Abstract
Background
Mediastinal infections are a potentially devastating complication of cardiac surgery. This study analyzed the frequency, risk factors, and perioperative outcomes of mediastinal infections after cardiac surgery.
Methods
In 2010, 5,158 patients enrolled in a prospective study evaluating infections after cardiac surgery, and their effect on readmissions and mortality for up to 65 days after surgery. Clinical and demographic characteristics, operative variables, management practices, and outcomes were compared for patients with and without mediastinal infections (deep sternal wound infection, myocarditis, pericarditis, or mediastinitis).
Results
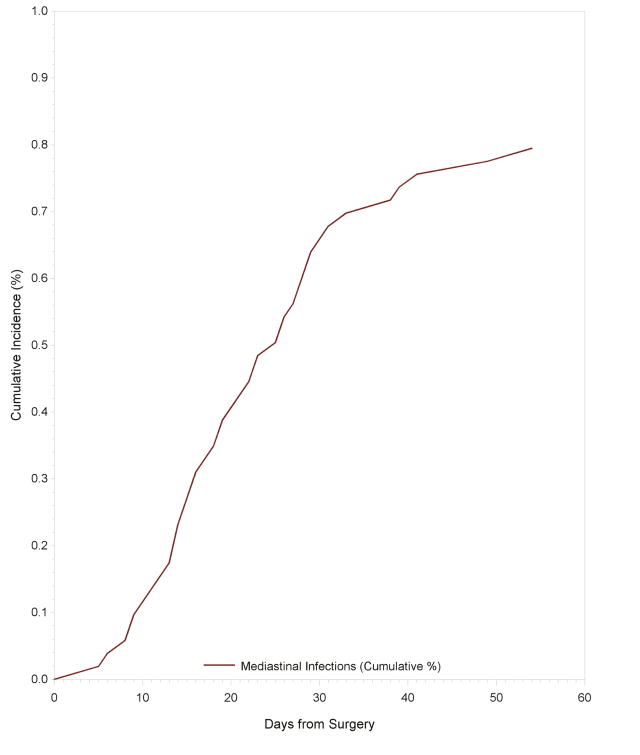
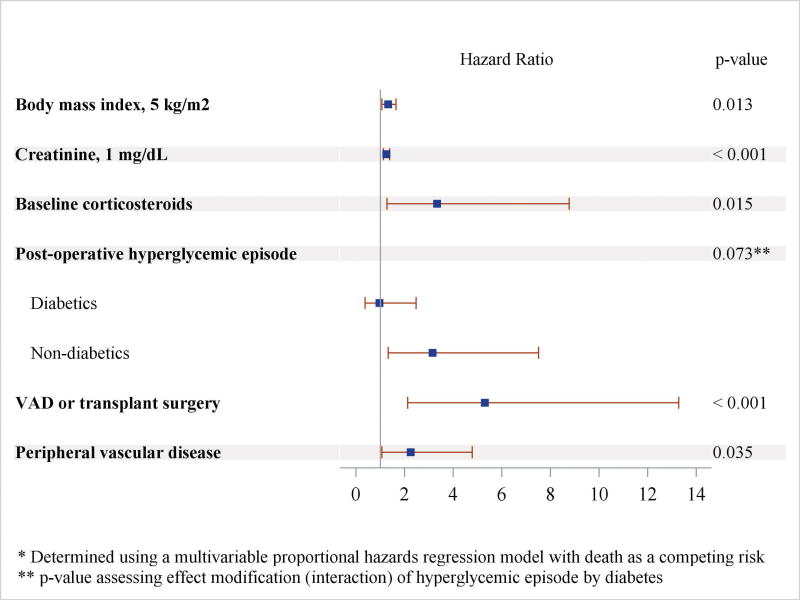
There were 43 mediastinal infections in 41 patients (cumulative incidence 0.79%; CI 0.60%-1.06%). Median time to infection was 20.0 days with 65% of infections occurring after index hospitalization discharge. Higher body mass index (HR 1.06; CI 1.01-1.10), higher creatinine (HR 1.25; CI 1.13-1.38), peripheral vascular disease (HR 2.47, CI 1.21-5.05), preoperative corticosteroid use (HR 3.33; CI 1.27-8.76), and ventricular assist device or transplant surgery (HR 5.81; CI 2.36-14.33) were associated with increased risk of mediastinal infection. Postoperative hyperglycemia (HR 3.15; CI 1.32-7.51) was associated with increased risk of infection in non-diabetic patients. Additional length of stay attributable to mediastinal infection was 11.5 days (bootstrap 95% CI; 1.88–21.11). Readmission rates and mortality were five times higher in patients with mediastinal infection than in patients without mediastinal infection.
