Abstract
To better understand country of birth-related shifts in the demography of people newly diagnosed with HIV infection, we compared demographic and clinical characteristics of foreign-born and U.S.-born residents of King County, WA diagnosed with HIV from 2006–2015. The proportion of cases that were foreign-born increased from 23% to 34% during this time. Most foreign-born cases were born in Africa (34%), Latin America (32%), Asia (22%), or Europe (7%). Latin Americans and Asians were similar to U.S.-born individuals by HIV risk factor and gender, while Africans were more likely to be female and less often men who have sex with men. In 2015, approximately 15% of cases presumptively newly diagnosed in King County were foreign-born individuals who self-reported a pre-immigration HIV diagnosis. Increases in foreign-born individuals previously diagnosed out of country may lead to inaccuracy in the count of new diagnoses, including an over-estimate of community-acquired HIV in King County.
Keywords: foreign-born, HIV, immigrants, migrants, surveillance
Introduction
An estimated 13% of the total U.S. population and 16% of U.S. residents diagnosed with HIV are foreign-born.(1, 2) Between 2000 and 2014 the foreign-born population in the U.S. was estimated to have increased by one third.(3) The overall U.S. foreign-born population was 42.1 million in 2015.(2) King County (KC), Washington includes the city of Seattle and is a major port of entry on the west coast. KC has been a center for refugee resettlement since the Vietnam War.(4, 5) The Seattle area is also a technology industry hub,(6) and draws many foreign-born workers.(7) As a result, KC has a larger proportion of foreign-born residents than the U.S. as a whole (21%),(8) and the county’s foreign-born population increased 61% from 2000 to 2015.(9, 10) While restrictions were in place to limit immigration to the U.S. for people living with HIV (PLWH) from 1992 until 2010,(11) current U.S. immigration policy permits foreign-born individuals to enter the United States regardless of HIV status and without undergoing HIV testing.(12)
The National HIV Surveillance System (NHSS) is used to monitor HIV in all U.S. jurisdictions, and collects data on nativity. NHSS defines cases as newly-diagnosed based on a first documented HIV positive test. Many foreign-born PLWH may have acquired HIV, and a portion of these may have been diagnosed with HIV, prior to entering the U.S. However, cases with a “new” diagnosis in the U.S. and no documentation of a previous positive HIV test elsewhere are counted as new HIV infections in NHSS. These cases are not preventable by local HIV prevention programs, and thus they require different public health resources than PLWH acquired in the U.S., including a greater emphasis on linkage to and retention in care, as well as partner services to prevent onward transmission. As such, the documentation of foreign-born PLWH diagnosed before arrival in the U.S. can help local health jurisdictions better understand and respond to their local epidemics.
One of the primary goals of the National HIV/AIDS Strategy is to reduce HIV-related health disparities. Foreign-born people are more likely than U.S.-born people to face challenges in accessing health care,(13–15) which may contribute to disparities across the HIV care continuum. We have found that African-born PLWH in King County have lower CD4 counts at diagnosis and are more likely to be diagnosed with stage 3 disease (AIDS) within three months of HIV diagnosis than U.S.-born PLWH.(16) Others have reported similar findings for foreign-born Latinos and foreign-born blacks, compared to their U.S.-born counterparts.(17–19) Thus, collecting and presenting nativity of PLWH may identify disparities that might otherwise be unrecognized and unaddressed.(20)
In this study, we examined 10-year trends among people classified as newly diagnosed with HIV in King County, WA to describe differences in NHSS and self-reported diagnosis dates. To address the issue of HIV-related disparities, we sought to compare viral suppression, linkage to care, and other clinical outcomes among foreign-born and U.S.-born PLWH in King County, and to further examine differences in these clinical outcomes by region of birth among foreign-born PLWH.
Methods
Data for King County residents diagnosed with HIV 2006 to 2015 were obtained from NHSS and supplemental surveillance activities to assess characteristics and trends in HIV diagnosis among foreign-born individuals, including how often these individuals self-reported HIV diagnoses prior to U.S. immigration or NHSS diagnosis date. Supplemental surveillance data include HIV incidence surveillance, molecular HIV surveillance, and partner services (PS) interview data.
NHSS data are collected from a variety of data sources using a standard confidential case report. Most initial HIV diagnostic data comes to the health department by passive laboratory reporting of diagnostic and other HIV-specific clinical tests, typically followed by a review of medical records by public health staff for additional clinical and socio-demographic data. Data may also be reported by medical providers and facilities. NHSS data include race/ethnicity, HIV risk factors, age, previous HIV tests (negative and positive), country of birth, and the results of CD4+ T lymphocyte (CD4) and plasma viral load (VL) tests. Current residence and vital status in NHSS are updated on an ongoing basis by database linkage and other auxiliary data sources and investigations. NHSS data, including relocation and vital status, are as of August 1st 2016.
