Significance
Emerging respiratory pathogens pose significant public health threats as a result of their potential for rapid global spread via multiple non-mutually exclusive modes of transmission. The relative significance of contact, droplet, and airborne transmission for many respiratory pathogens remains a knowledge gap, and better understanding is essential for developing evidence-based measures for effective infection control. Here, we describe and evaluate a transmission chamber that separates virus-laden particles in air by size to study airborne particles that mediate influenza transmission in ferrets. Our results provide direct experimental evidence of influenza transmission via droplets and fine droplet nuclei, albeit at different efficiency. This transmission device can also be applied to elucidate the mode of transmission of other respiratory pathogens.
Keywords: influenza virus, droplet transmission, airborne transmission, airborne particles, ferrets
Abstract
Epidemics and pandemics of influenza are characterized by rapid global spread mediated by non-mutually exclusive transmission modes. The relative significance between contact, droplet, and airborne transmission is yet to be defined, a knowledge gap for implementing evidence-based infection control measures. We devised a transmission chamber that separates virus-laden particles by size and determined the particle sizes mediating transmission of influenza among ferrets through the air. Ferret-to-ferret transmission was mediated by airborne particles larger than 1.5 µm, consistent with the quantity and size of virus-laden particles released by the donors. Onward transmission by donors was most efficient before fever onset and may continue for 5 days after inoculation. Multiple virus gene segments enhanced the transmissibility of a swine influenza virus among ferrets by increasing the release of virus-laden particles into the air. We provide direct experimental evidence of influenza transmission via droplets and fine droplet nuclei, albeit at different efficiency.
Influenza epidemics and pandemics are characterized by abrupt increases in cases reported concurrently at different geographic regions as a result of its rapid global spread, resulting in 250,000–500,000 deaths during epidemics and 0.2–50 million deaths during pandemics (1–3). Influenza can potentially be transmitted from person to person by three modes: contact transmission, in which infectious secretions are transferred directly or indirectly via fomites; droplet transmission, in which respiratory fluid-containing particles larger than 5 µm travel ballistically through the air and deposit onto mucous membranes within 3 ft as a result of gravity; and airborne transmission, in which dried particles (i.e., droplet nuclei) smaller than 5 µm remain suspended in air and disperse over long distances and are inhaled and deposited in the respiratory tract. Although influenza is thought to be transmitted via these non-mutually exclusive modes, the relative importance of each is unclear. It is especially challenging to delineate the relative significance of droplets vs. fine droplet nuclei in mediating influenza transmission in epidemiological studies, as the exposure history often cannot be clearly determined (4–6). Precautions against droplet transmission include face masks and eye protection during close contact with a patient, whereas airborne precautions include single-patient negative pressure rooms and respiratory protection such as the use of an N95 respirator (7). Recommendation on influenza infection control measures in health care and community settings are formulated despite major knowledge gaps in the relative significance of the different transmission modes.
Ferrets are naturally susceptible to influenza infection (8) and support influenza transmission via direct contact (i.e., with cohoused donors and recipients) or by respiratory droplets (i.e., with donors and recipients housed in cages separated by varying distances) under the experimental setting of continuous exposure (9, 10). As influenza viruses with sustained human-to-human transmissibility (e.g., human seasonal or pandemic influenza viruses) are transmissible among ferrets via respiratory droplets, ferrets are often used to assess the pandemic risk of zoonotic influenza viruses (11). However, the conventional experimental settings cannot clarify the relative transmission efficiency of airborne particles of different sizes that mediate droplet and airborne transmission. To address this knowledge gap, we developed a transmission chamber capable of separating influenza virus-laden particles into specific size ranges by the application of impactors. We report an experimental study that delineated the size of airborne particles mediating influenza transmission among ferrets.
Results
Airborne Transmission of Influenza Among Ferrets Was Mediated by Virus-Laden Particles Larger than 1.5 µm.
A transmission chamber capable of separating airborne particles into specific size ranges by the application of impactors was constructed. Our system captures particles larger than the desired cutoff size via inertial impaction while allowing smaller particles to remain in the air stream. The donor chamber is connected to the recipient chamber with an impactor (Fig. S1A) inside a class II biosafety cabinet (BSC; Fig. S1B). Impactors with 50% collection efficiencies (d50) of 9.9 µm, 5.3 µm, 2.5 µm, and 1.0 µm (12) were applied in separate experiments. Based on the collection efficiency curves, these impactors remove ≥95% of airborne particles with diameters ≥15.3 µm, ≥7.9 µm, ≥4.7 µm, and ≥1.5 µm (d95), respectively, from the air flowing from the donor chamber into the recipient chamber during the exposure period.
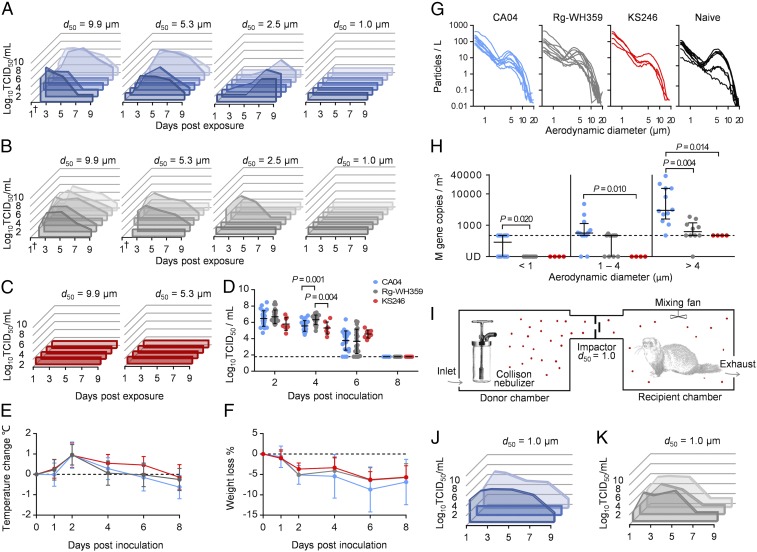
We first evaluated the transmission efficiency of A(H1N1)pdm09 (A/California/04/09; CA04) and recombinant human seasonal A(H3N2) (Rg-A/Wuhan/359/95; Rg-WH359) influenza viruses that have been shown to transmit efficiently among ferrets via “direct contact” and “respiratory droplets” under conventional experimental settings (13). Ferret-to-ferret transmission of the CA04 virus was efficiently mediated by particles that passed through the 9.9-µm, 5.3-µm, and 2.5-µm impactors with viral shedding detected in 4 of 6 (5 of 6 seroconverted), 4 of 6, and 3 of 6 recipient ferrets, respectively (Fig. 1A). Interestingly, none of the recipient ferrets (0 of 6) exposed to particles that passed through the 1.0-µm impactor shed virus or showed seroconversion. Among ferrets that were exposed to the particles passing through the 2.5-µm impactor, there was delayed virus shedding in nasal washes, but no changes in clinical signs were observed compared with those exposed with the 9.9-µm impactor (Dunn’s multiple comparisons test, P = 0.022). Similarly, transmission of Rg-WH359 virus was detected in 5 of 6, 2 of 6, 1 of 6, and 0 of 6 recipient ferrets after exposure to particles passing through the 9.9-µm, 5.3-µm, 2.5-µm, and 1.0-µm impactors, respectively (Fig. 1B). All Rg-WH359–infected recipient ferrets showed comparable virus-shedding patterns regardless of the impactor applied. These data demonstrated that efficient airborne transmission of human influenza viruses among ferrets was mediated by airborne particles ≥1.5 µm that could not pass through the 1.0-µm impactor.
