Abstract
Despite evidence that a greater focus on couples could strengthen HIV prevention efforts, little health-related research has explored relationship functioning and relationship quality among couples in Africa. Using data from 162 couples (324 individuals) resident in a peri-urban Ugandan community, we assessed actor and partner effects of sexual risk behaviors on relationship quality, using psychometric measures of dyadic adjustment, sexual satisfaction, commitment, intimacy, and communication. For women and men, poor relationship quality was associated with having concurrent sexual partners and suspecting that one’s partner had concurrent sexual partners (actor effects). Women’s poor relationship quality was also associated with men’s sexual risk behaviors (partner effects), although the inverse partner effect was not observed. These findings suggest that relationship quality is linked to HIV risk, particularly through the pathway of concurrent sexual partnerships, and that positive relationship attributes such as sexual satisfaction, intimacy, and constructive communication can help couples to avoid risk.
Keywords: HIV prevention, behavior change, couple relationship quality, concurrent sexual partnerships, alcohol
Introduction
Globally, HIV prevention efforts continue to focus on the individual rather than the “micro-social” context of the couple relationship within which risk behaviors occur (1). In sub-Saharan Africa, scant health-related research has explored couple functioning apart from specific behaviors such as intimate partner violence, HIV testing, and higher-risk sexual behaviors. While few tools to measure couple relationship quality and satisfaction have been validated in African contexts, some studies have found linkages between relationship quality and HIV risk behaviors using psychometric measures. In Kenya, married couples in fishing communities were more likely to report concurrent sexual partners if they reported low marital sexual satisfaction (2). In South Africa, couples who reported lower confidence in their ability to communicate about sexual risk reduction were also less likely to report consistent condom use, suggesting the need to build communication skills to reduce sexual risk (3). A study among HIV sero-positive and sero-discordant couples in Zambia found that individuals who reported higher relationship quality were less likely to report having multiple partners and more likely to report consistent condom use (4). One of the few studies that has examined how partners influence each other’s relationship quality in an African population found that South African men’s more equitable gender norms positively influenced their female partners’ relationship quality (5).
The current study was carried out in Uganda, where the majority of HIV transmission is through heterosexual sex (6) and the 2011 national sero-prevalence survey found that among adults aged 15–49, 8.2% of women and 6.1% of men were living with HIV (7). In the late 1980s and 1990s Ugandans achieved an unprecedented reversal of a high-prevalence generalized HIV epidemic (8). HIV incidence likely began to decline in the late 1980s (8), and national HIV prevalence fell from 18% in 1992 to 6% in 2002 (7). The elements of Uganda’s success have been identified as “communication, behavior change, and care,” rooted in community action rather than externally-funded interventions and resulting in a “social vaccine” with an estimated 75% efficacy (9, pp. 165–166). The main behavior change message was to reduce one’s number of sexual partners (10,11), and when Ugandans were asked in 1995 how they had changed their behavior in response to AIDS, more than half reported “sticking to one sexual partner” (65% of all married men) or abstaining from sex entirely (38% of all unmarried men) (9). Epidemiological data confirm this widespread behavior change, and between 1989 and 1995 the number of Ugandans reporting casual sexual partnerships declined by 60% (12). This decline in multiple sexual partners has been defined as the critical factor in changing the course of Uganda’s HIV epidemic (12,13).
More recently, gains made against the HIV epidemic have stagnated, with risky sexual behaviors including multiple sexual partners increasing nationally between 1989 and 2005 (14). Subsequently, HIV prevalence increased slightly between the 2004/5 and 2011 national sero-behavioral surveys, from 6.4% to 7.3%; concurrently, antiretroviral therapy was also introduced. Also during this period, our research in the current study community found that a majority of women and men were in a sexual partnership that they knew or suspected to be non-exclusive (due to their own or their partners’ concurrent sexual partnerships), and those who perceived AIDS to be more severe were less likely to report multiple and concurrent sexual partners (15). Members of the study community reported that they mainly heard HIV prevention messages centered on condoms and testing, a marked shift from the partner reduction messages common during the years in which HIV incidence was declining in Uganda (16). In focus groups, members of the study community reported that people no longer feared HIV as they had during the epidemic’s peak and that this had led to riskier sexual behavior (17).
