Abstract
Background
A thorough history and physical examination in patients with blunt abdominal trauma (BAT) is important to safely exclude clinically significant intra-abdominal injury (IAI). We seek to evaluate a correlation between self-reported abdominal pain, abdominal tenderness on examination and IAI discovered on CT or during exploratory laparotomy.
Methods
This retrospective analysis assessed patients with BAT ≥13 years old who arrived to the emergency department following BAT during the 23-month study period. Upon arrival, the trauma team examined all patients. Only those who underwent an abdominal and pelvic CT scan were included. Patients were excluded if they were unable to communicate or lacked documentation, had obvious evidence of extra-abdominal distracting injuries, had a positive drug or alcohol screen, had a Glasgow Coma Scale ≤13, or had a positive pregnancy screening. The primary objective was to assess the agreement between self-reported abdominal pain and abdominal tenderness on examination and IAI noted on CT or during exploratory laparotomy.
Results
Among the 594 patients included in the final analysis, 73.1% (n=434) had no self-reported abdominal pain, 64.0% (n=384) had no abdominal tenderness on examination, and 22.2% (n=132) had positive CT findings suggestive of IAI. Among the 352 patients who had no self-reported abdominal pain and no abdominal tenderness on examination, a significant number of positive CT scan results (14%, n=50) were still recorded. Furthermore, a small but clinically significant portion of these 50 patients underwent exploratory laparotomy (1.1%, n=4). All four of these patients ultimately underwent a splenectomy and all were completed on hospital day one.
Conclusion
Lack of abdominal pain and tenderness in patients with BAT with non-distracting injuries was associated with a small portion of patients who underwent a splenectomy. Patients with BAT without abdominal pain or tenderness may need a period of observation or CT scan to rule out IAI prior to discharge home.
Level of evidence
Level III, therapeutic/care management.
Keywords: blunt abdominal trauma, abdominal pain, abdominal tenderness, intra-abdominal injury
Introduction
Blunt abdominal trauma (BAT), most commonly resulting from motor vehicle accidents (MVA) and falls, is a mechanism of injury frequently encountered by both emergency physicians and trauma surgeons.1 2 Unlike penetrating abdominal injuries, unclear signs of traumatic injuries after BAT often leaves many treatment decisions to the acumen of the clinician.3–5 These challenges may result in a under triage and a delayed diagnosis of significant intra-abdominal injury (IAI) secondary to BAT, the consequences of which may potentially lead to severe morbidity and mortality.6–8 The estimated prevalence of IAI in patients with BAT presenting to the emergency department (ED) were reported at 13%; those with clinically significant injuries were reported at 4.7%.9
A thorough history and physical examination remains the primary initial step toward diagnosing IAI in patients with BAT; however, the reliability of this examination has been questioned.10 11 Studies suggest that in select situations, the physical examination alone may not be sufficient for excluding IAI.3 4 12–15 The utility of abdominal tenderness on physical examination as a screen for IAI was observed to be of limited sensitivity and specificity (ranging from 46% to 82% for sensitivity and 41% to 69% for specificity).12 13 16 Further, patients with trauma often present with altered mental status (AMS) and multisystem trauma resulting in distracting injuries, which may lead to an unreliable physical examination.2 4 9 12
CT has become an important adjunct to the physical examination when evaluating hemodynamically stable patients with blunt trauma with equivocal findings.9 10 14 16–19 A high-grade sensitivity (97%–98%) and specificity (97%–99%) for diagnosing IAI in patients with BAT has been noted and there have been several studies that advocate for the utilization of CT as a screening tool in patients with blunt trauma.16 18 20–22 One study reported that liberal whole body CT imaging in patients with blunt multisystem trauma without obvious signs of injury changed the course of management in nearly 19% of patients (eg, discharged home, sent directly to the operating room).21 However, others argue that the diagnostic yield of these additional CT findings may not significantly change overall patient management, resulting only in unnecessary patient radiation exposure, inefficient resource management, excessive patient and hospital expense, and increased time of initial evaluation.21 23–28
The utility of the history and physical examination during the initial assessment for IAI in patients with BAT is controversial. We seek to assess the feasibility of using self-reported abdominal pain and abdominal tenderness findings on physical examination to safely exclude IAI among patients with BAT by comparing these initial findings with CT scan and surgical findings.
Methods
This retrospective study was approved by the institutional review board at Arrowhead Regional Medical Center (ARMC). ARMC is a 456-bed acute care teaching facility and the only American College of Surgeons certified level II trauma center located in San Bernardino County, California, USA. The ARMC ED is one of the busiest in the state of California with more than 92 000 visits and over 2500 traumas annually.
