Key Points
Question
Is repair of the lateral nasal wall effective in adults with nasal airway obstruction?
Finding
In this systematic review and meta-analysis of 10 studies, which included a sample of 324 participants, the pooled effect size of functional rhinoplasty on the Nasal Obstruction Symptom Evaluation scale supported the effectiveness of functional rhinoplasty for nasal airway obstruction.
Meaning
Functional rhinoplasty may be an effective treatment for nasal airway obstruction caused by lateral nasal wall insufficiency.
This systematic review and meta-analysis examines the effectiveness of lateral wall repair in patients with nasal airway obstruction.
Abstract
Importance
While functional rhinoplasty has been broadly studied, to our knowledge no systematic review and meta-analysis of lateral wall repair has been done previously.
Objective
To evaluate the effectiveness of repair of the lateral nasal wall in adult patients with nasal airway obstruction.
Data Sources
Medline, Embase, Cinahl, Central, Scopus, and Web of Science databases and reference lists were searched for clinical and observational studies.
Study Selection
The selection criteria were defined according to the PICO (population, intervention, comparison, and outcome) framework. The relevant studies were selected by 2 independent reviewers based on the studies’ abstracts and full texts.
Data Extraction and Synthesis
Data were extracted using standardized lists chosen by the authors according to Cochrane Collaboration guidelines. The effect sizes were first calculated for each study and then pooled together using random effects synthesis. Heterogeneity was assessed using the I2 statistic, and publication bias was evaluated by the Egger test.
Main Outcomes and Measures
The results were reported as pooled row mean differences in changes from preoperative to postoperative Nasal Obstruction Symptom Evaluation scores at different times of follow-up (≤3 months, >3 to 6 months, and >6 months).
Results
Of 1522 initial records, 10 studies were considered relevant—all of them observational. The pooled study sample included 324 participants. When combining all the repeated measures together, the pooled effect size for functional rhinoplasty was −47.7 (95% CI, −53.4 to 42.1) points on the Nasal Obstruction Symptom Evaluation scale with high heterogeneity of 72%. The pooled effect size outcomes were similar in short- (−45.0 points [95% CI, −47.8 to −42.2 points]), mid- (−48.4 points [95% CI, −52.5 to −44.4 points]), and long-term (−49.0 points [95% CI, −62.1 to −35.8 points]) follow-ups.
Conclusions and Relevance
The pooled effect size of 10 observational studies supported the effectiveness of functional rhinoplasty for the treatment of nasal airway obstruction caused by lateral nasal wall insufficiency. To improve the level of evidence, randomized clinical trials are needed.
Level of Evidence
NA.
Introduction
The multifactorial etiology of nasal airway obstruction is well documented, and this condition can significantly affect patients’ quality of life.1 In 2010 the American Academy of Otolaryngology–Head and Neck Surgery released a clinical consensus statement describing nasal valve compromise as a distinct clinical entity leading to nasal airway obstruction.2 The clinical consensus statement also identified lateral nasal wall collapse or insufficiency as a distinct etiology of nasal valve compromise and described the importance of surgical correction for its treatment.2 Functional rhinoplasty is the treatment of choice for nasal valve compromise. The term functional rhinoplasty refers to a collection of various surgical techniques to correct obstruction of the internal or external nasal valves or both.3,4 The pathophysiology leading to compromise of both the internal and external nasal valves has been described extensively in the literature.2,3,5,6 The compromise of internal and external nasal valves can be either static or dynamic. The dynamic collapse of both internal and external nasal valves due to lateral nasal wall collapse is termed lateral wall insufficiency.3 This validated grading system is based on the location and percentage of closure of the lateral nasal wall toward the septum.7 The Nasal Obstruction Symptom Evaluation (NOSE) scale is a widely used, patient-reported outcome measure that effectively quantifies nasal obstruction symptoms.8,9 The NOSE scale is a reliable and valid method to assess nasal obstruction symptoms due to nasal valve compromise.8
Despite growing interest in nasal valve compromise and its surgical correction, only 2 previous systematic reviews have evaluated evidence for the effectiveness of functional rhinoplasty. Rhee et al10 have found evidence for the effectiveness of functional rhinoplasty in the treatment of nasal valve compromise. That study did not include a quantitative synthetic analysis. In turn, a systematic review by Floyd et al11 included a meta-analysis reporting significant differences between preoperative and postoperative NOSE scores in favor of functional rhinoplasty. Both previous reviews have included highly heterogeneous samples combining different study designs, rhinoplasty techniques, and causes of nasal valve compromise. Such a broad approach has left many questions unanswered. The objective of the present systematic review and meta-analysis was to evaluate the evidence for the effectiveness of functional rhinoplasty when lateral wall insufficiency was the primary cause of airway obstruction and lateral nasal wall repair the primary mode of treatment.
