Abstract
Background: Measures of carotid intima media thickness (cIMT) in adults are correlated with adiposity and the metabolic syndrome (MetS) and predict cardiovascular (CV) events. Relations in children are not as well studied. Our objective was to determine the relations of cIMT with body mass index (BMI) and CV risk score in children.
Methods: The study included 291 children (158 M/133 F) 6–18 years of age (140 aged 6–11/151 aged 12–18) with measurements of height, weight, waist circumference; fasting lipids, glucose, insulin, and cIMT. A CV risk cluster score was developed from sum of the z-scores of the five MetS components (waist circumference, blood pressure, serum triglycerides, high-density lipoprotein cholesterol, and insulin). Partial Pearson correlation coefficients were adjusted for age, sex, and race.
Results: There was no significant age difference in cIMT from 6 to 18 years of age. BMI and CV risk score were significantly correlated (P < 0.0001), and both were correlated with cIMT (r = 0.14, P = 0.02 and r = 0.16, P = 0.006, respectively). Slight age-related differences in associations of cIMT with CV risk score and BMI were explained by unusual values in a few children.
Conclusions: These cross-sectional data in normal children show that cIMT was stable from childhood into adolescence. However, both BMI and CV risk score had small, but significant positive correlations with cIMT. Therefore, maintaining normal levels of adiposity and other risk variables may be useful in preventing early changes associated with preclinical atherosclerosis.
Keywords: : cIMT, cardiovascular risk, children, adolescent, BMI, adiposity
Introduction
Subclinical atherosclerosis begins in early childhood and progresses into adulthood. An early manifestation of the atherosclerotic process is the accumulation of lipid in the intimal layer of arteries forming fatty streaks,1 leading to morphological changes,2 a potential impact on vascular function, and eventually leading to coronary artery disease and stroke.3 The development of atherosclerosis is accelerated in the presence of risk factors in youth, such as obesity,4–6 hypertension, dyslipidemia,7 and insulin resistance.4,7
Evidence from longitudinal adult studies has confirmed a significant relation between carotid intima media thickness (cIMT) and development of myocardial infarction and stroke.8–10 Data on cIMT are less clear in pediatric populations. Cross-sectional studies in children published by our group and others have shown significant relations for cIMT with obesity, blood pressure, metabolic syndrome (MetS), visceral adipose tissue, and insulin resistance,11–13 and persistence of cardiovascular (CV) risk factors in childhood has been associated with cIMT in adulthood.14–20 Others have shown increased cIMT in high-risk adolescents with diabetes and chronic kidney disease.21
Despite these prior studies, there continues to be a lack of information on cIMT during development of healthy children and adolescents and conflicting information on cIMT differences between healthy lean adolescents and adolescents with obesity or MetS.11,13 Defining the age course of cIMT and cIMT relations with presumed risk factors before adulthood is relevant to the early clinical approach to preventive cardiology and longitudinal studies of cIMT from childhood into adulthood. In this study, we focus on healthy children and adolescents to provide new data on the cIMT growth curve and on the association of cIMT with a CV risk cluster score and body mass index (BMI).
Materials and Methods
The study protocol was approved by the University of Minnesota Institutional Review Board, and consent/assent was obtained from parents/participants, respectively. Data were collected in 2007–2012 from participants in a community-based study evaluating cardiometabolic risk in healthy children who were the offspring of parents recruited when they were children in the 1970s.22 Participants included were nondiabetic, free from chronic diseases, and were not taking medications known to influence vascular function and/or glucose metabolism; no potential participants were excluded for these reasons. All testing were performed in the morning after an overnight fast (including no caffeine consumption) of at least 8 hr. Height was measured using a wall-mounted stadiometer and weight with an electronic scale. BMI was calculated as body weight in kilograms divided by height in meters squared. BMI percentiles were determined using age and sex-based Centers for Disease Control definitions.23 Blood pressure was measured twice on the right arm using a digital blood pressure monitor after participants were sitting in a quiet room for at least 5 min, and an average of the two values was reported for systolic blood pressure and diastolic blood pressure. A fasting lipid profile [total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol, triglycerides (TG)], and fasting insulin and glucose were measured using standard procedures in the Fairview Diagnostic Laboratories at the Fairview University Medical Center (Minneapolis, Minnesota), a Center for Disease Control and Prevention-certified laboratory.
