knowledge, this important association has not been demonstrated among indigenous Australian individuals, which, if present, may help to direct service provision and funding. We aimed to assess the association between VI and mortality among indigenous Australian individuals within remote central Australia.
Methods
The Central Australian Ocular Health Study took place in remote communities within central Australia and included a total target population of 2014 persons 40 years and older.5,6 Ophthalmic clinics were held at 30 of the largest communities between July 2005 and June 2008. Patients were recruited from those who identified themselves as indigenous Australian. Ethical approval from the Central Australian Human Research Ethics Committee was obtained, and the study conformed to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants, using an interpreter where necessary.
Visual acuity (VA) was determined using a tumbling E acuity chart at 3 m in a well-lit room. If the patient could not read the top letter (6/120 equivalent), they were recorded as either counting fingers at 2 m or 1 m, hand movements, light perception, or no light perception. Visual impairment was defined as a VA of less than 6/12 in the better eye.
Patients were then followed up in these remote clinics during the subsequent 10 years. Mortality and the cause of mortality for those 40 years or older at the time of recruitment was established by accessing records from Alice Springs Hospital, Alice Springs, Northern Territory, and the Department of Births, Deaths, and Marriages from South Australia.
Statistical Analysis, System 9.1 (SAS Institute Inc) was used for statistical analysis including descriptive statistics, t test, and Cox proportional hazards model. Age was considered as a continuous variable. Sex, VI, blindness, hypertension, and diabetes were considered as categorical variables. Test statistics, 95% confidence intervals, and P values are presented. A P value of less than .05 was considered statistically significant, and all P values were 2-sided.
Results
We recruited 1347 of 2014 individuals in the target population during the 36-month period. Ninety patients were lost to follow-up, with 1257 patients (93%) remaining. This included 476 men (37.9%) and 781 women (62.1%), and the mean (SD) age was 56 (11) years (t = 0.63; P = .53). The median time for patient follow-up in the remote clinics was 8.7 years (interquartile range, 7.8-9.5 years ), with 377 patients (30%) followed up for more than 9 years.
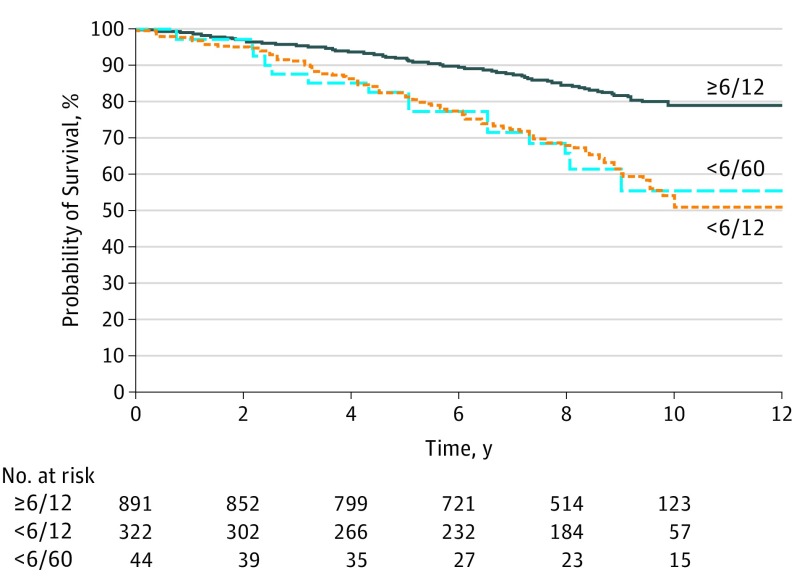
At the end of 10 years, all-cause mortality was found to be 29.3% (Figure). Of those with VA of 6/12 or better, 21.1% were deceased. However, this increased for those with reduced VA: 49.0% (95% CI, 39.6% to 58.4%) for VA of less than 6/12 to 6/60 (P < .001) and 44.7% (95% CI, 26.1% to 63.3%) for VA less than 6/60 (P < .001). There was no difference in 10-year all-cause mortality for those with VA of less than 6/12 to 6/60 and VA of less than 6/60 (difference of 4.3%; 95% CI, −23.7% to 32.3%; P = .69). Therefore, all patients who had VI were considered as a single group, which had a 10-year all-cause mortality rate of 48.5%. After multivariate adjustment for age, sex, diabetes, and hypertension, the VI group was 40% more likely to die during the 10 years of follow-up (hazard ratio [HR], 1.40; 95% CI, 1.16 to 1.70; P = .001) (Table 1). Causes of death could be established in 58% of those who died. The causes of death among the VI group were also analyzed (Table 2). Visual impairment was associated with increased renal-related mortality (HR, 1.85; 95% CI, 1.11 to 3.06; P = .02) after multivariate adjustments.