Fig. 1.
Ferret-to-ferret transmissibility is associated with the quantity and size of virus-laden particles in air released by the donor ferrets. Transmission of (A) CA04, (B) Rg-WH359, and (C) KS246 among ferrets via virus-laden particles that passed through the impactors with 50% collection efficiency at 9.9 µm, 5.3 µm, 2.5 µm, or 1 µm. Viral titers (log10TCID50/mL) detected in the nasal washes from recipient ferrets (detection limit at 1.789 log10TCID50/mL). For each impactor, the experiments were independently repeated three times for CA04 and Rg-WH359 (recipient, n = 6) and twice for KS246 (recipient, n = 4). (D) Viral titers detected in donor nasal washes after inoculation with CA04 (n = 24), Rg-WH359 (n = 24), or KS246 (n = 8) influenza viruses and overlaid with mean ± SD. (E) Temperature and (F) weight changes of donor ferrets after inoculation with CA04 (n = 22–24), Rg-WH359 (n = 20–24), or KS246 (n = 8) viruses and overlaid with mean ± SD. (G) APS was applied to determine size distribution (range, 0.52–20.53 µm) of total particles released in air by donor ferrets (n = 9, n = 10, and n = 4 for CA04, Rg-WH359, and KS246, respectively) at 2 dpi or by noninoculated ferrets (n = 9). (H) Quantity and size distribution of influenza virus-laden particles sampled from the donor chambers during the exposure period using the NIOSH bioaerosol sampler. The limit of linear range of quantification (476 M gene copies per cubic millimeter) is shown with the dotted line. Data from each exposure (n = 12, n = 10, and n = 4 for CA04, Rg-WH359, and KS246, respectively) are shown and overlaid with median and interquartile range. (I) Schematic representation of the transmission experiment with artificially generated aerosols. (J) Viral titers (log10TCID50/mL) detected in the nasal washes of recipients ferrets after exposure to nebulized CA04 aerosols that passed through the 1.0-µm impactor; the experiments were independently repeated three times. (K) Viral titers (log10TCID50/mL) detected in the nasal washes of recipients ferrets after exposing to nebulized Rg-WH359 aerosols that passed through the 1.0-µm impactor; the experiments were independently repeated three times. P values <0.05 from Dunn’s multiple comparisons after Kruskal–Wallis test are shown.
For comparison, an A(H1N2) triple-reassortant swine influenza virus (A/Sw/Kansas/00246/04; KS246) that showed inefficient direct contact transmission (1 of 2) and delayed “respiratory droplet” transmission (1 of 2) under conventional experimental settings was studied. No ferret-to-ferret transmission was observed with particles that passed through the 9.9-µm or 5.3-µm impactors (Fig. 1C).
The data from the experiments were fitted to the Wells–Riley model to determine the exhaled airborne infectious units (i.e., quanta) at different particle size ranges by the donor ferrets (Table 1) (14, 15). Based on the estimated infection risk, smaller particles that may pass through the 5.3-µm impactor play a more important role in mediating ferret-to-ferret transmission of the A(H1N1)pdm09 (CA04) virus compared with the seasonal A(H3N2) (Rg-WH359) virus.
Table 1.
Quanta generation rates at different particle size range from CA04 and Rg-WH359 inoculated donor ferrets
| Virus | Impactor | Infected/exposed ferrets | Infection risk, % (95% CI) | Quanta per hour (95% CI) | |
| d50, µm | d95, µm* | ||||
| CA04 | 9.9 | 15.3 | 5/6 | 83.33 (35.88–99.58) | 7.95 (1.97–24.49) |
| 5.3 | 7.9 | 4/6 | 66.67 (22.28–95.67) | 4.87 (1.12–13.93) | |
| 2.5 | 4.7 | 3/6 | 50.00 (11.81–88.19) | 3.07 (0.56–9.48) | |
| 1.0 | 1.5 | 0/6 | 0.00 (0.00–45.93) | 0.00 (0.00–2.73) | |
| Rg-WH359 | 9.9 | 15.3 | 5/6 | 83.33 (35.88–99.58) | 7.95 (1.97–24.49) |
| 5.3 | 7.9 | 2/6 | 33.33 (4.33–77.72) | 1.80 (0.19–6.66) | |
| 2.5 | 4.7 | 1/6 | 16.67 (0.42–64.12) | 0.81 (0.02–4.54) | |
| 1.0 | 1.5 | 0/6 | 0.00 (0.00–45.93) | 0.00 (0.00–2.73) | |
The transmission experiment results were fitted to the Well–Riley model to determine the exhaled airborne infectious units (quanta) at different particle size range by the donor ferrets.
Particles smaller than the cutoff size would be able to pass into the recipient chamber.
Limited Amounts of Virus-Laden Particles at Submicron Size Were Exhaled by Influenza-Inoculated Donor Ferrets.
