Abstract
Mesalamine, or 5-aminosalicylic acid, is a frequently used medication for the treatment of inflammatory bowel disease (IBD). We report the case of a 40-year-old woman recently diagnosed with IBD and started on mesalamine, who presented with new onset tender skin lesions 3 days following medication administration. One day following the onset of skin lesions, the patient developed acute chest pain, shortness of breath, ECG changes, troponemia, C-reactive protein elevation and pericardial enhancement on cardiac MRI consistent with myopericarditis. Subsequent skin biopsy confirmed the diagnosis of Sweet’s syndrome. On cessation of the drug, both the skin lesions and the cardiac symptoms resolved in combination with anti-inflammatory therapy. While mesalamine has been previously associated with myocarditis and pericarditis, to our knowledge this is the first case of coexisting Sweet’s syndrome with myopericarditis in the context of mesalamine therapy.
Keywords: inflammatory bowel disease, crohn’s disease, drugs: gastrointestinal system, pericardial disease, unwanted effects / adverse reactions
Background
5-Aminosalicylic acid products are widely used for the treatment of inflammatory bowel disease (IBD). Although not previously described for mesalamine-containing products, Sweet’s syndrome (SS), or acute febrile neutrophilic dermatitis, is an inflammatory skin condition which can be drug-induced. Rare cardiac complications of mesalamine therapy include both myocarditis and pericarditis, which have previously been described.1 We report the case of a patient who developed SS and myopericarditis within 1 week of initiation of mesalamine treatment, both of which resolved with cessation of the medication and concomitant anti-inflammatory therapy.
Case presentation
A previously healthy 40-year-old woman presented with new onset bright red blood per rectum and mucus-containing stools. Concurrently, she noticed discomfort in her lower vulvovaginal area and a mass on her left vaginal introitus that had been increasing in size over a 2-week time period. Physical examination and anoscopy revealed an anal fissure, a large rectovaginal septum ulcer (2×3 cm) and proctitis. CT of the abdomen and pelvis found a perirectal abscess, pelvic lymphadenopathy and rectal wall thickening. The patient was started on a 7-day course of amoxicillin at that time. A subsequent colonoscopy identified an anal fissure and moderate-to-severe colitis extending from the anus to the descending colon in a continuous and circumferential pattern, with pathological features consistent with Crohn’s disease (CD).
The patient was subsequently started on oral mesalamine and rectal suppository mesalamine, with no corticosteroids administered. Three days following initiation of the medication, she noticed a new onset rash on her face, neck, bilateral extremities and back, described as pruritic and tender to palpation (figure 1). The patient presented to a physician 3 days after the onset of the skin lesions with a temperature of 37.7°C and was advised to discontinue mesalamine products and apply antibiotic ointment to the affected areas. A subsequent biopsy of a left forearm lesion confirmed SS (figure 2), and topical clobetasol cream was administered. One day later, the patient developed acute onset shortness of breath and chest pain during sleep and presented to the emergency department with a temperature of 38.5°C. Laboratory testing showed an elevated troponin T of 0.12 ng/mL, C-reactive protein 184 mg/L, N-terminal of pro-Brain Natriuretic Peptide (NT-proBNP)7043 pg/mL and white cell count 12.5 x109/L (9.85 x109/L neutrophils). ECG showed diffuse ST elevations most prominent in the anteroseptal leads (figure 3). Cardiac MRI demonstrated diffuse pericardial enhancement and oedema (figure 4). Given her clinical picture and evidence of cardiac biomarker positivity, she was diagnosed with myopericarditis, and colchicine and indomethacin were initiated. The following day, the patient became hypotensive, tachycardic and febrile and was started on empiric antibiotics. An MRI of the pelvis was obtained which revealed a left perirectal abscess involving the left labia, proctitis associated with a complex rectal and trans-sphincteric perianal sinus tract. Anorectal and speculum examinations under anaesthesia confirmed the perianal sinus, proctitis and sinus tract. Blood cultures were obtained and were negative for growth, and the patient completed a 7-day course of ciprofloxacin and metronidazole.
