Abstract
Purpose
Approximately 348,000 ventral hernia repairs are performed annually in the United States and the incisional hernia recurrence rate is approximately 20% as a result of suture and mesh device failure. Device failure is related to changes at the suture/tissue interface that leads to acute or chronic suture pull-through and surgical failure. To better manage mechanical tension, we propose a modified mesh design with extensions and demonstrate its mechanical superiority.
Methods
Comparative uniaxial static tensile testing was conducted on polypropylene suture and a modified mesh. Subsequently, a standard of care (SOC) mesh and modified mesh were evaluated using a tensometer in an acute hernia bench-top model.
Results
Modified mesh breaking strength, extension knot breaking strength, extension disruption, and extension anchoring were superior to suture (p<0.05). Modified mesh ultimate tensile strength of anchoring was superior to SOC mesh (p<0.05). Various stitch patterns and modifications in device design significantly improved device tension-free performance far beyond clinically relevant benchmarks (p<0.05).
Conclusions
Testing demonstrates that the modified mesh outperforms SOC mesh and suture in all tested failure modes. SOC hernia mesh tears through tissue at stress levels below maximum physiologic stress, whereas, the modified hernia mesh is up to 200% stronger than SOC mesh at resisting suture tearing through tissue and maintains anchoring at stresses far beyond clinically relevant benchmarks. Modifying hernia mesh design significantly improves device mechanical performance and enhances tension-free repair.
Introduction
A hernia is the protrusion of an organ or tissue through a defect in the surrounding walls. Hernias are caused by excessive abdominal tension and occur in 10–30% of patients following laparotomy (Bhangu et al., 2012; Le Huu Nho et al., 2012; Pauli and Rosen, 2013; Sanders and Kingsnorth, 2012; Wechter et al., 2005). Surgeons have two options to perform ventral hernia repair; sutures alone to approximate the fascia or sutures with mesh to approximate the fascia and provide further bolster support. Both approaches aim to counteract tension by distributing forces over a broader surface area and also shifting the forces laterally for a successful hernia repair. In fact, several studies have shown that hernia repair with mesh is significantly better at preventing hernia recurrence than sutures alone. Use of sutures alone to repair hernia results in a hernia recurrence rate of approximately 30–50% (George and Ellis, 1986; Lamont and Ellis, 1988; Luijendijk et al., 2000) and the addition of mesh further reduces recurrence rates to approximately 20% (Fischer and Turner, 1974; George and Ellis, 1986; Hesselink et al., 1993; Korenkov et al., 2002; Luijendijk et al., 2000; Read and Yoder, 1989; Richards et al., 1983).
Since the first use of synthetic meshes in the 1960s, a variety of meshes, were designed with different materials and structures. The textile properties of a mesh determine its biomechanical behavior and affect the mechanical response of the repaired abdominal wall (Todros et al., 2017). Synthetic meshes can be classified into two general categories: non-absorbable and absorbable meshes (Deeken and Matthews, 2013). The advantage of non-absorbable devices is that they permanently anchor tissue. The disadvantage is that they may produce a prolonged foreign body response, cause chronic pain, or at risk for infection over the long term. The advantage of absorbable devices is that most of them are resorbed by 6–18 months (Pierce et al., 2009), while their main disadvantage is that they lose their mechanical properties as they degrade.
Understanding how a hernia mesh performs mechanically to mitigate stress from patient motion or increased intra-abdominal pressure is fundamental to understanding which meshes should be used for hernia repair and how these meshes should be applied. Successful distribution of mechanical stress laterally relates to how well the mesh and the mesh/tissue anchor points perform under tension (Carlson, 1997). The proper fixation of the mesh is important to prevent the recurrence. The number of fixation sites is another important factor. To a certain extent, increasing the number of fixation sites reduces the maximal force per single fixation point. However, as was shown by M. van’t Riet et al, the addition of more than three fixation points per 7 cm of length did not lead to a further increase in bursting strength (van't Riet et al., 2002)
The performance of mesh and the mesh-tissue anchor points relate to deformability and ultimate tensile strength (UTS), where UTS is the maximum amount of stress that a material can absorb prior to failing. A mesh whose deformability matches the abdominal walls’ deformability will perform well (Brown and Finch, 2010; Cobb et al., 2009). The UTS of mesh and the mesh/tissue anchor point need to exceed 16N/cm because this is the maximum amount of force placed on the abdominal wall (clinical benchmark for success) (Brown and Finch, 2010; Deeken et al., 2011; Junge et al., 2001; Klinge et al., 1996; Klinge et al., 1998; Melman et al., 2011). The UTS of moderate and heavy weight meshes exceeds 16N/cm; however, changes at the suture/tissue interface will lead to acute or chronic suture pull-through and surgical failure, which is why coughing or ileus frequently lead to mesh dehiscence and subsequent hernia recurrence, Therefore, mesh hernia repair failure often results from the separation of the mesh–fascia interface; not the mesh failing (Bilsel and Abci, 2012; Brown and Finch, 2010; Lanier et al., 2016). The UTS of mesh/tissue anchor points is determined by patient factors such as obesity, diabetes, smoking, collagen disorders, multiple operations, and steroids and it is also determined by the mesh/tissue anchor point area, since tension (σ)=force (F)/area (A); the larger the anchor point area the smaller the tension experienced by the anchor point (Fischer and Turner, 1974; George and Ellis, 1986; Varghese et al., 2002). The structure of the mesh determines the physicomechanical properties of the device. Rigid structures and stiff materials, for example, will not absorb tension or dissipate force (Brown and Finch, 2010; Cobb et al., 2009). The physical properties of a knitted hernia mesh are characterized as mesh thickness, filament thickness, filament density, and pore size. The mechanical properties are measured by testing ball burst, suture retention, tear resistance, and stress resistance (Brown and Finch, 2010; Cobb et al., 2009; Deeken et al., 2011). To demonstrate the relationship between mesh/tissue anchor point area, tension, and mesh failure, we created a mesh with increased anchor point area.
We compared the performance of a standard of care (SOC) hernia mesh to our modified mesh (Fig. 1) utilizing basic benchtop mechanical testing modalities. We then used a benchtop swine hernia model to investigate the anchor point performance in both the SOC mesh and the modified mesh. Lastly, we studied how varying application methods of the modified mesh affected anchor point performance. In short, our investigation illustrates how modifying mesh design and application significantly improves mesh performance across multiple clinically relevant benchmarks.