Public Health- Seattle and King County offers PS to all people with newly diagnosed HIV infection to help assure that their potentially exposed sex and needle/works sharing partners are HIV tested, and to assist people with HIV infection to link to medical care. As part of the PS interview, individuals are asked for country of birth, and for in-migrants, date of in-migration or length of residence in the U.S. Additionally, all persons interviewed for PS are asked about the date of their first positive (i.e. self-reported HIV diagnosis date) and last negative HIV test.
HIV incidence surveillance (HIS) activities include collecting remnant HIV diagnostic sera for serologic testing algorithm for recent HIV seroconversion (STARHS) as well as collecting additional surveillance data, including data regarding a self-reported first HIV diagnosis date which may have been documented in a medical record for individuals without a PS interview. Over the course of observation, two STARHS assays -- BED (2006–2014) and an Avidity assay (2014–2015) -- were used to determine the probability that recently diagnosed individuals were also infected with HIV recently.(21) A “STARHS recent” HIV infection is defined as one that occurred within approximately a half year of HIV diagnosis.
Molecular HIV surveillance (MHS) activities include seeking HIV-1 genotypic sequences from all genotypic drug resistance testing done for HIV-infected individuals in King County. MHS data are not yet fully part of routine, passive electronic laboratory surveillance conducted through NHSS, as the data most labs conducting genotypic testing report are the interpretations of a genotypic test, not the actual viral sequence. The MHS project seeks the viral sequences themselves. Sequences were analyzed for HIV strain and drug resistance using the Stanford database algorithm.3
Four main categories were created to describe the region of birth for foreign-born individuals: Latin America, Asia, Africa, and Other. Canadians, Europeans, people from Greenland, Oceania (Australia and New Zealand) and the U.S. territories were included in an “Other” category. Latin America included Mexico, Central and South America, the Caribbean countries, Bermuda, St. Pierre and Miquelon. The rest of the world was divided into Africa and Asia (which includes the Indian sub-continent).
We used Chi square tests to compare differences in proportions, and Chi square for trend to evaluate the statistical significance of trends. We utilized a Z score to compare death rates among overall foreign-born versus U.S.-born individuals (Epi Info version 6 Division of Health Informatics & Surveillance), Center for Surveillance, Epidemiology & Laboratory Services, Centers for Disease Control and Prevention [CDC]). For the comparison of death rates, follow-up time was calculated from NHSS HIV diagnosis until death, or until censor date (August 1, 2016).
Results
A total of 2,875 KC residents were diagnosed with HIV over the decade from 2006 to 2015; 2,724 (95%) had a known birthplace and 814 (30%) of these individuals were foreign-born. Foreign-born cases increased more than 50% over the decade – from 23% of total cases in 2006 to 34% in 2015 (χ2 for trend=22.7, p<0.001, data not shown). Foreign-born individuals included 34% from Africa, 32% from Latin America (Mexico, South America, Central America and the Caribbean), 22% from Asia, 7% from Europe, and 2% each from Canada, Oceania, and U.S. territories (Figure 1). Individuals with missing birthplace (N=151) are excluded from the remainder of the analyses. African-born individuals were born in 30 African countries – 98% were born in sub-Saharan countries. Over half were born in two countries: 41% from Ethiopia and 16% from Kenya, followed by 5% from Eritrea, 4% from Somalia and 4% from South Africa. Foreign-born Latin American individuals were predominantly born in Mexico (63%); this grouping includes 18 other countries with 17% from South America, 14% from Central America, and 5% from the Caribbean. Foreign-born Asian individuals included Pacific Islanders (API). API were born in 22 countries; the largest number of individuals were born in Vietnam (23%) followed by the Philippines (14%), Thailand (9%), Burma/Myanmar (9%), China (8%), and Cambodia (8%).
Figure 1. Birth regions of 2724 King County, WA residents diagnosed with HIV 2006–2015*.