To determine the mechanism leading to differential airborne transmissibility of the human and swine influenza viruses among ferrets, the viral replication kinetics in the ferret upper respiratory tract were compared. In nasal washes, KS246 swine influenza virus showed delayed replication efficiency compared with CA04 and Rg-WH359 human influenza viruses, with lower titers detected at 2 d (Kruskal–Wallis test, P = 0.075) and 4 d (Kruskal–Wallis test, P < 0.0001) after inoculation (Fig. 1D). However, the total amount of virus shed in the nasal wash as calculated by the area under the curve (AUC) values were comparable between CA04-, Rg-WH359–, or KS246-inoculated donor ferrets (Kruskal–Wallis test, P = 0.367). Donor ferrets inoculated with CA04, Rg-WH359, or KS246 viruses showed comparable temperature (Fig. 1E) and weight changes after inoculation (Fig. 1F), suggesting that the virulence of influenza viruses may be dissociated from transmissibility.
The size distribution of total particles released from influenza-infected donors was analyzed by an aerodynamic particle sizer (APS) at 2 d postinoculation (dpi). Approximately 76.8% of the particles were fine droplet nuclei with aerodynamic diameters of 0.52–1.54 µm, 16.8% were >1.54–4.87 µm, and only 6.4% were >4.87–20.53 µm (Fig. 1G). No significant difference in overall particle size distribution was noted between naïve ferrets and ferrets inoculated with CA04, Rg-WH359, or KS246, except that fewer particles at >4.87–20.53 µm were detected from the CA04-inoculated ferrets than from naïve ferrets (Dunn’s multiple-comparisons test, P = 0.039). We further determined the size and quantity of influenza virus-laden particles released into the air by donors during exposure by using the National Institute for Occupational Safety and Health (NIOSH) bioaerosol sampler that collects particles into three size ranges (>4 µm, 1–4 µm, and <1 µm) (16) followed by quantitative real-time RT-PCR to detect influenza viral RNA segment 7 (matrix gene). Higher quantities of virus-laden particles at particle sizes >4 µm were detected in air sampled from the donor chambers from ferrets inoculated with CA04 (Dunn’s multiple-comparisons test, P = 0.014) or Rg-WH359 (P = 0.655) than from those inoculated with KS246 virus (Fig. 1H), suggesting that efficient ferret-to-ferret transmissions via the airborne route is directly associated with the quantity of virus-laden particles in air released by the donor ferrets during the exposure period. These results demonstrate the significance of the increased quantity of virus laden-particles (17) rather than total airborne particles in mediating influenza transmission through air.
Artificially Generated Droplet Nuclei Smaller than 1.5 µm Efficiently Mediate Airborne Transmission of Influenza Virus.
No ferret-to-ferret transmission was observed with the 1.0-µm impactor (Fig. 1 A and B), which permitted particles <1.5 µm (d95) to pass from the donor chamber to the recipient chamber during exposure. This is consistent with the limited quantities of virus-laden particles detected from the donor chamber in this size range (Fig. 1H). To test the airborne transmission potential of particles <1.5 µm, a Collison nebulizer was applied to generate aerosols of CA04 and Rg-WH359 viruses inside the donor chamber; three naïve ferrets were independently exposed for 1 h to aerosols that passed through the 1.0-µm impactor (Fig. 1I). Two of three ferrets exposed to aerosolized CA04 virus shed virus in the nasal washes, and all three ferrets showed seroconversion at 12 d postexposure (Fig. 1J); all three ferrets exposed to aerosolized Rg-WH359 virus shed virus in the nasal washes (Fig. 1K). Overall, our results support the feasibility of airborne transmission via fine droplet nuclei less than 1.5 μm if viable viruses are successfully released into fine droplet nuclei. The size and quantity of aerosols released in air from different sources under hospital settings (e.g., influenza-infected patients with or without aerosol-generating procedures) may influence the modes of onward transmission.
Transmission Among Ferrets Through the Air Was Most Efficient Before Fever Onset of the Inoculated Donors and May Continue for at Least Five Days.
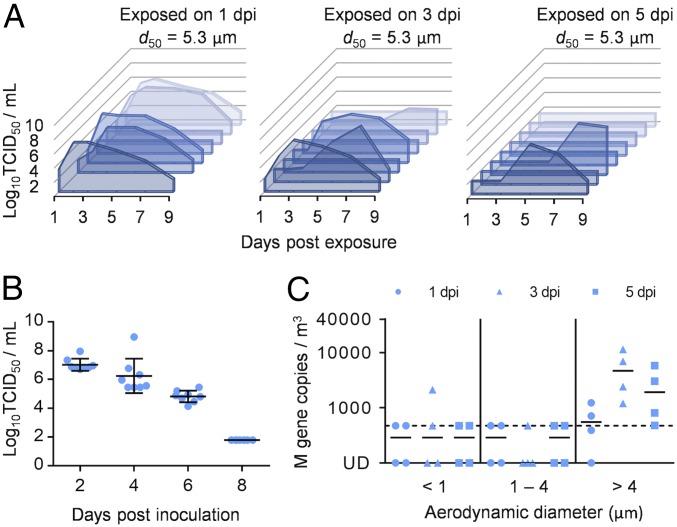
Donor ferrets inoculated with CA04 or Rg-WH359 viruses had no apparent clinical signs at 1 dpi (e.g., without fever or significant weight loss; Fig. 1 E and F) but released virus-laden particles that infected recipient ferrets. To further assess the potential communicable period by the CA04-inoculated donor ferrets, groups of two naïve ferrets were independently exposed to donors for 8 h on 1, 3, and 5 dpi by using the 5.3-µm impactor. Transmission through the air was detected in 5 of 7 (7 of 7 seroconverted), 4 of 8, and 2 of 8 recipient ferrets exposed at 1 dpi, 3 dpi, and 5 dpi, respectively (Fig. 2A), with delayed viral shedding noted in those exposed at 5 dpi compared with those exposed at 1 dpi (Dunn’s multiple comparisons test, P = 0.048; Fig. 2A). Infectious viral titers detected from donor nasal washes gradually decreased over time (Fig. 2B). The size distributions of total particles released from donors at 2, 4, and 6 dpi were comparable (Fig. S2). However, the quantity of virus-laden particles detected in the air from the donor chamber were higher at 3 and 5 dpi than at 1 dpi (Kruskal–Wallis test, P = 0.077), and virus was predominantly detected in particles >4 µm (Fig. 2C). Thus, despite continuous detection of virus-laden particles in air, the results suggest gradually decreased infectivity of virus-laden particles released from inoculated donors during the course of the infection, possibly as a result of host factors elicited after infection.
Fig. 2.
