Abstract
A hernia is defined as a protrusion of an organ or its fascia through a sac of its containing cavity. The presentation of an inflamed appendix inside an incarcerated femoral hernia is termed de Garengeot’s hernia. Almost exclusively seen in the female patient, this type of hernia like all others can undergo strangulation leading to complications including appendicitis with or without perforation. Management as described in literature usually comprises open or laparoscopic approach, followed by appendectomy and repair of the femoral hernia with or without mesh. We describe a case of a female patient who presented with an irreducible groin swelling, found to have a femoral hernia containing the inflamed appendix intraoperatively and how it was managed surgically through a laparoscopic approach with a small mesh and closure of defect. Literature review on this rare form of hernia is discussed thereafter.
Keywords: general surgery, pathology, radiology
Background
Hernia and appendicitis form two of the most frequently encountered surgical pathologies. These two occurring together in the form of an incarcerated femoral hernia is a very rare occurrence. Mostly discovered intraoperatively, these hernias can pose some challenge in management specially when discovered as a surprise. Imaging with CT scanning in certain cases can give a heads up preoperatively; however, since it is very rare, there are no clear universal management guidelines, and the surgical approach and procedure will depend on each clinical scenario and expertise of the surgeon. Due to the rarity of the pathology, the management can pose some challenges, and hence it forms and interesting case to look into how such hernia’s can present, diagnosed and managed.
Case presentation
A 71-year-old female patient presented to the emergency department in a district general hospital of Northeastern England with a complain of right-sided groin pain of 1 day duration. Pain described as worsening with movement and associated with a small lump in the right groin. No other complains were put forward. She had a history of an inguinal hernia mesh repair on the same side almost 4 months before. On examination, there was right iliac fossa tenderness and a hard irreducible lump in the right groin.
Investigations
Initial blood investigations showed all inflammatory markers within normal limits. Since the patient was clinically stable, she was further investigated with a CT scan prior to surgery which was reported as showing evidence of an inflamed appendix lying within a right inguinal hernia sac (figures 1–3).
Figure 1.

Sagittal section of CT scan showing the hernia.
Figure 2.

Coronal section of CT scan showing hernia with appendix inside.
Figure 3.

Transverse section of CT scan showing hernia with contents.
Treatment
As the patient was clinically and biochemically stable, a decision was made to proceed with laparoscopic resection of the appendix and repair of the hernia. Previously a right inguinal hernia open repair of the same side had been carried out, taking into account the altered anatomy due to that in the surgical region of interest, it was concluded that a laparoscopic approach will be less challenging, less invasive and will allow proper inspection of the hernia and its contents and will lead to a shorter recovery period. Another aspect to note here was that the CT had reported the appendix within a possibly recurred inguinal hernia and that too prompted the surgeon to proceed via a laparoscopic approach. It was only during the procedure that the femoral hernia was identified. Also, it was considered that delivering the appendix from the hernia via an open approach in an area of previous surgery might be difficult and would require extensive dissection and mobilisation of the structures and will lead to excessive trauma. Patient was consented and prepped for laparoscopic surgery. Under general anaesthesia, access was gained through a 10 mm port in the midline infraumbilical and left iliac fossa and a 5 mm suprapubic port. Intraoperatively, the previous hernia repair was found to be intact. The appendix along with its mesentery was found to be passing into the femoral orifice medial to the femoral vessels and hence identified as a femoral hernia (figure 4). The caecum was seen as normal. The appendix was dissected free from the sac and pulled out. It was found to be markedly inflamed; however, there were no signs of perforation, contamination or abscess formation and was subsequently resected (figures 5 and 6). The sac was pulled out and excised. Since there were no signs of contamination or perforation, that keeping in view with the clinical and biochemical picture of the patient, a decision was made for a mesh repair. The peritoneum was divided around the defect and a small composite mesh was placed and secured with a Vicryl V-lock suture with the peritoneum over it (figures 7 and 8). The cavity was washed and procedure concluded without any drains. Patient was kept on antibiotics in the postoperative period.
Figure 4.
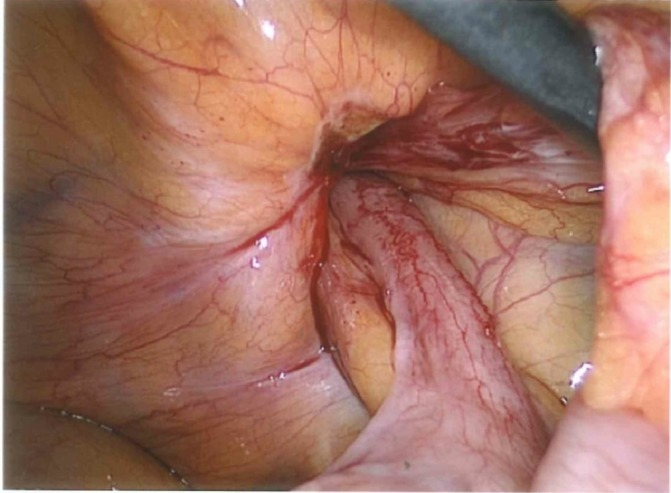
Intraoperative view of appendix going inside the hernia.
Figure 5.