Methods
The criteria for considering studies for this review were based on the PICO (population, intervention, comparison, and outcome) framework as follows:
Types of studies: Clinical and observational studies with available abstracts and published as full-scale original articles or brief reports in peer-reviewed academic journals with no restriction on language or time of publication. Pilot reports, case reports, case series (<5 patients), descriptive publications on surgical techniques, theses, conference proceedings, letters, and editorials were excluded.
Participants: Adults (≥18 years) with nasal obstruction due to lateral nasal valve compromise.
Intervention: Functional rhinoplasty.
Comparison: No treatment, other treatment, placebo, sham, or comparison between preoperative and postoperative measures within the same cohort.
Outcome: Differences between groups in preoperative and postoperative change in NOSE total scores.
Data Sources and Searches
The Medline, Embase, Scopus, Cochrane Central, Web of Science, and Cinahl databases were searched in July 2017 without restriction on the time of publication. The search clause for the Medline search was the following: (“Nasal Obstruction/surgery”[Mesh] OR “Rhinoplasty/methods”[Mesh] AND “Humans”[Mesh] NOT “Cadaver”[Mesh] NOT “In Vitro Techniques”[Mesh]) AND (“alar rim” [TIAB] OR “lateral nasal wall” [TIAB] OR “nasal dorsum collapse” [TIAB] OR “septum deviation” [TIAB] OR “deviated septum” [TIAB] OR “septal deviation” [TIAB] OR “inferior turbinate” [TIAB] OR “wide columella” [TIAB] OR “ptotic nasal tip” [TIAB]) OR “functional rhinoplasty”[TIAB] OR “nasal valve collapse”[TIAB] OR “nasal valve compromise” [TIAB] OR “nasal valve dysfunction”[TIAB] NOT Review[ptyp] NOT “Advertisements” [Publication Type] NOT “Comment” [Publication Type] NOT “Editorial” [Publication Type] NOT “Letter” [Publication Type] NOT “News” [Publication Type] NOT “Retraction of Publication” [Publication Type] NOT “Academic Dissertations” [Publication Type] NOT “Abstracts” [Publication Type] NOT “Meeting Abstracts” [Publication Type] NOT protocol[TI] NOT review[TI] NOT preliminary[TI] NOT case*[TI] NOT guideline*[TI] NOT practice*[TI] NOT child*[TI] NOT adolescen*[TI] NOT pediatri*[TI] NOT polyp*[TI] NOT rhinitis[TI] NOT sinusitis[TI] NOT radiofrequency[TI] AND hasabstract[text] Study selection.”
To avoid missing potentially relevant studies, the use of other limiters and filters was restricted, relying instead on manual selection. Similar clauses were used when searching the other databases. The references of identified articles and reviews were also checked for relevant articles.
After the exclusion of duplicates, theses, conference proceedings, etc, 2 independent reviewers (C.K.K. and E.A.S.) first assessed the relevance of the remaining records based on titles and abstracts, and then assessed full-text articles for eligibility. Disagreements between reviewers were resolved in both phases by consensus or by a third reviewer. As there were no relevant randomized clinical studies, the methodological quality of the included trials was not rated.
Data Extraction
Data needed for a quantitative analysis were extracted from the included trials using a standardized form based on recommendations by the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0, part 7.6.12 The protocol of the review was registered on the Prospero database (identifier CRD42017072072).
NOSE Scale
To differentiate patients with or without nasal obstruction, a severity scale for the NOSE score suggests using a score of 30 or higher.13 According to this scale, the symptoms of patients reporting nasal obstruction are categorized as mild (5-25), moderate (30-50), severe (55-75), and extreme (80-100).
