Abstract
A 48-year-old man presented as an emergency with a 3-week history of rectal bleeding. Examination of his rectum revealed a circumferential tumour, 2 cm from the anal verge. An MRI scan reported a locally infiltrative mid-lower rectal tumour staged as T3d/T4 N2 MX. A colonoscopy revealed appearances of severe proctitis and biopsies did not show any evidence of dysplasia or malignancy. The patient was discussed at the regional colorectal cancer multidisciplinary team meeting with a management plan for neoadjuvant chemoradiotherapy following repeat biopsies, which were again negative for malignancy. He tested positive for the HIV and was referred to genitourinary medicine. A positive Chlamydia trachomatis nucleic acid test from a rectal swab was serovar L2 consistent with a diagnosis of lymphogranuloma venereum. He was treated with doxycycline and subsequent MRI scans showed reduction in tumour size with eventual resolution. This case report highlights the importance of HIV testing in patients with newly diagnosed colorectal tumours.
Background
This case report highlights the importance of HIV testing in patients diagnosed with proctitis and colorectal malignancy, as well as the benefits of repeated history taking and investigations if the diagnosis is not clear.
Case presentation
A 48-year-old man presented as an emergency with a 3-week history of rectal mucus discharge and fresh rectal bleeding mixed with faeces and associated with tenesmus. He did not report any abdominal pain, weight loss or any other symptoms. He had a previous medical history of duodenitis and a family history of Crohn’s disease. He worked as an operations manager for social housing, lived alone and was divorcing his third wife. He smoked 20 cigarettes a day and did not drink any alcohol.
On examination, he had normal vital signs with a normal examination of his cardiovascular and respiratory systems. Abdominal examination did not reveal any abnormality. Digital rectal examination revealed a first-degree haemorrhoid at the 9 o’clock position and a circumferential rectal tumour, 2 cm from the anal verge.
Investigations
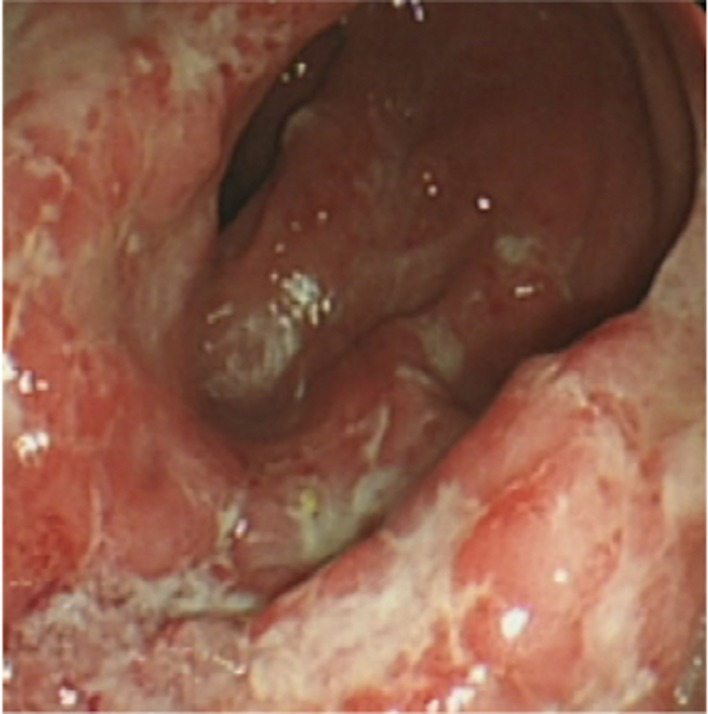
His blood tests showed: haemoglobin 15.4 (14–16) g/dL, white cell count 7.3 (3–11) 109/L, C reactive protein 20 (<7) mg/L, normal liver and renal function. His carcinoembryonic antigen (CEA) test was 1.8 (<3) ng/mL. The initial working diagnosis of a rectal cancer was made and the patient went on to have endoscopic investigations and radiological staging. A colonoscopy revealed appearances of ulcerative proctitis (figure 1) and biopsies showed severe patchy proctitis without evidence of dysplasia or malignancy. A high-resolution magnetic resonance image (MRI) reported appearances consistent with a locally infiltrative mid-lower rectal tumour staged as T3d/T4 N2 MX (figure 2). A CT scan of his chest, abdomen and pelvis suggested appearances of a rectal tumour with local invasion but without any distant metastases.
Figure 1.
Endoscopic view of the rectum showing severe proctitis.