As previously reported,24 we developed a CV risk cluster score, consisting of the average of standardized deviates of the primary components of the MetS (i.e., the sum of the z scores of waist circumference, SBP, TG, inverse HDL-C, and fasting glucose divided by 5. As base values, we used means and standard deviations for the five MetS components at mean age 11.7 and 22 years, namely the mean age of the cohort. Thus, the score at any age can be computed as: 1/5*[(waist circumference-77.7)/11.4 − (HDL-C-44.6)/10.2 + (TG-90.5)/52.9 + (SBP-107.6)/9.2 + (glucose-88.2)/7.4]. The concept allows the score to grow with age and changes in the MetS components by inserting the observed values of waist circumference, HDL-C, TG, SBP, and fasting glucose for that age into the formula. A higher z-score indicates that the components tend to cluster in the higher sections of the distributions, that is, represent overall higher risk. While it is theoretically possible that a high cluster score could arise from an extreme value of a single component, we verified that high scores are almost always the result of high values in two or more components.
Images for determining cIMT were obtained at end diastole (gated by R-wave on electrocardiography) using B-mode images obtained at the distal 10 mm of the left common carotid artery, as recommended by pediatric guidelines.11 An electronic wall-tracking software program was used for the analysis of cIMT. Our laboratory has previously documented satisfactory reproducibility for measurement of cIMT, with the mean difference for repeated measurements on separate days in the same subject of 0.02 ± 0.03 mm.25
Statistical analyses
Demographic, anthropometric, and cardiometabolic differences across age group were compared by paired t-test. Data were examined using both continuous and categorical analyses. Variables that were not normally distributed (i.e., fasting insulin, TG) were log transformed. However, because results were not qualitatively different from those using nontransformed data, nontransformed data were presented for simplicity and were used for the calculation of the CV cluster score.
cIMT was analyzed by ANCOVA using linear mixed models to adjust for sex, age, and race. We studied the linearity assumption made in computing correlations by examining data in categories. The data analysis for this article was generated using SAS software. Copyright© SAS Institute, Inc., Cary, NC. Significance was set at an alpha level of P < 0.05.
Results
Demographic and clinical characteristics of the study population are displayed in Table 1. A total of 291 children (158 males), 55% Caucasian, 31% Black, 14% other, with age range 6–18 years, mean age 11.7 years, were included in the study. Given the wide age range, participants were divided into childhood (younger children) (age 6–11) and adolescent (older children) (age 12–18) groups. The gender distribution was similar between the two age groups. While the mean BMI percentile was slightly higher in adolescents (with borderline significance), the mean waist circumference, systolic blood pressure, fasting insulin, CV risk cluster score, and cIMT were significantly greater in the adolescents than younger children. As shown in Table 2, there were significant differences in cIMT between ages 6–18 years, however, there was no clear progression with age and there was no significant age effect (P = 0.08).