Figure 1.
Scattered 1–2 cm well-demarcated edematous and erythematous plaques with some central blistering and erosions with crust. The lesions are evident on (A) the patient’s arm, (B) neck (fading away and consistent with erythematous macules) and (C) palate (erythematous plaque with central erosion).
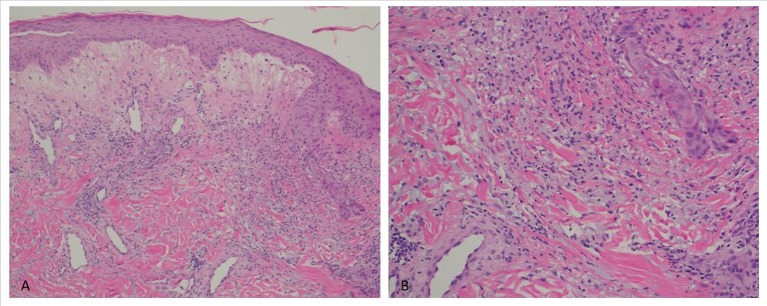
Figure 2.
(A) Papillary dermal oedema with an inflammatory infiltrate of the superficial to mid dermis, involving the perivascular and interstitial regions (x100 magnification). (B) Superficial and mid dermal perivascular and interstitial lymphohistiocytic inflammatory infiltrate with neutrophils and leucocytoclasis (x200 magnification).
Figure 3.
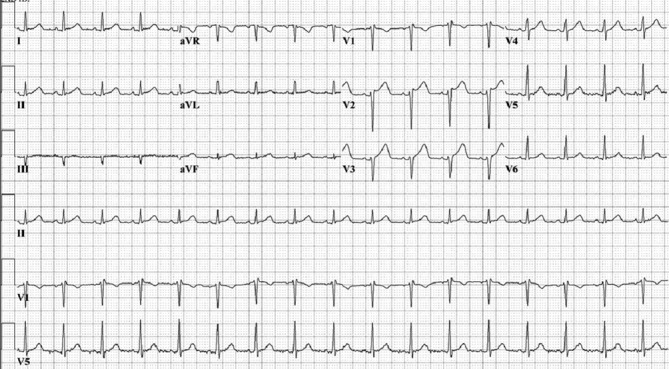
ECG revealing diffuse non-specific ST elevations most prominent in the anteroseptal leads (V2–V5).
Figure 4.
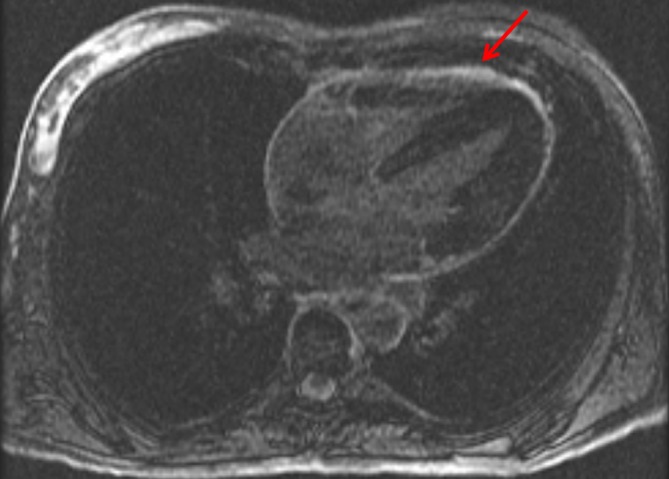
Cardiac MRI late gadolinium enhanced series: circumferential pericardial hyperenhancement (see arrow).
Differential diagnosis
Differential diagnosis of the patient’s fever and concurrent rash included infectious aetiologies (bacterial/viral), drug reaction, connective tissue disease, vasculitis, urticaria, erythema nodosum and SS.