Appendix released from hernia, showing evidence of inflammation.
Figure 6.
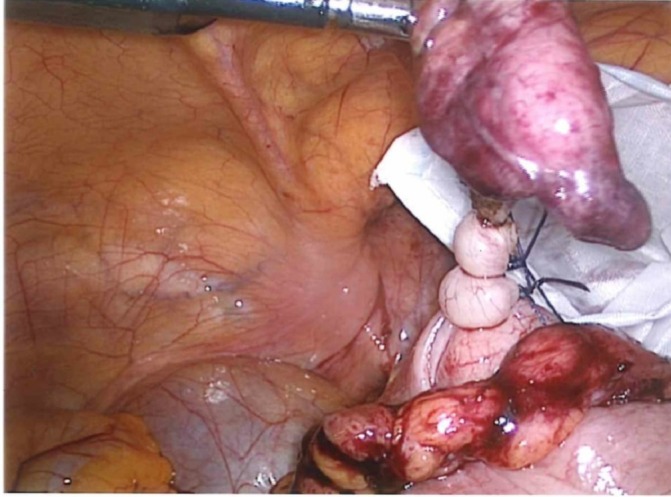
Appendix tied ready to be resected.
Figure 7.

Hernial defect seen after full reduction of the contents, dissection and appendectomy.
Figure 8.
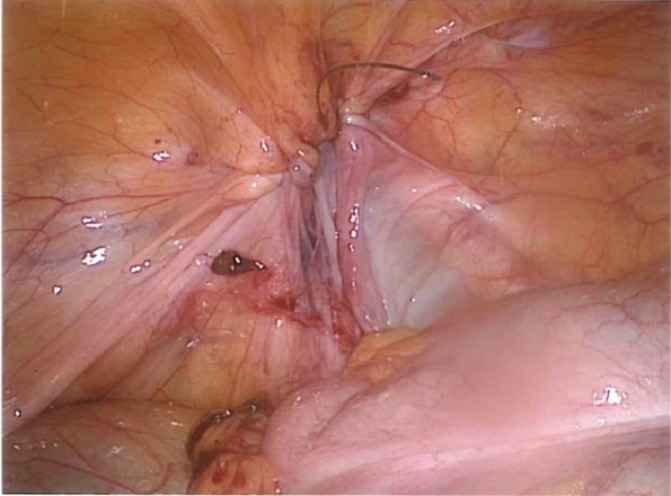
Defect repaired laparoscopically.
Outcome and follow-up
Patient was well postoperatively, and recovery was satisfactory. She was discharged on the second postoperative day after resuming base line activities.
Discussion
The presence of an inflamed appendix contained within an incarcerated femoral hernia was first described by a French surgeon Rene Jacques Croissant de Garengeot in 1731, and that is where this rare hernia gets its name from.1–3 This hernia is reported to be very rare with an incidence as low as 0.5%–3.0%, the presence of appendicitis within the femoral hernia sac is even rare with incidence reported around 0.08%–0.13%.1 4 5 Almost all the reported cases in literature were that of female patients with a predominance up to five times more than in men, with an age range from 36 years to 92 years.1–5 As in our case, presentation was that of painful groin lump without the specific symptoms of appendicitis.2 4 Preoperative diagnosis based on clinical ground is usually that of an incarcerated femoral hernia with or without bowel obstruction depending on the presentation.4 Imaging modalities are increasingly reported to be useful in the preoperative period specially with CT scanning as clinical examination alone has a limited value in determining the contents of the sac; however, in most instances, the diagnosis was made intraoperatively like in our case.5 Unlike in our case, where CT scan was not able to provide a diagnosis of the femoral hernia, it has been reported in literature to have a success rate in picking up the femoral hernia with the appendix in the sac in 44% of the patients.3 Only 17% of cases have been reported to have attained a preoperative diagnosis.1 Based on the clinical presentation, surgery can be laparoscopic, open or of combined approach; however, since this finding is so rare and is even rarely diagnosed preoperatively, there is no specific consensus on the approach and procedure.4 Various methods of treatment have been described, ranging from drainage followed by interval appendectomy for severe cases to appendectomy followed by interval hernia repair.6 7 The frequently reported procedure involves delivering the appendix from the hernia sac followed by a standard appendectomy in either approach which is followed by repair of the hernia defect. Laparoscopic approach like in our case is increasingly being reported in the literature.1 4–7 Case reports in the literature advocate the use of the transabdominal preperitoneal technique as used in this case. This is thought to be more useful in cases were a preoperative diagnosis is not available and a diagnostic followed by therapeutic laparoscopy is warranted.6 7 It seems that beginning the procedure for such cases with a laparoscopic approach can be further beneficial as it can lead to a proper assessment of the hernia and the appendix within.7 Compared with the open approach, where the position of the caecum can be a hindering factor for the appendectomy through the hernia, the laparoscopic technique nullifies this problem and so the argument can be made that laparoscopic approach should be considered first line where expertise are available, and it partly was the rationale employed in our case. The choice of laparoscopic approach is further re-enforced by the facts of shorter hospital stay, faster recovery and lower morbidity rates. A further debate which seems to arise is whether to use mesh for the hernia repair.8 Even though it is widely accepted that no foreign material should be used in the presence of infection, recent literature supports the use of mesh even in the presence of inflammation provided there is no perforation or