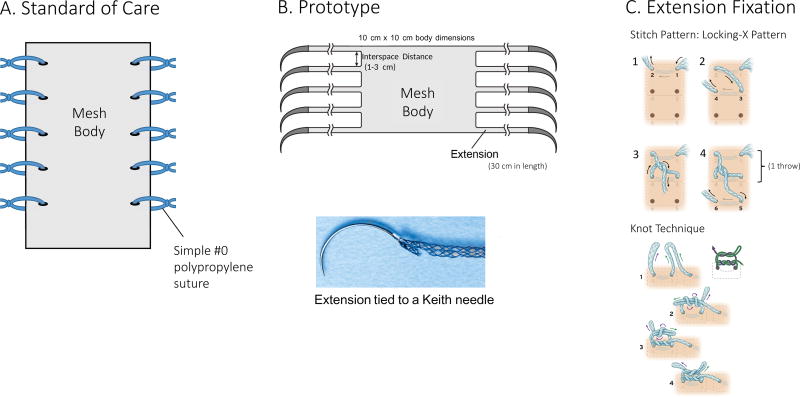
Fig. 1. Mesh Macro Design.
A. Illustration of a standard of care rectangular polypropylene mesh with #0 polypropylene sutures used for anchoring.
B. Illustration of the modified polypropylene mesh with continuous mesh extensions. Extensions are threaded onto a Keith needle eye and secured with #0 silk suture to hold the extensions in place while sewing. This enables sewing of the extensions into tissue akin to how suture is sewn into tissue. Interspace Distance is the distance between each mesh extension measured between adjacent edges. Extension Width and Extension Length is the mesh extension width and length, respectively.
C. Illustration of mesh extension anchoring to tissue. Sequential illustrations demonstrate a locking-x stitch pattern in frames 1 through 4, which is one of many stitch patterns that can be used to anchor the mesh. The mesh extension is then secured by tying a knot analogous to how a surgeon would tie a suture knot.
Methods and Materials
Mechanical properties of suture versus mesh extension anchors
To compare the properties of suture and mesh extension anchors, tensile testing was performed on suture (Surgipro, Covidien, Minneapolis, MN) and prototype mesh extensions according to American Society for Testing and Materials (ASTM) D3822 and ASTM 5035 using a servohydraulic materials testing machine (Model 1321, Instron Corp., Norwood, MA) (ASTM-Standard-D3822; ASTM-Standard-D5035, 2015). Stretch was applied at a rate of 100 mm/min and load versus displacement was recorded at a sampling rate of 100 Hz. Breaking force, knot breaking force, and suture pull out force were quantified (Fig. 2). Details of the testing methods are in the supplementary materials section.
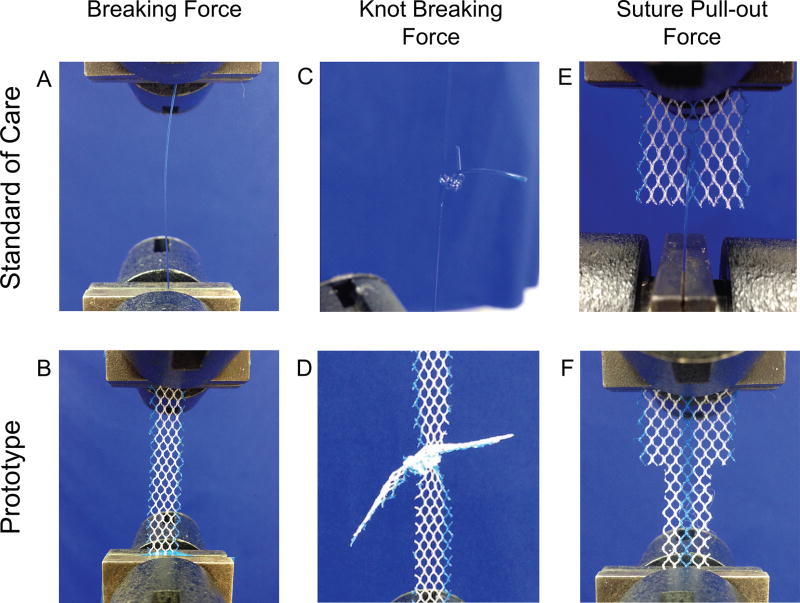
Fig. 2. Mechanical Bench-top Testing Design.
The following figure illustrates (A) Suture breaking strength (B) Mesh extension breaking strength (C) Suture knot breaking strength (D) Mesh extension knot breaking strength (E) Suture-mesh pull-out strength and (F) Mesh extension-mesh pull-out strength
Swine abdominal wall bench-top model
Each mesh anchoring modality was then evaluated in a swine abdominal wall model (Feng and Jasiuk, 2010). Details of the testing methods are in the supplementary materials section.
Standard of care: Hernia mesh anchored with simple interrupted polypropylene sutures (n= 6 per group)
To measure the effectiveness of the SOC suture anchoring mesh, a 5.5 cm × 10 cm rectangular mesh was secured to a hemi-dumbbell fascia-muscle slab with three simple interrupted sutures (Fig. 3A). The sutures were placed at 1 cm intervals through the fascial layer (5 mm deep) and secured with a surgeon’s knot and four square knots.