Outcome and follow-up
The patient began therapy for her CD with infliximab and was discharged from the hospital. One week following hospital discharge, the patient noticed increasing pain in her vaginal area and underwent incision and drainage of a left anterolateral perirectal abscess, and antibiotics were not begun at this time. A subsequent MRI enterography was performed 2 weeks later and found improving proctitis and perianal fistula from the previous imaging. One month post-hospitalisation, the patient’s CD was in remission, and she continued on infliximab and azathioprine treatment. For her myopericarditis, she was asymptomatic 20 days following the onset of her symptoms, but given a persistent friction rub on examination, it was elected to complete a 6-week course of indomethacin and colchicine. Additionally, the skin lesions improved soon after medication cessation, and only a few scattered lesions were evident at her 20-day follow-up with no evidence of recurrence at her 6-week follow-up.
Discussion
Mesalamine is a commonly used treatment for IBD. Generally, the medication is well tolerated, with rare side effects being predominately gastrointestinal, including nausea, diarrhoea and abdominal pain. Although highly uncommon, mesalamine has been previously reported to cause myocarditis and pericarditis.2–6 Despite the previous case descriptions, the mechanism of mesalamine-associated myocardial inflammation has yet to be elucidated. Of the previously published cases, few have confirmed myocarditis or pericarditis by MRI.7–10 Most of the reported cases describe cardiac involvement within 2–4 weeks of medication initiation and resolution of symptoms following cessation of the drug.7 Our patient had findings consistent with the previously described temporal relationship, as myopericarditis occurred within 4 days of medication initiation. Our patient continued with 6 weeks of indomethacin and colchicine for her myopericarditis and was asymptomatic from a cardiac perspective at follow-up.
SS, or acute febrile neutrophilic dermatosis, is an inflammatory skin disorder characterised by the abrupt onset of tender erythematous skin lesions. It typically involves a constellation of symptoms including fever, typical skin lesions (figure 1) and neutrophilic infiltrate in the upper dermis on histology. Additionally, SS can have extracutaneous involvement (eg, oropharynx, as was observed in our patient). The syndrome typically presents in three settings: classical (idiopathic), malignancy-associated and drug-induced.11 Multiple pharmacological agents have been reported to cause drug-induced SS, with the most common reported being granulocyte-colony stimulating factor. Drug-induced SS diagnostic criteria include all of the following: abrupt onset of painful erythematous plaques/nodules, histopathological evidence of a dense neutrophilic infiltrate, fever >38°C, temporal relation between drug ingestion and clinical presentation, and resolution of lesions following drug withdrawal or systemic steroid treatment.12 Treatment of drug-induced SS requires cessation of the suspected drug, as well as topical or intralesional corticosteroids.12 Other agents, such as colchicine, have demonstrated efficacy and was used in our case given the cardiac involvement.
Classical SS can be a rare manifestation of IBD, more common in CD than ulcerative colitis.13 However, our patient’s gastrointestinal symptoms began roughly 1 month prior to the onset of skin lesions and 3 days following initiation of mesalamine therapy. This temporal relationship therefore fits the aforementioned criteria for drug-induced SS (with the history of recent mesalamine exposure), making IBD-associated SS less likely in this case. According to the Naranjo Adverse Drug Reaction Probability Scale, our patient had a probable adverse drug reaction to mesalamine. To our knowledge, this is the first case of a patient presenting with concurrent SS (biopsy proven) and myopericarditis following initiation of mesalamine-containing products. Consideration for these rare but potentially serious side-effects should therefore be considered when mesalamine is administered.
Learning points.
Mesalamine is a frequently used medication for the management of inflammatory bowel disease and has been previously associated with myocarditis and pericarditis. Generally, this presents within 2–4 weeks of medication initiation.
New-onset tender skin lesions with concurrent fever in a patient with recent mesalamine exposure are suggestive of drug-induced SS; a skin biopsy is helpful for confirming the diagnosis.