Airborne transmissibility of CA04-inoculated ferrets gradually decreases over time and may last at least 5 d. (A) Viral titers (log10TCID50/mL) detected from the nasal washes of recipient ferrets after exposure for 8 h to CA04-inoculated donors at 1 dpi (n = 7), 3 dpi (n = 8), or 5 dpi (n = 8). The 5.3-µm impactor was applied to all experiments. Exposure at each dpi was independently repeated four times, and data were plotted for individual recipient ferrets. (B) Viral titers detected from the nasal washes of donor ferrets. Data were plotted for individual ferrets (n = 8) and overlaid with mean ± SD. (C) Quantity and size distribution of virus-laden particles sampled from the donor chambers at 1, 3, and 5 dpi during exposure. Data were plotted for each exposure event (n = 4) at each time point and overlaid with median.
Multiple Viral Gene Segments Enhanced the Transmissibility of a Swine-Origin H1N2 Influenza Virus Among Ferrets by Increasing the Release of Virus-Laden Particles into the Air.
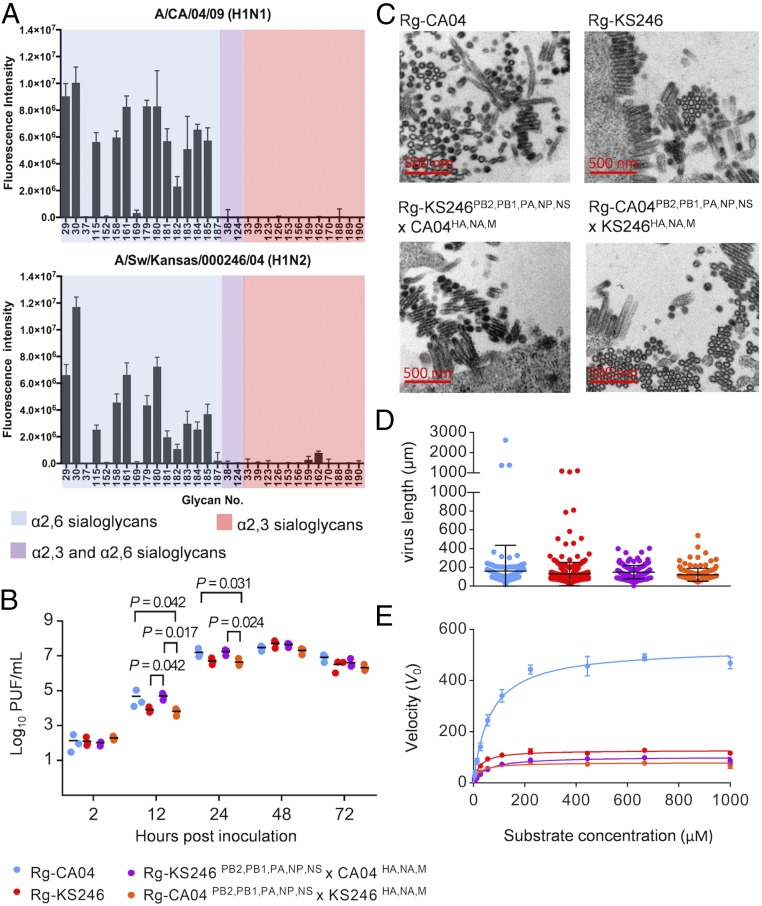
The A(H1N1)pdm09 virus that spread globally in 2009 emerged through genetic reassortment between two lineages of swine influenza viruses (triple-reassortant lineage and Eurasian lineage) that lacked sustained transmissibility among humans and respiratory droplet transmissibility in ferrets (13, 18, 19). The hemagglutinin (HA), neuraminidase (NA), and matrix (M) gene segments have been reported to confer increased transmission potential for the A(H1N1)pdm09 virus (13, 19–23). We further investigated viral factors that differentiated the transmission potential between the triple-reassortant swine influenza virus (KS246) and the A(H1N1)pdm09 virus (CA04) among ferrets. Applying glycan array analysis, we observed that the CA04 and KS246 viruses preferably bind to α2,6-sialoglycans, although differences in binding intensity were noted (Fig. 3A and Fig. S3). In differentiated human airway epithelial (HAE) cells, lower titers were noted for Rg-KS246 and Rg-KS246PB2,PB1,PA,NP,NS×CA04HA,NA,M viruses at 12 and 24 h postinoculation (Fig. 3B). Under transmission electron microscopes, the four recombinant viruses formed predominantly short and few long filamentous (>1 µm) virions (Fig. 3C) that were not significantly different based on virion length (P = 0.076, one-way ANOVA; Fig. 3D). Rg-CA04 showed significantly higher NA enzymatic activity than the other three recombinant viruses when using 2′-(4-methylumbelliferryl)-α-d-N-acetylneuraminic acid (MUNANA) as substrate (Fig. 3E). The N1 proteins of Rg-CA04 and Rg-KS246PB2,PB1,PA,NP,NS×CA04HA,NA,M viruses possessed higher Km (95% CI, 55.4–73.4 μM and 40.9–59.3 μM, respectively) than that of the N2 protein of Rg-KS246 and Rg-CA04PB2,PB1,PA,NP,NS×KS246HA,NA,M viruses (95% CI, 20.1–27.7 μM and 17.8–27.0 μM, respectively).
Fig. 3.
Characterization of CA04 and KS246 recombinant viruses in vitro. (A) Glycan array analysis of CA04 and KS246 viruses. CA04 and KS246 viruses were inactivated by 0.025% formaldehyde and diluted to 16 HA titers (0.5% turkey red blood cells) for analysis. The fluorescence signal was acquired by using the NimbleGen MS 200 Microarray Scanner. The experiment was repeated independently twice with six replicates at each repeat. (B) Replication kinetics of recombinant Rg-CA04, Rg-KS246, Rg-KS246PB2,PB1,PA,NP,NS×CA04HA,NA,M, and Rg-CA04PB2,PB1,PA,NP,NS×KS246HA,NA,M in differentiated HAE cells. The viral replication efficiencies in HAE cells at a multiplicity of infection (MOI) of 0.01 PFU/cell were determined (mean ± SD of three replicates shown). P values <0.05 from Dunn’s multiple comparisons after Kruskal–Wallis test are shown. (C) Representative images of virion morphology under a transmission electron microscope (8,900×) after 14 h propagation in MDCK cells at an MOI of 2 PFU/cell. (D) Comparison of virion length of recombinant viruses of different gene constellations. One hundred virions were randomly selected from images taken from transmission EM to determine the virion length (one-way ANOVA, P = 0.0761). (E) NA enzyme kinetics using the fluorogenic substrate MUNANA. The viruses were diluted to 106 PFU/mL, and the kinetic data were fit to the Michaelis–Menten equation by nonlinear regression to determine Km and Vmax of substrate conversion. The experiment was repeated independently twice, and mean ± SD is shown.