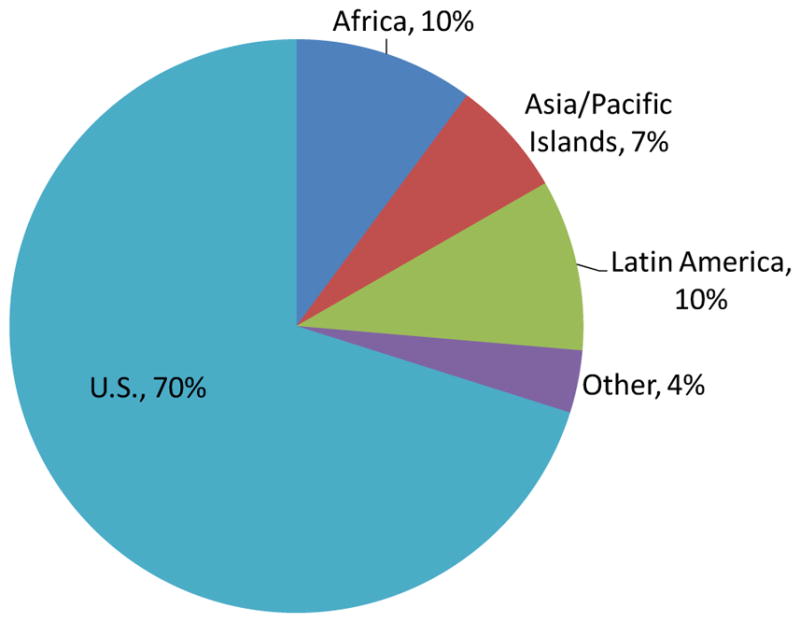
*Figure excludes 5% with missing country of birth
**“Other” category includes people born in Europe (59%), U.S. Territories (14%), Canada (14%), and Oceania (14%).
Compared to U.S.-born cases, foreign-born cases were less likely than U.S.-born cases to be men who have sex with men (MSM, 44% vs. 84%, χ2=151.2, p<.0001; Table I), more likely to be female, (27% versus 8%, χ2=186.8, p<0.001), and less likely to have the HIV strain B, the predominant strain in North America (60% versus 97%, χ2=505.6, p<0.001, Table II). Of all foreign-born individuals, those born in Africa were most likely to be female (58%, Table I) or be reported with heterosexual HIV risk (70% of those with a known risk, 30% overall) and least likely to be MSM (12% of those with known risks and 5% overall). Other foreign-born groups were more similar to U.S.-born cases. Latin Americans were most similar to U.S.-born individuals by gender and transmission category with 90% male, and 67% MSM (relative to 92% and 84% of U.S.-born individuals; Table I). Excluding those with unknown risk, 86% of Latin Americans newly diagnosed with HIV in King County were MSM, relative to 90% of U.S.-born individuals. Foreign-born API were 85% male and 56% MSM (Table I).
Table I.
Characteristics of U.S.-born and foreign-born individuals diagnosed with HIV in King County, 2006 to 2015.
| African N=276 n, (%) |
Asian/Pacific Islander N=179 n, (%) |
Latin/S. American N=263 n, (%) |
All Foreign-born** N=814 n, (%) |
U.S.-born*** N=1910 n, (%) |
||
|---|---|---|---|---|---|---|
| Gender | Female | 159 (58) | 27 (15) | 26 (10) | 222 (27) | 147 (8) |
| Transmissi on category | MSM* | 14 (5) | 100 (56) | 177 (67) | 360 (44) | 1596 (84) |
| IDU* | 2 (1) | 4 (2) | 7 (3) | 9 (2) | 176 (4) | |
| Heterosexual | 82 (30) | 19 (11) | 23 (9) | 131 (16) | 94 (5) | |
| Unknown | 159 (58) | 54 (30) | 56 (21) | 286 (35) | 136 (7) | |
| Age at HIV diagnosis | <20 years | 22 (8) | 5 (3) | 5 (2) | 34 (4) | 43 (2) |
| 50+ years | 58 (21) | 23 (13) | 23 (9) | 114 (14) | 291 (15) | |
| Linked to care | Within one month of HIV diagnosis | 247 (89) | 159 (89) | 220 (84) | 710 (87) | 1629 (85) |
| Initial CD4 | <200 | 102 (38) | 55 (31) | 82 (32) | 260 (33) | 383 (20) |
| 200–499 | 112 (42) | 81 (46) | 112 (44) | 348 (44) | 775 (41) | |
| 500+ | 55 (20) | 40 (23) | 63 (25) | 187 (24) | 712 (38) | |
| Late HIV diagnosis concurrent AIDS or within: | Concurrent | 106 (38) | 61 (34) | 81 (31) | 274 (34) | 404 (21) |
| 6 months | 119 (43) | 69 (39) | 94 (36) | 311 (38) | 451 (24) | |
| 1 year | 121 (44) | 72 (40) | 96 (37) | 319 (39) | 479 (25) | |
| Out-migration | Yes (as of April 2016) | 44 (16) | 22 (12) | 51 (19) | 147 (18) | 487 (25) |
| Most recent viral load | Suppressed (<200) | 234 (85) | 156 (87) | 220 (84) | 680 (84) | 1476 (77) |
| Not suppressed or missing (1–4) are missing) | 42 (15) | 23 (13) | 43 (16) | 134 (16) | 434 (23) | |
| Vital status | Died (as of April 2016) | 8 (3) | 10 (6) | 13 (5) | 37 (5) | 118 (6) |
|
African N=217 n, (%) |
Asian/Pacific Islander N=152 n, (%) |