NOSE Scale Minimal Clinically Important Difference
The minimal clinically important difference (MCID) is a score change associated with the smallest clinical change detectable by a patient. Previously, the MCID for the NOSE was calculated based on (1) an anchor (change in breathing status perceived by patients who have had an operation)9,14 and (2) a statistical distribution of scores.9,15 In this study, the distribution-based MCID of NOSE scores was used, setting the cutoff at 19.4 points.9
Statistical Analysis
The effect sizes of the included trials were calculated as a row mean difference in the change of total NOSE scores between groups. As the standard deviation of difference in means was reported by only a few studies, when pooling, the pre-post correlation coefficient was set at 0.6 and the sensitivity test was run with the coefficient set at 0.8. The effect sizes were accompanied by their 95% confidence intervals. As we had expected variability in study settings, a random-effects meta-synthesis was used regardless of the particular level of heterogeneity. The synthesis (1) combined the NOSE scores reported at all time points (seeking for change from baseline) and (2) combined the NOSE scores across 3 different postoperative follow-up periods (≤3 months, >3 to 6 months, and >6 months). We also performed a sensitivity test excluding the study by Egan and Kim16 from the meta-synthesis.
The test for heterogeneity was conducted using the I2 statistic describing the percentage of variation across studies originating more from heterogeneity than from chance. The potential publication bias was evaluated by an Egger test for asymmetry of the funnel plot (test for the y-intercept = 0 from the linear regression of normalized effect estimate against precision), where the trim-and-fill method was used to impute studies into the funnel plot to correct asymmetry. All the analyses were made using Comprehensive Meta-Analysis, version 3.3 (Biostat).
Results
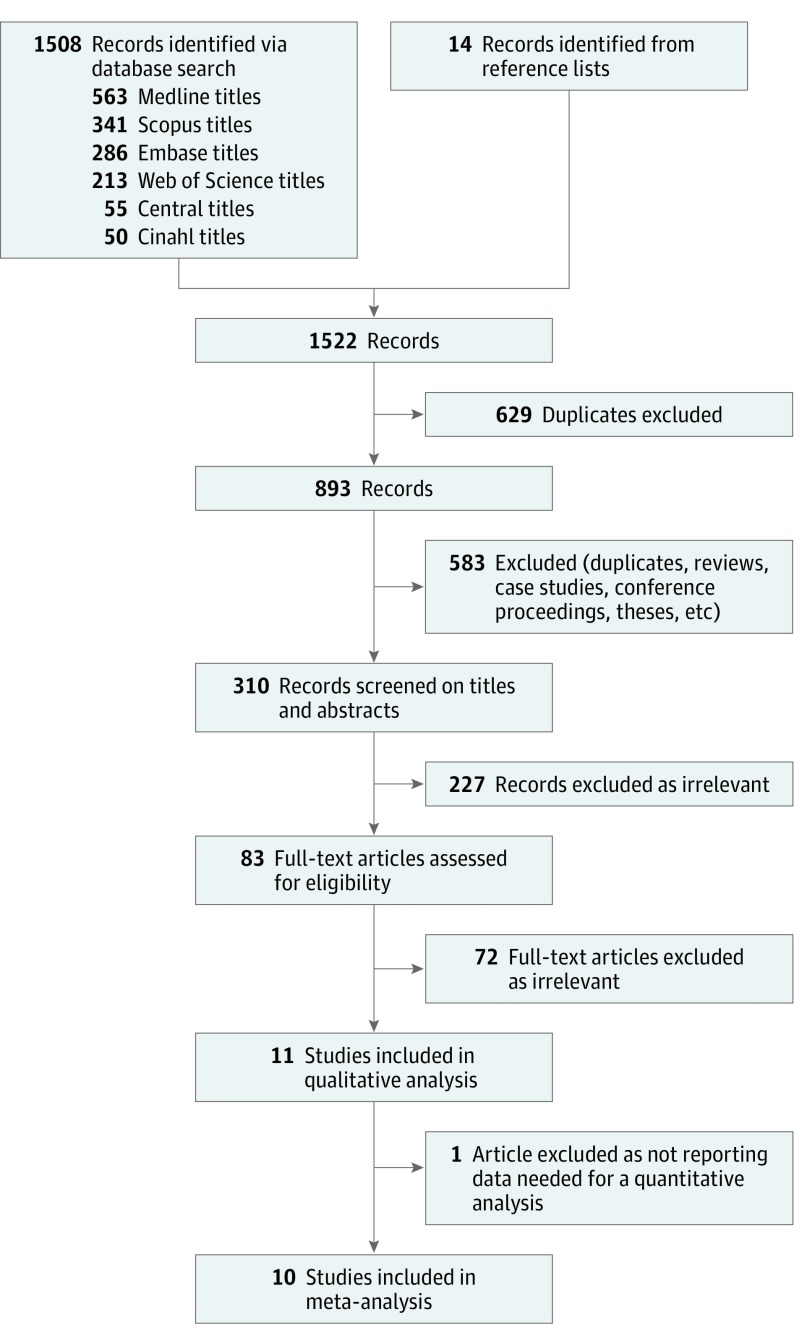
The search yielded 1522 records (Figure 1). After excluding duplicate records, reviews, case studies, conference proceedings, letters, editorials, and theses, 310 records were screened by 2 independent reviewers based on titles and abstracts. The remaining 83 records were further assessed based on their full texts. Eleven studies were considered relevant for the final analyses.4,16,17,18,19,20,21,22,23,24,25 All 11 studies had nasal valve dysfunction as the primary cause of nasal airway obstruction. Five of 11 studies included a deviated septum, turbinate hypertrophy, or both as a secondary cause of airway obstruction. After excluding the study by Sufyan et al23 with insufficient information on lateral nasal wall repair, 10 studies were included in the quantitative analysis. Although the study by Egan and Kim16 included 1 patient with composite graft repair for unilateral nasal stenosis, it also included 6 patients with nasal valve collapse due to internal nasal valve insufficiency and dynamic supra-alar lateral wall collapse who underwent functional rhinoplasty with placement of alar batten grafts. Hence, it was considered relevant and included in computing the effect size. As shown in Table 1, of the 10 included studies, 7 were conducted in the United States, 2 in Australia, and 1 in Canada. All the included studies were observational. Eight studies were prospective and 2 were retrospective. Sample sizes ranged from 6 to 79 patients. Six studies included revision surgery. Six4,16,18,21,22,24 of 10 studies reported baseline NOSE scores ranging from 55.0 to 86.5 points, indicating severe or extreme nasal obstruction. The pooled study sample included 324 participants in total.