Table 1.
Descriptive Characteristics of the Cohort
| Participants: age variables | All (6–18 years) n = 291, mean ± SD | Younger (6–11 years) n = 140, mean ± SD | Older (12–18 years) n = 151, mean ± SD | P-value (where appropriate) |
|---|---|---|---|---|
| Caucasian, n (%) | 161 (55) | 98 (70) | 63 (42) | |
| Black, n (%) | 89 (31) | 27 (19) | 62 (41) | |
| Native American, n (%) | 11 (4) | 5 (4) | 6 (4) | |
| Asian, n (%) | 10 (3) | 4 (3) | 6 (4) | |
| Hispanic, n (%) | 2 (1) | 0 (0) | 2 (1) | |
| Other, n (%) | 18 (6) | 6 (4) | 12 (8) | |
| Gender, n (%) | Male: 158 (54) | Male: 78 (56) | Male: 158 (54) | |
| Female: 133 (46) | Female: 62 (44) | Female: 133 (46) | ||
| BMI (kg/m2) | 21.3 ± 6.3 | 17.9 ± 3.4 | 24.4 ± 6.6 | <0.0001 |
| BMI percentile | 64.7 ± 29.7 | 61 ± 29.2 | 68 ± 29.9 | 0.047 |
| Overweight (BMI 85th percentile–95th percentile), n (%) | 52 (17.9) | 24 (17.1) | 28 (18.5) | |
| Obese (BMI ≥95th percentile), n (%) | 54 (18.6) | 16 (11.4) | 38 (25.2) | |
| Waist (cm) | 72.7 ± 16.1 | 63.5 ± 10.1 | 81.1 ± 15.9 | <0.0001 |
| SBP (mm Hg) | 104 ± 10 | 100 ± 9.1 | 107 ± 9.7 | <0.0001 |
| DBP (mm Hg) | 57 ± 7 | 56 ± 6.8 | 59 ± 7.7 | 0.003 |
| Fasting insulin (μU/L) | 7.7 ± 7.4 | 4.6 ± 5.5 | 10.5 ± 7.8 | <0.0001 |
| Total-C (mg/dL) | 154.4 ± 28.1 | 160 ± 28.3 | 149 ± 26.9 | 0.0006 |
| LDL-C (mg/dL) | 88.5 ± 23.7 | 93 ± 23.2 | 84 ± 23.3 | 0.0008 |
| HDL-C (mg/dL) | 51.1 ± 11.8 | 54 ± 10.9 | 48 ± 12.1 | <0.0001 |
| TG (mg/dL) | 73.9 ± 38.9 | 65 ± 28.4 | 82 ± 45 | 0.0001 |
| Fasting glucose (mg/dL) | 76.9 ± 13.8 | 69 ± 13.1 | 84 ± 10.2 | <0.0001 |
| CV risk cluster score with waist | 0.03 ± 0.6 | −0.4 ± 0.5 | 0.38 ± 0.5 | <0.0001 |
| cIMT (mm) | 0.45 ± 0.04 | 0.44 ± 0.04 | 0.45 ± 0.04 | 0.9 |
SD, standard deviation; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; Total-C, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglyceride; cIMT, carotid intima media thickness; CV, cardiovascular.
Table 2.
Carotid Intima Media Thickness by Age in Children and Adolescents
| Age (years) | N | cIMT mean (mm) ± SE | P |
|---|---|---|---|
| 6 | 31 | 0.44 ± 0.007 | <0.0001 |
| 7 | 24 | 0.44 ± 0.008 | <0.0001 |
| 8 | 22 | 0.46 ± 0.009 | <0.0001 |
| 9 | 22 | 0.44 ± 0.008 | <0.0001 |
| 10 | 23 | 0.44 ± 0.008 | <0.0001 |
| 11 | 18 | 0.48 ± 0.009 | <0.0001 |
| 12 | 18 | 0.45 ± 0.009 | <0.0001 |
| 13 | 22 | 0.44 ± 0.008 | <0.0001 |
| 14 | 28 | 0.44 ± 0.007 | <0.0001 |
| 15 | 26 | 0.44 ± 0.008 | <0.0001 |
| 16 | 20 | 0.44 ± 0.009 | <0.0001 |
| 17 | 17 | 0.44 ± 0.010 | <0.0001 |
| 18 | 20 | 0.44 ± 0.009 | <0.0001 |
SE, standard error.
There was a significant correlation between BMI and the CV risk score (r = 0.61, P < 0.0001). Although deleting waist from the CV risk score attenuated the correlation with BMI, it remained highly significant (r = 0.43, P < 0.0001).