abscess formation, in which case it is advised to delay the hernia repair or use non- absorbable sutures.2 4 5 8 The use of a biological mesh has been reported in the literature as was done in our case even in the presence of inflammation; however, its use is limited by its high cost and the fact that it should be avoided in cases where overt contamination is identified as with any other form of mesh.8 In culmination, even though the management seems simple enough when viewed separately and when described in literature, it can come off as quite a surprise especially when the surgeon is unaware of the contents of the sac preoperatively. In the absence of universal guidelines, more studies are required to look into outcomes of surgical management for this form of hernia; however, the laparoscopic approach with a mesh repair in the absence of clear contraindications is seemingly becoming the recent norm for treating this rare surgical presentation.
Learning points.
Incarcerated femoral hernia although encountered somewhat frequently in the surgical field can present with an inflamed appendix as its contents which forms a rare but important surgical pathology.
A surgeon should always be mindful of such rare hernias especially within the right clinical setting.
When in doubt, preoperative imaging can assist in identifying such hernias.
Management should be catered to each clinical scenario, following standard appendectomy either with a simple closure of defect or a mesh repair depending on the level of contamination.
The laparoscopic approach is increasingly being used in management of such cases due to well-documented advantages.
Footnotes
Contributors: SI conducted the literature review and composed the manuscript. He also took written consent from the patient. AK was the first contact with the patient, involved in preoperative workup and prepoperative and postoperative management. He also took verbal consent from the patient. DS was involved in proof reading the manuscript. SMA performed the surgery and involved in post operative management and proofreading the manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Sibona A, Gollapalli V, Parithivel V, et al. Case report: De Garengeot’s hernia. Appendicitis within femoral hernia. Diagnosis and surgical management. Int J Surg Case Rep 2016;27:162–4. 10.1016/j.ijscr.2016.08.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shum J, Croome K. Management of appendicitis in a femoral hernia. Int J Surg Case Rep 2012;3:10–11. 10.1016/j.ijscr.2011.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gülseren MO, Şimşek B, Şimşek B, et al. Incarcerated appendix within femoral hernia. Formosan Journal of Surgery 2014;47:231–2. 10.1016/j.fjs.2014.06.001 [DOI] [Google Scholar]
- 4. Garcia-Amador C, De la Plaza R, Arteaga V, et al. Garengeot’s hernia: two case reports with CT diagnosis and literature review. Open Med 2016;11:354–60. 10.1515/med-2016-0065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jin Z, Imtiaz MR, Nnajiuba H, et al. De Garengeot’s hernia: two case reports with correct preoperative identification of the vermiform appendix in the hernia. Case Rep Surg 2016;2016:2424657 10.1155/2016/2424657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Al-Subaie S, Mustafa H, Al-Sharqawi N, et al. A case of de Garengeot hernia: the feasibility of laparoscopic transabdominal preperitoneal hernia repair. Int J Surg Case Rep 2015;16:73–6. 10.1016/j.ijscr.2015.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Comman A, Gaetzschmann P, Hanner T, et al. De Garengeot hernia: transabdominal preperitoneal hernia repair and appendectomy. JSLS 2007;11:496–501. [PMC free article] [PubMed] [Google Scholar]
- 8. Klipfel A, Venkatasamy A, Nicolai C, et al. Surgical management of a De Garengeot’s hernia using a biologic mesh: a case report and review of literature. Int J Surg Case Rep 2017;39:273–5. 10.1016/j.ijscr.2017.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]