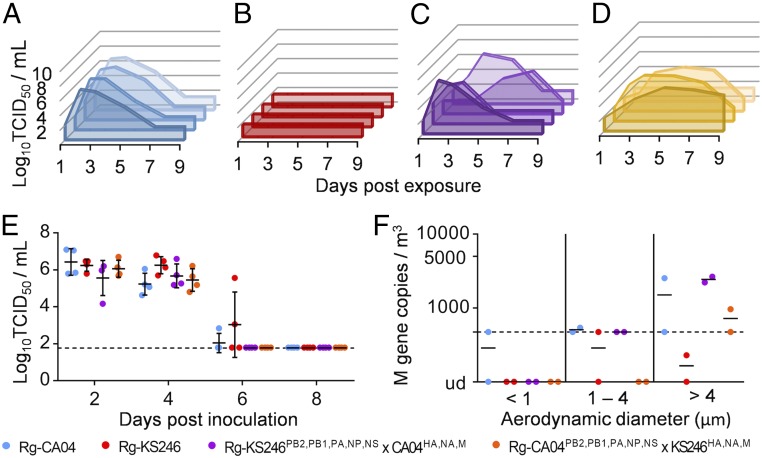
Airborne transmissibility was assessed by exposing naïve ferrets to donors at 1 dpi by using the 5.3-µm impactor. The Rg-CA04 (Fig. 4A) and Rg-KS246 (Fig. 4B) viruses showed comparable transmission potential as the parental CA04 (Fig. 1A) and KS246 (Fig. 1C) viruses and were transmitted to 4 of 4 and 0 of 4 recipient ferrets, respectively. Introducing the HA, NA, and M gene segments of the CA04 virus into swine influenza KS246 increased the airborne transmission potential, with the Rg-KS246PB2,PB1,PA,NP,NS×CA04HA,NA,M virus being transmitted to 4 of 4 recipients (Fig. 4C). Replacing the HA, NA, and M gene segments of CA04 with that of the KS246 virus reduced the transmissibility of the Rg-CA04PB2,PB1,PA,NP,NS×KS246HA,NA,M virus to 3 of 4 (4 of 4 seroconverted) but did not completely eliminate airborne transmission (Fig. 4D), suggesting that the five remaining gene segments of CA04 contain determinants that facilitate airborne transmission. Although all four recombinant viruses replicated to comparable titers in the donor nasal washes (Fig. 4E), more virus-laden particles, predominantly at particle size >4 µm, were detected in air sampled from the donor chambers during the exposure of Rg-CA04, Rg-KS246PB2,PB1,PA,NP,NS×CA04HA,NA,M, and Rg-CA04PB2,PB1,PA,NP,NS×KS246HA,NA,M viruses (Kruskal–Wallis test, P = 0.148; Fig. 4F). These data suggest that A(H1N1)pdm09 virus possesses multiple viral factors that contribute to its increased airborne transmissibility in ferrets by increasing the release of virus-laden particles in air.
Fig. 4.
Multiple viral gene segments from CA04 confer enhanced transmissibility of KS246 by increasing the release of virus-laden particles into the air. Transmission of (A) Rg-CA04, (B) Rg-KS246, (C) Rg-KS246PB2,PB1,PA,NP,NS×CA04HA,NA,M, and (D) Rg-CA04PB2,PB1,PA,NP,NS×KS246HA,NA,M recombinant viruses among ferrets via virus-laden particles that passed through the 5.3-µm impactor. Viral titers (log10TCID50/mL, detection limit at 1.789 log10TCID50/mL) detected in the nasal washes of each recipient ferret. For each recombinant virus, the experiments were independently repeated twice with a total of four recipients. (E) Viral titers detected in the nasal washes of donor ferrets inoculated with 105 TCID50 of the recombinant viruses. Data were plotted for individual donor ferrets (n = 4) and overlaid with mean ± SD. (F) Quantity and size distribution of influenza virus-laden particles sampled from the donor chambers during the exposure period by using the NIOSH bioaerosol sampler. The limit of linear range of quantification (476 M gene copies per cubic meter) is shown. Data were plotted for two independent exposures and overlaid with medians.
Discussion
The relative significance of the multiple non-mutually exclusive modes mediating influenza transmission remains a knowledge gap despite many well-designed animal transmission models carried out to date. Specifically, the conventional experimental design that houses donors and recipients in cages separated by varying distances cannot clarify the contributions of large droplets and fine droplet nuclei to transmission. These two modes of transmission have markedly different spatial-temporal constraints during transmission. With the application of a transmission chamber, we experimentally characterized the transmissibility of influenza virus-laden particles by size, naturally exhaled from influenza-inoculated animals into the air. Our results show that transmissions between ferrets were mediated by large and fine virus laden-particles ≥1.5 µm. The application of a series of impactors with different cutoff sizes also allowed us to estimate the infection risk of the A(H1N1)pdm09 and the seasonal A(H3N2) viruses. Our system assessed transmissibility of particles <15.3 μm (d95) when the 9.9-μm impactor was used. We note that smaller particles may play a more important role in mediating ferret-to-ferret transmission of the A(H1N1)pdm09 virus than the seasonal A(H3N2) virus, suggesting that there are important strain-to-strain variations in modes of transmission. Overall, the results provided experimental evidence to support influenza transmission among ferrets via droplets (15.3–5 μm) as well as fine droplet nuclei (5–1.5 μm).
Influenza transmission dynamics, including the minimal contact duration and the period of communicability, are largely unknown. We showed that airborne transmission of influenza virus among ferrets was most efficient before onset of fever in the donors and progressively decreased from 1 to 5 dpi over the course of the infection when the exposure period was kept constant (8 h; Fig. 2A). Interestingly, we continue to detect influenza virus RNA in air sampled from the donor chamber during the 8-h exposure period at 1, 3, or 5 dpi despite the gradually decreased infectivity of virus-laden particles (Fig. 2C). A gradually decreased transmissibility among ferrets has been also been observed by Koster et al. (24) and Roberts et al. (25). However, the fact that virus-laden particles continue to be shed in air despite decreasing infectivity was not reported previously. Restrictive host factors elicited after infection may be coreleased with virus-laden particles in air that directly reduced the infectivity of the virus-laden particles or may indirectly induce the innate defense of the naïve ferrets. Future studies should apply proteomic analysis to investigate potential host factors released from the exhale breath after influenza infection.