Conclusions
Mediastinal infection after cardiac surgery is associated with substantial increases in length of stay, readmissions, and mortality. Reducing these infections remains a high priority and improving post-operative glycemic management may reduce their risk in patients without diabetes.
Classifications: Adult, Cardiac, Mediastinal infection, Outcomes, Quality care, management, Statistics, risk analysis/modeling, Surgery, complications
Major infection after cardiac surgery remains a complication of significant concern to physicians and patients alike. Despite advances in care and multiple initiatives to decrease postoperative infections, nearly 5% of patients continue to experience major infection after cardiac surgery.[1] These infections have been shown to increase morbidity, mortality, and costs.[1,2]
Efforts to eliminate the occurrence of mediastinal infection have been largely unsuccessful. The reported incidence of this serious complication after cardiac surgery is 0.2–8.0%, with most estimates between 1–2%, and has remained stable over time. [3-9] Although a number of risk factors for mediastinal infection after cardiac surgery have been described, most studies are single center, retrospective, did not adjudicate infections, and lack follow-up past discharge or 30 days postoperatively.[9] In this study, using prospective data collected by the Cardiothoracic Surgical Trials Network (CTSN), we aim to characterize mediastinal infections in cardiac surgery patients and to analyze patient risk factors and processes of care associated with these infections.
Patients and Methods
Patient Population
The study cohort included all patients at CTSN sites (Appendix I and CONSORT Diagram) who participated in the prospective observational study “Management Practices and the Risk of Infection Following Cardiac Surgery” (NCT01089712).[1] Participating sites enrolled patients consecutively between February and October 2010 who had a clinical indication for cardiac surgery, did not have an active systemic infection, were at least 18 years of age, and provided written informed consent. The study was approved by Institutional Review Boards at each participating clinical center and at the data coordinating center.
Study Design
The primary outcome of interest in this analysis was the incidence of mediastinal infection, defined as deep sternal wound infection (DSWI), mediastinitis, pericarditis, or infectious myocarditis (Appendix II). Participants were followed for up to 65 days to determine incidence of major and minor infections, all-cause mortality, and hospital readmission. Infections were classified based on definitions from the Centers for Disease Control and Prevention and the National Healthcare Safety Network surveillance. All major infections including mediastinal infections and a subset of minor infections were adjudicated by an Event Adjudication Committee that included three infectious disease experts.[10]
Data were collected on comorbidities, procedure-related variables, and management practices. Postoperative hyperglycemia was defined as one or more blood sugar measurements above 180 mg/dL during the first 48 hours post-operatively.
Statistical Analysis
Univariate Cox proportional hazards regression models were used to assess differences in patient demographics, operative characteristics, and post-operative management by whether or not a patient had a mediastinal infection during the 65 day follow up period. Factors with a p-value ≤ 0.15 in univariate analyses were considered for inclusion in a multivariate model. A multivariate Cox proportional hazards regression model treating death as a competing risk was used to determine the cumulative incidence of mediastinal infection and the association of patient characteristics and management practices with mediastinal infection.[11] The interaction between diabetes and hyperglycemia was tested at the p=0.10 threshold; all other variables included in the final model were tested at the p=0.05 level.