Figure. Survival Curve for All-Cause Mortality After Recruitment Into the Central Australian Ocular Health Study, Stratified for Initial Presenting Bilateral Visual Acuity (VA).
≥6/12 Indicates bilateral presenting VA of equal to or better than 6/12 at the time of recruitment; <6/12 indicates bilateral presenting VA of worse than 6/12 but better than or equal to 6/60; and <6/60 indicates bilateral presenting VA of worse than 6/60.
Table 1. Likelihood That a Patient With the Listed Risk Factors Died During Follow-up.
| Risk Factor | Hazard Ratio (95% CI) | |
|---|---|---|
| Univariate | Multivariatea | |
| Age, y | ||
| 40-49 | 1 [Reference] | 1 [Reference] |
| 50-59 | 1.49 (1.14-1.94)b | 1.41 (1.08-1.84)b |
| ≥60 | 2.57 (2.00-3.31)c | 2.24 (1.73-2.90)c |
| Bilateral presenting visual acuity | ||
| ≥6/12 | 1 [Reference] | 1 [Reference] |
| <6/12 | 1.82 (1.51-2.20)c | 1.40 (1.16-1.70)c |
| Sex | ||
| Male | 1 [Reference] | 1 [Reference] |
| Female | 0.88 (0.68-1.05) | 0.87 (0.72-1.03) |
Multivariate data were adjusted for all listed risk factors and the presence of diabetes mellitus and systemic hypertension.
P < .01.
P < .001.
Table 2. Likelihood That a Patient With Visual Impairment Died of the Listed Causes During Follow-up.
| Cause of Death | Hazard Ratio (95% CI) | |
|---|---|---|
| Univariate | Multivariatea | |
| Cardiac | 1.58 (0.90-2.78) | 1.53 (0.83-2.81) |
| Respiratory | 3.21 (0.96-10.77) | 1.95 (0.72-5.30) |
| Cerebral | 1.89 (0.87-4.13) | 1.44 (0.64-3.25) |
| Renal | 1.61 (1.04-2.50)b | 1.85 (1.11-3.06)b |
| Sepsis | 2.13 (1.17-3.88)b | 1.44 (0.78-2.65) |
| Cancer | 1.83 (1.28-2.64)c | 1.30 (0.92-1.84) |
| Other | 1.68 (1.22-2.32)c | 1.01 (0.73-1.39) |
Multivariate data were adjusted for age, sex, and the presence of diabetes mellitus and systemic hypertension.
P < .05.
P < .01.
Discussion
This study found that among indigenous Australian individuals within central Australia, VI at baseline was strongly correlated with higher mortality, which is consistent with what has been found in other populations.3,4,7 Those with VI had 40% higher mortality during the 10-year follow-up period compared with those with normal vision. Although this is similar to that found in other studies,3 the 10-year mortality rate among indigenous Australian individuals with visual impairment (48.5%) was 3 times that of the Australian population as a whole (13.7%).8,9
Declining VA may be a marker of frailty, biological aging, and predictors of mortality,10 with individuals having poorer mobility and physical function7 and at higher risk of falls, accidents, and subsequent health complications.4 Visual impairment is tied strongly to independence,11,12 which is linked to cognitive decline and also with adverse psychosocial effects such as isolation and depression, all of which have been linked to higher mortality.12,13
We showed that VI is associated with increased renal-related mortality, similar to that found among hemodialysis patients with VI.14 The prevalence of VI is higher among patients with chronic renal disease, partly owing to sharing of common systemic risk factors such as hypertension, diabetes mellitus, and smoking.15
Limitations
Our study is limited by the method through which the sample was recruited. The study recruited patients for 3 years and sampled 67% of the target population. Because patients needed to voluntarily present to an eye clinic, there is the potential that the prevalence of VI within this sample may have been overrepresented, and that this cohort may have had more health problems than the remaining 33% of the population, which might lead to an overestimation of the association between VI and mortality. However, visits to these remote communities occurred only once or twice per year; therefore, the health workers in the communities would actively encourage every resident to attend the clinics regardless of their symptoms. Ninety-five percent of patients presented because of diabetes (regardless of symptoms), because of presbyopia, or without any symptoms. We therefore feel that because most presented for a checkup because the clinic was available and not because of symptoms, the data collected should reflect an accurate estimate of mortality and its association with VI within this indigenous population. Because the study was unfunded and took place in remote indigenous Australian communities, it was necessary that it occur in the context of service provision, which limited the ability to collect data of other potential confounding covariates such as mobility, mental health status, smoking and socioeconomic status; therefore, these could not be included in the analysis. In addition, the study was only powered to detect the prevalence of conditions that lead to VI and not to detect the effect of each of these conditions on mortality. We therefore reported the effect of VI on mortality because this can not only affect mortality directly via its cause (eg, diabetes) but also have indirect effects on mortality such as by increasing the risks of falls and depression.