Although rare, this case highlights myopericarditis and Sweet’s syndrome as potential side-effects of mesalamine-initiation treatment; consideration for these conditions should occur in the appropriate clinical setting.
Footnotes
Contributors: SAS was involved in the conception/design of the work, data collection, interpretation, critical revision of the article and final approval of the published version. NYT was involved in the conception/design of the work, data collection, interpretation, critical revision of the article and final approval of the published version. RSP was involved in data collection, interpretation, critical revision of the article and final approval of the published version. KAP was involved in data collection, interpretation, critical revision of the article and final approval of the published version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Brown G. 5-Aminosalicylic Acid-Associated myocarditis and pericarditis: a narrative review. Can J Hosp Pharm 2016;69:466–72. 10.4212/cjhp.v69i6.1610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kristensen KS, Høegholm A, Bohr L, et al. Fatal myocarditis associated with mesalazine. Lancet 1990;335:605 10.1016/0140-6736(90)90387-K [DOI] [PubMed] [Google Scholar]
- 3.García-Morán S, Sáez-Royuela F, Pérez-Alvarez JC, et al. Myopericarditis and mitral insufficiency associated with ulcerative colitis treated with mesalazine. Inflamm Bowel Dis 2006;12:334–5. 10.1097/01.MIB.0000209788.19952.b7 [DOI] [PubMed] [Google Scholar]
- 4.Doganay L, Akinci B, Pekel N, et al. Mesalazine-induced myopericarditis in a patient with ulcerative colitis. Int J Colorectal Dis 2006;21:199–200. 10.1007/s00384-004-0706-1 [DOI] [PubMed] [Google Scholar]
- 5.Stelts S, Taylor MH, Nappi J, et al. Mesalamine-associated hypersensitivity myocarditis in ulcerative colitis. Ann Pharmacother 2008;42:904–5. 10.1345/aph.1K288 [DOI] [PubMed] [Google Scholar]
- 6.García-Ferrer L, Estornell J, Palanca V. Myocarditis by mesalazine with cardiac magnetic resonance imaging. Eur Heart J 2009;30:1015 10.1093/eurheartj/ehn615 [DOI] [PubMed] [Google Scholar]
- 7.Waite RA, Malinowski JM. Possible mesalamine-induced pericarditis: case report and literature review. Pharmacotherapy 2002;22:391–4. 10.1592/phco.22.5.391.33188 [DOI] [PubMed] [Google Scholar]
- 8.Merceron O, Bailly C, Khalil A, et al. Mesalamine-induced myocarditis. Cardiol Res Pract 2010;2010:1–3. 10.4061/2010/930190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galvão Braga C, Martins J, Arantes C, et al. Mesalamine-induced myocarditis following diagnosis of Crohn’s disease: a case report. Rev Port Cardiol 2013;32:717–20. 10.1016/j.repc.2012.12.018 [DOI] [PubMed] [Google Scholar]
- 10.Nair AG, Cross RR. Mesalamine-induced myopericarditis in a paediatric patient with Crohn’s disease. Cardiol Young 2015;25:783–6. 10.1017/S1047951114001048 [DOI] [PubMed] [Google Scholar]
- 11.Cohen PR. Sweet’s syndrome--a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis 2007;2:34 10.1186/1750-1172-2-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walker DC, Cohen PR. Trimethoprim-sulfamethoxazole-associated acute febrile neutrophilic dermatosis: case report and review of drug-induced sweet’s syndrome. J Am Acad Dermatol 1996;34:918–23. 10.1016/S0190-9622(96)90080-8 [DOI] [PubMed] [Google Scholar]
- 13.Lopes Caçola R, Soares M, Cardoso C, et al. Sweet’s syndrome complicating ulcerative colitis: a rare association. BMJ Case Rep 2016;2016 10.1136/bcr-2015-212990 [DOI] [PMC free article] [PubMed] [Google Scholar]