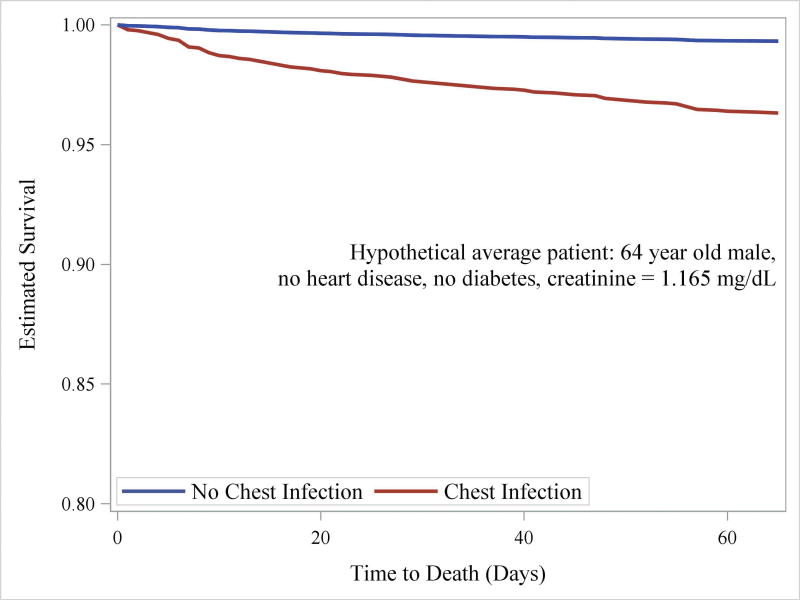
Mortality by time-varying mediastinal infection was assessed by a Cox proportional hazards regression model adjusted for variables shown to be associated with mortality in the cohort as a whole.[1] Survival estimates for the average patient in the cohort (age 64 years, creatinine 1.165 mg/dL, no diabetes or heart failure) were generated from the proportional hazards regression model and plotted by time-varying mediastinal infection status.
A time-inhomogeneous multi-state Markov model was used to determine the excess length of stay (LOS) of the index hospitalization due to mediastinal infection.[12] The model allowed transitions to multiple states from a single initial state (uninfected at time of index surgical procedure). State transitions could occur to death (competing risk), discharge (event of primary interest), or infection and then to death or discharge (Supplemental Figure 1). Transition hazards were calculated and used to estimate the excess LOS due to infection. A bootstrap standard error and 95% confidence interval (CI) for the excess LOS was computed based on 1,000 bootstrap samples. All analyses were conducted using SAS version 9.4 (SAS Institute, Inc., Cary, NC) and R 3.1.1.
Results
Mediastinal Infection and Patient Characteristics
The cohort included 5,158 patients who enrolled in the study. There were 43 mediastinal infections in 41 patients, a cumulative incidence of 0.79% (95% CI, 0.60%-1.06%; see Figure 1). Of the 43 mediastinal infections, 26 were DSWIs (61%), 12 mediastinitis (28%) and 5 myocarditis or pericarditis (12%). In the patients with two mediastinal infections, one had a DSWI followed by a later occurrence of mediastinitis, and one had two separate myocarditis or pericarditis events.
Figure 1. Cumulative incidence of mediastinal infection with death as a competing risk.
Compared to non-infected patients, patients with mediastinal infections typically had higher BMI, higher creatinine, lower hemoglobin, and lower ejection fractions (Table 1). They were more likely to be on preoperative circulatory support (extracorporeal membrane oxygenation [ECMO], intra-aortic balloon pump [IABP], and/or ventricular assist device [VAD]); to have diabetes, renal failure, or peripheral vascular disease; and to be on corticosteroids pre-operatively. In both groups, the most common procedures were isolated valve, isolated CABG, and combined CABG and valve procedures. Sternotomy approach was used in 90.5% of patients, and 91.1% of procedures were done on cardiopulmonary bypass. Increased operative and bypass time, packed red blood cell (PRBC) transfusions, and ventilation time were more common in patients with mediastinal infections (Table 2). These patients were also more likely to have prolonged antibiotic exposure and postoperative hyperglycemia.
Table 1. Baseline characteristicsa.
