Abstract
Aims and Objectives
The aim of the study is to retrospectively analyse the incidence of facial fractures along with age, gender predilection, etiology, commonest site, associated dental injuries and any complications of paediatric patients operated in Craniofacial unit of SDM college of dental sciences and hospital.
Materials and Methods
This retrospective study was conducted at the department of OMFS, SDM College of Dental Sciences, Dharwad from January 2003–December 2013. All the patients below 15 years of age were included in the study. Data were recorded for the cause of injury, age and gender distribution, frequency and type of injury, localization and frequency of soft tissue injuries, dentoalveolar trauma, facial bone fractures, complications, concomitant injuries and different treatment protocols.
Results
A total of 68 cases of paediatric fracture were treated during these 10 years. Boys were commonly injured than girls with a ratio of 2.9:1, the commonest cause of trauma was fall (59 %), mandible was the commonest bone to be fractured (83 %), treatment protocols were dependant on the age, region and type of fracture but in most of the cases closed reduction was the choice of treatment, dental injuries were seen in 26 % patients and the commonest injury was avulsion.
Conclusion
This study was done not only to analyse the different types of facial fractures and the pattern of fracture of paediatric cases admitted at this centre, but also to act as a contributional data which will help us to take preventive measures to avoid such injuries and make the appropriate treatment plan and execute it to achieve the pre-injury status of form and function.
Electronic supplementary material
The online version of this article (doi:10.1007/s12663-016-0965-8) contains supplementary material, which is available to authorized users.
Keywords: Pediatric, Maxillofacial, Trauma, Dental injuries
Introduction
Incidence of paediatric trauma is less compared to adults but due to a significant difference in facial anatomy of children they require a mention as a special group of patients in maxillofacial surgery. Depending on the age, these differences include small size of the bones, small volume of the paranasal sinuses, growth potential, presence of tooth germs in the jaws during the primary and the mixed dentition, a quicker healing process, as well as difficulty in cooperation and the need for general anaesthesia in more cases than adults [1]. In a study done by Rowe of 1500 facial fractures, children younger than 12 years of age sustained fewer than 5 % of all injuries, and children younger than 6 years, fewer than 1 % [2]. As a result, experience of individual physician with paediatric patients is limited, so it is useful to examine the experience of a surgical team at a large trauma centre where reported cases of paediatric trauma is more and where current craniofacial techniques to treat these patients are available.
The challenges faced in treating these patients are also multi fold. A child is more difficult to examine both clinically and radiologically. The small size, lack of development, and lack of pneumatization of paranasal sinuses make the diagnosis of maxillofacial trauma by radiographic examination much more difficult in children. The maxilla and mandible of a child contain unerupted teeth or there is a mixed dentition this makes fixation more difficult via either internal means or by intermaxillary fixation [3]. Unwarranted operative intervention in the child, including unnecessary internal fixation, inadequate treatment, may lead to greater long-term deficits and deformities in the child than in the adult [3]. The objectives of this study were to record the pattern of facial injuries treated over a 10-year period and to document the associated injuries, soft tissue injuries, dental injuries, treatments provided and any complications that occurred.
Materials and Methods
During a period of 10 years from January 2003 to December 2013 1146 patients reported to SDM Craniofacial unit with facial fractures among them 68 were paediatric patients aged from 0 to 15 years. Data were collected from medical history, clinical and radiographic examination. The records were studied according to age and gender predilection, etiology, fracture pattern in upper 3rd of face, midface and mandible, dental trauma, soft tissue injuries, complications, associated injuries, treatment modalities. Comparisons were performed using Chi square test.
Results
From January 2003 to December 2013, 68 cases of paediatric facial fractures were recorded who were below 15 years of age and were treated in our unit.
-
Age and gender distribution: The age of occurrence of injury ranged between 0 and 15 years of age with a mean age of 8 years. The commonest age group of paediatric fractures were between 11 and 15 years reporting 33 cases (53.22 %), followed by age group between 6 and 10 years of age reporting 24 cases (35.29 %) and finally age group between 0 and 5 years of age reporting 11 cases (16.17 %).
A greater proportion of injured patients were boys (52) compared with girls (16) resulting in a ratio of 3.25:1.
Etiology: The commonest etiology seen in all age groups is Fall reporting 40 cases (58.82 %), followed by RTA reporting 20 cases (29.41 %) and finally other etiology like assault and sports related injuries reported 8 cases (11.76 %).