Figure 1. PRISMA Flow Diagram.
Databases were searched for relevant studies using criteria from the PICO (population, intervention, comparison, and outcome) framework. After examining records and excluding duplicates and articles that did not meet study criteria, 83 full-text articles describing clinical and observational studies were assessed for eligibility. Of these, 10 studies were determined to be appropriate for inclusion in the meta-analysis.
Table 1. Basic Characteristics of the Included Studies.
| Source (Location) |
Design | Nasal Valve Disfunction | Intervention or Comparison | Groups | ||
|---|---|---|---|---|---|---|
| Total Patients, No. (Patients in Subgroups, No.) | Age of Total Patients, Mean, y (Age of Patients in Subgroups, Mean, y) | Women in Total Patient Population, % (Women in Study Subgroups, %) | ||||
| Barham et al,17 2015, (Australia) | Prospective observational comparative | External | Group 1: cephalic turn-in maneuver; group 2: costal cartilage grafts | 41 (25/16) | 35 (32/41) | 61 (76/38) |
| Chambers et al,18 2015, (US) | Prospective observational | External and internal | Open functional rhinoplasty with graftsa | 40 | 39 | 43 |
| Deroee et al,19 2011 (US) | Retrospective observational | External | Group 1: stab technique; group 2: marginal incision technique | 35 (15/20) | NR | NR |
| Egan and Kim,16 2005 (US) | Retrospective case series | Internal and external or nostril stenosis | Open functional rhinoplasty with either alar batten graft placement or composite graft repair | 7 | NR | NR |
| Lindsay,4 2012 (US) | Prospective observational comparative | External and internal | Group 1: internal nasal valve; group 2: external nasal valve; group 3: both nasal valves; mixed surgery techniques including open functional rhinoplasty with graft placement; spreader or autospreader grafts with flaring sutures, lateral crural strut grafts | 60 (14/16/30) | 40 | 28 |
| Palesy et al,20 2015 (Australia) | Prospective case series | External | Lateral crural cephalic turn-in or lateral crural underlay strut graft | 19 | 33 | 68 |
| Rhee et al,21 2005 (US) | Prospective observational | External and internal | Mixed surgery techniques including open functional rhinoplasty, septoplasty, spreader grafts with or without flaring sutures, turbinate reduction, and alar batten graft | 20 | 34 | 85 |
| Roofe and Most,22 2007 (US) | Prospective case series | External | Mixed surgery techniques including lateral nasal suspension suture via external rhinoplasty, turbinate reduction, and bilateral and unilateral suspension | 8 | 51 | 50 |
| Sufyan et al,23 2012 (US) | Prospective observational | External and Internal | Polyethylene batten grafts | 18 | 27-77 | 6 |
| Tan and Rotenberg,24 2012 (Canada) | Prospective observational | External and Internal | Lateral crural J-flap repair | 15 | 46 | 53 |
| Yeung et al,25 2016 (US) | Prospective observational comparative | External and Internal | Group 1: functional rhinoplasty; group 2: aesthetic-functional rhinoplasty; mixed surgery techniques including alar batten and spreader grafts of diverse materials | 79 (31/48) | 36 (39/34) | 52 (22/71) |
Abbreviation: NR, not reported.