Previous qualitative research in Uganda has confirmed that poor relationship quality can be a risk factor for HIV infection and present a barrier to effective HIV prevention. In rural Rakai, a qualitative case-control study which investigated differences between HIV-positive cases and HIV-negative controls using life history interviews identified differences only in the realm of sexual relationships, with cases reporting poorer communication and less trust of partners (18). Men in rural eastern Uganda stated in focus groups that they were dissuaded from seeking HIV testing because they perceived their relationships as lacking in trust and feared that testing would create conflict (19). Women and men in rural southwestern Uganda reported during in-depth interviews that although they valued commitment and fidelity in relationships, these values were challenged by negative realities such as lack of love and affection, and for women by men’s lack of material support (20). Quantitative research in Uganda has also revealed the extent to which risk of sexual violence for women living with HIV is rooted in relationship dynamics, specifically lack of relationship power and control (21).
In the current study, we attempted to build on previous research by using psychometric measures to assess relationship quality and increase our understanding of various dimensions of couple relationships among women and men in a peri-urban Ugandan community. We also assessed sexual risk behaviors and associations between relationship quality and risk factors for HIV transmission such as multiple and concurrent sexual partnerships, lack of condom use, and alcohol use. Multiple and concurrent sexual partnerships have been identified as a key driver of HIV transmission in generalized HIV epidemics such as Uganda’s, based on epidemiological evidence that concurrent sexual partnerships greatly increase the potential for epidemic spread and that a major proportion of HIV transmission is attributable to concurrency among both concordant negative and discordant couples (22). We posited that couples with higher relationship quality in domains such as communication, trust, intimacy, and sexual satisfaction would be less likely to engage in HIV risk behaviors such as having multiple and concurrent sexual partnerships, and might also be less likely to have other risk factors such as alcohol use.
Methods
Study procedures
We carried out this study in Tebuyoleka Zone, Bwaise II Parish, Kawempe Division, Uganda. Kawempe Division is a high-density, low-income, peri-urban area of Kampala, with a population of approximately 250,000 and more than 8000 people per square kilometer. We obtained permission for the study from the Resident District Commissioner of Kawempe Division and the local leadership of Tebuyoleka Zone. The local leaders were strongly supportive of the study, as they have been for previous studies conducted by the same research team in this community (15,17,23).
Participants were eligible if they identified as currently being in a cohabiting or married relationship, were aged 20–49 years (both partners), currently resided in the study area, and both they and their spouses or partners consented to participate in the study. While individuals in polygamous unions were included in the study, we enrolled into the study only one female spouse or partner per man. Community leaders drew up a list of 200 eligible couples and research assistants then went to the homes of these couples to explain the study and enroll participants. Although we did not have a complete listing or census of residents, we believe based on conversations with community leaders that these 200 couples came close to constituting a total sample of all eligible couples in Tebuyoleka Zone and thus are generally representative of the community. We enrolled 162 of these 200 couples (324 individuals) into the study.
Members of the study team carried out face-to-face interviews at the participants’ homes at a time when privacy could be ensured using a paper questionnaire. Interviews were conducted in English or Luganda, according to the preference of the participant. Participants gave written informed consent before the interview, and were also invited to attend a 3-session couple relationship strengthening intervention. All data presented are from the baseline survey, which was conducted before the intervention.
Measures
The survey questionnaire included questions about demographic factors, sexual risk behaviors, and an assessment of couple relationship satisfaction and quality. We considered four sexual risks behaviors in this analysis: having a concurrent sexual partner, having sex with someone believed or suspected to have concurrent sexual partners, lack of condom use, and alcohol use with sex. We defined concurrent sexual partners as sexual partners in addition to one’s regular sexual partner or spouse(s), and did not consider polygamous men to have concurrent sexual partners if they reported having sex only with their wives. We considered as a sexual risk behavior having sex with someone believed or suspected to have concurrent sexual partners (i.e. answering “yes” or “don’t know” to the question, “In the past 6 months, do you think your wife/husband or cohabiting partner has had another sexual partner besides you?” and not counting the 2 women who reported themselves to be in a polygamous relationship). We assessed condom use by asking participants whether they never, sometimes, or always used condoms. Participants also reported whether at last sex with their primary partners, they or their partners had used alcohol to the extent that either partner was drunk. For simplicity, we report this variable as “alcohol use with sex.”