-
Fracture Pattern: The commonest facial bone fractured is mandible reporting 57 cases (83.82 %), followed by dentoalveolar fracture of upper anterior teeth in 6 cases (8.82 %), and followed by nasal bone fractures in 3 cases (4.41 %) other fractures like NOE was reported in 1 case and Le Fort II in 1case.
In mandible the commonest region of fracture was parasymphysis region reporting 46 cases (80.70 %), followed by condyle region (17.54 %) and angle also reporting 10 cases (17.54 %), and followed by symphysis and body fractures.
Combination fractures were mostly Parasymphysis with angle or parasymphysis with condyles. Out of the 57 mandible fractures 18 (31.57 %) were combination fractures. Among them prasymphysis with angle was commonest reporting 12 cases followed by parasymphysis with condyle reporting 6 cases.
In midface dentoalveolar fractures were commonest followed by nasal bone fractures.
In only one case there was both mandible and midface fracture.
Most commonly seen soft tissue injury associated with fracture is lacerations reported in 20 cases, followed by haematoma in 6 cases.
Associated dental injury commonly seen is avulsion reported in 10 cases, followed by 4 cases with intrusion and 4 cases with Ellis Class I fracture.
The commonest treatment protocol followed in management of these fractures was closed reduction by cap splinting and circummandibular wiring which was done in 25 cases (36.76 %). These were commonly cases of mandibular fractures and those children below 12 years of age. Children above 13 years were treated mainly by open reduction and internal fixation, done in 31 cases (45.59 %). Arch bar fixation was done in upper dentoalveolar fracture cases provided they were above 12 years of age, done in 5 cases. Nasal bone fractures were treated by closed reduction. Exception was in 2 cases that is one of Le Fort II and the other in case of NOE fracture where these cases were treated by open reduction and internal fixation even though when they were below 12 years of age.
Commonest complication reported was plate infection leading to plate exposure and finally plate removal in 4 cases, other than that 2 cases of sublingual haematoma and 2 cases of wound dehiscence was also reported among all the 68 cases of paediatric fracture.
2 cases of clavicle fracture was the only associated injury seen in our paediatric fracture cases.
Discussion
The incidence of facial fractures in children has been well documented in the oral and maxillofacial surgery literature since World War II. Perhaps one of the most dramatic changes in this field has been the shifting patterns of etiology, incidence, prevention and surgical management [4].
Reports have stated that the incidence of paediatric fractures varies between 1.4 and 15.0 % of all maxillofacial fracture under the age of 16 and incidence varies 0.87–1 % under the age of 5 [5, 6]. The incidence is considerably low in children below 5 years of age because younger children are less active and lighter in weight and, therefore, fall less frequently and less heavily, which may explain the lower incidence of fractures in children younger than 5 years of age [7] (Figs. 1, 2, 3, 4, 5, 6).
Fig. 1.

Pre operative mandibular fracture—step deformity right parasymphysis fracture
Fig. 2.
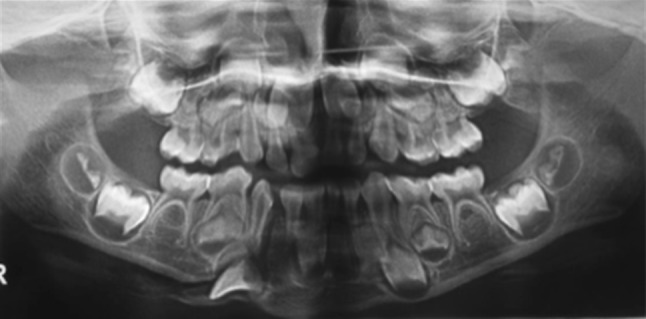
Preoperative Orthopantomograph of the mandibular fracture
Fig. 3.

Immediate postoperative with cap splint
Fig. 4.