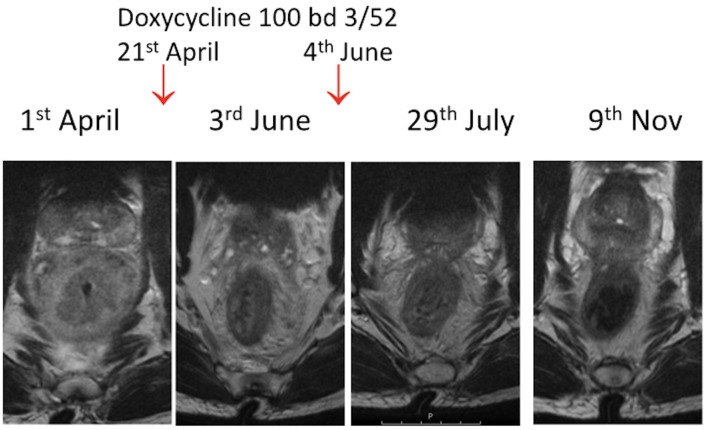
Figure 2.
Sequential MRI of the pelvis scans from diagnosis to treatment—demonstrating extensive circumferential soft tissue thickening and stranding into mesorectal fat (extramural tumour spread) with extramural venous invasion into the superior rectal vessels in the first image.
The patient re-presented to the emergency department with increasing anal pain. Further questioning revealed he had had multiple female sexual partners and he consented to an HIV test which was positive. He had a CD4 cell count of 420mm3 and an undetectable viral load. He was negative for hepatitis A, B and C and any AIDS-defining illnesses.
A repeat biopsy after 2 weeks showed inflamed and ulcerated large bowel mucosa with inflamed polypoidal granulation-type tissue formation, no dysplasia or malignancy. The diagnosis of lymphogranuloma venereum (LGV) was made following a positive L2 serovar Chlamydia trachomatis nucleic acid test of a rectal swab. It subsequently transpired that the patinet’s risk factors for HIV included injecting crystal meth and sharing of rectal sex toys which are likely to have contributed to the acquisition of LGV.
Differential diagnosis
Rectal cancer
Proctitis secondary to inflammatory bowel disease
Cytomegalovirus colitis
Herpes simplex virus colitis
Treatment
The patient commenced empirical mesalazine (AsacolMR, Warner Chilcott) 800 mg three times a day and prednisolone enemas (Predsol, RPH) 20 mg twice a day, based on the initial endoscopic findings of proctitis. The case was discussed at the regional colorectal multidisciplinary team (MDT) meeting and the decision was made for the patient to have neoadjuvant chemoradiotherapy and subsequent surgery based on response, following repeat biopsies. In the interim, the patient tested positive for HIV prompting a referral to genitourinary medicine (GUM) physicians. He had an emergency laparoscopic defunctioning loop colostomy due to symptoms and impending bowel obstruction. Following the rectal swab diagnosis of LGV, he completed a 3-week course of doxycycline 100 mg twice a day. He required a second course because of ongoing rectal bleeding. For his HIV treatment, he was commenced on Truvada (Gilead) (tenofovir and emtricitabine fixed-dose tablet) and dolutegravir.
Outcome and follow-up
Following treatment with oral doxycycline for LGV, the patient did not consent to a repeat flexible sigmoidoscopy but had repeat MRI scans which showed resolution of the tumour. He subsequently had a reversal of his colostomy and made a good recovery.
Discussion
We present a case of LGV mimicking a rectal tumour in a heterosexual man with a recent diagnosis of HIV, as an unusual cause of a rectal tumour. This is a sexually transmitted infection caused by the obligate intracellular bacterium C. trachomatis.1 The condition is characterised by genital papules or ulcers followed by painful inguinal and/or femoral lymphadenopathy causing buboes. If there is rectal involvement, a patient may present with rectal bleeding, pain and tenesmus due to proctitis or proctocolitis.2 Hence, the symptoms may be confused with colitis or malignancy which importantly need to be excluded first. There have been only a few case reports of rectal LGV but only one associated with rectal cancer.3 4
The transmission of LGV is via anal, oral and vaginal sexual intercourse or the use of shared sex toys.5 LGV is endemic in parts of Africa, South and Central America, the Caribbean and South East Asia, and has previously rarely been reported in high-income countries. It has become increasingly common however in Western Europe and the USA particularly among men who have sex with men (MSM).2 In the UK, 99% of cases occur in MSM.6 The diagnosis of LGV is frequently associated with hepatitis C and HIV.7 Treatment with a 3-week course of doxycycline prevents the complications of LGV such as rectal strictures, fistulae, permanent genital lymphoedema (elephantiasis), bowel obstruction and bowel perforation.8 9
Our patient initially only disclosed part of his social and sexual history, omitting his use of intravenous recreational drugs and rectal sex toys with women. He denied any MSM contact, which makes his presentation of LGV with a new diagnosis of HIV unusual. The recognition of this clinical entity is important to ensure the appropriate therapy. It is essential to rule out infective causes of colitis in order to avoid unnecessary treatments and surgery associated with the misdiagnoses of indeterminate inflammatory bowel disease or rectal cancer. Our patient was discussed in the colorectal MDT, with the convincing MRI scans, and could have potentially undergone chemoradiotherapy with all its associated adverse effects if he did not have an HIV test to prompt referral to the GUM clinic. Therefore, it is crucial not to rely on the MDT solely for the diagnosis but for the management plans post diagnosis, in order to avoid overtreatment and potential harm.10 Partner notification is also an essential part of the management of LGV to ensure sexual contacts are treated and to prevent reinfection or further onward transmission.