Emergency and surgical attending or resident physicians completed the initial examination of patients with BAT. Patients with trauma presenting to the ARMC ED during the 23-month study period from 1 February 2009 to 31 December 2010, with documented BAT who received a CT scan were extracted from the trauma registry. All patients with BAT were initially evaluated and managed according to Advanced Trauma Life Support (ATLS) protocol in the ED by trauma team members.29 Obtaining CT imaging with intravenous contrast was based on provider clinical judgement. Patients deemed low risk by the trauma team for IAI based on mechanism of injury did not receive a CT scan, as well as hemodynamically unstable patients with BAT who were transferred directly to the operating room.29 These patients were not included in our analysis. Our institutional protocol for adult splenectomy is based on hemodynamic stability. Splenectomy is performed if the patient fails non-operative management based on hemodynamic instability. Based on this protocol, our institution salvage rate is 95%.
The inclusion criteria were (1) patients ≥13 years of age presenting with BAT following a motor vehicle accident (MVA) or motor cycle accident (MCA), (2) Glasgow Coma Scale (GCS) score of >13, (3) patients who received a complete history and physical examination by trauma team members, and (4) patients who received a CT abdomen and pelvis with intravenous contrast while in the ED. Patients were excluded from the study if they were (1) unable to communicate or were lacking documentation in the medical record, (2) under the influence of alcohol intoxication (blood alcohol level >0.08%) or illicit drug use documented on urine drug screen completed as part of the routine trauma panel for all patients with trauma at our trauma centre, (3) distracting extra-abdominal injuries (eg, long bone fractures, large lacerations or degloving injuries, crush injuries, large burns, or other obvious extra-abdominal injuries documented in the medical record and noted to have sufficiently distracted from a reliable abdominal exam), and (4) patients with a positive pregnancy test on urine qualitative human chorionic gonadotropin testing. Inclusion and exclusion criteria aimed to reduce the incidence of distracting injuries and were validated in previous studies.4 5 12–14 24 30
The primary objective was to assess the agreement between abdominal pain and abdominal tenderness findings (both self-reported and on physical examination), and IAI noted on CT or during exploratory laparotomy among patients with BAT. Patients reporting abdominal pain during the initial encounter were recorded as positive for self-reported abdominal pain. Patients with any noted findings of abdominal tenderness on physical examination including tenderness to palpation were recorded as having positive abdominal tenderness on physical examination. A positive CT scan (Brilliance CT 64 Channel-DS; Phillips, Andover, Massachusetts, USA) was defined as exhibiting any of the following findings, regardless of the lesion severity: liver injury (eg, hematoma, laceration), splenic injury, kidney injury, bowel injury (eg, perforation, edema), great vessel injury, free fluid, and/or free air. All abdominal and pelvic CT imaging was completed with intravenous contrast by certified technologists and interpreted by radiology attending or resident physicians. A positive surgical finding included any surgical intervention undertaken to stabilize the patients during exploratory laparotomy. Intra-abdominal organ injury noted on CT imaging and during exploratory laparotomy was classified based on the American Association for the Surgery of Trauma grading scale.31
Additional variables assessed in this study included sex, ethnicity, GCS, injury severity score (ISS), mechanism of injury, intra-abdominal findings on exploratory laparotomy, time to surgical intervention, and patient outcomes for those who underwent surgical intervention.
Statistical analysis
All statistical analyses were conducted using the SAS software for windows version 9.3 (SAS Institute, Cary, North Carolina, USA). Descriptive statistics were presented as frequencies and proportions for continuous variables. Χ2 cross-tab analyses were conducted to identify associations between factors associated with subjective, objective, and combined abdominal pain or tenderness findings separately. All statistical analyses were two sided. p<0.05 was considered to be statistically significant.
Results
Of the original 818 patients, 594 patients were included in the final analysis (see figure 1 for flow chart). A total of 224 patients were excluded due to extra-abdominal distracting injuries (n=83), alcohol intoxication (n=89), GCS≤13 (n=50), drug intoxication (n=16), unreliable history or lack of medical documentation (n=16), and positive pregnancy screen (n=1). More than half of the sample population were male (64%, n=380, table 1). Less than half identified as Caucasian (45.5%, n=270), followed by Hispanic (38.6%, n=229). The median ISS of 10 (Q1 7, Q3 17) and had a GCS 15 (n=535, 90.1%).
Figure 1.
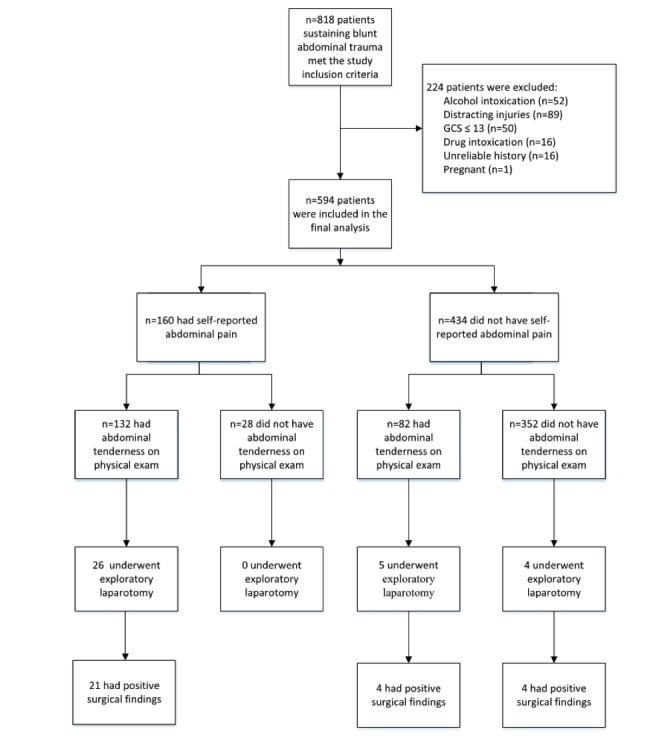
Patient flow chart.