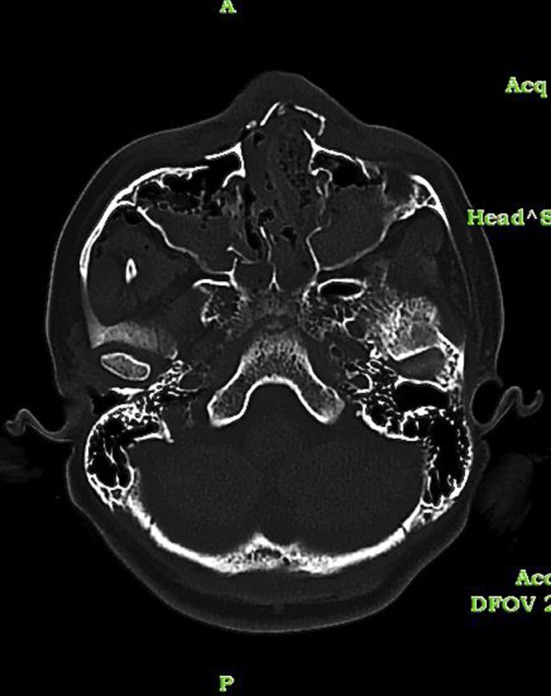
Axial section showing fracture of the nasal bone and fracture of the right Maxillary sinus walls
Fig. 5.
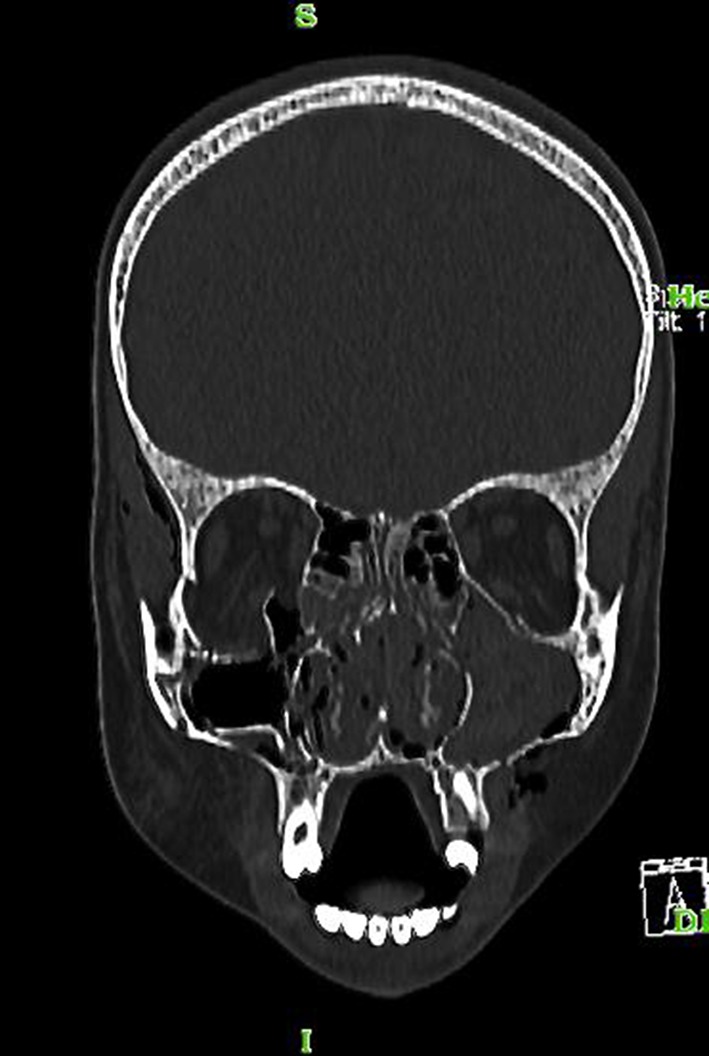
Coronal section showing medial wall and floor of orbit fracture on right side
Fig. 6.