Latin/S. American N=224 n, (%) |
All Foreign-born N=677 n, (%) |
U.S.-born N=1576 n, (%) |
||
| Interval of self-reported HIV date to documented HIV date^ | <=3 months | 122 (56) | 114 (75) | 189 (84) | 496 (73) | 1473 (93) |
| 4–12 months | 12 (6) | 2 (1) | 4 (2) | 21 (3) | 30 (2) | |
| >1 year | 83 (38) | 36 (24) | 31 (14) | 160 (24) | 73 (5) |
MSM=Men who have sex with men; IDU = injection drug users, excluding MSM.
Includes others not born in Africa, Asia or Latin America, namely: 57 Europeans, 14 Canadians, 14 people born in Oceania, and 14 individuals born in U.S. territories
Excludes individuals born in U.S. territories
Includes only people with a self-reported HIV date
Table II.
HIV strain by region of birth for individuals diagnosed with HIV in King County, 2006 to 2015.
| HIV strain | African N=179 n, (%) |
Asian/Pacific Islander N=115 n, (%) |
Latin/S. American N=204 n, (%) |
All Foreign-born** N=562 n, (%) |
U.S.-born*** N=1547 n, (%) |
|---|---|---|---|---|---|
| A | 24 (13) | 1 (1) | -- | 30 (5) | -- |
| B | 14 (8) | 74 (64) | 193 (95) | 336 (60) | 1500 (97) |
| C | 91 (51) | 3 (3) | -- | 95 (17) | 10 (1) |
| CRF01AE | 11 (6) | 34 (30) | -- | 48 (8) | -- |
| CRF02AG | 27 (15) | 1 (1) | -- | 29 (5) | -- |
| Other* | 12 (7) | 2 (2) | 8 (4) | 24 (4) | 24 (2) |
Other includes 48 individuals, half U.S.-born and half foreign-born with the following strains: D (54%), G (23%), F (10%), H (4%), J (4%), and K (4%)
Includes others not born in Africa, Asia or Latin America, namely: Europeans, Canadians, people born in Oceania, and individuals born in U.S. territories
Excludes individuals born in U.S. territories
Latin American individuals had a comparable prevalence of strain B (95%) to those born in the U.S. (97%, Table II). Strains among foreign-born API were also predominantly B (64%), but also included CRF01 AE (30%) and C (3%). Reflecting a greater diversity of strains from the region of origin,(22), African-born individuals had the lowest prevalence of strain B (8%); other viral strains included C (51%), A (13%), CRF02-AG (15%), CRF02-AE (6%), and others (G, H, J, K totaling 7%).
Self -reported date of first HIV diagnosis was available for 2,258 individuals (83%). Foreign-born cases were roughly five times as likely as U.S.-born cases to self-report HIV diagnosis >1 year prior to NHSS diagnosis date (24% vs 5%, χ2=184.4, p<0.0001). Among foreign-born cases, African-born individuals were most likely (38%) to report an HIV diagnosis >1 year prior to the National HIV Surveillance System (NHSS) HIV diagnosis date, compared to 14% among Latin American cases and 24% among foreign-born API. We had date of entry to the U.S. for 269 of 814 (33%) of foreign-born cases; of these, 195 (72%) entered the U.S. before (or within one month of) their HIV diagnosis in NHSS and a corresponding 28% were diagnosed with HIV prior to or at the time of U.S. entry. However among those with dates of both self-reported first HIV diagnosis and entry to the U.S., 103 of 236 (44%) reported an HIV diagnosis prior to or at the time of entry to the U.S.