Conclusions
Visual impairment was associated with 40% (95% CI, 16%-70%) higher 10-year mortality risk. These data suggest it is important to have provision of comprehensive ophthalmic health care to remote indigenous Australian individuals as part of a collaborative effort to close the gap in morbidity and mortality outcomes.
References
- 1.Australian Bureau of Statistics Experimental life tables for Aboriginal and Torres Strait Islander Australians, 2005-2007. http://www.abs.gov.au/ausstats/abs@.nsf/mf/3302.0.55.003. Published 2009. Accessed January 3, 2018.
- 2.Australian Bureau of Statistics 2006 Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA): Table 2 Statistical Local Area (SLA) Index of relative Socio-economic Advantage and Disadvantage. Canberra, Australia: Australian Bureau of Statistics; 2006. [Google Scholar]
- 3.McCarty CA, Nanjan MB, Taylor HR. Vision impairment predicts 5 year mortality. Br J Ophthalmol. 2001;85(3):322-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang JJ, Mitchell P, Simpson JM, Cumming RG, Smith W. Visual impairment, age-related cataract, and mortality. Arch Ophthalmol. 2001;119(8):1186-1190. [DOI] [PubMed] [Google Scholar]
- 5.Landers J, Henderson T, Craig J. Central Australian ocular health study: design and baseline description of participants. Clin Exp Ophthalmol. 2010;38(4):375-380. [DOI] [PubMed] [Google Scholar]
- 6.Australian Bureau of Statistics 2006 Census of Population and Housing: Basic Community Profiles: Central Northern Territory (Statistical Subdivision): I03 Age by Indigenous Status by Sex. Canberra, Australia: Australian Bureau of Statistics; 2006. [Google Scholar]
- 7.Khanna RC, Murthy GV, Giridhar P, et al. Cataract, visual impairment and long-term mortality in a rural cohort in India: the Andhra Pradesh eye disease study. PLoS One. 2013;8(10):e78002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Australian Bureau of Statistics Deaths, Summary, States and Territories: 2004 to 2014. Canberra, Australia: Australian Bureau of Statistics; 2015. [Google Scholar]
- 9.Australian Bureau of Statistics Death rates, Summary, States and Territories: 2004 to 2014. Canberra, Australia: Australian Bureau of Statistics; 2015. [Google Scholar]
- 10.Klein BE, Klein R, Knudtson MD, Lee KE. Frailty, morbidity and survival. Arch Gerontol Geriatr. 2005;41(2):141-149. [DOI] [PubMed] [Google Scholar]
- 11.Zheng DD, Christ SL, Lam BL, Arheart KL, Galor A, Lee DJ. Increased mortality risk among the visually impaired: the roles of mental well-being and preventive care practices. Invest Ophthalmol Vis Sci. 2012;53(6):2685-2692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Christ SL, Zheng DD, Swenor BK, et al. Longitudinal relationships among visual acuity, daily functional status, and mortality: the Salisbury Eye Evaluation Study. JAMA Ophthalmol. 2014;132(12):1400-1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172(14):1078-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hong YA, Kim SY, Kim S-H, et al. The association of visual impairment with clinical outcomes in hemodialysis patients. Medicine (Baltimore). 2016;95(19):e3591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong CW, Lamoureux EL, Cheng C-Y, et al. Increased burden of vision impairment and eye diseases in persons with chronic kidney disease—a population-based study. EBioMedicine. 2016;5:193-197. [DOI] [PMC free article] [PubMed] [Google Scholar]