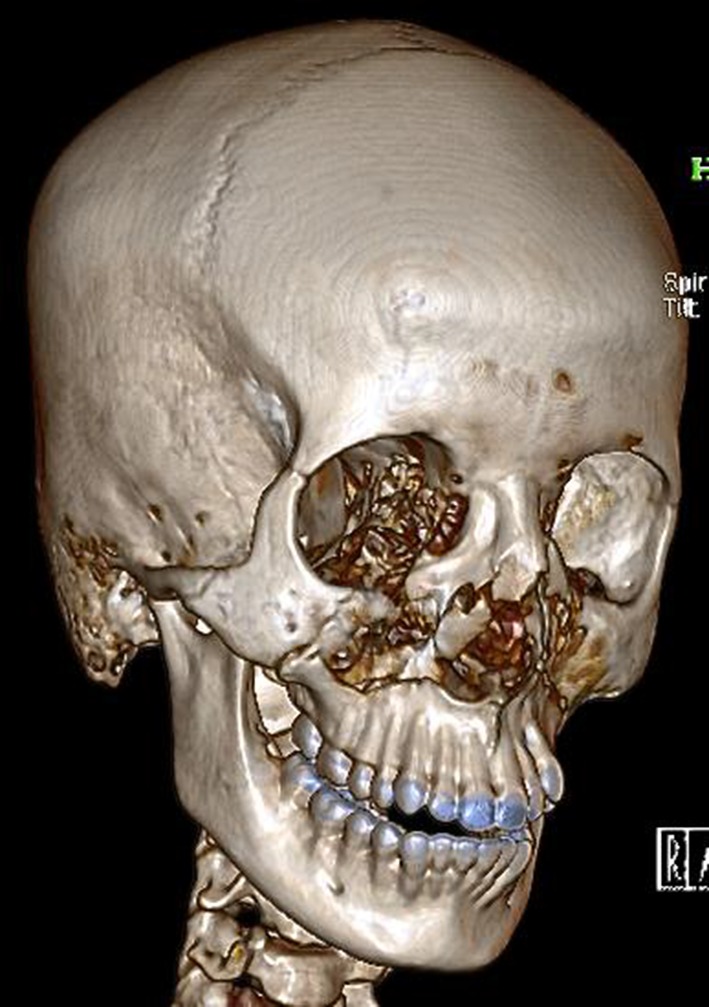
3 D reconstruction CT scan showing multiple midface bones fractures
In our study incidence of paediatric facial fractures is 6 % of all the patients. This result was very much similar to the studies done by Gassner et al. [3] where the incidence of paediatric population among all patients that reported with facial fractures was 4 %. Our results were also similar to studies done by Steinhardt (1962), McCoy et al. [8], Rowe [9], Velgos et al. (1969), Kiyota [10] and Nishijima et al. [11] who also stated that the incidence varies between 1.4 and 15 %.
In our study the commonest age group is 11–15 years. Our results exhibit mild increases in numbers of patients with age, and demonstrate a remarkable increase at 11–15 years. This result are similar with some reports (Tanaka et al. [5]; Zachariades et al. [12]; Thore´n et al. [13]), although there have been some studies showing the largest subgroup to be somewhat younger (Posnick et al. [2]; Oji [7]; Stylogianni et al. [14]; Gu¨ven [15], 1993; Anderson [16], 1998; Holland et al. [17]).
Our study also found a preponderance of boys in our population affected with maxillofacial fractures compared to girls giving a ratio of 2.9:1 which were similar to studies done by Posnick et al. [2], Tanaka et al. [5], Oji [7], Zachariades et al. [12], Thore´n et al. [13], Stylogianni et al. [14], Guven [15], Anderson [16], Adekeye [18], Kotilainen et al. [19], Infante Cossio et al. [20], Acton et al. [21], Bamjee et al. [22] and Zerfowski and Bremerich [23]. The reason is that boys are generally more boisterous than girls and spend more time outdoors [7].
The incidence of paediatric trauma is less when compared to adults because of multiple reasons:
The body mass of adults is greater than children so during traumatic episode there is greater force per unit body area acting.
The child’s incompletely calcified skeleton is close to the internal organs with less fat and more elastic connective tissue. These factors result in multiple internal organ injuries, often without facial fractures.
Children are susceptible to secondary brain injury because of differences in cerebral physiology and oxygen demand. The cranial-mass-to-body-mass ratio is high, which results in higher-energy impacts to the cranium [6].
In our study the commonest etiology of paediatric fractures is fall seen in 58 % which was similar to the studies done by Kaban [4], Tanaka et al. [5], Thore´n et al. [13], Stylogianni et al. [14], Guven [15], Holland et al. [17] and Kotilainen et al. [19]. Another note that we would like to make from our study is that it shows a significant increase in Road Traffic Accidents as the etiology of paediatric facial fractures. One of the reasons may be because conventional lap belts do not properly restrain or protect paediatric patients because the anterior superior iliac spine is not completely developed. The restraint, therefore, rides up onto the abdomen and chest and may itself cause serious injuries and secondly when a car rapidly decelerates, the child may whip forward with greater force than an adult because of the child’s high centre of gravity and greater body mass above the waist [4].