Relationship satisfaction and quality were assessed with a number of psychometric measures. We chose these measures by first identifying through a literature review any measures that had been previously used in Africa. The study team, which included Ugandans and Americans, then discussed which domains of relationship functioning were most important to address, based on our knowledge of Ugandan culture and previous experience with the study population. We adapted the measures to make them more culturally appropriate and understandable to the study population and shortened some scales to reduce the length of the research interview. We pilot tested the questionnaire in a community similar to the study community and made further minor changes based on the pilot test. The pilot test demonstrated the challenge of persuading participants to complete a lengthy research interview, and confirmed our decision to shorten some relationship quality scales rather than risk incomplete interviews and compromised data quality.
Dyadic adjustment
We adapted the Dyadic Adjustment Scale (DAS), one of the most widely used measures of overall dyadic adjustment and relationship satisfaction. The DAS was developed to be used with cohabiting or married couples and contains 32 items in 4 subscales measuring dyadic satisfaction, dyadic cohesion, dyadic consensus and affectional expression (24). Items have Likert-scale or binary responses, and the entire DAS has a score range of 0 to 151, with higher scores indicating greater dyadic adjustment and relationship quality. We preserved the original scoring but dropped the question, “Do you kiss your mate?” as we thought it was not an accurate measure of affection in the cultural context of the study community. We also removed items which asked about agreement between partners on “matters of recreation” and “philosophy of life,” as we felt these phrases would not be relevant or understood by study participants. Finally, in a section which asked how often a couple engaged in various activities together, we added two items about the following activities: “work together on caring for the children” and “work together on household chores or duties.” Based on our knowledge of the cultural context of the study community, we felt that these activities were important measures of couple cohesion. The revised version of the DAS used in this study had 31 items and a score range of 0 to 147, which we rescaled to have a range of 0 to 100. Cronbach’s alpha for the 31-item scale was 0.88.
Sexual satisfaction subscale
We adapted a sexual satisfaction subscale from the 25-item Index of Sexual Satisfaction (ISS), which assesses sexual satisfaction with one’s partner using 25 items (some reverse-scored) ranked on a 5-point Likert scale (25). We determined that 25 items were too many given our goal of limiting the length of the research interview, so we retained 14 items which we thought were most culturally relevant to the study population. The original ISS had a score range of 0 to 100, with higher scores denoting problems in the sexual relationship. The revised ISS used in this study had a score range of 0 to 56, which we reverse-scored so that higher scores denoted higher quality relationship and rescaled to a range of 0 to 100. Cronbach’s alpha for the 14-item scale was 0.40.
Commitment and intimacy subscales
We adapted the decision/commitment and intimacy subscales from Sternberg’s triangular love scale, which includes subscales for three components of romantic love: intimacy, passion, and decision/commitment (26). Both the decision/commitment and intimacy subscales included 15 items, ranked on a 9-point Likert scale. We dropped 7 items from each scale, retaining for each scale the 8 items which seemed most culturally relevant to the study population. We then rescored the scales to be consistent with the other scales used, so that each scale had a range of 0 to 100 with higher values denoting higher relationship quality. Cronbach’s alpha for the 8-item commitment scale was 0.93 and for the 8-item intimacy scale was 0.88.
Communication subscale
Communication was measured using two subscales from the Communication Patterns Questionnaire (27). Three items assess positive communication patterns and four items assess destructive communication patterns, and all are scored on a 9-point Likert scale. We retained all 7 items and made no changes to wording. The original scales are scored by subtracting the score on the destructive communication patterns subscale from the score on the positive communication patterns subscale, creating a score range of −33 to 23. We instead reverse-scored the items assessing destructive communication patterns, so that higher scores denoted more positive communication. We then combined the scores for the positive and negative communication subscales and rescaled them to have a range of 0 to 100. Cronbach’s alpha was 0.78 for the 3-item positive communication scale, 0.63 for the 4-item destructive communication scale, and 0.69 for the combined 7-item scale.