Table 1.
Demographic summary of the included patients (n=594)
| Frequency (n=594) |
Percentage (%) | |
|---|---|---|
| Sex | ||
| Female | 214 | 36 |
| Male | 380 | 64 |
| Ethnicity | ||
| African American | 44 | 7.4 |
| Asian | 32 | 5.4 |
| Caucasian | 270 | 45.5 |
| Hispanic | 229 | 38.6 |
| Other | 19 | 3.2 |
| Glasgow Coma Scale | ||
| 14 | 59 | 9.9 |
| 15 | 535 | 90.1 |
| Self-reported abdominal pain | ||
| No | 434 | 73.1 |
| Yes | 160 | 26.9 |
| Abdominal tenderness on examination | ||
| No | 380 | 64 |
| Yes | 214 | 36 |
| CT scan findings | ||
| Negative | 462 | 77.8 |
| Positive | 132 | 22.2 |
| Exploratory laparotomy | ||
| No | 559 | 94.1 |
| Yes | 35 | 5.9 |
| Exploratory laparotomy findings | ||
| Negative | 6 | 17.1 |
| Positive | 29 | 82.9 |
| Frequency missing=563 | ||
| Abdominal pain or tenderness | ||
| Negative self-reported abdominal pain and negative abdominal tenderness on physical examination | 352 | 59.3 |
| Negative self-reported abdominal pain and positive abdominal tenderness on physical examination | 82 | 13.8 |
| Positive self-reported abdominal pain and negative abdominal tenderness on physical examination | 28 | 4.7 |
| Positive self-reported abdominal pain and positive abdominal tenderness on physical examination | 132 | 22.2 |
| Injury severity score, median (Q1, Q3) | 10 (7, 17) | |
Table 1 also presented the self-reported abdominal pain and abdominal tenderness findings on physical examination. Overall, 73.1% (n=434) reported no abdominal pain, 64% (n=380) had no abdominal tenderness on physical examination, and 22.2% (n=132) had positive CT findings suggestive of IAI. A total of 35 (5.9%) patients of the total cohort underwent an exploratory laparotomy. Of these 35 patients, 29 had positive intraoperative abdominal findings on exploratory laparotomy for which surgical intervention was undertaken for patient stabilization. A total of 356 (59.4%) patients had both a negative self-reported abdominal pain and negative abdominal tenderness on physical examination.
Further examination of self-reported abdominal pain and abdominal tenderness findings on physical examination was conducted. The results were presented in table 2. Of the patients without self-reported abdominal pain and abdominal tenderness on physical examination, a significant number of positive CT scan results (14.2%, n=50) were recorded. Furthermore, a small but clinically significant portion of patients with seemingly benign abdominal findings underwent exploratory laparotomy and splenectomy after non-operative splenic salvage failed due to hemodynamic instability (1.1%, n=4) (see table 3 for details on mechanism of injury, intra-abdominal findings, and outcomes). Of the patients with positive self-reported abdominal pain and abdominal tenderness on physical examination, positive CT findings were noted in 40.6% (n=53), exploratory laparotomies were undertaken in 19.7% (n=26), and positive surgical findings were noted in 15.9% (n=21).
Table 2.
Factors associated with having abdominal pain findings
| Abdominal pain or tenderness | N | Positive CT finding | Had exploratory laparotomy | Positive surgical finding | |||
| N (%) | p Value | N (%) | p Value | N (%) | p Value | ||
| Self-reported abdominal pain | |||||||
| No | 434 | 75 (17.3) | <0.001 | 9 (2.1) | <0.001 | 8 (1.8) | 0.1093 |
| Yes | 160 | 57 (35.6) | 26 (16.3) | 21 (13.1) | |||
| Abdominal tenderness on physical examination | |||||||
| No | 380 | 54 (14.2) | <0.001 | 4 (1.1) | <0.001 | 4 (1.1) | 0.0415 |
| Yes | 214 | 78 (36.5) | 31 (14.5) | 25 (11.7) | |||
| Negative self-reported abdominal pain and negative abdominal tenderness on physical examination | 352 | 50 (14.2) | <0.001 | 4 (1.1) | <0.001 | 4 (1.1) | 0.0043 |
| Negative self-reported abdominal pain and positive abdominal tenderness on physical examination | 82 | 25 (30.5) | 5 (6.1) | 4 (4.9) | |||
| Positive self-reported abdominal pain and negative abdominal tenderness on physical examination | 28 | 4 (14.3) | 0 (0) | 0 (0) | |||
| Positive self-reported abdominal pain and positive abdominal tenderness on physical examination | 132 | 53 (40.2) | 26 (19.7) | 21 (15.9) | |||
*The corresponding p value was <0.05 among the four abdominal pain groups.