Assuming those with non-missing data are representative of all foreign-born individuals, roughly 15% of individuals diagnosed with HIV in King County in 2015 were actually diagnosed among foreign-born individuals prior to U.S. entry (34% of newly diagnosed individuals were foreign-born in 2015, multiplied by 44% of them with self-reported diagnoses prior to NHSS diagnosis dates). In other words, misclassification of diagnosis date of foreign-born cases led to an estimated 15% over-estimate of new King County HIV diagnoses in 2015.
Approximately half of individuals (51%) diagnosed with HIV during the study period had results for serologic testing algorithm for identifying recent HIV infection (STARHS). Of these, African PLWH were least likely to have a result indicating they likely had a recent HIV infection (Table III, 15%) relative to 48% of U.S.-born individuals (χ2=51.3, p<0.001).
Table III.
Serologic testing algorithm for determining recent HIV infection (STARHS) results by nativity King County, 2006 to 2015.
| African (N^=133) N, % |
Asian/Pacific Islander (N^=78) N, % |
Latin/S. American (N^=133) N, % |
All Foreign-born** (N^=386) N, % |
U.S.-born *** (N^=1014) N, % |
||
|---|---|---|---|---|---|---|
| STARHS recent versus long-standing infection | Recent infection * | 20 (15) | 20 (26) | 52 (39) | 104 (27) | 485 (48) |
| Long-standing infection | 113 (85) | 58 (74) | 81 (61) | 282 (73) | 529 (52) | |
| Missing (not included with other two rows) | 143 | 101 | 130 | 428 | 896 |
Recent infection indicates serologic testing algorithm for recent HIV surveillance (STARHS) test results suggestive of infection within about half of a year from National HIV Surveillance System HIV diagnosis date.
Includes others not born in Africa, Asia or Latin America, namely: Europeans, Canadians, people born in Oceania, and individuals born in U.S. territories
Excludes individuals born in U.S. territories
Column totals (N^) exclude those with no STARHS results
At the time of HIV diagnosis, 33% of foreign-born individuals had an AIDS-defining CD4 count of <200 cells/microL and 39% of foreign-born individuals had an AIDS diagnosis within one year of HIV diagnosis. This compares to 20% and 25% of U.S.-born individuals respectively (χ2=45.5 for CD4 count <200 cells/microL, χ2=54.9 for AIDS diagnosis within one year, p < 0.001 for both comparisons). Among foreign-born cases, African-born individuals were most likely (44%) to have had an AIDS diagnosis within a year of their HIV diagnosis, followed by API (40%) and Latin Americans (37%); all groups have a higher prevalence of late diagnosis (AIDS diagnosed within a year of HIV diagnosis) than observed among U.S.-born cases (25%).
While foreign-born persons were more likely to have a late HIV diagnosis, they were also more likely to achieve viral suppression. A most recent viral load test indicated viral suppression (<200 copies per mL) for 84% of foreign-born versus 77% of U.S.-born individuals (Table I, χ2=13.5, p=0.002). Of all birth regions, API were most likely to have a recent viral load indicative of viral suppression with < 200 copies (87% with viral suppression among API versus 77% among U.S.-born, χ2=9.3, p=0.002). Mortality was roughly equivalent with 5% of foreign-born cases and 6% of U.S.-born cases known to have died by mid-2016 (χ2=2.8, P > 0.05; Table I). As length of follow-up for foreign-born individuals tended to be shorter than those born in the U.S. (mean 5.2 years versus 5.8 years), we also compared deaths per 100 person-years. Foreign-born individuals had 0.9 deaths per 100 person-years relative to 1.1 deaths per 100 person years among U.S.-born individuals (Fisher’s exact test=2.8, mid-p=0.17).
Conclusions
We found that approximately 30% of persons newly reported with HIV in King County from 2005–2015 were foreign-born, and that this proportion increased over time, with foreign-born individuals accounting for over one-third of new cases in 2015. While this is consistent with growth in the foreign-born population in King County as a whole, from 11% of the total county population in 1990 to 25% in 2012,(23) it has important implications for HIV surveillance and prevention planning. We estimate that approximately 15% of presumptive new HIV diagnoses in our county during the study period occurred among foreign-born persons who had been diagnosed with HIV prior to their arrival in the U.S. Although these diagnoses may have been “new” in the U.S., counting these as incident HIV cases does not reflect true HIV incidence in King County, nor does it allow us to accurately measure the effectiveness of our local HIV prevention efforts. Finally, we also observed some positive outcomes for foreign-born persons living with HIV: despite the fact that foreign-born individuals were more likely than their U.S.-born counterparts to have an AIDS diagnosis within one year of HIV diagnosis (39% vs. 25%), we found greater levels of viral suppression among foreign-born compared to U.S.-born cases, and equivalent measures of mortality across the two groups.