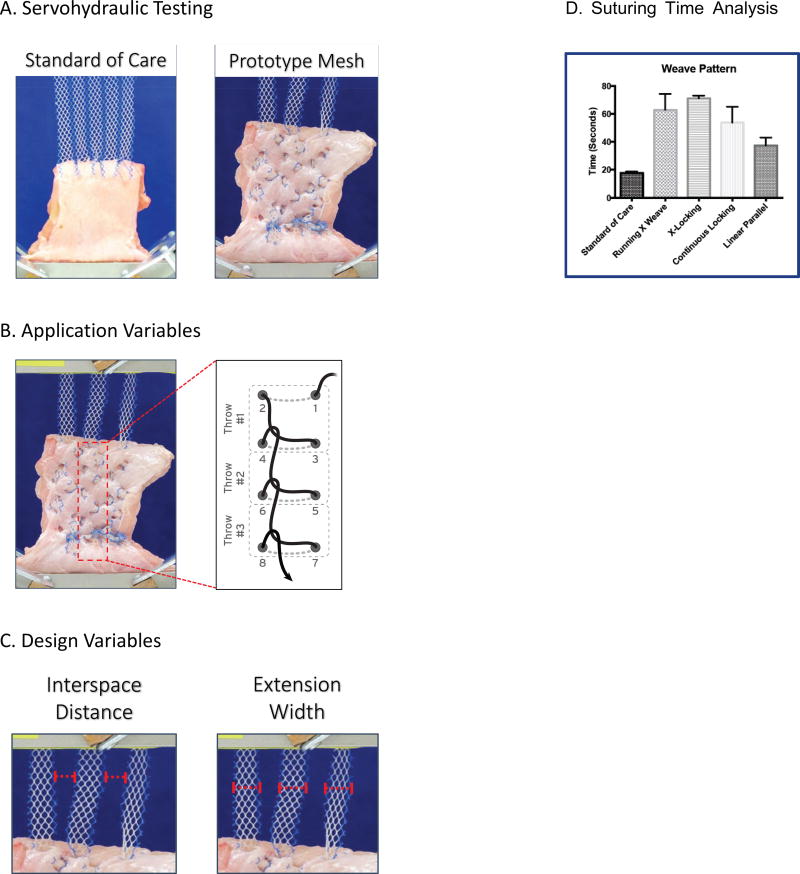
Fig. 3. Swine Abdominal Wall Bench-top Model.
A. Servohydaulic testing. Standard of care (left) and modified hernia mesh (right) anchored with mesh extensions
B. Application Variables. Stitch pattern and throw count
C. Design Variables. Interspace distance and extension width
D. Analysis of time required to achieve different suturing patterns. As can be noted, a standard of care stitch is faster to place than any of the various consecutive suturing patterns.
Modified hernia mesh anchored with mesh extensions
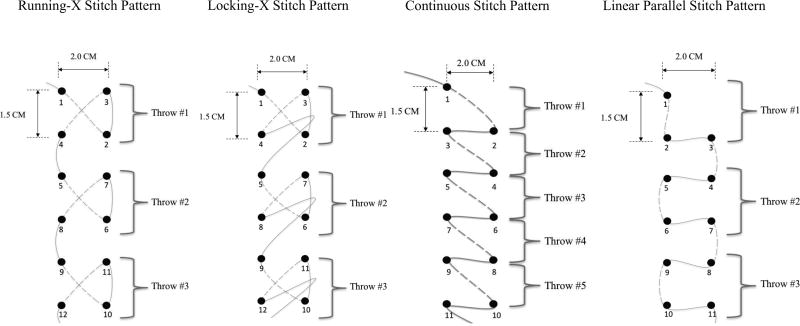
The modified hernia mesh was designed by cutting an Ultrapro Monocryl-Prolene Composite Mesh (Ethicon, Inc. Somerville, NJ) with scissors such that three extensions emanated from the body of the mesh on the lateral aspects (Fig. 1B) to assess the performance of integral mesh extensions on anchoring hernia mesh. Extensions were not placed cephalad caudal because hernia forces are from medial to lateral and not from medial to cephalad or medial to caudal because of the rib cage and pelvis. The Ultrapro Monocryl-Prolene Composite Mesh does not unravel when cut so it is appropriate for testing purposes. Each mesh extension was loaded onto a curved Keith needle (Richard Allan Scientific Company, Kalamazoo, MI) by threading the extension through the eye of the needle and then using a silk suture to tie the extension to the needle (Fig. 1B). The mesh extensions were then sewn into the fascia layers varying stitch pattern and throw count between experiments (Fig. 3A–3B). The stitch pattern, throw count, interspace distance between the extensions and extension widths were then varied as described in the supplementary materials section (Fig. 1B).
Elastic Modulus
described in the supplementary materials section
Statistical Analysis
Mean and standard deviation of observations were reported. Comparisons between the groups were assessed through Wilcoxon-Mann-Whitney test (WMW). The threshold for declaring statistical significance was set to α = 0.05. All statistical analyses were performed with R statistical software (Team, 2015).
Results
Mechanical properties of suture and mesh extensions
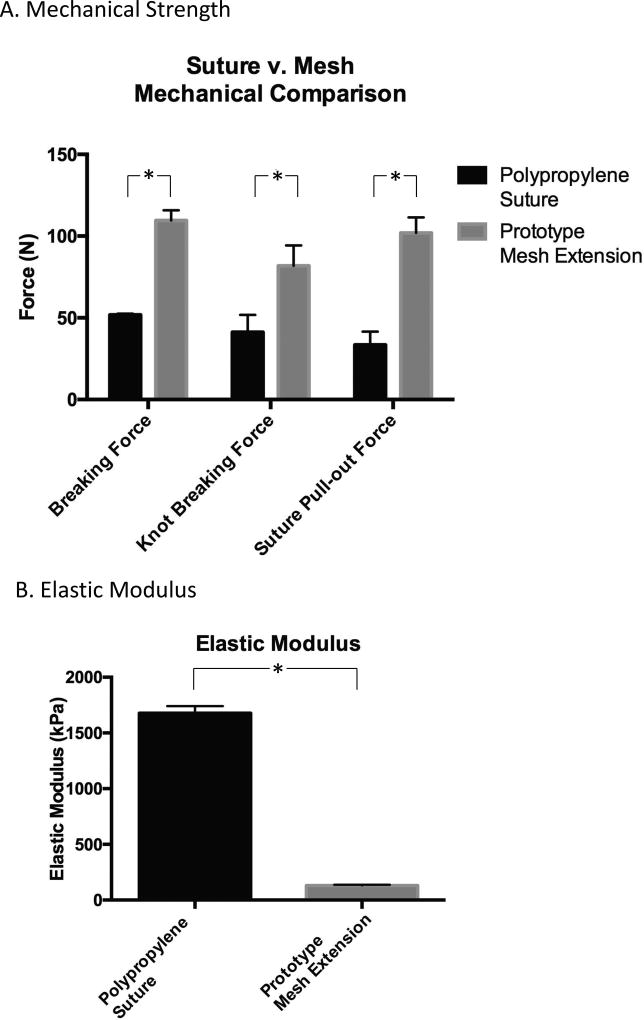
Breaking force
(Fig. 5A) The suture had a mean breaking force of 51.8 ± 0.7 N (n=10), while the composite mesh extension had a mean breaking force of 109.5 ± 6.3 N (n=10), indicating the mesh extension was two-fold stronger than suture (WMW-test, p<0.001). The polypropylene suture had a mean elastic modulus of 1677 ± 64.2 kPa (n=10), while the composite mesh had a mean elastic modulus of 131 ± 5.8 kPa (n=10), indicating the mesh extension can deform to a greater extent and mitigate stress when exposed to applied force more than suture (WMW-test, p<0.0001) (Fig. 5B).