Table 3.
Surgical findings among the patients presenting without self-reported abdominal pain or abdominal tenderness on physical examination
| ID | Self-reported abdominal pain | Abdominal tenderness on examination | Mechanism of injury | Intra-abdominal findings | Time from arrival to surgical intervention (min) | Outcome |
| 1 | No | No | Rollover MVA | Grade 3 splenic laceration s/p exploratory laparotomy with splenectomy | 99 | Discharged home on day 6 |
| 2 | No | No | MVA | Grade 4 splenic laceration s/p exploratory laparotomy with splenectomy | 151 | Discharged home on day 13 |
| 3 | No | No | MVA | Grade 2 liver laceration, Grade 5 splenic laceration post s/p exploratory laparotomy with splenectomy | 84 | Discharged home on day 7 |
| 4 | No | No | Rollover MVA | Grade 4 splenic laceration s/p exploratory laparotomy with splenectomy | 102 | Discharged home on day 4. |
| 5 | No | Yes | Rollover MVA | Extraperitoneal bladder rupture with intraperitoneal fluid s/p exploratory laparotomy with bladder repair | 270 | Discharged home on day 7 |
| 6 | No | Yes | MVA | Sigmoid mesenteric injury with arterial bleed s/p exploratory laparotomy with mesenteric vessel ligation | 176 | Discharged home on day 5 |
| 7 | No | Yes | MCA | Left colonic injury, left renal artery injury, and abdominal compartment syndrome s/p exploratory laparotomy with abdominal decompression and bogota bag placement | 99 | Discharged home on day 63 |
| 8 | No | Yes | MVA | Grade 4 splenic laceration, grade 1 left renal laceration s/p exploratory laparotomy with splenectomy and transverse colon resection | 220 | Discharged home on day 5 |
| 9 | Yes | Yes | MVA | Gangrene of the ileum, cecum, and sigmoid s/p exploratory laparotomy with ileal, cecal, sigmoidal resection | 220 | Deceased on hospital day 2 |
| 10 | Yes | Yes | MCA | Grade 4 splenic laceration s/p exploratory laparotomy with splenectomy | 125 | Discharged home on day 4 |
| 11 | Yes | Yes | MCA | Grade 4 splenic laceration s/p exploratory laparotomy with splenectomy | 90 | Discharged home on day 4 |
| 12 | Yes | Yes | MCA | Grade 3 splenic laceration s/p exploratory laparotomy with splenectomy | 135 | Discharged home on day 5 |
| 13 | Yes | Yes | MVA | Avulsion of the mesentery of the distal ileum, transverse colon, and sigmoid colon s/p exploratory laparotomy with resection of small bowel, sigmoid resection and primary anastomosis | 125 | Discharged home on day 5 |
| 14 | Yes | Yes | MCA | Grade 3 pancreatic tail laceration, grade 1 splenic laceration, grade 1 renal laceration s/p exploratory laparotomy with distal pancreatectomy and splenectomy | 165 | Discharged home on day 6 |
| 15 | Yes | Yes | MVA | Avulsion of the small bowel and sigmoid mesentery with mesenteric bleeding s/p exploratory laparotomy with sigmoidectomy, small bowel resection, and primary anastomosis | 65 | Transferred to outside facility on day 5 |
| 16 | Yes | Yes | MVA | Retroperitoneal hematoma s/p embolization by interventional radiology | 340 | Discharged home on day 3 |
| 17 | Yes | Yes | MCA | Left diaphragmatic rupture s/p exploratory laparotomy with diaphragmatic repair | 61 | Discharged home on day 18 |
| 18 | Yes | Yes | Rollover MVA | Small bowel perforation and grade 1 splenic laceration s/p exploratory laparotomy with small bowel resection and primary anastomosis | 896 | Discharged home on day 11 |
| 19 | Yes | Yes | Rollover MVA | Small bowel and mesenteric injury s/p exploratory laparotomy with small bowel resection and primary anastomosis | 255 | Discharged home on day 11 |
| 20 | Yes | Yes | MVA | Mesenteric avulsion of the distal ileum and ascending colon, deserosalization of the sigmoid colon, grade 1 liver laceration without active bleeding s/p exploratory laparotomy with right hemicolectomy and sigmoid colectomy | 36 | Transferred to outside facility on day 9 |
| 21 | Yes | Yes | MVA | Ruptured abdominal aortic aneurysm and ruptured iliac aneurysm s/p exploratory laparotomy with abdominal aortic aneurysm repair and left-sided aortoiliac anastomosis and right-sided aortofemoral anastomosis | 164 | Deceased on hospital day 2 |
| 22 | Yes | Yes | MVA | Right colon and mid-transverse colon necrotic and necrotic, non-perforated gallbladder s/p exploratory laparotomy with hemicolectomy and cholecystectomy | 205 | Discharged home on day 22 |
| 23 | Yes | Yes | MVA | Small bowel and right colon injury s/p exploratory laparotomy with small bowel resection and distal ileum to right colon resection with anastomosis | 128 | Discharged home on day 4 |