Statistical analysis
We used Stata version 14 (StataCorp LP, College Station, Texas) for all analyses. We carried out descriptive and bivariate analyses of demographic characteristics, sexual risk behaviors, and relationship quality measures. To examine differences by gender, we used paired t-tests for linear variables and McNemar’s chi-square test for categorical variables. To examine differences by marital status (all variables categorical) we used chi-squared statistics or Fisher’s exact test in the case of one or more empty cells. For each relationship quality scale, we calculated Cronbach’s alpha (a measure of internal reliability) for all participants as well as for 4 sub-groups: cohabiting women, married women, cohabiting men, and married men. We calculated Pearson’s correlation (r) to assess pairwise bivariate correlations between all relationship variables, including as a measure of non-independence of relationship quality scores of partners.
In order to evaluate the performance of each scale, we carried out confirmatory factor analysis of each relationship quality scale using Stata 14’s GSEM command. We omitted items with very low standardized factor loadings (< 0.20) and non-significant p-values (p > .05), and used Cronbach’s alpha to compare the reliability of the shortened versus original scales. These criteria indicated removing one item from the communication scale (increasing coefficient alpha from .69 to .73), but structural equation models using the shortened 6-item communication scale failed to converge, so we retained the original 7-item communication scale. We omitted 6 items from the 14-item sexual satisfaction scale, increasing coefficient alpha from .40 to .59 for the shortened 8-item scale, and used this shortened scale in all further analysis. No other changes were made to scales. We recalculated each relationship quality scale to have a range of 0 to 100, with higher values denoting higher relationship quality. Finally, relationship quality scores were centered around the grand mean (the mean of both women’s and men’s scores).
For our primary analysis, we used the Actor-Partner Interdependence Model (APIM) (28) to evaluate hypothesized actor and parther effects of relationship quality on sexual risk behaviors. We used the scores from the revised relationship quality scales in structural equation models (SEM) which included the effect of each partner’s relationship quality on his or her own sexual behavior (actor effect) and on the partner’s sexual behavior (partner effect) (Figure 1). Kenny et al. (28) recommend SEM as the preferred approach for distinguishable dyads such as heterosexual couples. Including both actor and partner effects in the same model allows for analysis of interdependence in the couple. Modeling the relationship construct as a latent variable comprised of individual scale items created too many degrees of freedom for the model to converge, so we used a summary score for each relationship quality domain. The final models thus contained no latent variables. The outcome variables (sexual risk behaviors) were dichotomous and thus did not contain error terms, so the models could not correlate outcome variables within couples. All models utilized maximum likelihood estimation and were created using Stata 14’s GSEM command, which can accommodate non-linear outcome variables.
Figure 1.
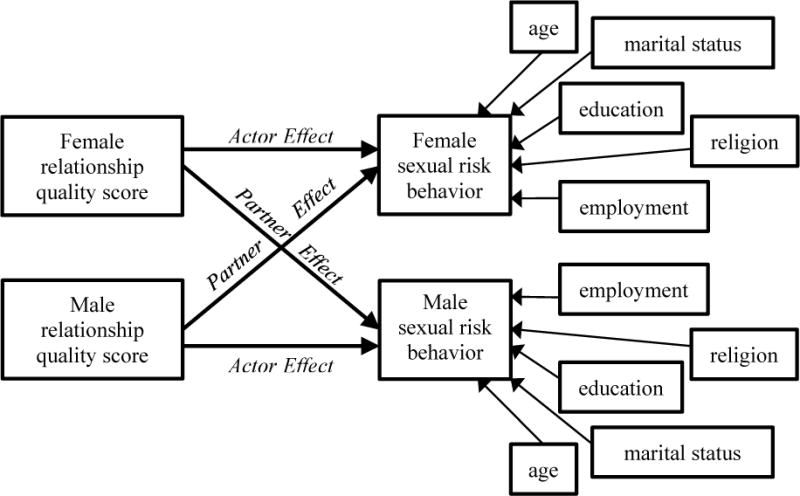
Structural equation model of actor and partner effects of relationship quality on sexual risk behavior
We created a separate model for the effect of each relationship quality domain on each sexual risk behavior, for a total of 20 models (given 5 relationship quality domains and 4 sexual risk behaviors). The first of the 20 models is shown in Figure 2. We included as covariates in the final models age, marital status (cohabiting or married), religion (Muslim, Anglican, Catholic, or other Christian), education (primary or less, some secondary, completed secondary, tertiary), and employment (formal, informal, or none). These covariates were chosen for theoretical reasons, such as previous literature showing their relevance to sexual risk behaviors and relationship quality, as well as through stepwise comparison of nested models using likelihood ratio tests to assess how inclusion of covariates affected model fit. Two variables (length of marriage and having been previously divorced) were not retained in the final models as their inclusion did not improve model fit. All covariates were included in the model as individual-level variables and path coefficients for the effect of these variables on outcomes were set to be equal for women and men.