Grafts used were spreader grafts (n = 39), columellar strut grafts (n = 23), lateral crural strut grafts (n = 20), flaring sutures (n = 6), and alar rim grafts (n = 5).
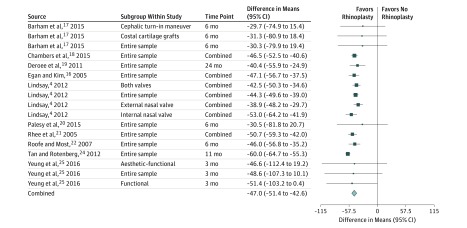
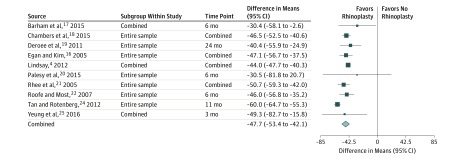
The main results reported by the included studies were converted in unified form and presented in Table 2. The same information is presented in graphical form in Figure 2. The effect sizes varied from −21 to −60 points on the NOSE scale and were statistically significant in all but 3 studies (Barham et al,17 Palesy et al,20 and Yeung et al25). When combining the data across all 10 studies and from all available time points, the pooled effect size was −47.7 (95% CI, −53.4 to −42.1) points (Figure 3), with high heterogeneity (I2 = 72%) and no need for trim-and-fill correction with an Egger coefficient of 0.67 (95% CI, −1.81 to 3.18; P = .54). The sensitivity test was conducted excluding the study by Egan and Kim.16 In that case, the pooled estimate remained essentially the same (−47.7 points [95% CI, −54.0 to −41.4 points]) when combining all the repeated measures. Combining the short-term figures (≤3 months), the pooled effect was similar (−45.0 points [95% CI, −47.8 to −42.2 points]) but with low heterogeneity (I2 = 0%) (eFigure 1 in the Supplement). For mid-term follow-up (>3 to 6 months), the pooled effect was −48.4 points (95% CI, −52.5 to −44.4 points) with low heterogeneity (I2 = 0%) (eFigure 2 in the Supplement). The pooled effect observed in a long-term follow-up (>6 months) was −49.0 points (95% CI, −62.1 to −35.8 points) with high heterogeneity (I2 = 93%) (eFigure 3 in the Supplement). The lower limit of all the calculated pooled effect sizes exceeds 19.4 points, a previously suggested NOSE score level for a minimal detectable change,9 and greater than twice the MCID for NOSE scores indicating a successful surgical outcome.15 The risk of publication bias was insignificant for all 4 analyses, with no need for a trim-and-fill correction.
Table 2. Nasal Obstruction Symptom Evaluation Scores of Studies Analyzed.