| 24 | Yes | Yes | MCA | Grade 4 splenic laceration s/p exploratory laparotomy with splenectomy | 375 | Transferred to outside facility on day 4 |
| 25 | Yes | Yes | MVA | Grade 5 splenic laceration s/p exploratory laparotomy with splenectomy | 73 | Discharged home on day 2 |
| 26 | Yes | Yes | MVA | Large jejunal mesenteric tear and ischemic small bowel s/p exploratory laparotomy with small bowel resection and primary anastomosis | 274 | Discharged home on day 4 |
| 27 | Yes | Yes | MVA | Mesenteric hematoma of the gastrocolic artery with no disruption s/p exploratory laparotomy with sigmoid colon colorrhaphy | 175 | Deceased on hospital day 13 |
| 28 | Yes | Yes | MCA | Grade 4 splenic laceration and grade 1 laceration of the left kidney s/p exploratory laparotomy with splenectomy | 137 | Discharged home on day 5 |
| 29 | Yes | Yes | MVA | Mesenteric tear at the transverse colon with active bleeding, mesenteric tear at ileocecal base, grade 1 liver laceration s/p exploratory laparotomy ligation of arteries | 100 | Discharged home on day 2 |
MCA, motorcycle accident; MVA, motor vehicle accident; s/p, status post.
Discussion
The utility of the history and physical examination in the evaluation for IAI in patients with BAT has been widely debated. It is understandable that patients with BAT with distracting injuries or AMS would warrant a CT scan due to the inability to safely exclude IAI.12 However, in patients with normal mentation and without distracting injuries, little evidence exists assessing the correlation between self-reported abdominal pain and abdominal tenderness findings in comparison to IAI noted on CT imaging or during exploratory laparotomy findings in patients with BAT.
In the current investigation, a portion of patients with BAT presenting to our institution did not report abdominal pain or have abdominal tenderness on initial evaluation. These patients were seemingly non-critical as evidenced by their ISS and GCS. However, 14% of these patients with BAT with benign history and physical e had evidence of IAI on CT imaging. Most notably, 1.1% (n=4) of patients without self-reported abdominal pain or abdominal tenderness on examination ultimately underwent an exploratory laparotomy and splenectomy (table 3). These patients exhibited evidence of abdominal free fluid and solid organ injury on CT scan. Non-operative splenic salvage failed after these patients subsequently experienced hemodynamic instability within hours after arrival and splenectomy was undertaken. In one of these cases, splenic embolization had been planned; however, the patient became hypotensive while awaiting the procedure and subsequently underwent a splenectomy. In the other three cases, the patients experienced hemodynamic instability shortly after arrival to the trauma center. As such, splenic embolization was deferred and splenectomy was undertaken.
The explanation for the seemingly benign presentation in this subset of patients is likely multifactorial in nature. It may be explained by the fact that fresh blood is not a significant noxious stimuli initially and only after cell lysis occurs later in a patients clinical course do mechanosensitive pain receptors become activated.32 Additionally, the retroperitoneal nature of the spleen and lack of peritoneal irritation from spilled enteric contents and biliary material has been cited as a potential mechanism contributing to the occasional paucity of abdominal examination findings in similar cases of IAI.12 In these four patients with splenic injuries that did not have abdominal pain or tenderness, their IAI may have been missed without a CT scan.
Few similar studies exist assessing the accuracy of reported abdominal pain and abdominal tenderness findings on physical examination in patients with BAT. Livingston et al completed a large, multi-institutional study of 2299 patients which concluded that although abdominal tenderness made the presence of IAI more likely, 19% of patients with no abdominal tenderness had IAI on CT imaging.14 Ferrera et al noted that among 142 patients without self-reported abdominal pain or findings of abdominal tenderness on physical examination, 10 patients (7%) were found to have IAI on CT imaging.12 One patient expired in the operating room. Of note, all 10 patients in this study had extra-abdominal injuries.12 In another investigation, among 23 patients with isolated BAT and no abnormal abdominal examination findings, seven (30%) were found to have IAI on CT imaging.4 Four (17%) subsequently underwent exploratory laparotomy and injuries noted included intestinal perforation and splenic rupture.