Several studies across diverse settings have found that U.S.-born individuals with HIV are more likely than foreign-born individuals to have acquired HIV through male to male sexual contact, while foreign-born persons are more likely to be have been exposed through heterosexual contact.(1, 12, 13, 25) We also noted differences in the epidemiology of HIV across foreign-born persons by region of birth, similar to findings reported by Prosser, et al. and Sheehan et al. for U.S. Blacks and Florida Latinos, respectively.(1, 13) Furthermore, similar to our finding, other investigators have found evidence of late diagnosis among foreign-born PLWH,(17, 24–27) putting individual PLWH at risk for increased HIV-related morbidity, and foreign-born communities at risk for greater onward transmission of HIV.
The proportion of the U.S.-born population that is foreign-born increased from 12.5% in 2006(28) to 13.2% in 2014.(29) As the foreign-born population grows, it is perhaps to be expected that the proportion of newly diagnosed HIV cases that are foreign-born will also increase, and that immigrants from countries with generalized HIV epidemics may be both more likely to arrive with an HIV diagnosis and to reflect a heterosexual epidemic, as we have observed with African immigrants in King County.(16) Some racial and ethnic groups, as well as local areas with large foreign-born populations, are likely to be more significantly impacted by this trend. For example, in 2014, 34% of Latinos living in the U.S. were foreign-born, but from 2008–2013 an estimated 43% of Latino PLWH were foreign-born.(29, 30) Similarly, the South, the area most impacted by HIV in the U.S., experienced a 55% increase in the foreign-born population from 2000–2013, the largest growth in the foreign-born population in the country.(31) In New York City, Wiewel and colleagues have reported the proportion of newly diagnosed HIV cases among foreign-born individuals increased from 17% in 2001 to 28% in 2009.(27) Differences in the epidemiology of HIV by region of birth may result in some foreign-born populations not being well served by existing HIV prevention programs – for example, the HIV epidemic in King County is concentrated among MSM, but roughly 10% of new diagnoses annually occur among African-born people, the majority of whom acquired HIV via heterosexual contact. Language and cultural differences may present additional barriers to either developing new or implementing existing HIV prevention programs for foreign-born populations. These barriers may require additional public health resources to overcome. Our observation that foreign-born populations are diagnosed later than U.S.-born people and the increasing number of foreign-born people in the U.S. highlight the need for resources to find people who are undiagnosed and prevent ongoing transmission in foreign-born communities.
Two previous studies have compared date of HIV diagnosis according to NHHS to self-report, and/or medical record data.(32, 33) Hall et al. found that 30% of participants self-reported an earlier diagnosis year than the NHSS diagnosis year.(32) Although both groups of investigators concluded that migration could account for some of the discrepancies observed in diagnosis dates, neither analysis included data about place of birth. While we found that a lower percentage of King County cases had a self-reported date of diagnosis more than one year before the date reported in NHHS (11% overall), this phenomenon was much higher among foreign-born cases (24%).
One of the strengths of our analysis is that PHSKC routinely collects information on country of birth and self-reported date of first HIV diagnosis, data which are not consistently collected for foreign-born persons in many jurisdictions in the U.S. We also attempt to contact all patients newly reported with HIV in King County for partner services, providing us with the opportunity to ask patients for additional information that may not be available from providers or through case reports. However, our study is also subject to several limitations. First, we were missing self-reported date of first HIV diagnosis for 17% of cases, and this proportion varied somewhat over time. While we believe that these data are missing at random, if PLWH who were missing these data were more or less likely to be diagnosed 1 year before their date of diagnosis in NHHS, it could have resulted in an over or underestimate of foreign-born persons who were diagnosed with HIV prior to arrival in the U.S. Additionally, the foreign-born population of King County varies from the U.S. foreign-born population as a whole, and from other local areas; King County has a higher proportion of Asian and African immigrants and refugees, and a lower proportion of foreign-born Latinos, than the U.S. population overall. As such, our results may not be representative of the foreign-born population living with HIV in the U.S., or in other local jurisdictions.
In conclusion, a growing percentage of King County’s residents classified as having newly diagnosed HIV infection – over one-third of such cases in 2015 – occur in people born outside of the U.S. Over one-third of these foreign-born individuals self-reported HIV diagnoses more than a year prior to their HIV diagnosis date, leading to an overestimate of the number of new diagnoses each year and a growing proportion of cases which could not have been averted through local HIV prevention efforts. HIV prevention has always been a global issue, and these local data emphasize the interrelatedness of HIV infections around the globe. The increase in the proportion of new cases occurring in foreign-born people and the indicators of late diagnosis we observed in this population also highlight the need for greater local efforts to promote testing and other prevention interventions in foreign-born communities, as well as the need for improved data on nativity, HIV testing history, and immigration dates from people with newly diagnosed HIV.