In our study mandible is the commonest bone to be fractured among all (83 %) and parasymphysis was the commonest region of fracture. Our results were similar to the studies done by of Oikarinen and Malmastrom [25], AI-Aboosi and Perriman [26]. Other studies have also shown condylar fractures were the most common site Reil and Kranz [27], McGuiri and Salisbury [28] and Amaratunga [29]. In our study condylar fracture is the second most common fracture site.
Compared with occurrence rates reported in studies of adults, the frequency of midfacial injury was relatively low in our patients. The reason for a low incidence may be because children are protected from midfacial fractures by incomplete development of the facial sinuses and fissures, flexibility of osseous suture lines, and thicker adipose tissue [2]. The incidence of midface fracture in our unit was 16.17 %. These results were quite similar to those of Tanaka et al. [5], Oji [7], Guven [15], Reil and Kranz [27], Kaban et al. [30] and Gussack et al. [31]. In midface dentoalveolar fractures of maxilla were commonest followed by nasal bone fractures. Our results were similar to that of Tanaka et al. [5], Zachariades et al. [12] and Maniglia and Kline [32].
Pediatric soft tissue injuries are frequently overlooked when discussing pediatric trauma. Yet they occur in association with facial fractures 29–56 % of the time [6]. In our study the incidence of soft tissue injuries was 38.2 %. The modalities of management of such injuries are similar to that of adults but it has to be kept in mind that healing process starts faster so chances of formation of hypertrophic scar or keloid is more [3].
The incidence of dental injury in our cases was 25 % and the commonest injury was avulsion. The maxillary central incisors were the commonest teeth to be avulsed. This is expected because maxillary central incisors are the most protrusive teeth, and therefore, they are more likely to be struck by an object or hit the ground first.
When formulating a plan of treatment for pediatric patients with facial trauma, a number of elements must be considered. These include the age of the patient (to maximize growth and development), the anatomic site (to optimize form and function), the complexity of the injury (displacement, comminution, and the number of sites), the time elapsed since injury (ideal to treat within 4 days), concomitant injury (fitness for anesthesia and duration of surgery), and the surgical approach (closed versus open). We will discuss about the treatment modalities depending on the site of fracture.
Mandibular Fractures: In our study most of the mandibular fractures were treated by cap splinting and circummandibualr wiring. Because of the presence of tooth buds and the softness of the bone, closed reduction and immobilization with either splints or combinations of splints and maxillomandibular fixation have remained standard treatment during the deciduous dentition [4]. Only patients above 12 years of age were subjected to open reduction and internal fixation, since it can be assumed that the teeth were safely away from inferior border. As stated by Kaban et al. [4] the most common treatment for condylar fractures in children continues to be analgesics, a liquid to soft diet, and observation in the absence of malocclusion, or a short period of immobilization (7 to 10 days) in the presence of pain and malocclusion. The critical elements of treatment are still early mobilization and close observation of the occlusion. Open reduction should be considered when the occlusion cannot be re-established because of the position of the fractured condylar segment [6]. In our study we followed the same protocol as stated by Kaban et al. only in one case of bilateral subcondylar fracture we did open reduction and internal fixation of the left condyle.
Midface Fractures: Maxillary dentoalveolar fractures were mostly treated by composite wire splinting for patients below 12 years of age; those above 12 years were subjected to arch bar fixation. Nasal bone fractures were treated by closed reduction only. Similar treatment protocol was followed for nasal bone fracture by Posnick et al. [3] and Kaban et al. [4]. Only one case of Le Fort II and one case of NOE fracture was recorded in our study and both of them were treated by open reduction and internal fixation with miniplates.
The incidence of postoperative complication in our study is 12 %. Among them 4 cases were of infected plates which were removed eventually, 2 cases were of postoperative sublingual haematoma and 2 cases of wound dehiscence.
The only reported associated injury in these cases was clavicle fracture which was seen in 2 cases only. Our incidence of associated injuries was quite less compared to study done by Gassner et al. where the incidence of such injuries is 6.3 %. The reason for such a difference in result may be attributed to the fact that our institute is a tertiary health care centre and most of the associated injuries are already been addressed in primary and secondary health care and the patient is stable before reporting to our unit.