In contrast, a study that assessed 703 hemodynamically stable patients with BAT with negative abdominal exams and no extra-abdominal injuries found that only three (0.4%) of these patients had evidence of IAI on CT.24 These three cases were managed conservatively. Authors from this study suggested that patients with BAT fitting this profile could be safely discharged without adjunctive evaluation with CT or diagnostic peritoneal lavage.24
Despite this evidence, conflicting information still remains that demonstrate that a proportion (1.1%–17%) of seemingly non-critical patients with BAT with normal initial exams ultimately underwent potentially life-saving surgical intervention (though provider-dependent differences may have impacted the accuracy of these compiled findings from our study and other studies).4 12 The four patients in this study underwent splenectomy on hospital day 1 after failed non-operative management (table 3). If the history and physical examination were to be utilized in isolation with this group of potential surgical candidates, this small but clinically significant percentage of patients with BAT with IAI would be at significant risk for a delay in surgical intervention that may result in increased morbidity and mortality.6 8
Patients with BAT with no abdominal pain or tenderness findings and negative abdominal and pelvis CT findings were also assessed in this study. Analysis noted that none of the patients in this subgroup were later diagnosed with IAI, underwent exploratory laparotomy, or died. Holmes et al found that the rate of IAI among 2141 hospitalized patients with BAT with normal CT findings was 0.37% (n=8). Of these eight patients, AMS and extra-abdominal injury were present.18 Authors concluded that in those patients with normal mental status, normal abdominal exams, and normal abdominal CT scans, the rate of IAI was zero. The findings of the current study validate this assertion and support the safe discharge of this portion of patients with unremarkable abdominal and pelvic CT findings directly from the ED.
Past studies have further sought to define a subset of patients with BAT deemed ‘low risk’ that may be discharged from the ED without radiographic imaging or observation. Kendall et al examined 1169 patients with BAT and determined that 20% could be classified as ‘low risk’ based on predefined criteria including lack of abdominal pain or tenderness, vital sign abnormalities, hematuria, distracting injuries, and intoxication. These patients were deemed safe for discharge without observation or CT imaging; none were later diagnosed with IAI or died.30 A similar study validated a decision instrument aimed at identifying patients with BAT at ‘low risk’ for any IAI and who were unlikely to benefit from CT imaging. The sensitivity and specificity were noted at 95.8% and 29.9%, respectively.5 These criteria, which include assessment for abdominal pain and tenderness, appear effective toward accurately identifying and excluding IAI in a proportion of patients with BAT without CT imaging.
Limitations
Due to its retrospective nature, this study was dependent on the accuracy of the providers’ documentation and clinical acumen. The method of abdominal examination and the detail in which the providers documented the patient’s complaint of abdominal pain and the examination findings may differ slightly among the providers. Given this variation in documentation of findings, we were not able to expand our study to include the degree of pain expressed by the patient or the degree of tenderness on examination. Further, variation in provider documentation may also have impacted the identification and exclusion of patients with distracting injuries.
In regard to the physical examination, we only addressed abdominal tenderness. This study did not address other objective abdominal findings including seatbelt sign, contusions, or abrasions. As such, interpretation of the results of our study may be limited to the context of abdominal tenderness findings in correlation with CT imaging and exploratory laparotomy findings.
Another limitation stems from the exclusion of patients with BAT who did not receive an abdominal or pelvic CT. This may have resulted in the missed inclusion of relevant cases. Patients were also not followed after discharge and as such, we were unable to assess if they were seen at other hospitals with similar complaints due to a delayed IAI diagnosis.
Finally, the utilization of ultrasound in the diagnosis of BAT was not considered in this study as bedside ED ultrasound was not fully implemented at our institution during the data collection period. Though ultrasound was available and used at bedside intermittently during trauma patient evaluation, its value may have been operator dependent.33 34 However, this study sought specifically examine the correlation between the history and physical examination and CT scan findings. For this study, the history and physical examination were routinely completed before an ultrasound evaluation, thus eliminating the possibility of any confounding influence of that ultrasound findings may have had on the history and physical examination findings.
Conclusions
Based on the current results, the absence of abdominal pain and tenderness in patients with BAT with non-distracting injuries continues to be associated with a small portion of patients needing life-saving surgical intervention for solid organ injury. In these patients, a period of observation or CT imaging may be utilized as useful adjuncts to identify IAI. The consequence of missed or delayed recognition and treatment of IAI may jeopardize patient’s well-being and be potentially fatal if a patient is unknowingly discharged home.
Overall, patients with BAT present a difficult clinical scenario for emergency physicians and trauma surgeons. Further research is needed to determine additional criteria (eg, vital signs, lab tests, serial abdominal exams, ultrasound exams) to complement an unremarkable history and physical that would aid in accurately identifying IAI and determining patients that could safely be discharged from the ED without observation or CT imaging.
Acknowledgments
Authors would like to thank Sahar Nikdel, Tyler Jacks, Massoud Rabiei, Richard Vara and Sharon Brown for data collection and Michelle McBride for editing.
Footnotes
Contributors: MMN and DW conceived the study. MMN, DW, KJ and KK contributed to the design of the study and development of study protocols. DW and AS were involved in the data collection and database compilation. FD performed statistical analyses. MMN, DH, JT, KK and KJ drafted the initial manuscript. MMN managed all aspects of the study. All authors contributed significantly during the revision process.