| Mediastinal Infection (N = 41) | No Mediastinal Infection (N = 5117) | Hazard Ratio | P-valueb | |
|---|---|---|---|---|
| Demographics | ||||
| Age, mean (SD) | 64.4 (14.5) | 64.4 (13.2) | 1.00 | 0.991 |
| Male | 25 (61.0) | 3425 (66.9) | 0.77 | 0.405 |
| Race | 0.849 | |||
| White | 33 (80.5) | 4289 (83.8) | 0.83 | |
| Black | 5 (12.2) | 535 (10.5) | ||
| Other | 3 (7.3) | 293 (5.7) | 1.11 | |
| Body Mass Index | 32.1 (25.4, 37.2) | 28.2 (25.1, 32.2) | 1.07 | <.001 |
| Baseline Laboratories | ||||
| WBC, ×103/ml | 6.8 (5.5, 8.5) | 7.0 (5.7, 8.4) | 1.02 | 0.695 |
| Creatinine, mg/dL | 1.2 (1.0, 1.4) | 1.0 (0.8, 1.2) | 1.24 | <.001 |
| Hemoglobin, g/dL | 12.3 (10.6, 13.7) | 13.4 (12.0, 14.5) | 0.78 | 0.001 |
| Cardiac morbidity | ||||
| Heart failure | 17 (41.5) | 1488 (29.1) | 1.75 | 0.079 |
| Ejection fraction | 55.0 (37.0, 60.0) | 55.0 (48.0, 60.0) | 0.98 | 0.030 |
| Previous cardiac surgery | 11 (26.8) | 947 (18.5) | 1.62 | 0.173 |
| Baseline circulatory support | 4 (9.8) | 131 (2.6) | 4.08 | 0.008 |
| History of infective endocarditis | 1 (2.4) | 60 (1.2) | 2.08 | 0.471 |
| Noncardiac morbidity | ||||
| Smoker | 23 (56.1) | 2434 (47.6) | 1.41 | 0.278 |
| Diabetesc | 18 (43.9) | 1151 (22.5) | 2.69 | 0.002 |
| COPD | 0.457 | |||
| None | 33 (80.5) | 4379 (85.6) | ||
| Mild or moderate | 6 (14.6) | 638 (12.5) | 1.25 | |
| Severe | 2 (4.9) | 100 (2.0) | 2.68 | |
| Renal Failure | 0.010 | |||
| No | 31 (75.6) | 4531 (88.5) | ||
| Yes, Dialysis Dependent | 4 (9.8) | 86 (1.7) | 6.84 | |
| Yes, Not Dialysis Dependent | 6 (14.6) | 500 (9.8) | 1.79 | |
| History of cerebrovascular accident | 6 (14.6) | 514 (10.0) | 1.53 | 0.333 |
| Peripheral vascular disease | 11 (26.8) | 524 (10.2) | 3.23 | <.001 |
| Other | ||||
| Transferred from outside hospital | 7 (17.1) | 714 (14.0) | 1.27 | 0.559 |
| Preoperative corticosteroids | 5 (12.2) | 171 (3.3) | 4.04 | 0.004 |
| Days admitted prior to surgery | 0.0 (0.0, 2.0) | 0.0 (0.0, 2.0) | 1.02 | 0.505 |
Continuous variables are expressed as mean (SD) or median (IQR) and categorical variables as count (%).
Based on Cox proportional hazards model where outcome is time to chest infection and predictor is patient or operative characteristic.
Insulin or oral medications.
Table 2. Operative and postoperative characteristicsa.
| Mediastinal Infection (N = 41) | No Mediastinal Infection (N = 5117) | Hazard Ratio | P-valueb | |
|---|---|---|---|---|
| Procedure | 0.007 | |||
| Isolated CABG | 16 (39.0) | 1661 (32.5) | 0.82 | |
| Isolated valve | 7 (17.1) | 1871 (36.6) | 0.32 | |
| CABG + valve | 8 (19.5) | 684 (13.4) | ||
| Transplant or VAD | 5 (12.2) | 117 (2.3) | 3.65 | |
| Thoracic aortic | 2 (4.9) | 426 (8.3) | 0.40 | |
| Other | 3 (7.3) | 358 (7.0) | 0.72 | |
| S. aureus nasal decontamination | 15 (36.6) | 2412 (47.2) | 0.65 | 0.181 |
| Surgery type | 0.614 | |||
| Elective | 28 (68.3) | 3778 (73.8) | ||
| Urgent | 11 (26.8) | 1203 (23.5) | 1.23 | |
| Emergent | 2 (4.9) | 136 (2.7) | 2.00 | |
| Surgery time, hours | 4.9 (3.8, 6.1) | 4.2 (3.3, 5.2) | 1.25 | 0.008 |
| Bypass time, hoursc | 2.0 (1.4, 2.8) | 1.8 (1.3, 2.3) | 1.37 | 0.036 |
| Sternotomy | 40 (97.6) | 4629 (90.5) | 4.18 | 0.158 |
| Use of IMA in CABG patientsd | 0.56 | |||
| No IMA | 6 (25.0) | 438 (18.7) | 0.96 | |
| Single IMA | 15 (62.5) | 1698 (72.4) | 0.62 | |
| Bilateral IMA | 3 (12.5) | 209 (8.9) | ||
| Number of vein grafts | 1.5 (1.0, 2.0) | 2.0 (1.0, 2.0) | 0.99 | 0.973 |
| Total PRBCs | 2.0 (0.0, 4.0) | 0.0 (0.0, 3.0) | 1.05 | 0.001 |
| Surgical site scrub with chlorhexadine preparations | 30 (78.9) | 4118 (81.7) | 0.85 | 0.672 |
| Ioban | 24 (58.5) | 2867 (56.0) | 1.11 | 0.751 |