Figure 2.
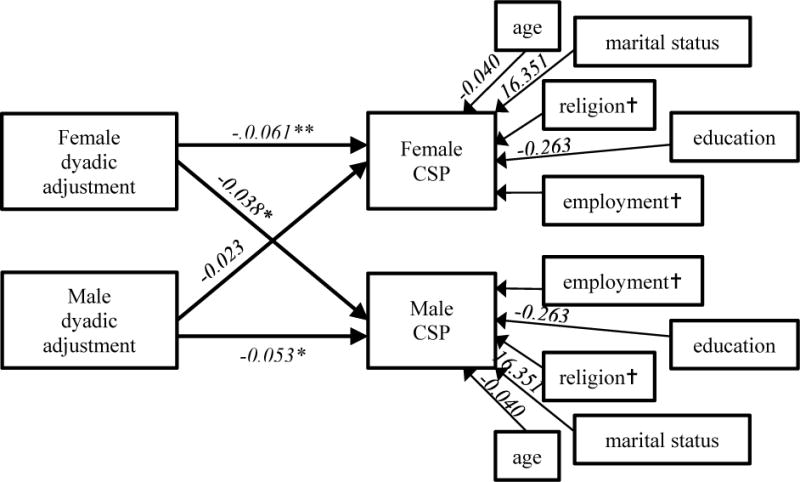
Structural equation model of actor and partner effects of dyadic adjustment on concurrent sexual partnerships (CSP) in past 6 months, with unstandardized path coefficients
* p < .05 ** p < .01
†Path coefficients are not shown for categorical variables as these variables are included in the model as factor variables and thus have a path from each category of the variable to the outcome variable. These paths are not shown for the sake of clarity. In this model, these path coefficients are as follows (note that all covariate path coefficients are set to be equal for women and men):
Religion: Muslim (0.000, reference); Anglican (−0.143); Catholic (−0.340); other Christian (−16.210);
Employment: formal employment (0.000, reference); informal employment (1.258); no employment (−0.079).
No covariate path coefficients are significant at p < .05.
In cases in which both actor effects within a model were statistically significant (at p < .05), we set actor effects to be equal to assess whether actor effects differed by gender. We did the same with partner effects when both partner effects in a model were significant at p < .05. If comparing the constrained and non-constrained models using likelihood ratio tests showed no significant difference (at p < .05) between the models, we concluded that the actor (or partner) effects did not differ significantly by gender.
Ethics
The Mengo Hospital Research Ethics Committee (Protocol 566/6-14) and the Uganda National Council for Science and Technology (Protocol SS3668), both located in Kampala, Uganda, approved the study. The New Paradigm Fund (Washington, DC) provided funding for the study.
Results
Participant characteristics
Table 1 shows characteristics of the 324 participants (162 women and 162 men). Women had a mean age of 28 years, while men had a mean age of 34 years. Approximately a third of women and men had primary school education or no education, while a minority of participants had completed secondary school or progressed to tertiary education. The great majority of participants were informally employed or unemployed, with only 10% of women and 20% of men reporting formal employment. Most participants were from the Baganda sociolinguistic group, and similar proportions belonged to the three major religious groups (Muslim, Anglican, and Catholic). Most participants reported that they were cohabiting but unmarried (90% of women and 86% of men), while 2 women and 5 men reported being in a polygamous relationship. The average relationship duration for both women and men was 7 years, and approximately a quarter of participants had been previously divorced or separated from a partner.
Table 1.