Competing interests: None declared.
Patient consent: Detail has been removed from this case description/these case descriptions to ensure anonymity. The editors and reviewers have seen the detailed information available and are satisfied that the information backs up the case the authors are making.
Ethics approval: Institutional Review Board at Arrowhead Regional Medical Center.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Heron M. Deaths: leading causes for 2014. Natl Vital Stat Rep 2016;65:1–96. [PubMed] [Google Scholar]
- 2.Isenhour JL, Marx J. Advances in abdominal trauma. Emerg Med Clin North Am 2007;25:713–33. doi:10.1016/j.emc.2007.06.002 [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez A, DuPriest RW, Shatney CH. Recognition of intra-abdominal injury in blunt trauma victims. A prospective study comparing physical examination with peritoneal lavage. Am Surg 1982;48:457–9. [PubMed] [Google Scholar]
- 4.Schurink GW, Bode PJ, van Luijt PA, van Vugt AB. The value of physical examination in the diagnosis of patients with blunt abdominal trauma: a retrospective study. Injury 1997;28:261–5. doi:10.1016/S0020-1383(97)00007-7 [DOI] [PubMed] [Google Scholar]
- 5.Holmes JF, Wisner DH, McGahan JP, Mower WR, Kuppermann N. Clinical prediction rules for identifying adults at very low risk for intra-abdominal injuries after blunt trauma. Ann Emerg Med 2009;54:575–84. doi:10.1016/j.annemergmed.2009.04.007 [DOI] [PubMed] [Google Scholar]
- 6.Fakhry SM, Brownstein M, Watts DD, Baker CC, Oller D. Relatively short diagnostic delays (<8 hours) produce morbidity and mortality in blunt small bowel injury: an analysis of time to operative intervention in 198 patients from a multicenter experience. J Trauma 2000;48:408–14. [DOI] [PubMed] [Google Scholar]
- 7.Miller PR, Croce MA, Bee TK, Malhotra AK, Fabian TC. Associated injuries in blunt solid organ trauma: implications for missed injury in nonoperative management. J Trauma 2002;53:238–44. doi:10.1097/00005373-200208000-00008 [DOI] [PubMed] [Google Scholar]
- 8.Clarke JR, Trooskin SZ, Doshi PJ, Greenwald L, Mode CJ. Time to laparotomy for intra-abdominal bleeding from trauma does affect survival for delays up to 90 minutes. J Trauma 2002;52:420–5. doi:10.1097/00005373-200203000-00002 [DOI] [PubMed] [Google Scholar]
- 9.Nishijima DK, Simel DL, Wisner DH, Holmes JF. Does this adult patient have a blunt intra-abdominal injury? JAMA 2012;307:1517–27. doi:10.1001/jama.2012.422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoff WS, Holevar M, Nagy KK, Patterson L, Young JS, Arrillaga A, Najarian MP, Valenziano CP. Eastern asociation for the surgery of trauma. Practice management guidelines for the evaluation of blunt abdominal trauma: the East practice management guidelines work group. J Trauma 2002;53:602–15. doi:10.1097/00005373-200209000-00038 [DOI] [PubMed] [Google Scholar]
- 11.ATLS sub committee American college of surgeons’ committee on trauma international ATLS working group. Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care Surg 2013;74:1363–6. doi:10.1097/TA.0b013e31828b82f5 [DOI] [PubMed] [Google Scholar]
- 12.Ferrera PC, Verdile VP, Bartfield JM, Snyder HS, Salluzzo RF. Injuries distracting from intraabdominal injuries after blunt trauma. Am J Emerg Med 1998;16:145–9. doi:10.1016/S0735-6757(98)90032-8 [DOI] [PubMed] [Google Scholar]
- 13.Poletti PA, Mirvis SE, Shanmuganathan K, Takada T, Killeen KL, Perlmutter D, Hahn J, Mermillod B. Blunt abdominal trauma patients: can organ injury be excluded without performing computed tomography? J Trauma 2004;57:1072–81. doi:10.1097/01.TA.0000092680.73274.E1 [DOI] [PubMed] [Google Scholar]
- 14.Livingston DH, Lavery RF, Passannante MR, Skurnick JH, Fabian TC, Fry DE, Malangoni MA. Admission or observation is not necessary after a negative abdominal computed tomographic scan in patients with suspected blunt abdominal trauma: results of a prospective, multi-institutional trial. J Trauma 1998;44:273–80. [DOI] [PubMed] [Google Scholar]
- 15.Mackersie RC, Tiwary AD, Shackford SR, Hoyt DB. Intra-abdominal injury following blunt trauma. Identifying the high-risk patient using objective risk factors. Arch Surg 1989;124:809–13. [DOI] [PubMed] [Google Scholar]
- 16.Richards JR, Derlet RW. Computed tomography for blunt abdominal trauma in the ED: a prospective study. Am J Emerg Med 1998;16:338–42. doi:10.1016/S0735-6757(98)90122-X [DOI] [PubMed] [Google Scholar]