| Post-operative hyperglycemia | 27 (65.9) | 2201 (43.1) | 2.55 | 0.004 |
| Days of post-operative antibiotic prophylaxis | 0.008 | |||
| 2 Days (24-48 hours) | 10 (24.4) | 2110 (41.2) | ||
| 1 Day (0-24 hours) | 22 (53.7) | 2574 (50.3) | 1.80 | |
| 3 Days (>48 hours) | 9 (22.0) | 433 (8.5) | 4.47 | |
| Perioperative second generation cephalosporins | 14 (34.1) | 2391 (46.7) | 1.11 | 0.751 |
| Ventilation duration, days | 0.8 (0.6, 1.3) | 0.6 (0.4, 1.0) | 1.08 | 0.007 |
| Non-chest infection (prior to onset of first mediastinital infection) | 8 (19.5) | 554 (10.8) | 2.00 | 0.079 |
Continuous variables are expressed as median (IQR). Categorical variable is described as count (%).
Based on Cox proportional hazards model where outcome is time to chest infection and predictor is postoperative characteristic.
91.1% of patients had on-pump surgical procedure
24 patients with chest infection and 2345 without chest infection underwent CABG (isolated or combined)
Timing and Organisms Responsible for Mediastinal Infections
Median time to first mediastinal infection was 20 days (IQR 14 – 28). Nearly two-thirds of mediastinal infections were diagnosed after discharge. Eight patients had another infection prior to the onset of the mediastinal infection (2 had prior superficial sternal wound infections, 3 had symptomatic urinary tract infections [UTI], 1 had endocarditis, 2 had bloodstream infections, 1 had a symptomatic UTI and a bloodstream infection, and 1 had a superficial chest surgical site infection and a bloodstream infection).
Data regarding the organisms responsible for the mediastinal infection were available in 39 (90%) of infections. There was a single organism isolated in 33 infections (85%), while two organisms were isolated in 5 infections (13%), and three organisms were isolated in one infection (3%). The most common organism isolated was Staphylococcus aureus (41%). Most isolates (67%) were gram positive; 26% were gram negative, and the remaining isolates were yeast or mold (7%). Among the patients with multiple isolates, 5 had both gram positive and gram negative bacteria; 1 had gram positive bacteria and yeast or mold. The occurrence of Mycobacterium chimaera was not specifically captured.
Risk Factors for Mediastinal Infection
Preoperative characteristics associated with increased risk of mediastinal infection in multivariate analysis included higher BMI (HR 1.06; 95% CI, 1.01-1.10; p = 0.013) and creatinine (HR 1.25; 95% CI, 1.13 – 1.38; p < 0.001), peripheral vascular disease (HR 2.25; 95% CI, 1.06 to 4.78; p < 0.035), and corticosteroid use (HR 3.33; 95% CI, 1.27 – 8.76; p = 0.015; see Figure 2). VAD and transplant operations were also associated with an increased risk of mediastinal infection (HR, 5.30; 95% CI, 2.12 to 13.27; p < 0.001). Postoperative hyperglycemia occurred in 68% of patients with diabetes and 34% of non-diabetics. Postoperative hyperglycemia was associated with an increased risk of mediastinal infection in non-diabetics (HR 3.15; 95% CI, 1.32 – 7.51) but not in diabetics (HR 0.96; 95% CI, 0.37 – 2.47).
Figure 2. Factors associated with increased risk of mediastinal infection*.
Length of Stay
For patients with onset of mediastinal infection prior to index hospital discharge, observed median time in the ICU was 6 days (IQR, 4 – 11) versus 2 days (IQR, 1 – 3) for patients who did not. Observed median LOS from admission was 33 days (IQR, 28 – 41) versus 8 days (IQR, 6 -12) for these groups. Additional LOS following surgery that was attributable to mediastinal infection was 11.5 days (bootstrap 95% CI, 1.88 – 21.11 days).