Fig. 5. Basic Mechanical Testing Results.
A. Bar graph of suture and mesh extension mechanical testing of breaking force, knot breaking force, and suture-pull out force. The mesh extension was significantly stronger with regards to breaking force, knot breaking force, and suture pull-out force (*p<0.05).
B. Bar graph of the elastic modulus (kPa) of the polypropylene suture versus the prototype mesh extension. The suture had a higher elastic modulus than the mesh extension (*p<0.05), meaning the suture was stiffer than the mesh extension.
Knot breaking force
(Fig. 5A) The suture knot had a mean breaking force of 41.6 ± 10.6 N (n=10), while the composite mesh extension knot had a mean breaking force of 81.8 ± 12.5 N (n=10), indicating the mesh extension knot was nearly two fold stronger than suture (WMW-test, p<0.0001). At failure, both the suture and the mesh extension fractured directly adjacent to the knot. The surgeon knot never unraveled.
Suture pull-out force
(Fig. 5A) The mean force required to pull a suture through the mesh was 33.4 ± 8.1 N (n=10), while the mean force required to detach a continuous mesh extension from the mesh was 101.9 ± 9.5 N (n=10), indicating the mesh extension requires 300% more force to pull-out from the mesh (WMW-test, p<0.0001).
Swine abdominal wall bench-top model
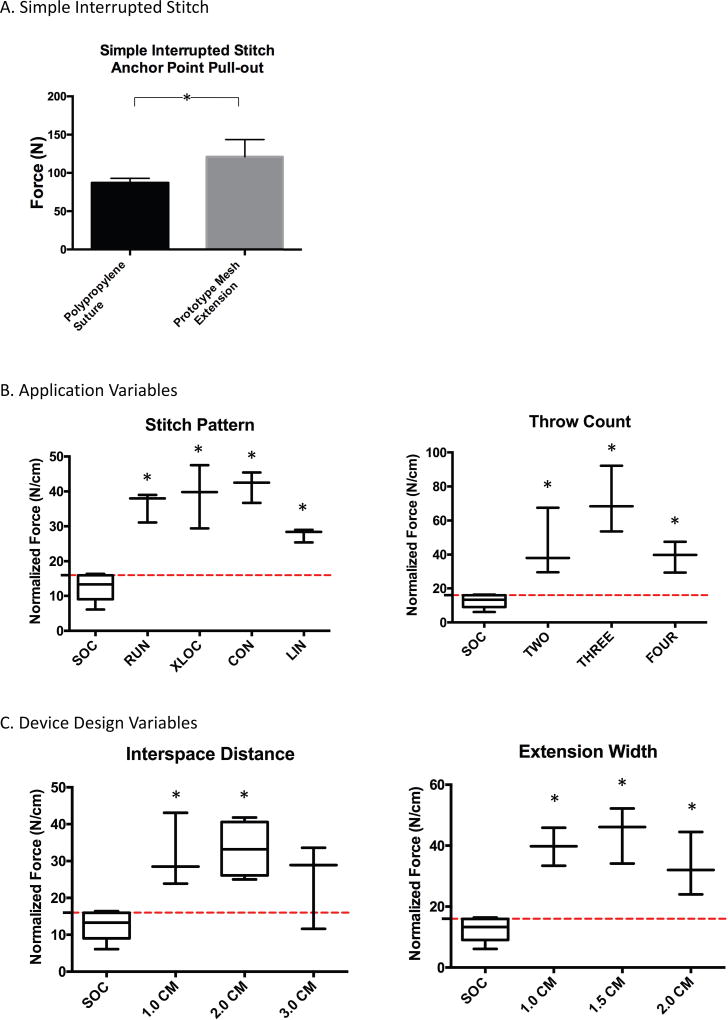
Simple interrupted stitch anchor point pull-out
The suture anchor point (Fig. 6A) had a pull-out force of 87.13 N ± 5.8 (n=4), while the composite mesh extension anchor point had a pull-out force of 121.1 N ± 22.5 (n=4), indicating that the mesh extension is 50% stronger than suture (WMW-test, p=0.0286).
Fig. 6. Application and Design Tensile Strength Results.
A. Bar graph of the force required to disrupt suture or mesh from pig abdominal wall using a single simple interrupted stitch. The mesh extension had a 50% high pull-out force in comparison to suture (*p<0.05).
B. Boxplot of the normalized breaking force (N/cm) of device application variables: stitch pattern and throw count. The RUN, XLOC, CON, and LIN suture patterns all had significantly higher normalized breaking forces than suture (*p<0.05). The TWO, THREE, and FOUR throw counts all significantly outperformed the suture (*p<0.05). Mean and standard deviation of observations were reported.
C. Boxplot of the normalized breaking force (N/cm) of device design variables: interspace distance and arm width. The 1 cm and 2 cm interspace distances significantly outperformed suture (*p<0.05). The 3 cm interspace was not statistically different from the suture. The 1 cm, 1.5 cm, and 2 cm mesh extension widths significantly outperformed suture (*p<0.05). The red line indicates the maximum intra-abdominal force (16 N/cm2) a human can generate. Mean and standard deviation of observations were reported.
SOC Mesh anchoring
Hernia mesh was anchored with simple interrupted polypropylene sutures (Fig. 6B). The mesh anchored with suture had a normalized breaking force of 12.7 ± 4.1 N/cm (n=5); consistently below the commonly reported 16 N/cm benchmark. We report 16 N/cm because we seek to frame the clinical relevance of the study in relation to a relevant clinical standard benchmark for necessary anchoring performance between suture, mesh, and tissue to overcome intra-abdominal pressures that causes hernia. The proposed mesh is not necessarily meant to have better mesh mechanics such as suture retention, ball burst, tensile stress, etc. so these tests were not performed.
Hernia mesh anchored with mesh extensions
Stitch pattern
The RUN, XLOC, CON, and LIN suture patterns from Fig. 4 had mean normalized breaking forces of 36.0 ± 4.3 N/cm, 38.1 ± 9.1 N/cm, 41.5 ± 4.4 N/cm, and 27.6 ± 1.9 N/cm, respectively (n=3) (Fig. 6B). The RUN, XLOC, CON, and LIN suture patterns all had significantly higher normalized breaking forces than suture (WMW-test: p=0.00178 for all comparisons).