- 17.Heilbrun ME, Chew FS, Tansavatdi KR, Tooze JA. The role of negative CT of the abdomen and pelvis in the decision to admit adults from the emergency department after blunt trauma. J Am Coll Radiol 2005;2:889–95. doi:10.1016/j.jacr.2005.06.013 [DOI] [PubMed] [Google Scholar]
- 18.Holmes JF, McGahan JP, Wisner DH. Rate of intra-abdominal injury after a normal abdominal computed tomographic scan in adults with blunt trauma. Am J Emerg Med 2012;30:574–9. doi:10.1016/j.ajem.2011.02.016 [DOI] [PubMed] [Google Scholar]
- 19.Beck D, Marley R, Salvator A, Muakkassa F. Prospective study of the clinical predictors of a positive abdominal computed tomography in blunt trauma patients. J Trauma 2004;57:296–300. doi:10.1097/01.TA.0000130612.60661.C3 [DOI] [PubMed] [Google Scholar]
- 20.Peitzman AB, Makaroun MS, Slasky BS, Ritter P. Prospective study of computed tomography in initial management of blunt abdominal trauma. J Trauma 1986;26:585–92. doi:10.1097/00005373-198607000-00001 [DOI] [PubMed] [Google Scholar]
- 21.Salim A, Sangthong B, Martin M, Brown C, Plurad D, Demetriades D. Whole body imaging in blunt multisystem trauma patients without obvious signs of injury: results of a prospective study. Arch Surg 2006;141:468–73. doi:10.1001/archsurg.141.5.468 [DOI] [PubMed] [Google Scholar]
- 22.Caputo ND, Stahmer C, Lim G, Shah K. Whole-body computed tomographic scanning leads to better survival as opposed to selective scanning in trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg 2014;77:534–9. doi:10.1097/TA.0000000000000414 [DOI] [PubMed] [Google Scholar]
- 23.Gupta M, Schriger DL, Hiatt JR, Cryer HG, Tillou A, Hoffman JR, Baraff LJ. Selective use of computed tomography compared with routine whole body imaging in patients with blunt trauma. Ann Emerg Med 2011;58:e15:407–16. doi:10.1016/j.annemergmed.2011.06.003 [DOI] [PubMed] [Google Scholar]
- 24.Grieshop NA, Jacobson LE, Gomez GA, Thompson CT, Solotkin KC. Selective use of computed tomography and diagnostic peritoneal lavage in blunt abdominal trauma. J Trauma 1995;38:727–31. doi:10.1097/00005373-199505000-00008 [DOI] [PubMed] [Google Scholar]
- 25.Gardner RL, Sarkar U, Maselli JH, Gonzales R. Factors associated with longer ED lengths of stay. Am J Emerg Med 2007;25:643–50. doi:10.1016/j.ajem.2006.11.037 [DOI] [PubMed] [Google Scholar]
- 26.Pannu N, Wiebe N, Tonelli M. Alberta kidney disease network. Prophylaxis strategies for contrast-induced nephropathy. JAMA 2006;295:2765–79. doi:10.1001/jama.295.23.2765 [DOI] [PubMed] [Google Scholar]
- 27.Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, Berrington de González A, Miglioretti DL. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med 2009;169:2078–86. doi:10.1001/archinternmed.2009.427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rizzo AG, Steinberg SM, Flint LM. Prospective assessment of the value of computed tomography for trauma. J Trauma 1995;38:338–43. doi:10.1097/00005373-199503000-00005 [DOI] [PubMed] [Google Scholar]
- 29.Kool DR, Blickman JG. Advanced trauma life support. ABCDE from a radiological point of view. Emerg Radiol 2007;14:135–41. doi:10.1007/s10140-007-0633-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kendall J, Kestler A, Whitaker K, Adkisson M-M, Haukoos J, et al. Blunt abdominal trauma patients are at very low risk for intra-abdominal injury after emergency department observation. West J Emerg Med 2011;12:496–504. doi:10.5811/westjem.2010.11.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moore EE, Shackford SR, Pachter HL, McAninch JW, Browner BD, Champion HR, Flint LM, Gennarelli TA, Malangoni MA, Ramenofsky ML. Organ injury scaling: spleen, liver, and kidney. J Trauma 1989;29:1664–6. [PubMed] [Google Scholar]
- 32.Kamkin A, Kiseleva I, Mechanosensitivity in cells and tissues. Moscow: Academia, 2005. [PubMed] [Google Scholar]
- 33.Tsui CL, Fung HT, Chung KL, Kam CW. Focused abdominal sonography for trauma in the emergency department for blunt abdominal trauma. Int J Emerg Med 2008;1:183–7. doi:10.1007/s12245-008-0050-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carter JW, Falco MH, Chopko MS, Flynn WJ, Wiles Iii CE, Guo WA. Do we really rely on fast for decision-making in the management of blunt abdominal trauma? Injury 2015;46:817–21. doi:10.1016/j.injury.2014.11.023 [DOI] [PubMed] [Google Scholar]