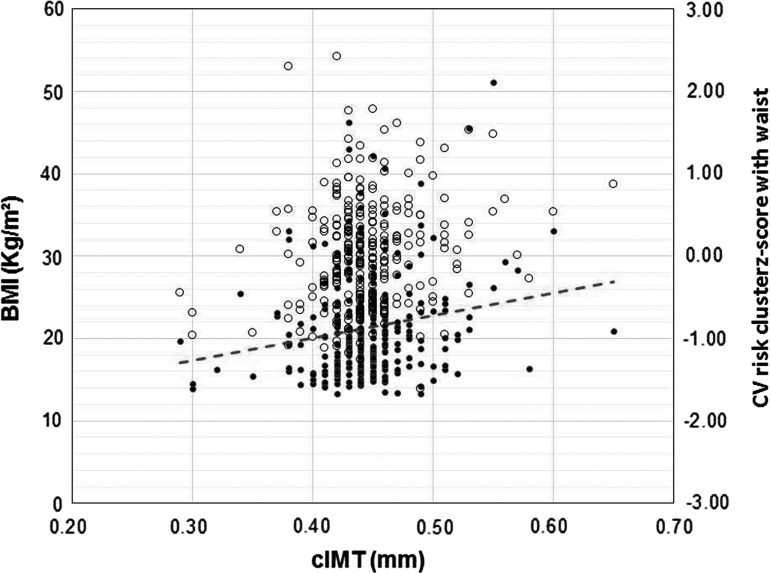
The correlations of cIMT with BMI and the CV cluster score are shown in Table 3. In analyses of the total cohort, cIMT had a weak but significant association with BMI (r = 0.14, P = 0.02; Table 3 and Fig. 1) and the CV risk cluster (r = 0.16, P = 0.006). Due to the wide age range (6–18 years) of the cohort, we examined the relations among cIMT, adiposity, and CV risk scores separately in the younger (age 6–11 years, n = 140) and older (age 12–18 years, n = 151) children (Table 3). In interpreting the apparent lack of correlation in BMI with cIMT in 6–11 year olds we should exercise caution, since it might have been influenced by the eight children with mean BMI = 27.2 and with surprisingly low cIMT, relative to the linear trends observed in children with lower BMI.
Table 3.
Relation of Carotid Intima Media Thickness to Body Mass Index and Cardiovascular Risk Cluster Score by Age Group
| Total cohort N = 291 | cIMT | BMI r = 0.14; P = 0.02 | CV risk cluster score r = 0.16; P = 0.01 |
|---|---|---|---|
| Age 6–11 years, N = 140 (48%) | cIMT | r = 0.04; P = 0.65* | r = 0.20; P = 0.02 |
| Age 12–18 years, N = 151 (52%) | cIMT | r = 0.21; P = 0.01 | r = 0.14; P = 0.10 |
CV risk cluster score included the sum of the z scores of waist circumference, SBP, triglycerides, inverse HDL-C and fasting glucose divided by 5. Analyses were adjusted for sex, race, and age.
This was considered unreliable due to outliers. After elimination of the outliers, the correlation coefficient r improved (r = 0.16), but P-value was still not significant (P = 0.07).
FIG. 1.
Filled–BMI, unfilled–CVR cluster score with waist. BMI, body mass index; CV risk, cardiovascular risk; cIMT, carotid intima media thickness.
Discussion
In this cross-sectional study in healthy youth we found that cIMT did not change significantly between childhood and adolescence. The literature is inconsistent regarding cIMT changes in healthy children. The age trend of cIMT in a cohort of 1100 healthy children from the largest currently available pediatric study26 was positive but small, supporting our hypothesis that changes in vascular morphology progress slowly. Conversely, a report in 280 healthy Brazilian children, in whom cIMT measured at the distal 10 mm of the far wall of both the right and left common carotid artery, was constant in children younger than 10 years, but increased significantly between ages 10–15 years.27 This variability, although small, may be related to variations in cIMT measurement site and method or to differences in population characteristics.
Studies in obese and diabetic youth have found that the earliest atherosclerotic changes in cIMT occur at the carotid bulb and internal carotid artery,11 suggesting that measurements in these carotid locations in the Brazilian study, rather than only at the left common cIMT used in our and previous studies25 in healthy children, may have resulted in the age-related increases in cIMT. Increased cIMT has been reported in children with traditional CV risk factors, such as obesity, hypertension, and chronic kidney disease.28–31 Contrary to a previous study showing lack of association between cIMT and BMI in healthy children less than 15 years of age,27 we observed an association between cIMT and both BMI and CV risk cluster score. While the association with BMI was stronger in adolescents (age 12–18) than in young children, cIMT showed stronger association with the CV risk score in younger children (age 6–11). These findings persisted after excluding waist circumference from the CV risk score analyses, suggesting that a CV risk score of traditional CVD risk factors, independent of adiposity, is related to cIMT. However, we acknowledge that all CV risk factors may be confounded by waist, and simply excluding waist from the CV risk score may not remove its total influence on CV risk.