The quantity of virus-laden particles released by the donors was directly associated with the airborne transmission potential of the A(H1N1)pdm09 virus (CA04) and the genetically related swine influenza virus (KS246), which is consistent with results reported previously (17, 19). We observed that multiple viral gene constellations may increase the quantity of virus-laden particles released from infected ferrets that facilitated airborne transmissibility. In addition to the role of HA, NA, and M gene segments proposed by us and others (13, 19–23), we also observed that replacing the HA, NA, and M genes of the transmissible CA04 virus with those from the nontransmissible KS246 did not completely abolish the transmission potential, suggesting that additional enhancement factors for airborne transmission are present in these remaining five gene segments. The importance of PB2 residues 627 and 701 in conferring influenza transmission through the air has been shown previously (26, 27). The PB2 proteins of A(H1N1)pdm09 virus CA04 and the TRIG-like swine influenza virus KS246 share the same evolutionary origin (28), including the adaptive SR polymorphism at positions 590/591 that may partially compensate the functionality of K627 and increase polymerase activity in mammalian cells (29). The result highlights the plasticity of segmented RNA viruses in achieving enhanced transmission phenotype through genetic reassortment compared with sequential adaptation.
Approximately 76.8% of total airborne particles released from the donor ferrets were fine droplet nuclei with aerodynamic diameters of 0.52–1.54 µm; however, virus-laden particles were predominantly enriched in particles >4 µm. As a twofold increase in the aerodynamic diameter would lead to an approximately eightfold increase in mass, it is possible that larger particles may contain more virions than do the fine droplet nuclei. Previous studies proposed that fine particles in exhaled breath are formed during the opening of collapsed small airways and alveoli (30, 31). However, the anatomic sites of viral replication in the airway from which these virus-laden particles arise for onward transmission require further investigation. As with ferrets, greater numbers of fine particles are released compared with larger particles in the exhaled breath from healthy or influenza-infected human subjects (32–34). Furthermore, influenza virus-laden particles of different size ranges have been detected from human patients during breathing or coughing (35–39). Milton et al. (38) detected viral RNA from fine (≤5 μm) and coarse (>5 μm) particles released from influenza-infected human subjects during 30 min of normal breathing with coughs; viable virus was detected from 2 of 37 patients from the fine fraction particles, although isolation was not attempted for the coarse particles. Gralton et al. (35) reported detection of viral RNA by using cascade impactors from patients with influenza-like or cold-like illness; influenza and RSV viruses were detected predominantly at particles >4.7 μm, whereas rhinovirus and parainfluenza viruses were detected from multiple particle size ranges >0.65 μm. Lednicky and Loeb (39) detected viral RNA and viable virus from particles >2.5 μm and from particles at <1.0 μm by using a personal cascade impactor placed at different locations inside the apartment where two patients with influenza resided. Among 32 patients with influenza with viral RNA detected from their coughs, viral RNA was detected by the NIOSH bioaerosol sampler from 90%, 81%, and 75% of patients in >4-μm, 1–4-μm, and <1-μm size fractions, respectively; viable virus was detected from the >4-μm fraction from only one subject (36). A follow-up study using a combination of a spirometer and an SKC BioSampler detected viable influenza virus from the coughs of symptomatic patients at the particle size fraction of 0.3–8 μm (37). Although these studies reported the size ranges of virus-laden particles that were detected in the air exhaled by influenza-infected individuals, the relative significance of droplets and fine droplet nuclei in mediating influenza transmissions among humans is still not fully elucidated. Our results from ferrets may not be directly extrapolated to infer the modes of influenza transmission among humans. However, our results suggest the feasibility of adopting a similar experimental setting to directly assess transmissibility of virus-laden particles released by influenza-infected human subjects to naïve ferrets. Results from such studies may provide evidence-based guidance for developing interventions to reduce transmission of influenza viruses during epidemics and pandemics. Such a design could be further applied to assess the relative significance between droplet and airborne transmission of other respiratory pathogens.
Materials and Methods
Design and Validation of the Exposure Chamber.
The donor and recipient chambers were made of stainless steel with a front opening and exterior dimensions of 55 cm × 36 cm × 38 cm (length × depth × height). The two chambers were connected via an impactor with a d50 of 9.9 µm, 5.3 µm, 2.5 µm, or 1.0 µm (12) by using two custom-made connectors sealed by duct tape during operation to prevent air leakage. Stainless-steel wire cages 45 cm × 36 cm × 30 cm (length × depth × height) in size were placed inside the chambers to hold the ferrets during the exposure period. The donor and recipient chambers were tightly closed by a stainless-steel door with eight clamps; a glass window (30.2 cm × 21.1 cm) on the door allowed observation of ferret activity during the experiments. To ensure the chambers were airtight, foam weather-strip tape was applied between the chamber and the door and extra sealing with duct tape was applied during the experiments. A mixing fan that runs with an average velocity of 0.4 m/s was installed at the top of the recipient chamber to counteract the rising thermal plume of the ferrets and to ensure that the virus-laden particles entering from the source chamber were well mixed inside the recipient chamber. The air inlet was located at the bottom of the side wall of the donor chamber. A vacuum pump (cat. no. 228–9605B; SKC) was connected at the exhaust air outlet located at the bottom of the side wall of the recipient chamber to create a unidirectional flow by drawing air from the donor chamber into the recipient chamber. A HEPA filter was installed before the vacuum pump to remove infectious particles. The entire exposure chamber was placed inside a class II BSC.
Maintenance of stable airflow is prerequisite for the impactor function. For each run of the experiment, the recipient chamber tightness was evaluated by checking the airflow rate by using a mass flowmeter (model 4043; TSI) before the impactor continuously for 10 min and for another 10 min between the outlet and the vacuum pump. Using the 1.0 µm impactor, the measured results were 30.02 ± 0.05 L/min (mean ± SD) for the former and 30.12 ± 0.02 L/min for the latter, with a difference of <0.4% of the total flow rate. The difference was even smaller when the 5.3-µm and 9.9-µm impactors were applied, as the pressure decreases are much smaller than that of the 1.0-µm impactor. To assess the effect of ferret movement and breathing inside the recipient chamber on airflow stability, the flow rate at the inlet of the 1-µm impactor was measured for 30 min with two naïve ferrets inside the recipient chamber. The measured flow rates were within the range of 29.76–30.40 L/min (mean ± SD at 30.14 ± 0.10 L/min), with a maximum fluctuation range of 0.64 L/min during the 30-min measurement. When the 5.3-µm impactor and the 9.9-µm impactor were used, the fluctuation ranges were 0.17 L/min and 0.11 L/min, respectively. Overall, the results showed little change in airflow regardless of the impactors used for the experiments.