| Source | Mean (SD) | Cohort Size, No. |
|---|---|---|
| Barham et al,17 2015 | ||
| Change in score for entire samplea | −30.25 (25.33) | 41 |
| Change in score for cephalic turn-in maneuver | −29.73 (23.05) | 25 |
| Change in score for costal cartilage grafts | −31.25 (25.33) | 16 |
| Chambers et al,18 2015 | ||
| Baseline score | 75.7 (20.1) | 40 |
| Score at 2 mo | 31.4 (27.2) | 40 |
| Score at 4 mo | 34.0 (19.8) | 40 |
| Score at 6 mo | 22.1 (18.8) | 40 |
| Deroee et al,19 2011 | ||
| Change in score | −40.4 (7.9) | 12 |
| Egan and Kim,16 2005 | ||
| Baseline score | 67.1 (10.4) | 6 |
| Postoperative score | 18.6 (14.6 | 6 |
| Score at 3 mo | 21.4 (15.2) | 6 |
| Lindsay,4 2012 | ||
| Entire sample | ||
| Baseline score | 66.42 (20.25) | 60 |
| Score at 1-3 mo | 21.85 (20.68) | 54 |
| Score at 6-12 mo | 22.33 (23.05) | 45 |
| Internal nasal valve | ||
| Baseline score | 61.79 (23.34) | 14 |
| Score at 1-3 mo | 13.46 (19.19) | 13 |
| Score at 6-12 mo | 4.09 (7.35) | 11 |
| External nasal valve | ||
| Baseline score | 59.69 (20.69) | 16 |
| Score 1-3 mo | 22.69 (15.22) | 13 |
| Score 6-12 mo | 18.85 (17.34) | 13 |
| Both valves | ||
| Baseline score | 72.17 (17.30) | 30 |
| Score at 1-3 mo | 25.36 (22.93) | 28 |
| Score at 6-12 mo | 34.05 (25.03) | 21 |
| Palesy et al,20 2015 | ||
| Change in score | −30.53 (26.14) | 19 |
| Rhee et al,21 2005 | ||
| Baseline score | 68.9 (20.9) | 20 |
| Score at 3 mo | 20.7 (19.5) | 14 |
| Score at 6 mo | 15.8 (18.2) | 20 |
| Roofe and Most,22 2007 | ||
| Baseline score | 65.0 (7.6) | 8 |
| Score at 6 mo | 19.0 (18.9) | 8 |
| Change in 4 mob | −46.0 (16.53) | 42 |
| Sufyan et al 2012c | ||
| Tan and Rotenberg,24 2012d | ||
| Baseline score | 86.5 (8.0) | 15 |
| Score at 11 mo | 26.5 (11.5) | 15 |
| Yeung et al,25 2016b | ||
| Change at 3 mo for entire sample | −48.6 (29.93) | 79 |
| Change at 3 mo for functional | −51.4 (26.42) | 31 |
| Change at 3 mo for aesthetic-functional | −46.6 (33.58) | 48 |
Standard deviation adopted from reported postoperative standard deviation (costal cartilage grafts group).
Standard deviations were calculated from reported 95% confidence intervals.
No data needed for effect size calculation reported.
The Nasal Obstruction Symptom Evaluation scores are reported on a 20-point scale; thus, the scores were multiplied by 5.
Figure 2. Change in Effect Sizes (Nasal Obstruction Symptom Evaluation Score Change) Across the 10 Analyzed Studies.
The effect sizes of the included trials were calculated as a row mean difference in the change of total Nasal Obstruction Symptom Evaluation scores between groups. The effect sizes were accompanied by their 95% confidence intervals.
Figure 3. Pooled Effect Size in the Pooled Study Population of 324 Participants.
When combining the data across all 10 studies and from all available time points, the pooled effect size suggested that favorable results of the repair are also seen more than half a year later.
Discussion
In this systematic review and meta-analysis of 10 observational studies and pooled sample of 324 patients, the NOSE scores showed significant overall improvement after lateral nasal wall repair. The results were similar when pooling effect sizes for short-, mid-, and long-term follow-up figures. The calculated pooled effect sizes suggested that favorable results of the repair are also seen more than half a year later. This meta-analysis included only studies evaluating lateral nasal wall repair with outcomes based on NOSE score changes.
Limitations
The included observational studies were mostly conducted on small samples, and no randomized studies on the topic fulfilled the inclusion criteria. Although this meta-analysis favored the effectiveness of surgical lateral nasal wall repair, the main limitation of this review was the inclusion of low-quality observational studies, retrospective studies, and studies without controls. The ethical issues related to conducting randomized trials in surgery may explain the absence of randomized studies on the topic of interest.26 Because of the low number of studies in each separate follow-up analysis, results must be interpreted cautiously, as small studies are prone to random error that can affect the results of the meta-analysis. Rhee et al10 and Floyd et al11 attribute the inability to structure optimal study designs for higher levels of evidence to the multifactorial nature of nasal valve compromise and variable surgical techniques necessary for its correction.