Notably, in the majority of the existing literature in children, associations of cIMT and adiposity are compared between lean and obese youth.32 In the current study, despite the overwhelming majority of youth being nonobese and generally healthy, the fact that both major concepts of what might constitute adult risk (BMI and CV risk score) correlated with cIMT is important in the notion of primary prevention of CVD. Therefore, maintaining normal levels of adiposity and other risk variables may be useful in preventing early changes associated with preclinical atherosclerosis.
The most unique finding is the lack of growth in cIMT during childhood and adolescence in healthy youth, despite growth in body size. Although the idea that childhood obesity and MetS features are somewhat predictive of cIMT is less novel, the study provides insight in important features of growth and biology.
Some limitations of this study should be considered. Differences among the younger and older children in the acquisition of data did not allow complete comparisons of some variables, such as Tanner stage and socioeconomic status. By virtue of this being an observational study, we cannot exclude residual confounding or make definitive statements regarding causality. Nevertheless, data are consistent with the notion that excess adiposity in childhood and adolescence is related to higher levels of MetS-related variables and with concurrently measured cIMT throughout childhood and adolescence. These concepts are also consistent with recommendations to maintain normal BMI during these critical periods of growth.
Acknowledgments
National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases R01DK072124 (J.S.), the National Center for Research Resources Grants 1UL1RR033183 to the University of Minnesota Clinical and Translational Science Institute, and the General Clinical Research Center Program M01-RR00400, and T32DK65519)–Dr. J.S., MD, MS.
Author Disclosure Statement
No conflicting financial interests exist. No honorarium, grant, or other form of payment was given to anyone to produce the article.
References
- 1.McGill HC., Jr. The pathogenesis of atherosclerosis. Clin Chem 1988;34:B33–B39 [PubMed] [Google Scholar]
- 2.Ross R. Atherosclerosis is an inflammatory disease. Am Heart J 1999;138:S419–S420 [DOI] [PubMed] [Google Scholar]
- 3.Libby P. Inflammation in atherosclerosis. Nature 2002;420:868–874 [DOI] [PubMed] [Google Scholar]
- 4.Raghuveer G. Lifetime cardiovascular risk of childhood obesity. Am J Clin Nutr 2010;91:1514S–1519S [DOI] [PubMed] [Google Scholar]
- 5.Freedman DS, Patel DA, Srinivasan SR, et al. . The contribution of childhood obesity to adult carotid intima-media thickness: The Bogalusa Heart Study. Int J Obes (Lond) 2008;32:749–756 [DOI] [PubMed] [Google Scholar]
- 6.Berenson GS, Srinivasan SR, Bao W, et al. . Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med 1998;338:1650–1656 [DOI] [PubMed] [Google Scholar]
- 7.Le J, Zhang D, Menees S, et al. . “Vascular age” is advanced in children with atherosclerosis-promoting risk factors. Circ Cardiovasc Imaging 2010;3:8–14 [DOI] [PubMed] [Google Scholar]
- 8.Chambless LE, Heiss G, Folsom AR, et al. . Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: The Atherosclerosis Risk in Communities (ARIC) Study, 1987–1993. Am J Epidemiol 1997;146:483–494 [DOI] [PubMed] [Google Scholar]
- 9.Lorenz MW, Markus HS, Bots ML, et al. . Prediction of clinical cardiovascular events with carotid intima-media thickness: A systematic review and meta-analysis. Circulation 2007;115:459–467 [DOI] [PubMed] [Google Scholar]
- 10.O'Leary DH, Polak JF, Kronmal RA, et al. . Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med 1999;340:14–22 [DOI] [PubMed] [Google Scholar]
- 11.Urbina EM, Kimball TR, McCoy CE, et al. . Youth with obesity and obesity-related type 2 diabetes mellitus demonstrate abnormalities in carotid structure and function. Circulation 2009;119:2913–2919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gidding SS, Daniels SR. Obesity, vascular changes, and the development of atherosclerosis. J Pediatr 2016;168:5–6 [DOI] [PubMed] [Google Scholar]
- 13.Iannuzzi A, Licenziati MR, Acampora C, et al. . Carotid artery wall hypertrophy in children with metabolic syndrome. J Hum Hypertens 2008;22:83–88 [DOI] [PubMed] [Google Scholar]