Transmission Experiments.
All animal experiments were approved by the Committee on the Use of Live Animals in Teaching and Research at the University of Hong Kong (2925-12 and 3352–14) and received animal ethics approval from the Chinese University of Hong Kong (13-110-MIS), following the Code of Practice for care and use of animals for experimental purposes established by the Animal Welfare Advisory Group, approved by the Government of the Hong Kong. Desexed male ferrets were obtained from Wuxi Sangosho Biotechnology at 4–8 mo old and weighed 1.0–2.0 kg. Ferrets were confirmed to be seronegative for influenza A virus NP protein by competitive ELISA (ID.vet) and with hemagglutination inhibition (HI) titer ≤10 to seasonal influenza A viruses A/California/07/2009 (H1N1), A/Perth/16/2009 (H3N2), and A/Switzerland/9715293/2013 (H3N2). Sample sizes were determined on the basis of statistical considerations for identifying differences in the transmissibility (40).
Animal experiments were conducted at the Laboratory Animal Service Center at the Chinese University of Hong Kong. For each experiment, two donor ferrets were anesthetized by ketamine and xylazine and were inoculated intranasally with 105 of the 50% tissue culture infectious dose (TCID50) of influenza viruses in 0.5 mL media. Donors were housed inside individually ventilated ferret cages (IVC) after inoculation. Naïve ferrets were exposed to inoculated contacts on specified dpi. Two naïve ferrets were handled first and were placed into the recipient chamber with ad libitum water supply. The recipient chamber was fully sealed and had the stability of airflow checked. The donor chamber was then connected to the impactor, and two donor ferrets were introduced into the donor chamber. The whole exposure chamber was set up inside a 6-ft class II BSC (Thermo Fisher) with 1% Virkon S solution used as a disinfectant to decontaminate all tools and surfaces inside the BSC. To test the transmission potential of artificially generated aerosols that pass through the 1-µm impactor, a one-jet Collison nebulizer was used to generate virus-laden particles inside the donor chamber at 2.5 L/min for 30 min by using CA04 virus resuspended in minimum essential medium (MEM) at 106 plaque-forming units (PFU)/mL. One naïve ferret was exposed for 1 h at 24 air changes per hour. After exposure, each animal was individually housed inside IVCs. All ferrets were monitored for clinical signs daily, and nasal washes were collected every other day. Each animal was handled by using separate tools, with frequent Virkon decontamination in between procedures.
Transmission was defined as detection of virus shedding in nasal washes or by seroconversion of sera collected on 15 dpi (14 d postexposure) by HI assay. A negative control experiment was performed with a HEPA filter installed (replacing the impactor) in between the donor and recipient cages; after 8 h exposure to CA04-inoculated donors, no transmission to recipient ferrets (0 of 2) was detected. The relative humidity and temperature in the animal facility during the 24-mo test period were 57.3 ± 5.5% and 24.2 ± 0.9 °C (mean ± SD), respectively.
Supplementary Material
Acknowledgments
We thank G. M. Leung, D. K. Milton, S. T. Ferguson, M. Wolfson, and P. C. L. Kwok for helpful discussions, V. J. Fang for statistical support, W. K. Leung for assistance in constructing the transmission chamber, and H. S. Chan and S. F. Chan for assistance in animal husbandry. This work was supported by National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services under contract HHSN272201400006C;, General Research Fund 784313; and Theme-based Research Scheme project no. T11-705/14N from the Hong Kong Government and AXA Research Fund. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health and the Centers for Disease Control and Prevention.
Footnotes
Conflict of interest statement: B.J.C. received research funding from Sanofi. The other authors declare no conflict of interests.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1716771115/-/DCSupplemental.
References
- 1.Dawood FS, et al. Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: A modelling study. Lancet Infect Dis. 2012;12:687–695. doi: 10.1016/S1473-3099(12)70121-4. [DOI] [PubMed] [Google Scholar]
- 2.WHO 2018 Influenza (Seasonal). Available at www.who.int/mediacentre/factsheets/fs211/en. Accessed January 16, 2018.
- 3.Johnson NP, Mueller J. Updating the accounts: Global mortality of the 1918-1920 “Spanish” influenza pandemic. Bull Hist Med. 2002;76:105–115. doi: 10.1353/bhm.2002.0022. [DOI] [PubMed] [Google Scholar]
- 4.Brankston G, Gitterman L, Hirji Z, Lemieux C, Gardam M. Transmission of influenza A in human beings. Lancet Infect Dis. 2007;7:257–265. doi: 10.1016/S1473-3099(07)70029-4. [DOI] [PubMed] [Google Scholar]
- 5.Tellier R. Aerosol transmission of influenza A virus: A review of new studies. J R Soc Interface. 2009;6(6 suppl 6):S783–S790. doi: 10.1098/rsif.2009.0302.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tellier R. Review of aerosol transmission of influenza A virus. Emerg Infect Dis. 2006;12:1657–1662. doi: 10.3201/eid1211.060426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siegel JD, Rhinehart E, Jackson M, Chiarello L. Health Care Infection Control Practices Advisory Committee 2007 guideline for isolation precautions: Preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35(10 suppl 2):S65–S164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith W, Andrewes CH, Laidlaw PP. A virus obtained from influenza patients. Lancet. 1933;222:66–68. [Google Scholar]
- 9.Belser JA, Eckert AM, Tumpey TM, Maines TR. Complexities in ferret influenza virus pathogenesis and transmission models. Microbiol Mol Biol Rev. 2016;80:733–744. doi: 10.1128/MMBR.00022-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andrewes CH, Glover RE. Spread of infection from the respiratory tract of the ferret. I. Transmission of influenza A virus. Br J Exp Pathol. 1941;22:91–97. [Google Scholar]
- 11.Buhnerkempe MG, et al. Mapping influenza transmission in the ferret model to transmission in humans. eLife. 2015;4:e07969. doi: 10.7554/eLife.07969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Demokritou P, Lee SJ, Ferguson ST, Koutrakis P. A compact multistage (cascade) impactor for the characterization of atmospheric’ aerosols. J Aerosol Sci. 2004;35:281–299. [Google Scholar]