Conclusion
It is clear that the foundations for diagnosis and the basic principles of management have changed little since 1943 and probably since the work of Kazanjian in World War I [4]. In addition, the advent of antibiotics; new imaging techniques (particularly CT), and availability of new instrumentation and rigid internal fixation have all revolutionized the specific treatment of pediatric facial fractures. Results of our studies and similar studies done by Ida et al. 2002 and Gassner et al. 2004 show that the decisive limit for studying paediatric maxillofacial fractures should be 15 years as patients older than this age limit resembled fracture patterns similar to those of adults.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Compliance with Ethical Standards
Conflict of interest
Author Dr. Rajarshi Ghosh, Author Dr. K. Gopalkrishnan, and Author Dr. Jawahar Anand declare that they have no conflict of interest.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s12663-016-0965-8) contains supplementary material, which is available to authorized users.
Contributor Information
Rajarshi Ghosh, Email: rg_everywhere@yahoo.co.in.
K. Gopalkrishnan, Email: gops15@gmail.com
Jawahar Anand, Email: jawanand@yahoo.co.uk.
References
- 1.Kyrgidis A, et al. Incidence, aetiology, treatment outcome and complications of maxillofacial fractures. A retrospective study from Northern Greece. J Craniomaxillofac Surg. 2013;41:637–643. doi: 10.1016/j.jcms.2012.11.046. [DOI] [PubMed] [Google Scholar]
- 2.Posnick JC, Wells M, Pron GE. Pediatric facial fractures: evolving patterns of treatment. J Oral Maxillofac Surg. 1993;51:836–844. doi: 10.1016/S0278-2391(10)80098-9. [DOI] [PubMed] [Google Scholar]
- 3.Gassner R, Tuli T, Hachl O. Craniomaxillofacial trauma: a 10 year review of 9543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31:51–61. doi: 10.1016/S1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 4.Kaban LB. Diagnosis and treatment of fractures of facial bones in children 1943–1993. J Oral Maxillofac Surg. 1993;51:722–729. doi: 10.1016/S0278-2391(10)80409-4. [DOI] [PubMed] [Google Scholar]
- 5.Tanaka N, et al. Maxillofacial fractures in children. J Craniomaxillofac Surg. 1993;21:289–293. doi: 10.1016/S1010-5182(05)80349-X. [DOI] [PubMed] [Google Scholar]
- 6.Ida S, Matsuya T. Paediatric maxillofacial fractures: their aetiological characters and fracture patterns. J Craniomaxillofac Surg. 2002;30:237–241. doi: 10.1054/jcms.2002.0295. [DOI] [PubMed] [Google Scholar]
- 7.Oji C. Fractures of the facial skeleton in children: a survey of patients under the age of 11 years. J Craniomaxillofac Surg. 1998;26:322–325. doi: 10.1016/S1010-5182(98)80062-0. [DOI] [PubMed] [Google Scholar]
- 8.MacCoy FJ, Chandler RA, Crow ML. Facial fractures in children. Plast Reconst Surg. 1966;37:209–215. doi: 10.1097/00006534-196603000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Rowe NL. Fractures of the jaws in children. J Oral Surg. 1969;27:497–507. [PubMed] [Google Scholar]
- 10.Kiyota K. Clinical and roentgenographic studies on fractures of the jaw in children. J Jpn Stomatol. 1976;43:479–508. doi: 10.5357/koubyou.43.479. [DOI] [PubMed] [Google Scholar]
- 11.Nishijima K, et al. Clinicostatistical observation and prognosis of pediatric mandibular fracture cases in our department during the past 15 years. Jpn J Pediatr Dent. 1978;16:461–467. [Google Scholar]
- 12.Zachariades N, Papavassiliou D, Koumoura F. Fractures of the facial skeleton in children. J Craniomaxillofac Surg. 1990;18:151–153. doi: 10.1016/S1010-5182(05)80509-8. [DOI] [PubMed] [Google Scholar]