Fig. 4. Device Application Variables.
A basic schematic of four stitch patterns: the running-x stitch pattern (RUN), the locking-x stitch pattern (XLOC), the continuous stitch pattern (CON), and the linear parallel stitch pattern (LIN). The numbered points represent the order in which the suture needle enters and exits the tissue. Dashed lines represent suture lying below fascia; solid lines represent suture lying above fascia. A ‘throw’ is a repetition of a complete the stitch pattern.
Throw count
Two throws, three throws, and four throws had normalized breaking forces of 45.0 ± 19.9 N/cm, 71.4 ± 19.5 N/cm, and 38.1 ± 9.1 N/cm, respectively (n=3) (Fig. 6B). The TWO, THREE, and FOUR stitch counts all significantly outperformed the suture (WMW-test: p=0.0178 for all comparisons).
Interspace distance
The 1 cm, 2 cm, and 3 cm interspaces had normalized breaking forces of 31.8 ± 10.0 N/cm, 33.3 ± 8.7 N/cm, and 24.7 ± 11.6 N/cm, respectively (n=3) (Fig. 6C). The 1 cm and 2 cm interspace distances significantly outperformed suture (WMW-test: p=0.0178 and p=0.0079, respectively). The 3 cm interspace was not statistically different from the suture (WMW-test, p=0.196).
Extension width
The 1 cm, 1.5 cm, and 2.0 cm arm wide extensions had normalized breaking forces of 39.7 ± 6.3 N/cm, 44.1 ± 9.2 N/cm, and 33.5 ± 10.3 N/cm, respectively (n=3) (Fig. 6C). The 1 cm, 1.5 cm, and 2 cm mesh extension widths significantly outperformed suture (WMW-test: p=0.0178 for all comparisons). The 2 cm extension was noted to create holes in the tissue and to curl upon itself.
Suturing time analysis
The standard of care suture takes ~20 sec to perform, the RUN weave takes ~60 sec to perform, the XLOC pattern takes ~70 sec to perform, and the CON takes ~52 sec to perform, and the LIN takes ~38 sec to perform (Fig 3B).
Discussion
For a hernia repair to be successful, the undeformed mesh and mesh/tissue anchor points need to overcome four common failure modes: suture breaking, suture knot unraveling, suture pulling through mesh, and suture tearing through tissue at 16N/cm2 of stress. Several products have been used in recent years to provide better fixation and overcome the failure modes of the sutures, including metallic tacks, absorbable tacks, and fibrin sealants. However, studies have demonstrated that suture is greater than these fixation methods (Melman et al., 2010).
To demonstrate how modifying mesh design leads to improved device performance, a modified hernia mesh was created and tensile testing completed. Because the modified mesh contained elements of a suture and mesh in one device, the physico-mechanical properties of the modified hernia mesh were compared to SOC suture and mesh using ASTM standards. We then utilized a swine hernia benchtop model to illustrate how the anchor points of the modified mesh perform compared to a standard mesh secured with suture. For the purposes of this study, we attached a Keith needle to the mesh extensions manually. This labor intensive, time-consuming technique of provisionally attaching each individual extension to an individual needle was used so that we could sew the mesh extensions into the tissue to test the performance of the mesh. From a commercial perspective, this approach would not be used by instead needles would need to be secured to the mesh extensions by a manufacturing process that involves machining and crimping through specialized dies and specialized needles. The complex needle swaging approach is beyond the scope of this paper.
First, uniaxial static tensile testing was conducted to compare the device breaking strength of a mesh extension versus a suture. Mesh extension had a significantly higher breaking strength and significantly lower elastic modulus in comparison to suture. We attribute these observations to the larger load bearing area of the knitted extension compared to the solid fiber polypropylene suture and the extensions greater deformability. Even though an appropriate mechanical match to the tissue is important, the elastic modulus results demonstrate that the mesh extension can deform to a greater extent and mitigate stress better when exposed to applied force more than suture. From a clinical perspective, the lower elastic modulus of an extension compared to a suture indicates that an extension will not generate high shear forces but will accommodate a greater degree of deformation and dissipate stress before cutting through tissue. We have chosen to report elastic modulus in this study, as opposed to stiffness, because it has been previously reported that the elastic modulus of a mesh contributes to the efficacy of a repair in some capacity and we wanted the elastic modulus data to be comparable.(Saberski et al., 2011)
Next, uniaxial tensile testing was performed to determine the force required to unravel an extension knot versus a suture knot. We found the mesh extension knot and polypropylene suture knot never unraveled but instead both always failed adjacent to the knot. The friction of the knot exceeded the UTS of the suture and extension and the extension failed at nearly double the force of the suture. Hence, knot unraveling is unlikely to contribute to device failure.
Last, we performed a suture pull-out test to evaluate the force required to pull a suture through a standard mesh versus the force required to dismember a mesh extension from the mesh body. Uniaxial static tensile testing revealed that a mesh extension is approximately 200% stronger than a suture placed through mesh. As such, a continuous mesh extension would likely never tear away from the mesh body in humans.
Having completed basic benchtop mechanical testing, we proceeded to examine the forces required to disrupt mesh-tissue anchor points. We observed that a simple interrupted extension stitch anchor point withstands approximately 50% more stress than a simple interrupted suture anchor point. We attribute this finding to increased extension deformability and increased extension surface area. To further define how distribution of force over a large surface area enhances anchor point performance, we modified extension stitch pattern and throw count reasoning that these anchoring approaches would significantly improve performance based on textile literature (Karahan et al., 2010; Karahan et al., 2013; Mouritz et al., 1997). We found that all stitch patterns had significantly higher UTS compared to control suture and all significantly exceeded the clinically relevant benchmark of 16 N/cm. Suture failed at 12N/cm. The two main failure modes of the mesh extensions were serial stitch breakdown and tissue tearing distal to the anchor knot both of which were attributed to model failure at supra-physiologic stresses. Because of model failure, we could not determine which stitch pattern performed best but we conclude that since all patterns exceeded 16N/cm the differences between stitch pattern performance is not critical. We found that 2, 3, or 4 throws all had UTS above the 16 N/cm threshold and there was no significant difference between throw counts. We speculate that the similar performance of 2, 3, and 4 throws may be attributable to the fact that 2 throws is sufficient to distribute force adequately and that subsequent throws carry less load until throws far very away carry no load. Last, we focused on how extension interspace distance and extension width would impact performance. We found that the 1.0 cm and 2.0 cm interspaces were significantly stronger than suture, whereas the 3.0 cm interspace was not stronger than suture indicating there is a minimum density of extensions necessary to secure the mesh to tissue for improved anchoring. As for extension width, we found that all widths performed above the 16 N/cm threshold.