Previous systematic reviews of functional rhinoplasty have been useful in providing higher-level evidence of the utility of functional rhinoplasty in treating patients with nasal obstruction due to valve narrowing.10,11 However, both of these terms are somewhat loosely defined to include multiple treatments and diagnoses, respectively. The current study was designed to overcome limitations faced by 2 prior systematic reviews of functional rhinoplasty by concomitantly specifying disease state, treatment type, and outcome measure. The primary etiology of nasal airway obstruction in the studies was narrowed to include only lateral wall insufficiency, either by itself or in combination with an internal nasal valve. Following with the selected etiology, the primary surgical technique was to include only lateral nasal wall repair with or without concurrent septoplasty, turbinoplasty, or both to address the specific secondary causes of nasal airway obstruction. Finally, the outcome measures to be studied were based on the NOSE scale, a validated and widely used patient-reported outcome measure.8 By designing our study based on a specific intervention for a particular etiology using a single outcome measure, we have attempted to more specifically determine the efficacy of lateral wall stabilization in the face of lateral wall insufficiency.
In the current study, based on reported baseline NOSE scores, all included studies except 1 were reported to have severe or extreme nasal obstruction. These scores are in line with the study by Floyd et al,11 in which the reported average preoperative NOSE score of 67.4 would indicate a severe nasal obstruction according to established severity classification.13 The mean improvement in NOSE scores at the 3- to 6-month postoperative period was also comparable to the observations by Floyd et al11 for this period. These results suggest that the cohort of patients included in our study could be a subset of the population included in the study by Floyd et al,11 which dealt with functional rhinoplasty as an intervention in general. Herein, however, we have provided more specific data regarding lateral wall stabilization, which one may argue treats a fundamentally different disease process than static airway obstruction.
Future research should favor controlled (preferably randomized) trials with outcomes based on validated patient-reported outcome measures such as the NOSE score.27
Conclusions
The pooled effect size of 10 observational studies supported the effectiveness of functional rhinoplasty when treating nasal airway obstruction caused by lateral nasal wall insufficiency. To improve the level of evidence, randomized controlled trials on the subject are needed.
eFigure 1. Analysis of short-term follow-up (up to 3 months) on 206 participants
eFigure 2. The pooled effect at 3 to 6 months postoperatively on 128 participants
eFigure 3. The pooled effect over 6 months postoperatively of 110 participants
References
- 1.Fuller JC, Levesque PA, Lindsay RW. Assessment of the EuroQol 5-dimension questionnaire for detection of clinically significant global health-related quality-of-life improvement following functional septorhinoplasty. JAMA Facial Plast Surg. 2017;19(2):95-100. [DOI] [PubMed] [Google Scholar]
- 2.Rhee JS, Weaver EM, Park SS, et al. Clinical consensus statement: diagnosis and management of nasal valve compromise. Otolaryngol Head Neck Surg. 2010;143(1):48-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Most SP. Trends in functional rhinoplasty. Arch Facial Plast Surg. 2008;10(6):410-413. [DOI] [PubMed] [Google Scholar]
- 4.Lindsay RW. Disease-specific quality of life outcomes in functional rhinoplasty. Laryngoscope. 2012;122(7):1480-1488. [DOI] [PubMed] [Google Scholar]
- 5.Lee J, Constantinides M. Trends in functional rhinoplasty 2008. Curr Opin Otolaryngol Head Neck Surg. 2009;17(4):295-301. [DOI] [PubMed] [Google Scholar]
- 6.Cannon DE, Rhee JS. Evidence-based practice: functional rhinoplasty. Otolaryngol Clin North Am. 2012;45(5):1033-1043. [DOI] [PubMed] [Google Scholar]
- 7.Tsao GJ, Fijalkowski N, Most SP. Validation of a grading system for lateral nasal wall insufficiency. Allergy Rhinol (Providence). 2013;4(2):e66-e68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg. 2004;130(2):157-163. [DOI] [PubMed] [Google Scholar]
- 9.Stewart MG, Smith TL, Weaver EM, et al. Outcomes after nasal septoplasty: results from the Nasal Obstruction Septoplasty Effectiveness (NOSE) study. Otolaryngol Head Neck Surg. 2004;130(3):283-290. [DOI] [PubMed] [Google Scholar]
- 10.Rhee JS, Arganbright JM, McMullin BT, Hannley M. Evidence supporting functional rhinoplasty or nasal valve repair: a 25-year systematic review. Otolaryngol Head Neck Surg. 2008;139(1):10-20. [DOI] [PubMed] [Google Scholar]
- 11.Floyd EM, Ho S, Patel P, Rosenfeld RM, Gordin E. Systematic review and meta-analysis of studies evaluating functional rhinoplasty outcomes with the NOSE score. Otolaryngol Head Neck Surg. 2017;156(5):809-815. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 London, UK: Cochrane Collaboration; 2011. http://handbook.cochrane.org.