Readmissions
There were 945 readmissions among the 5,059 patients discharged alive; 150 readmissions (15.9%) were for infection. Mediastinal infections (n = 26, 17.3%) were collectively the third most common reason for admission due to infection after pneumonia and superficial sternal wound infection. There were 20 readmissions for DSWI, 4 for mediastinitis, and 2 for myocarditis or pericarditis. Readmission rates within 65 days were 0.470 per patient month in the mediastinal infection group compared to 0.089 per patient month in the group without mediastinal infections (p < 0.001).
Mediastinal Infection and Mortality
Death was more common among patients with mediastinal infection (7.32% vs. 1.84%). In a Cox proportional hazards model treating mediastinal infection as a time-varying covariate and adjusting for variables determined to be associated with risk of mortality in the entire cohort (age, male sex, baseline creatinine, congestive heart failure, and diabetes), mediastinal infection was associated with a five-fold increase in risk of mortality (HR 5.414; 95% CI, 1.67 – 17.53, p = 0.005, Figure 3 and Supplemental Table 1,).
Figure 3. Survival by time-varying chest infection status for the hypothetical “average” patient in cohort.
Comment
In this prospective multi-institutional study, we demonstrated that mediastinal infection after cardiac surgery is often diagnosed after initial discharge and is associated with increased length of stay, readmissions and mortality. In addition, those with higher BMI and pre-operative creatinine, receiving baseline corticosteroids, with peripheral vascular disease, and undergoing VAD placement or transplantation are at increased risk of developing a mediastinal infection. In addition, non-diabetics who experience postoperative hyperglycemic episodes are at increased risk of developing these infections.
The incidence of mediastinal infection in this study was 0.79% at 65 days of follow-up, similar to what has been reported in other studies over the past two decades. It is somewhat surprising that the incidence in this study remains at levels seen historically given the high level of adherence with Surgical Care Improvement Project (SCIP) and Society for Thoracic Surgeons (STS) guidelines[1,4,9]. The stable rate of these devastating infections suggests that prevention is not achieved by simple adherence to guidelines, but may also be related to potentially non-modifiable patient risk factors and the surgical procedure.
Our findings are similar to other reports showing that BMI, preoperative creatinine, peripheral vascular disease, and VAD or transplant surgery are risk factors for mediastinal infection. Moreover, postoperative hyperglycemia was found to be a risk factor in non-diabetic patients. The literature has somewhat conflicting findings related to post-operative hyperglycemia and diabetes. Some studies have shown hyperglycemia in diabetic patients to be associated with increased risk of infection or death while others have shown hyperglycemia to be a risk factor only in non-diabetic patients or even to be protective in diabetic patients.[13-17] There might be several reasons for these discrepancies, including differences in the study populations, as diabetes defines a heterogeneous illness with a broad spectrum of severity, or differences in the study definitions of hyperglycemia. Our study defined hyperglycemia as a single blood glucose measurement above a given threshold (180 mg/dL) < 48 hours after surgery while others considered the average or median blood glucose over an extended period of time. Prolonged or extreme hyperglycemia may be a risk factor in diabetics; however, small numbers of such patients in our study limit our ability to explore this hypothesis.
Unlike other studies, we did not find an increased risk of mediastinal infection with urgent procedure status, increased blood transfusions, bilateral internal mammary artery grafting (BIMA) in CABG patients, or type or duration of antibiotic. Procedure status was not predictive of any major infection in the overall cohort, so it is not unexpected that neither is predictive of mediastinal infection alone.[1] Blood transfusions were highly correlated with procedure, particularly VAD and transplant procedures and were not a significant predictor independent of these procedures.
Some studies have shown an increased risk of mediastinal infection with BIMA grafting, particularly in diabetic and/or obese patients, likely due to the decreased sternal blood supply.[18-20] It has been suggested that BIMA harvest and grafting is not a risk factor for chest infection if patients are selected properly (i.e., are not diabetic and/or obese).[21] We found that diabetic CABG patients in this cohort were significantly less likely to have BIMA grafts (odds ratio [OR] 0.650; 95% CI, 0.538 – 0.786; p < 0.0001) which may explain why we did not observe an increased risk of mediastinal infection with BIMA grafting.