The diagnosis and management of this patient was successfully carried out through multiprofessional teamwork by colorectal surgeons, GUM physicians, radiologists, histopathologists, microbiologists and clinical nurse specialists. It is important for HIV testing to be incorporated as part of the management plan for colorectal malignancies.
Learning points.
Importance of sexual history and HIV testing in patients with new diagnoses of colorectal tumours and proctitis.
The MRI images of lymphogranuloma venereum can mimic rectal carcinoma—treat the patient not the image.
Sexually transmitted infections need to be considered as a cause of proctitis.
Acknowledgments
Thank you to Mr Paul Tommey, Consultant Colorectal Surgeon for his expertise, Dr Essam Raweily, Consultant Pathologist for reviewing on the pathology specimens and Dr Nalin Kholsa, Consultant Radiologist for reviewing and selecting the appropriate images.
Footnotes
Contributors: MAW and CS: reviewing literature, writing case report and reviewing of manuscript. SM: literature review. DP: review of manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hechtman JF, Dimaio CJ, Matloff J, et al. Rectal lymphogranuloma venereum mimicking cancer. Endoscopy 2013;45:E315–E316. 10.1055/s-0033-1344407 [DOI] [PubMed] [Google Scholar]
- 2.Richardson D, Goldmeier D. Lymphogranuloma venereum: an emerging cause of proctitis in men who have sex with men. Int J STD AIDS 2007;18:11–16. 10.1258/095646207779949916 [DOI] [PubMed] [Google Scholar]
- 3.Mistrangelo M, Dal Conte I, Gregori G, et al. Rectal lymphogranuloma venereum. Colorectal Dis 2012;14:e792–e793. 10.1111/j.1463-1318.2012.03000.x [DOI] [PubMed] [Google Scholar]
- 4.Papagrigoriadis S, Rennie JA. Lymphogranuloma venereum as a cause of rectal strictures. Postgrad Med J 1998;74:168–9. 10.1136/pgmj.74.869.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vall-Mayans M. Be aware of proctitis and lymphogranuloma venereum. Eur J Dermatol 2009;19:203–4. 10.1684/ejd.2009.0659 [DOI] [PubMed] [Google Scholar]
- 6.Ward H, Alexander S, Carder C, et al. The prevalence of lymphogranuloma venereum infection in men who have sex with men: results of a multicentre case finding study. Sex Transm Infect 2009;85:173–5. 10.1136/sti.2008.035311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rüther U, Rupp W, Müller HA, et al. Rectal pseudotumor due to Chlamydia trachomatis in a male homosexual. Endoscopy 1990;22:237–8. 10.1055/s-2007-1012857 [DOI] [PubMed] [Google Scholar]
- 8.Nieuwenhuis RF, Ossewaarde JM, Götz HM, et al. Resurgence of lymphogranuloma venereum in Western Europe: an outbreak of Chlamydia trachomatis serovar l2 proctitis in The Netherlands among men who have sex with men. Clin Infect Dis 2004;39:996–1003. 10.1086/423966 [DOI] [PubMed] [Google Scholar]
- 9.Ward H, Martin I, Macdonald N, et al. Lymphogranuloma venereum in the United kingdom. Clin Infect Dis 2007;44:26–32. 10.1086/509922 [DOI] [PubMed] [Google Scholar]
- 10.Eigenmann F. Multidisciplinary team meetings encourage overtreatment. BMJ 2015;351:h4630 10.1136/bmj.h4630 [DOI] [PubMed] [Google Scholar]