- 13.Thore´n H, et al. Different patterns of mandibular fractures in children. An analysis of 220 fractures in 157 patients. J Craniomaxillofac Surg. 1992;20:292–296. doi: 10.1016/S1010-5182(05)80398-1. [DOI] [PubMed] [Google Scholar]
- 14.Stylogianni L, Arsenopoulos A, Patrikiou A. Fractures of the facial skeleton in children. Br J Oral Maxillofac Surg. 1991;29:9–11. doi: 10.1016/0266-4356(91)90164-Z. [DOI] [PubMed] [Google Scholar]
- 15.Guven O. Fractures of the maxillofacial region in children. J Craniomaxillofac Surg. 1992;20:244–247. doi: 10.1016/S1010-5182(05)80435-4. [DOI] [PubMed] [Google Scholar]
- 16.Anderson PJ. Fractures of the facial skeleton in children. Injury. 1995;26:47–50. doi: 10.1016/0020-1383(95)90552-9. [DOI] [PubMed] [Google Scholar]
- 17.Holland AJ, et al. Facial fractures in children. Pediatr Emerg Care. 2001;17:157–160. doi: 10.1097/00006565-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Adekeye EO. Paediatric fractures of the facial skeleton: a survey of 85 cases from Kaduna, Nigeria. J Oral Surg. 1980;38:355–358. [PubMed] [Google Scholar]
- 19.Kotilainen R, Karja J, Kullaa-Mikkonen A. Jaw fractures in children. Int J Pediatr Otorhinolaryngol. 1990;19:57–61. doi: 10.1016/0165-5876(90)90195-W. [DOI] [PubMed] [Google Scholar]
- 20.Infante Cossio P, et al. Mandibular fractures in children. A retrospective study of 99 fractures in 59 patients. Int J Oral Maxillofac Surg. 1994;23:329–331. doi: 10.1016/S0901-5027(05)80047-5. [DOI] [PubMed] [Google Scholar]
- 21.Acton CH, Nixon JW, Clark RC. Bicycle riding and oral/maxillofacial trauma in young children. Med J Aust. 1996;165:249–251. doi: 10.5694/j.1326-5377.1996.tb124957.x. [DOI] [PubMed] [Google Scholar]
- 22.Bamjee Y, et al. Maxillofacial injuries in a group of South Africans under 18 years ofage. Br J Oral Maxillofac Surg. 1996;34:298–302. doi: 10.1016/S0266-4356(96)90006-6. [DOI] [PubMed] [Google Scholar]
- 23.Zerfowski M, Bremerich A. Facial trauma in children and adolescents. Clin Oral Invest. 1998;2:120–124. doi: 10.1007/s007840050056. [DOI] [PubMed] [Google Scholar]
- 24.Iizuka T, et al. Midfacial fractures in pediatric patients. Frequency, characteristics and causes. Arch Otolaryngol Head Neck Surg. 1995;121:1366–1371. doi: 10.1001/archotol.1995.01890120026005. [DOI] [PubMed] [Google Scholar]
- 25.Oikarinen VJ, Malmstrom M. Jaw fractures. Suom Hammaslaak Toim. 1969;65:95–99. [PubMed] [Google Scholar]
- 26.AI-Aboosi K, Perriman A. One hundred cases of mandibular fractures in children in Iraq. Int J Oral Surg. 1976;5:8–12. doi: 10.1016/S0300-9785(76)80004-X. [DOI] [PubMed] [Google Scholar]
- 27.Reil B, Kranz S. Traumatology of the maxillofacial region in childhood (Statistical evaluation of 210 cases in the last 13 years) J Maxillofac Surg. 1976;4:197–201. doi: 10.1016/S0301-0503(76)80035-5. [DOI] [PubMed] [Google Scholar]
- 28.McGuiri WF, Salisbury PL. Mandibular fractures. Arch Otolaryngol Head Neck Surg. 1987;113:257–261. doi: 10.1001/archotol.1987.01860030033003. [DOI] [PubMed] [Google Scholar]
- 29.de Amaratunga NAS. Mandibular fractures in children. A study of clinical aspects, treatment needs, and complications. J Oral Maxillofac Surg. 1988;46:637–640. doi: 10.1016/0278-2391(88)90105-X. [DOI] [PubMed] [Google Scholar]
- 30.Kaban LB, Mulliken JB, Murray JE. Facial fractures in children. Plast Reconstr Surg. 1977;59:15–20. doi: 10.1097/00006534-197701000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Gussack GS, et al. Pediatric maxillofacial trauma: unique features in diagnosis and treatment. Laryngoscope. 1987;97:925–930. doi: 10.1288/00005537-198708000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Maniglia AJ, Kline SH. Maxillofacial trauma in the paediatric age group. Otolaryngol Clin North Am. 1983;16:717–730. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