We also did not find that nasal decontamination or scrubbing with chlorhexidine preparations was protective of mediastinal infection as others have found.[22,23] Although nasal decontamination and chlorhexidine scrubs target S. aureus, S. aureus was still the most common isolate in this study (22 of 46 infections). Interestingly, this is less common than the reported incidence of up to 80% presence in mediastinal infections cited in the literature. [24-26]
Most of the risk factors identified in this study are patient factors that are not modifiable; however postoperative glycemic control may represent an opportunity to reduce the incidence of mediastinal infections particularly in patients without diabetes. Nonetheless, whether acute hyperglycemia truly increases the risk of infection or is merely marker of a sicker, more vulnerable patient is unknown.
Perhaps most importantly, this study clearly demonstrates the added morbidity and mortality associated with the development of a mediastinal infection after cardiac surgery. In addition, those with mediastinal infections have increased length of stays and more frequent hospital readmission.
This study has several important limitations. The purpose of the “Management Practices and the Risk of Infection Following Cardiac Surgery study” was to identify management practices associated with a reduced risk of a broad range of infections, and therefore the power to look at specific infections is limited. With a larger sample size and number of events, we may have discovered additional factors associated with risk of infection in a multivariate model. Most of the mediastinal infections identified occurred relatively late in the 65 day follow up period, thus additional events may have been discovered with longer follow up. Blood glucose measurements were only recorded every 6 hours for the first 48 hours after surgery; additional measurements or measurements beyond the first 48 hours may have been illusory. We unfortunately also lack data regarding management of these infections.
In conclusion, the incidence of mediastinal infections is low in experienced cardiac surgery centers, however, these infections have a substantial effect on length of stay, readmissions, and mortality. BMI, peripheral vascular disease, preoperative creatinine and corticosteroid use, and VAD or transplant surgery are risk factors for this complication. Improving postoperative glycemic management may reduce the risk of mediastinal infection.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gelijns AC, Moskowitz AJ, Acker MA, et al. Management practices and major infections after cardiac surgery. J Am Coll Cardiol. 2014;64:372–81. doi: 10.1016/j.jacc.2014.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greco G, Shi W, Michler RE, et al. Costs associated with health care-associated infections in cardiac surgery. J Am Coll Cardiol. 2015;65:15–23. doi: 10.1016/j.jacc.2014.09.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Risnes I, Abdelnoor M, Almdahl SM, Svennevig JL. Mediastinitis after coronary artery bypass grafting risk factors and long-term survival. Ann Thorac Surg. 2010;89:1502–9. doi: 10.1016/j.athoracsur.2010.02.038. [DOI] [PubMed] [Google Scholar]
- 4.Eklund AM, Lyytikäinen O, Klemets P, et al. Mediastinitis After More Than 10,000 Cardiac Surgical Procedures. Ann Thorac Surg. 2006;82:1784–9. doi: 10.1016/j.athoracsur.2006.05.097. [DOI] [PubMed] [Google Scholar]
- 5.Shaikhrezai K, Robertson FL, Anderson SE, Slight RD, Brackenbury ET. Does the number of wires used to close a sternotomy have an impact on deep sternal wound infection? Interactive Cardiovascular and Thoracic Surgery. 2012;15:219–22. doi: 10.1093/icvts/ivs200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tschudin-Sutter S, Meinke R, Schuhmacher H, et al. Drainage days-an independent risk factor for serious sternal wound infections after cardiac surgery: a case control study. Am J Infect Control. 2013;41:1264–7. doi: 10.1016/j.ajic.2013.03.311. [DOI] [PubMed] [Google Scholar]
- 7.Zeitani J, Penta de Peppo A, De Paulis R, et al. Benefit of partial right-bilateral internal thoracic artery harvesting in patients at risk of sternal wound complications. Ann Thorac Surg. 2006;81:139–43. doi: 10.1016/j.athoracsur.2005.06.025. [DOI] [PubMed] [Google Scholar]