- 14.Freedman DS, Dietz WH, Tang R, et al. . The relation of obesity throughout life to carotid intima-media thickness in adulthood: The Bogalusa Heart Study. Int J Obes Relat Metab Disord 2004;28:159–166 [DOI] [PubMed] [Google Scholar]
- 15.Magnussen CG, Venn A, Thomson R, et al. . The association of pediatric low- and high-density lipoprotein cholesterol dyslipidemia classifications and change in dyslipidemia status with carotid intima-media thickness in adulthood evidence from the cardiovascular risk in Young Finns study, the Bogalusa Heart study, and the CDAH (Childhood Determinants of Adult Health) study. J Am Coll Cardiol 2009;53:860–869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Magnussen CG, Cheriyan S, Sabin MA, et al. . Continuous and dichotomous metabolic syndrome definitions in youth predict adult type 2 giabetes and carotid artery intima media thickness: The cardiovascular risk in Young finns Study. J Pediatr 2016;171:97–103 e1–e3 [DOI] [PubMed] [Google Scholar]
- 17.Juonala M, Magnussen CG, Berenson GS, et al. . Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med 2011;365:1876–1885 [DOI] [PubMed] [Google Scholar]
- 18.Raitakari OT, Juonala M, Kahonen M, et al. . Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: The cardiovascular risk in Young Finns Study. JAMA 2003;290:2277–2283 [DOI] [PubMed] [Google Scholar]
- 19.Davis PH, Dawson JD, Riley WA, et al. . Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation 2001;104:2815–2819 [DOI] [PubMed] [Google Scholar]
- 20.Ryder JR, Dengel DR, Jacobs DR Jr., et al. . Relations among adiposity and insulin resistance with flow-mediated dilation, carotid intima-media thickness, and arterial stiffness in children. J Pediatr 2016;168:205–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mitsnefes MM. Understanding carotid artery intima-media thickness in childhood: Lessons from studies in children with renal transplants. Pediatr Transplant 2008;12:377–380 [DOI] [PubMed] [Google Scholar]
- 22.Steffen LM, Sinaiko AR, Zhou X, et al. . Relation of adiposity, television and screen time in offspring to their parents. BMC Pediatr 2013;13:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, et al. . 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11 2002;246:1–190 [PubMed] [Google Scholar]
- 24.Kelly AS, Steinberger J, Jacobs DR, et al. . Predicting cardiovascular risk in young adulthood from the metabolic syndrome, its component risk factors, and a cluster score in childhood. Int J Pediatr Obes 2011;6:e283–e289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dengel DR, Jacobs DR, Steinberger J, et al. . Gender differences in vascular function and insulin sensitivity in young adults. Clin Sci (Lond) 2011;120:153–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Doyon A, Kracht D, Bayazit AK, et al. . Carotid artery intima-media thickness and distensibility in children and adolescents: Reference values and role of body dimensions. Hypertension 2013;62:550–556 [DOI] [PubMed] [Google Scholar]
- 27.Baroncini LA, Sylvestre Lde C, Pecoits Filho R. Assessment of intima-media thickness in healthy children aged 1–15 years. Arq Bras Cardiol 2016;106:327–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Urbina EM, Williams RV, Alpert BS; American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young. Noninvasive assessment of subclinical atherosclerosis in children and adolescents: Recommendations for standard assessment for clinical research: A scientific statement from the American Heart Association. Hypertension 2009;54:919–950 [DOI] [PubMed] [Google Scholar]
- 29.Brady TM, Schneider MF, Flynn JT, et al. . Carotid intima-media thickness in children with CKD: Results from the CKiD study. Clin J Am Soc Nephrol 2012;7:1930–1937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gazolla FM, Neves Bordallo MA, Madeira IR, et al. . Association between cardiovascular risk factors and carotid intima-media thickness in prepubertal Brazilian children. J Pediatr Endocrinol Metab 2015;28(5–6):579–587 [DOI] [PubMed] [Google Scholar]
- 31.Melo X, Santa-Clara H, Santos DA, et al. . Single and combined effects of body composition phenotypes on carotid intima-media thickness. Pediatr Obes 2016;11:272–278 [DOI] [PubMed] [Google Scholar]
- 32.Park MH, Skow Á, De Matteis S, et al. . Adiposity and carotid-intima media thickness in children and adolescents: A systematic review. BMC Pediatr 2015;15:161. [DOI] [PMC free article] [PubMed] [Google Scholar]