The hernia literature is replete with studies describing the performance of hernia meshes in animal models and humans, and there are many studies and reviews that discuss the importance of limiting mechanical tension for successful repair (Amato et al., 2011; Cobb et al., 2006; Dumanian et al., 2015; Gonzalez et al., 2005; Luijendijk et al., 2000; Melman et al., 2011). However, few hernia studies consider how modifying device design and application mitigate tensile stress in a meaningful clinical way. Recently, Dumanian et al. demonstrated that a mesh suture significantly reduces hernia defect size compared with conventional suture and that mesh suture is less likely than suture to pull through surrounding tissue (Souza et al., 2015). In follow-up studies, he noted the mesh suture anchor point was about 100% stronger at resisting tensile stress and the mesh suture significantly outperformed suture in a live swine hernia model (Dumanian et al., 2015).
The modified hernia mesh was designed by cutting an Ultrapro Monocryl-Prolene Composite Mesh into desired configurations for testing. This is the same hernia mesh the Dumanian group modified for in vitro and in vivo testing, as well as clinical studies of their modified mesh sutures (Dumanian et al., 2015; Lanier et al., 2016; Souza et al., 2015). Due to the knitted design, the mesh does not unravel when cut, unlike several other hernia meshes on the market. The extensions are on the lateral aspects of the mesh but not the cephalad or caudal aspects. This design was created so that the lateral extensions would counteract the prevailing medial-lateral forces that cause hernia. From a physiologic perspective, there are minimal forces that act cephalad and caudal to create a hernia (because of the abdominal wall muscular anatomy and rib cage and pelvis). We do not recommend cutting an Ultrapro Monocryl-Prolene Composite Mesh in an operating room and implanting a cut mesh into humans for several reasons. First, cutting the mesh to our design leads to mesh integrity compromise and potential mesh extension weakness. This mesh was not fabricated to support mesh extension strength. Second, cutting a mesh causes fraying of the edges which can cause tissue micro-trauma and damage tissue. To achieve a clinically applicable modified hernia mesh of the same design, a new mesh will need to be developed. Cutting a pre-existing mesh with a scissor or other cutting tool would seriously affect mesh integrity leading to frayed ends and potential mesh unraveling. This could likely affect device performance and patient safety and would be non-compliant with FDA approval. To develop a commercially available mesh that matches the described configuration, one would need to knit a novel mesh with continuous seamless extensions.
Certainly, a common question is which anatomic layer to place such a modified hernia mesh. While there are multiple locations the mesh could be placed, we did not analyze mesh performance according to anatomic location. Hence, we cannot comment on where to place the mesh. Perhaps future mechanistic studies could be performed to answer this question.
There are a few limitations to our study. First, we were unable to evaluate how tension was distributed across each stitch pattern. The distribution of tensile stress is difficult to measure in heterogeneous tissue. Finite element simulation and analysis may help to achieve this goal in the future, through modeling the mechanical behavior of the abdominal wall before and after implantation of both mesh types. (Hernandez-Gascon et al., 2011; Pachera et al., 2016). Another weakness is that we only tested three different extension arm widths and three different interspace distances. Our studies could have been more detailed to inform future device design. Lastly, we did not test the effects of cyclic stress or torsion stress on device performance. These stresses are commonly encountered from patient twisting and repeated bouts of coughing or straining and could be important to measure. Cyclic strain leads to micro tears which may summate to affect device performance. Another limitation which is related to the benchtop model we have used, is that we could not evaluate the foreign body response, the biologic tissue reaction to acute injury, nor chronic adverse reactions.
In conclusion, we have observed that mesh modification leads to improved mechanical performance. Similar to previous reports of a mesh suture that has improved anchoring strength, the prototype mesh functions by similar mechanisms and is a significant improvement over standard of care mesh. Mesh extensions are up to 200% stronger than suture at resisting mesh/tissue anchor point dehiscence. The prototype mesh distributes tensile stress and keeps the tensile stress below the UTS of the device/tissue anchor point. In all testing, the UTS of the prototype device far exceeded benchmarks necessary for clinical success. We are currently working with a medical textile manufacturer to knit a mesh that meets the physical properties discussed herein and this mesh will be tested for safety and performance, but this effort is beyond the scope of this investigation and will be reported in a later manuscript. Future studies will include ongoing device development and performance evaluations in living swine hernia models.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR001117. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work was also supported by a grant from MedBlue. We would like to acknowledge Bruce Klitzman, PhD and Beth Lorden, PhD for reviewing the manuscript and Neese’s Country Sausage for donating whole porcine abdominal wall for our bench-top studies.
H.L. reports grants from MedBlue during the conduct of the study; other support from Deep Blue Medical Advances outside the submitted work. In addition, H.L. has a patent for “Implantable Mesh and Methods of Use” pending.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presentations:
Data from this manuscript was accepted and presented at the Plastic Surgery Research Council Annual Meeting on May 21, 2016 in New York City, NY. The title of the presentation was, “Development of a Suture-less Hernia Mesh with Enhanced Anchoring Strength.”
AUTHOR ROLES
Contribution: M.I, L.P. and H.L. designed experiments and interpreted data; L.P., R.G., A.C., and M.I. performed experiments; L.P. and A.F. performed statistical analysis, K.G. reviewed and interpreted data; M.I, L.P. and H.L. wrote the manuscript. M.I. revised the manuscript. All authors reviewed the manuscript. All authors were fully involved in the study and preparation of the manuscript. The material within has not been and will not be submitted for publication elsewhere.
FINANCIAL DISCLOSURE AND PRODUCTS PAGE
Howard Levinson, MD and Duke University have patented the tested device. Dr. Levinson has created a company to advance the product towards commercialization. The remaining authors have no financial interests to disclose.