- 8.Gummert JF, Barten MJ, Hans C, et al. Mediastinitis and cardiac surgery--an updated risk factor analysis in 10,373 consecutive adult patients. Thorac Cardiovasc Surg. 2002;50:87–91. doi: 10.1055/s-2002-26691. [DOI] [PubMed] [Google Scholar]
- 9.Balachandran S, Lee A, Denehy L, et al. Risk Factors for Sternal Complications After Cardiac Operations: A Systematic Review. Ann Thorac Surg. 2016;102:2109–17. doi: 10.1016/j.athoracsur.2016.05.047. [DOI] [PubMed] [Google Scholar]
- 10.Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–32. doi: 10.1016/j.ajic.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Fine JP, Gray RJ. A Proportional Hazards Model for the Subdistribution of a Competing Risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 12.Allignol A, Schumacher M, Beyersmann J. Empirical Transition Matrix of Multi-State Models: The etm Package. J Stat Softw. 2011;38(4) [Google Scholar]
- 13.Furnary AP, Wu Y. Clinical effects of hyperglycemia in the cardiac surgery population: the Portland Diabetic Project. Endocr Pract. 2006;12(3):22–6. doi: 10.4158/EP.12.S3.22. [DOI] [PubMed] [Google Scholar]
- 14.Frioud A, Comte-Perret S, Nguyen S, Berger MM, Ruchat P, Ruiz J. Blood glucose level on postoperative day 1 is predictive of adverse outcomes after cardiovascular surgery. Diabetes Metab. 2010;36:36–42. doi: 10.1016/j.diabet.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 15.Székely A, Levin J, Miao Y, et al. Impact of hyperglycemia on perioperative mortality after coronary artery bypass graft surgery. J Thorac Cardiovasc Surg. 2011;142:430–1. doi: 10.1016/j.jtcvs.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 16.Swenne CL, Lindholm C, Borowiec J, Schnell AE, Carlsson M. Peri-operative glucose control and development of surgical wound infections in patients undergoing coronary artery bypass graft. J Hosp Infect. 2005;61:201–12. doi: 10.1016/j.jhin.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 17.Greco G, Ferket BS, D'Alessandro DA, et al. Diabetes and the Association of Postoperative Hyperglycemia With Clinical and Economic Outcomes in Cardiac Surgery. Diabetes Care. 2016;39:408–17. doi: 10.2337/dc15-1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kouchoukos NT, Wareing TH, Murphy SF, Pelate C, Marshall WG., Jr Risks of bilateral internal mammary artery bypass grafting. Ann Thorac Surg. 1990;49:210–9. doi: 10.1016/0003-4975(90)90140-2. [DOI] [PubMed] [Google Scholar]
- 19.Eagle KA, Guyton RA, Davidoff R, et al. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery) Circulation. 2004;110:e340–437. [PubMed] [Google Scholar]
- 20.Borger MA, Rao V, Weisel RD, et al. Deep sternal wound infection: risk factors and outcomes. Ann Thorac Surg. 1998;65:1050–6. doi: 10.1016/s0003-4975(98)00063-0. [DOI] [PubMed] [Google Scholar]
- 21.Ridderstolpe L, Gill H, Granfeldt H, Ahlfeldt H, Rutberg H. Superficial and deep sternal wound complications: incidence, risk factors and mortality. Eur J Cardiothorac Surg. 2001;20:1168–75. doi: 10.1016/s1010-7940(01)00991-5. [DOI] [PubMed] [Google Scholar]
- 22.Wenzel RP. Minimizing surgical-site infections. N Engl J Med. 2010;362:75–7. doi: 10.1056/NEJMe0908753. [DOI] [PubMed] [Google Scholar]
- 23.Segers P, Speekenbrink RGH, Ubbink DT, van Ogtrop ML, de Mol BA. Prevention of nosocomial infection in cardiac surgery by decontamination of the nasopharynx and oropharynx with chlorhexidine gluconate: a randomized controlled trial. JAMA. 2006;296:2460–6. doi: 10.1001/jama.296.20.2460. [DOI] [PubMed] [Google Scholar]
- 24.Baskett RJ, MacDougall CE, Ross DB. Is mediastinitis a preventable complication? A 10-year review. Ann Thorac Surg. 1999;67:462–5. doi: 10.1016/s0003-4975(98)01195-3. [DOI] [PubMed] [Google Scholar]
- 25.Risnes I, Abdelnoor M, Ulimoen G, et al. Mediastinitis after coronary artery bypass grafting increases the incidence of left internal mammary artery obstruction. Int Wound J. 2014;11:594–600. doi: 10.1111/iwj.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huckfeldt R, Redmond C, Mikkelson D, Finley PJ, Lowe C, Robertson J. A clinical trial to investigate the effect of silver nylon dressings on mediastinitis rates in postoperative cardiac sternotomy incisions. Ostomy Wound Manage. 2008;54:36–41. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.