Acknowledgments
Funding: This work was supported by CDC cooperative agreement CDC-RFA-PS13-1302, and by NIAD K01 AI095060 (to R.K.).
Footnotes
Compliance with Ethical Standards
Previous publication: Portions of this work appeared previously in a local HIV epidemiology report (circulation about 350 combined paper and email distribution).
Conflict of Interest: The authors declare that they have no conflicts of interest.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: This was an analysis of data collected for surveillance purposes. For this type of study, formal consent is not required.
References
- 1.Prosser AT, Tang T, Hall HI. HIV in persons born outside the United States, 2007–2010. JAMA. 2012;308(6):601–7. doi: 10.1001/jama.2012.9046. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Census Bureau. United States Quick Facts. 2016 [cited 2016 June 29]. Available from: http://www.census.gov/quickfacts/table/PST045215/00.
- 3.Migration Policy Institute. Frequently Requested Statistics on Immigrants and immigration in the United States. 2016 [cited 2016 May 31]. Available from: http://www.migrationpolicy.org/article/frequently-requested-statistics-immigrants-and-immigration-united-states.
- 4.Banel F. Refugee, immigration controversy has long history in Washington: MYNorthwest. 2015 [cited 2017 September 8]. Available from: http://mynorthwest.com/147827/refugee-immigration-controversy-has-long-history-in-washington/
- 5.Balk G. Seattle Times. 2015. Nov 19, What King County’s refugee populations look like|Interactive map. [Google Scholar]
- 6.Sims R. Managing High-Tech Growth in King County. Brookings Institution; 2000. [cited 2017 September 8]. Available from: https://www.brookings.edu/articles/managing-high-tech-growth-in-king-county/ [Google Scholar]
- 7.Henderson T. Asians Replace Mexicans in U.S. Immigration stream. Providence Journal. 2016 May 7;
- 8.King County Office of Economic and Financial Analysis. Demographic Trends of King County: King County Office of Economic and Financial Analysis. 2016 [Available from: http://www.kingcounty.gov/independent/forecasting/benchmarks/Demographics.aspx.
- 9.U.S. Census Bureau. Profile of Selected Social Characteristics. 2000 [cited 2017 July 20]. Available from: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=CF.
- 10.U.S. Census Bureau. Selected characteristics of the native and foreign-born populations. King County; Washingon: [cited 2017 July 19]. Available from: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_5YR_S0501&prodType=table. [Google Scholar]
- 11.Centers for Disease Control and Prevention. Immigrant and Refugee Health: General Questions and Answers. [cited 2016 April 4]. Available from: http://www.cdc.gov/immigrantrefugeehealth/laws-regs/hiv-ban-removal/final-rule-general-qa.html.
- 12.Centers for Disease Control and Prevention. Medical examination of aliens - Removal of human immunodeficiency virus (HIV) infection from definition of communicable disease of public health significance. Final rule. Fed Regist. 2009;74:56547–62. [PubMed] [Google Scholar]
- 13.Wafula EG, Snipes SA. Barriers to health care access faced by black immigrants in the US: theoretical considerations and recommendations. J Immigr Minor Health. 2014;16(4):689–98. doi: 10.1007/s10903-013-9898-1. [DOI] [PubMed] [Google Scholar]
- 14.Lebrun LA, Dubay LC. Access to primary and preventive care among foreign-born adults in Canada and the United States. Health Serv Res. 2010;45(6 Pt 1):1693–719. doi: 10.1111/j.1475-6773.2010.01163.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vargas Bustamante A, Chen J, Fang H, Rizzo JA, Ortega AN. Identifying health insurance predictors and the main reported reasons for being uninsured among US immigrants by legal authorization status. Int J Health Plann Manage. 2014;29(1):e83–96. doi: 10.1002/hpm.2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kerani RP, Herbeck JT, Buskin SE, et al. Evidence of Local HIV Transmission in the African Community of King County, Washington. J Immigr Minor Health. 2017;19(4):891–6. doi: 10.1007/s10903-016-0458-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Espinoza L, Hall HI, Hu X. Diagnoses of HIV infection among Hispanics/Latinos in 40 states and Puerto Rico, 2006–2009. J Acquir Immune Defic Syndr. 2012;60(2):205–13. doi: 10.1097/QAI.0b013e31824d9a29. [DOI] [PubMed] [Google Scholar]