- 0 Polypropylene Suture (Surgipro, Covidien, Minneapolis, MN)
- ULTRAPRO Monocryl-Prolene Composite Mesh (Ethicon, Inc., Somerville, NJ)
- Curved Keith Needle. Style Size: Mayo ½ Taper (Richard Allan Scientific Company, Kalamazoo, MI)
Conflict of Interest Statement
M.M.I. has nothing to disclose.
L.P.P. has nothing to disclose.
R.R.G. has nothing to disclose.
A.C. has nothing to disclose.
A.E.F. has nothing to disclose.
K.G. has nothing to disclose.
Ethical Standards
All experiments comply with the current laws of the United States. This article does not contain any studies with human participants or animals performed by any of the authors.
References
- Amato G, Lo Monte AI, Cassata G, Damiano G, Romano G, Bussani R. A new prosthetic implant for inguinal hernia repair: its features in a porcine experimental model. Artificial organs. 2011;35:E181–190. doi: 10.1111/j.1525-1594.2011.01272.x. [DOI] [PubMed] [Google Scholar]
- ASTM-Standard-D3822. Standard Test Method for Tensile Properties of Single Textile Fibers. ASTM International; West Conshohocken, PA: [Google Scholar]
- ASTM-Standard-D5035. Standard Test Method for Breaking Force and Elongation of Textile Fabrics (Strip Method) ASTM International; West Conshohocken, PA: 2015. [Google Scholar]
- Bhangu A, Nepogodiev D, Futaba K, West Midlands Research C. Systematic review and meta-analysis of the incidence of incisional hernia at the site of stoma closure. World journal of surgery. 2012;36:973–983. doi: 10.1007/s00268-012-1474-7. [DOI] [PubMed] [Google Scholar]
- Bilsel Y, Abci I. The search for ideal hernia repair; mesh materials and types. International journal of surgery. 2012;10:317–321. doi: 10.1016/j.ijsu.2012.05.002. [DOI] [PubMed] [Google Scholar]
- Brown CN, Finch JG. Which mesh for hernia repair? Annals of the Royal College of Surgeons of England. 2010;92:272–278. doi: 10.1308/003588410X12664192076296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson MA. ACUTE WOUND FAILURE. Surgical Clinics of North America. 1997;77:607–636. doi: 10.1016/s0039-6109(05)70571-5. [DOI] [PubMed] [Google Scholar]
- Cobb WS, Burns JM, Peindl RD, Carbonell AM, Matthews BD, Kercher KW, Heniford BT. Textile analysis of heavy weight, mid-weight, and light weight polypropylene mesh in a porcine ventral hernia model. The Journal of surgical research. 2006;136:1–7. doi: 10.1016/j.jss.2006.05.022. [DOI] [PubMed] [Google Scholar]
- Cobb WS, Peindl RM, Zerey M, Carbonell AM, Heniford BT. Mesh terminology 101. Hernia. 2009;13:1–6. doi: 10.1007/s10029-008-0428-3. [DOI] [PubMed] [Google Scholar]
- Deeken CR, Abdo MS, Frisella MM, Matthews BD. Physicomechanical evaluation of polypropylene, polyester, and polytetrafluoroethylene meshes for inguinal hernia repair. Journal of the American College of Surgeons. 2011;212:68–79. doi: 10.1016/j.jamcollsurg.2010.09.012. [DOI] [PubMed] [Google Scholar]
- Deeken CR, Matthews BD. Ventralight ST and SorbaFix versus Physiomesh and Securestrap in a porcine model. JSLS : Journal of the Society of Laparoendoscopic Surgeons. 2013;17:549–559. doi: 10.4293/108680813X13693422520125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumanian GA, Tulaimat A, Dumanian ZP. Experimental study of the characteristics of a novel mesh suture. The British journal of surgery. 2015;102:1285–1292. doi: 10.1002/bjs.9853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng L, Jasiuk I. Effect of specimen geometry on tensile strength of cortical bone. Journal of biomedical materials research. Part A. 2010;95:580–587. doi: 10.1002/jbm.a.32837. [DOI] [PubMed] [Google Scholar]
- Fischer JD, Turner FW. Abdominal incisional hernias: a ten-year review. Canadian journal of surgery. Journal canadien de chirurgie. 1974;17:202–204. [PubMed] [Google Scholar]
- George CD, Ellis H. The results of incisional hernia repair: a twelve year review. Ann R Coll Surg Engl. 1986;68:185–187. [PMC free article] [PubMed] [Google Scholar]
- Gonzalez R, Fugate K, McClusky D, 3rd, Ritter EM, Lederman A, Dillehay D, Smith CD, Ramshaw BJ. Relationship between tissue ingrowth and mesh contraction. World journal of surgery. 2005;29:1038–1043. doi: 10.1007/s00268-005-7786-0. [DOI] [PubMed] [Google Scholar]
- Hernandez-Gascon B, Pena E, Melero H, Pascual G, Doblare M, Ginebra MP, Bellon JM, Calvo B. Mechanical behaviour of synthetic surgical meshes: finite element simulation of the herniated abdominal wall. Acta biomaterialia. 2011;7:3905–3913. doi: 10.1016/j.actbio.2011.06.033. [DOI] [PubMed] [Google Scholar]
- Hesselink VJ, Luijendijk RW, de Wilt JH, Heide R, Jeekel J. An evaluation of risk factors in incisional hernia recurrence. Surgery, gynecology & obstetrics. 1993;176:228–234. [PubMed] [Google Scholar]
- Junge K, Klinge U, Prescher A, Giboni P, Niewiera M, Schumpelick V. Elasticity of the anterior abdominal wall and impact for reparation of incisional hernias using mesh implants. Hernia. 2001;5:113–118. doi: 10.1007/s100290100019. [DOI] [PubMed] [Google Scholar]
- Karahan M, Karahan N, Ulcay Y, Eren R, Kaynak G. Investigation into the Tensile Properties of Stitched and Unstitched Woven Aramid/Vinyl Ester Composites. Textile Research Journal. 2010;80:880–891. [Google Scholar]
- Karahan M, Ulcay Y, Karahan N, Kus A. Influence of Stitching Parameters on Tensile Strength of Aramid/Vinyl Ester Composites. Materials Science-Medziagotyra. 2013;19:67–72. [Google Scholar]
- Klinge U, Conze J, Limberg W, Brucker C, Ottinger AP, Schumpelick V. [Pathophysiology of the abdominal wall] Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen. 1996;67:229–233. [PubMed] [Google Scholar]