- 13.Yen HL, et al. Hemagglutinin-neuraminidase balance confers respiratory-droplet transmissibility of the pandemic H1N1 influenza virus in ferrets. Proc Natl Acad Sci USA. 2011;108:14264–14269. doi: 10.1073/pnas.1111000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riley EC, Murphy G, Riley RL. Airborne spread of measles in a suburban elementary school. Am J Epidemiol. 1978;107:421–432. doi: 10.1093/oxfordjournals.aje.a112560. [DOI] [PubMed] [Google Scholar]
- 15.Wells WF. Airborne Contagion and Air Hygiene. Harvard Univ Press; Cambridge, MA: 1955. [Google Scholar]
- 16.Cao G, Noti JD, Blachere FM, Lindsley WG, Beezhold DH. Development of an improved methodology to detect infectious airborne influenza virus using the NIOSH bioaerosol sampler. J Environ Monit. 2011;13:3321–3328. doi: 10.1039/c1em10607d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gustin KM, Katz JM, Tumpey TM, Maines TR. Comparison of the levels of infectious virus in respirable aerosols exhaled by ferrets infected with influenza viruses exhibiting diverse transmissibility phenotypes. J Virol. 2013;87:7864–7873. doi: 10.1128/JVI.00719-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Belser JA, et al. Pathogenesis and transmission of triple-reassortant swine H1N1 influenza viruses isolated before the 2009 H1N1 pandemic. J Virol. 2011;85:1563–1572. doi: 10.1128/JVI.02231-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lakdawala SS, et al. Eurasian-origin gene segments contribute to the transmissibility, aerosol release, and morphology of the 2009 pandemic H1N1 influenza virus. PLoS Pathog. 2011;7:e1002443. doi: 10.1371/journal.ppat.1002443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Campbell PJ, et al. The M segment of the 2009 pandemic influenza virus confers increased neuraminidase activity, filamentous morphology, and efficient contact transmissibility to A/Puerto Rico/8/1934-based reassortant viruses. J Virol. 2014;88:3802–3814. doi: 10.1128/JVI.03607-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zanin M, et al. Pandemic swine H1N1 influenza viruses with almost undetectable neuraminidase activity are not transmitted via aerosols in ferrets and are inhibited by human mucus but not swine mucus. J Virol. 2015;89:5935–5948. doi: 10.1128/JVI.02537-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chou YY, et al. The M segment of the 2009 new pandemic H1N1 influenza virus is critical for its high transmission efficiency in the guinea pig model. J Virol. 2011;85:11235–11241. doi: 10.1128/JVI.05794-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu R, et al. Functional balance of the hemagglutinin and neuraminidase activities accompanies the emergence of the 2009 H1N1 influenza pandemic. J Virol. 2012;86:9221–9232. doi: 10.1128/JVI.00697-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koster F, et al. Exhaled aerosol transmission of pandemic and seasonal H1N1 influenza viruses in the ferret. PLoS One. 2012;7:e33118. doi: 10.1371/journal.pone.0033118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roberts KL, Shelton H, Stilwell P, Barclay WS. Transmission of a 2009 H1N1 pandemic influenza virus occurs before fever is detected, in the ferret model. PLoS One. 2012;7:e43303. doi: 10.1371/journal.pone.0043303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steel J, Lowen AC, Mubareka S, Palese P. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog. 2009;5:e1000252. doi: 10.1371/journal.ppat.1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van Hoeven N, et al. Human HA and polymerase subunit PB2 proteins confer transmission of an avian influenza virus through the air. Proc Natl Acad Sci USA. 2009;106:3366–3371. doi: 10.1073/pnas.0813172106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith GJ, et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature. 2009;459:1122–1125. doi: 10.1038/nature08182. [DOI] [PubMed] [Google Scholar]
- 29.Mehle A, Doudna JA. Adaptive strategies of the influenza virus polymerase for replication in humans. Proc Natl Acad Sci USA. 2009;106:21312–21316. doi: 10.1073/pnas.0911915106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johnson GR, Morawska L. The mechanism of breath aerosol formation. J Aerosol Med Pulm Drug Deliv. 2009;22:229–237. doi: 10.1089/jamp.2008.0720. [DOI] [PubMed] [Google Scholar]
- 31.Fabian P, Brain J, Houseman EA, Gern J, Milton DK. Origin of exhaled breath particles from healthy and human rhinovirus-infected subjects. J Aerosol Med Pulm Drug Deliv. 2011;24:137–147. doi: 10.1089/jamp.2010.0815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fairchild CI, Stampfer JF. Particle concentration in exhaled breath. Am Ind Hyg Assoc J. 1987;48:948–949. doi: 10.1080/15298668791385868. [DOI] [PubMed] [Google Scholar]
- 33.Papineni RS, Rosenthal FS. The size distribution of droplets in the exhaled breath of healthy human subjects. J Aerosol Med. 1997;10:105–116. doi: 10.1089/jam.1997.10.105. [DOI] [PubMed] [Google Scholar]
- 34.Fabian P, et al. Influenza virus in human exhaled breath: An observational study. PLoS One. 2008;3:e2691. doi: 10.1371/journal.pone.0002691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gralton J, Tovey ER, McLaws ML, Rawlinson WD. Respiratory virus RNA is detectable in airborne and droplet particles. J Med Virol. 2013;85:2151–2159. doi: 10.1002/jmv.23698. [DOI] [PubMed] [Google Scholar]
- 36.Lindsley WG, et al. Measurements of airborne influenza virus in aerosol particles from human coughs. PLoS One. 2010;5:e15100. doi: 10.1371/journal.pone.0015100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lindsley WG, et al. Viable influenza A virus in airborne particles from human coughs. J Occup Environ Hyg. 2015;12:107–113. doi: 10.1080/15459624.2014.973113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Milton DK, Fabian MP, Cowling BJ, Grantham ML, McDevitt JJ. Influenza virus aerosols in human exhaled breath: Particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013;9:e1003205. doi: 10.1371/journal.ppat.1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lednicky JA, Loeb JC. Detection and isolation of airborne influenza a H3N2 virus using a Sioutas personal cascade impactor sampler. Influenza Res Treat. 2013;2013:656825. doi: 10.1155/2013/656825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nishiura H, Yen HL, Cowling BJ. Sample size considerations for one-to-one animal transmission studies of the influenza A viruses. PLoS One. 2013;8:e55358. doi: 10.1371/journal.pone.0055358. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.