- 18.Johnson AS, Hu X, Dean HD. Epidemiologic differences between native-born and foreign-born black people diagnosed with HIV infection in 33 U.S. states, 2001–2007. Public Health Rep. 2010;125(Suppl 4):61–9. doi: 10.1177/00333549101250S410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sheehan DM, Trepka MJ, Fennie KP, Maddox LM. Rate of new HIV diagnoses among Latinos living in Florida: disparities by country/region of birth. AIDS Care. 2015;27(4):507–11. doi: 10.1080/09540121.2014.978731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koku EF, Rajab-Gyagenda WM, Korto MD, et al. HIV/AIDS among African Immigrants in the U.S.: The Need for Disaggregating HIV Surveillance Data by Country of Birth. J Health Care Poor Underserved. 2016;27(3):1316–29. doi: 10.1353/hpu.2016.0128. [DOI] [PubMed] [Google Scholar]
- 21.Hanson DL, Song R, Masciotra S, et al. Mean Recency Period for Estimation of HIV-1 Incidence with the BED-Capture EIA and Bio-Rad Avidity in Persons Diagnosed in the United States with Subtype B. PLoS One. 2016;11(4):e0152327. doi: 10.1371/journal.pone.0152327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hemelaar J, Gouws E, Ghys PD, Osmanov S. WHO-UNAIDS Network for HIV Isolation Characterisation. Global trends in molecular epidemiology of HIV-1 during 2000–2007. AIDS. 2011;25(5):679–89. doi: 10.1097/QAD.0b013e328342ff93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The Pew Charitable Trusts. Changing Patterns in U.S. Immigration and Population. 2014. Dec 18, [Google Scholar]
- 24.Levy V, Prentiss D, Balmas G, et al. Factors in the delayed HIV presentation of immigrants in Northern California: implications for voluntary counseling and testing programs. J Immigr Minor Health. 2007;9(1):49–54. doi: 10.1007/s10903-006-9015-9. [DOI] [PubMed] [Google Scholar]
- 25.Saganic L, Carr J, Solorio R, Courogen M, Jaenicke T, Duerr A. Comparing Measures of Late HIV Diagnosis in Washington State. AIDS Res Treat. 2012;2012:182672. doi: 10.1155/2012/182672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sheehan DM, Trepka MJ, Fennie KP, et al. Individual and Neighborhood Determinants of Late HIV Diagnosis Among Latinos, Florida, 2007–2011. J Immigr Minor Health. 2017;19(4):825–34. doi: 10.1007/s10903-016-0422-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wiewel EW, Torian LV, Nasrallah HN, Hanna DB, Shepard CW. HIV diagnosis and utilisation of HIV-related medical care among foreign-born persons in New York City, 2001–2009. Sexually transmitted infections. 2013;89(5):380–2. doi: 10.1136/sextrans-2012-050677. [DOI] [PubMed] [Google Scholar]
- 28.Gonzales F. Statistical Portrait of the Foreign-born Population in the United States, 2006. Pew Research Center; Jan 23, 2008. [Google Scholar]
- 29.Patten E. The Nation’s Latino Population is Defined by Its Youth. Washington, D.C: Pew Research Center; 2016. Apr, [Google Scholar]
- 30.Gray KM, Valverde EE, Tang T, Siddiqi AE, Hall HI. Diagnoses and Prevalence of HIV Infection Among Hispanics or Latinos - United States, 2008–2013. MMWR Morb Mortal Wkly Rep. 2015;64(39):1097–103. doi: 10.15585/mmwr.mm6439a2. [DOI] [PubMed] [Google Scholar]
- 31.Pew Research Center. Modern Immigration Wave Brings 59 Million to U.S., Driving Population Growth and Change through 2065: Views of Immigration’s Impact on U.S. Society Mixed. Washington, D.C: Sep 28, 2015. [Google Scholar]
- 32.Hall HI, Li J, Campsmith M, Sweeny P, Lee LM. Date of first positive HIV test: reliability of information collected for HIV/AIDS surveillance in the United States. Public Health Rep. 2005;120(1):89–95. doi: 10.1177/003335490512000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCoy SI, Jones B, Leone PA, et al. Variability of the date of HIV diagnosis: a comparison of self-report, medical record, and HIV/AIDS surveillance data. Ann Epidemiol. 2010;20(10):734–42. doi: 10.1016/j.annepidem.2010.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