- 13.Lipan MJ, Most SP. Development of a severity classification system for subjective nasal obstruction. JAMA Facial Plast Surg. 2013;15(5):358-361. [DOI] [PubMed] [Google Scholar]
- 14.Mondina M, Marro M, Maurice S, Stoll D, de Gabory L. Assessment of nasal septoplasty using NOSE and RhinoQoL questionnaires. Eur Arch Otorhinolaryngol. 2012;269(10):2189-2195. [DOI] [PubMed] [Google Scholar]
- 15.Lodder WL, Leong SC. What are the clinically important outcome measures in the surgical management of nasal obstruction? Clin Otolaryngol. 2017;00:1-5. [DOI] [PubMed] [Google Scholar]
- 16.Egan KK, Kim DW. A novel intranasal stent for functional rhinoplasty and nostril stenosis. Laryngoscope. 2005;115(5):903-909. [DOI] [PubMed] [Google Scholar]
- 17.Barham HP, Knisely A, Christensen J, Sacks R, Marcells GN, Harvey RJ. Costal cartilage lateral crural strut graft vs cephalic crural turn-in for correction of external valve dysfunction. JAMA Facial Plast Surg. 2015;17(5):340-345. [DOI] [PubMed] [Google Scholar]
- 18.Chambers KJ, Horstkotte KA, Shanley K, Lindsay RW. Evaluation of improvement in nasal obstruction following nasal valve correction in patients with a history of failed septoplasty. JAMA Facial Plast Surg. 2015;17(5):347-350. [DOI] [PubMed] [Google Scholar]
- 19.Deroee AF, Younes AA, Friedman O. External nasal valve collapse repair: the limited alar-facial stab approach. Laryngoscope. 2011;121(3):474-479. [DOI] [PubMed] [Google Scholar]
- 20.Palesy T, Pratt E, Mrad N, Marcells GN, Harvey RJ. Airflow and patient-perceived improvement following rhinoplastic correction of external nasal valve dysfunction. JAMA Facial Plast Surg. 2015;17(2):131-136. [DOI] [PubMed] [Google Scholar]
- 21.Rhee JS, Poetker DM, Smith TL, Bustillo A, Burzynski M, Davis RE. Nasal valve surgery improves disease-specific quality of life. Laryngoscope. 2005;115(3):437-440. [DOI] [PubMed] [Google Scholar]
- 22.Roofe SB, Most SP. Placement of a lateral nasal suspension suture via an external rhinoplasty approach. Arch Facial Plast Surg. 2007;9(3):214-216. [DOI] [PubMed] [Google Scholar]
- 23.Sufyan A, Ziebarth M, Crousore N, Berguson T, Kokoska MS. Nasal batten grafts: are patients satisfied? Arch Facial Plast Surg. 2012;14(1):14-19. [DOI] [PubMed] [Google Scholar]
- 24.Tan S, Rotenberg B. Functional outcomes after lateral crural J-flap repair of external nasal valve collapse. Ann Otol Rhinol Laryngol. 2012;121(1):16-20. [DOI] [PubMed] [Google Scholar]
- 25.Yeung A, Hassouneh B, Kim DW. Outcome of nasal valve obstruction after functional and aesthetic-functional rhinoplasty. JAMA Facial Plast Surg. 2016;18(2):128-134. [DOI] [PubMed] [Google Scholar]
- 26.McDonald PJ, Kulkarni AV, Farrokhyar F, Bhandari M. Ethical issues in surgical research. Can J Surg. 2010;53(2):133-136. [PMC free article] [PubMed] [Google Scholar]
- 27.Vaezeafshar R, Moubayed SP, Most SP. Repair of lateral wall insufficiency. JAMA Facial Plast Surg. 2018;20(2):111-115. doi: 10.1001/jamafacial.2017.0718 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Analysis of short-term follow-up (up to 3 months) on 206 participants
eFigure 2. The pooled effect at 3 to 6 months postoperatively on 128 participants
eFigure 3. The pooled effect over 6 months postoperatively of 110 participants