- Klinge U, Klosterhalfen B, Conze J, Limberg W, Obolenski B, Ottinger AP, Schumpelick V. Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg. 1998;164:951–960. doi: 10.1080/110241598750005138. [DOI] [PubMed] [Google Scholar]
- Korenkov M, Sauerland S, Arndt M, Bograd L, Neugebauer EA, Troidl H. Randomized clinical trial of suture repair, polypropylene mesh or autodermal hernioplasty for incisional hernia. The British journal of surgery. 2002;89:50–56. doi: 10.1046/j.0007-1323.2001.01974.x. [DOI] [PubMed] [Google Scholar]
- Lamont PM, Ellis H. Incisional hernia in re-opened abdominal incisions: an overlooked risk factor. The British journal of surgery. 1988;75:374–376. doi: 10.1002/bjs.1800750426. [DOI] [PubMed] [Google Scholar]
- Lanier ST, Dumanian GA, Jordan SW, Miller KR, Ali NA, Stock SR. Mesh Sutured Repairs of Abdominal Wall Defects. Plastic and reconstructive surgery. Global open. 2016;4:e1060. doi: 10.1097/GOX.0000000000001060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Huu Nho R, Mege D, Ouaissi M, Sielezneff I, Sastre B. Incidence and prevention of ventral incisional hernia. Journal of visceral surgery. 2012;149:e3–14. doi: 10.1016/j.jviscsurg.2012.05.004. [DOI] [PubMed] [Google Scholar]
- Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, JN IJ, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel J. A comparison of suture repair with mesh repair for incisional hernia. The New England journal of medicine. 2000;343:392–398. doi: 10.1056/NEJM200008103430603. [DOI] [PubMed] [Google Scholar]
- Melman L, Jenkins ED, Deeken CR, Brodt MD, Brown SR, Brunt LM, Eagon JC, Frisella M, Matthews BD. Evaluation of acute fixation strength for mechanical tacking devices and fibrin sealant versus polypropylene suture for laparoscopic ventral hernia repair. Surgical innovation. 2010;17:285–290. doi: 10.1177/1553350610379427. [DOI] [PubMed] [Google Scholar]
- Melman L, Jenkins ED, Hamilton NA, Bender LC, Brodt MD, Deeken CR, Greco SC, Frisella MM, Matthews BD. Histologic and biomechanical evaluation of a novel macroporous polytetrafluoroethylene knit mesh compared to lightweight and heavyweight polypropylene mesh in a porcine model of ventral incisional hernia repair. Hernia. 2011;15:423–431. doi: 10.1007/s10029-011-0787-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouritz AP, Leong KH, Herszberg I. A review of the effect of stitching on the in-plane mechanical properties of fibre-reinforced polymer composites. Composites Part A: Applied Science and Manufacturing. 1997;28:979–991. [Google Scholar]
- Pachera P, Pavan PG, Todros S, Cavinato C, Fontanella CG, Natali AN. A numerical investigation of the healthy abdominal wall structures. Journal of biomechanics. 2016;49:1818–1823. doi: 10.1016/j.jbiomech.2016.04.019. [DOI] [PubMed] [Google Scholar]
- Pauli EM, Rosen MJ. Open ventral hernia repair with component separation. The Surgical clinics of North America. 2013;93:1111–1133. doi: 10.1016/j.suc.2013.06.010. [DOI] [PubMed] [Google Scholar]
- Pierce RA, Perrone JM, Nimeri A, Sexton JA, Walcutt J, Frisella MM, Matthews BD. 120-day comparative analysis of adhesion grade and quantity, mesh contraction, and tissue response to a novel omega-3 fatty acid bioabsorbable barrier macroporous mesh after intraperitoneal placement. Surgical innovation. 2009;16:46–54. doi: 10.1177/1553350608330479. [DOI] [PubMed] [Google Scholar]
- Read RC, Yoder G. Recent trends in the management of incisional herniation. Archives of surgery (Chicago, Ill. 1960) 1989;124:485–488. doi: 10.1001/archsurg.1989.01410040095022. [DOI] [PubMed] [Google Scholar]
- Richards PC, Balch CM, Aldrete JS. Abdominal wound closure. A randomized prospective study of 571 patients comparing continuous vs. interrupted suture techniques. Annals of surgery. 1983;197:238–243. doi: 10.1097/00000658-198302000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders DL, Kingsnorth AN. The modern management of incisional hernias. BMJ (Clinical research ed.) 2012;344:e2843. doi: 10.1136/bmj.e2843. [DOI] [PubMed] [Google Scholar]
- Souza JM, Dumanian ZP, Gurjala AN, Dumanian GA. In vivo evaluation of a novel mesh suture design for abdominal wall closure. Plastic and reconstructive surgery. 2015;135:322e–330e. doi: 10.1097/PRS.0000000000000910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Team, R.C. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2015. [Google Scholar]
- Todros S, Pavan PG, Pachera P, Natali AN. Synthetic surgical meshes used in abdominal wall surgery: Part II-Biomechanical aspects. Journal of biomedical materials research. Part B: Applied biomaterials. 2017;105:892–903. doi: 10.1002/jbm.b.33584. [DOI] [PubMed] [Google Scholar]
- van't Riet M, de Vos van Steenwijk PJ, Kleinrensink GJ, Steyerberg EW, Bonjer HJ. Tensile strength of mesh fixation methods in laparoscopic incisional hernia repair. Surgical endoscopy. 2002;16:1713–1716. doi: 10.1007/s00464-001-9202-7. [DOI] [PubMed] [Google Scholar]
- Varghese TK, Denham DW, Dawes LG, Murayama KM, Prystowsky JB, Joehl RJ. Laparoscopic ventral hernia repair: an initial institutional experience. The Journal of surgical research. 2002;105:115–118. doi: 10.1006/jsre.2002.6383. [DOI] [PubMed] [Google Scholar]
- Wechter ME, Pearlman MD, Hartmann KE. Reclosure of the disrupted laparotomy wound: a systematic review. Obstetrics and gynecology. 2005;106:376–383. doi: 10.1097/01.AOG.0000171114.75338.06. [DOI] [PubMed] [Google Scholar]
- Saberski ER, Orenstein SB, Novitsky YW. Anisotropic evaluation of synthetic surgical meshes. Hernia : the journal of hernias and abdominal wall surgery. 2011;15:47–52. doi: 10.1007/s10029-010-0731-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.