Participant characteristics by gender
| Women (N = 162) |
Men: (N = 162) |
Differences by gender | |||
|---|---|---|---|---|---|
|
| |||||
| % (N) | mean (SD) | % (N) | mean (SD) | p-value | |
|
| |||||
| Age (in years) | 28.4 (6.0) | 33.8 (7.2) | .000*** | ||
| Education | |||||
| Primary or less | 32.3% (52) | 38.8% (62) | .189 | ||
| Some secondary | 49.1% (79) | 31.3% (50) | .001** | ||
| Completed secondary | 8.7% (14) | 13.1% (21) | .265 | ||
| Tertiary | 9.9% (16) | 16.9% (27) | .052 | ||
|
| |||||
| Employment | |||||
| Informal | 54.7% (88) | 77.6% (125) | .000*** | ||
| Formal | 9.9% (16) | 19.9% (32) | .009** | ||
| Unemployed | 35.4% (57) | 2.5% (4) | .000*** | ||
|
| |||||
| Ethnic group | |||||
| Baganda | 64.0% (103) | 71.4% (115) | .152 | ||
| Other | 36.0% (58) | 28.6% (46) | |||
|
| |||||
| Religion | |||||
| Muslim | 28.0% (45) | 31.9% (51) | .208 | ||
| Anglican | 30.4% (49) | 28.8% (46) | .662 | ||
| Catholic | 24.2% (39) | 30.0% (48) | .289 | ||
| Other Christian | 17.4% (28) | 9.4% (15) | .007** | ||
|
| |||||
| Marital status | |||||
| Cohabiting | 90.1% (145) | 86.3% (139) | .058 | ||
| Married, monogamous | 8.7% (14) | 10.6% (17) | .453 | ||
| Married, polygamous | 1.2% (2) | 3.1% (5) | .375 | ||
|
| |||||
| Duration of marriage or partnership to current partner (in years) | 6.6 (5.2) | 6.7 (5.1) | .681 | ||
|
| |||||
| Number of times previously divorced or separated | |||||
| 0 | 76.4% (123) | 65.6% (105) | .014* | ||
| 1 | 22.4% (36) | 28.1% (45) | .199 | ||
| 2+ | 0.6% (1) | 6.3% (10) | .007** | ||
Differences by gender calculated using paired t-tests for linear variables and McNemar’s chi-square test for categorical variables.
SD = standard deviation
p < .05
p < .01
p < .001
The great majority of participants reported being sexually active in the past 6 months, and 10 women (6%) and 19 men (12%) reported having concurrent sexual partners in the past 6 months (Table 2). Notably, all of the women and men reporting concurrent sexual partnerships were cohabiting and not married. A majority of women and men who reported concurrent sexual partners in the past 6 months said that their primary partners did not know about these other partnerships (60% of women and 62% of men), and a majority additionally reported that they believed their secondary partners also had concurrent sexual partners (70% of women and 47% of men). Half of women and men said that they did not know if their primary partner had had other sexual partners in the past 6 months, and 14% of women and 4% of men said that they thought their primary partner had had concurrent sexual partners. Actor-partner analysis showed that for only 15% of individuals who thought their primary partner had or might have a concurrent sexual partner did the partner report a concurrent sexual partner. This proportion did not vary significantly by participants’ level of certainty (i.e. whether they answered “yes” or “don’t know” to the question about the partner having a concurrent sexual partner), or between women and men.
Table 2.
Sexual risk behaviors by gender and marital status
| Cohabiting women (N = 145) |
Married women (N = 16) |
Cohabiting men (N = 139) |
Married men (N = 22) |
Differences by
|
||
|---|---|---|---|---|---|---|
| Gender | Marital status | |||||
|
| ||||||
| % (N) | % (N) | % (N) | % (N) | p-value | p-value | |
| CSP, past 6 monthsa | ||||||
| Yes | 7.1% (10) | 0.0% (0) | 14.0% (19) | 0.0% (0) | .088* | .034* |
| No | 92.9% (131) | 100.0% (16) | 86.0% (117) | 100.0% (22) | ||
|
| ||||||
| Thinks primary partner knows about CSPb | ||||||
| Yes | 40.0% (4) | 27.8% (5) | ||||
| No | 60.0% (6) | 62.2% (13) | ||||
|
| ||||||
| Thinks primary partner has had CSP, past 6 monthsa,c | .020* | |||||
| Yes | 13.4% (19) | 18.8% (3) | 5.2% (7) | 0.0% (0) | .004** | |
| No | 33.8% (48) | 56.3% (9) | 40.7% (55) | 68.2% (15) | .080 | |
| Don’t know | 52.8% (75) | 25.0% (4) | 54.1% (73) | 31.8% (7) | .896 | |
|
| ||||||
| Thinks secondary partner has had CSP, past 6 monthsb | ||||||
| Yes | 70.0% (7) | 47.4% (9) | ||||
| No | 20.0% (2) | 21.1% (4) | ||||
| Don’t know | 10.0% (1) | 31.6% (6) | ||||
|
| ||||||
| Condom use, primary partnera,c | .759 | |||||
| Never | 79.6% (113) | 93.8% (15) | 84.6% (115) | 81.8% (18) | .369 | |
| Sometimes | 16.9% (24) | 0.0% (0) | 12.5% (17) | 18.2% (4) | .513 | |
| Always | 3.5% (5) | 6.3% (1) | 2.9% (4) | 0.0% (0) | .317 | |
|
| ||||||
| Condom use, secondary partnerb,d | ||||||
| Never | 0.0% (0) | 15.8% (3) | ||||
| Sometimes | 0.0% (0) | 10.5% (2) | ||||
| Always | 100.0% (10) | 73.7% (14) | ||||
|
| ||||||
| Alcohol use with sex (either partner drunk at last sex with primary partner)b | ||||||
| Yes | 21.3% (30) | 6.3% (1) | 13.3% (18) | 4.5% (1) | .009** | .138 |
| No | 78.7% (111) | 93.7% (15) | 86.7% (117) | 95.5% (21) | ||
Differences by gender calculated using McNemar’s test. Differences by marital status (cohabiting versus married) calculated using chi-squared statistics and Fisher’s exact test (in the case of one or more empty cells).
CSP = concurrent sexual partner(s), i.e. sexual partner(s) in addition to regular sexual partner or spouse(s) and not including wives of polygamous men
p < .05
p < .01
p < .001
Among those who reported sex in past 6 months.
Among those who reported CSP in past 6 months. No married women or men were asked this question as none reported CSP in past 6 months.
For first wife reported, for polygamous men who reported 2 or more wives. Excludes response of 1 woman who reported a cohabiting, polygamous relationship and that her partner had CSP.
For first CSP reported, for participants who reported 2 or more CSP.
Condom use showed a striking association with type of sexual partnership, with only 3% of participants reporting always using condoms with primary partners and 83% of participants reporting never using condoms with primary partners. In contrast, all women and most men with secondary partners reported always using condoms with those partners. A number of participants (20% of women and 12% of men) reported alcohol use with sex (i.e. that during last sex with primary partner, at least one partner was drunk).
Relationship quality and its correlates
Cohabiting women and men and married women and men generally reported high relationship quality, with median scores consistently above 80 on a scale of 0 to 100 for dyadic adjustment, intimacy, and communication (Table 3). Median scores on the sexual satisfaction and commitment scales were above 90 for all four sub-groups examined. Men reported higher relationship quality than did women, and these differences were statistically significant (at p < .01) for all domains except sexual satisfaction. Pearson’s correlation, a test of non-independence of partners’ scores, scored as significant (at p < .05) for all relationship quality domains with coefficient values of .16 to .39, suggesting a small to moderate positive correlation between couples’ scores on the relationship quality scales (Table 4).
Table 3.
Relationship quality across 5 domains, by gender and marital status
| Cohabiting women (N = 145) |
Married womena (N = 16) |
Cohabiting men (N = 139) |
Married mena (N = 22) |
Total (N = 324) |
Differences by
|
||
|---|---|---|---|---|---|---|---|
| Gender | Marital status | ||||||
| Dyadic adjustment | |||||||
| Cronbach’s alpha | .92 | .90 | .86 | .82 | .88 | ||
| Median (IQR) | 82.3 (70.8 - 89.1) |
82.0 (75.2 - 92.9) |
85.0 (77.6 - 89.1) |
85.0 (77.6 - 89.1) |
84.4 (74.8 - 89.1) |
p = .002** | p = .265 |
|
| |||||||
| Sexual satisfactionc | |||||||
| Cronbach’s alpha | .69 | .57 | .43 | .46 | .59 | ||
| Median (IQR) | 93.8 (84.4 - 100.0) |
93.8 (76.6 - 100.0) |
93.8 (81.3 - 100.0) |
95.3 (84.4 - 100.0) |
93.8 (81.3-100.0) |
p = .355 | p = .997 |
|
| |||||||
| Commitment | |||||||
| Cronbach’s alpha | .93 | .71 | .92 | .76 | .93 | ||
| Median (IQR) | 90.6 (68.8 - 100.0) |
100.0 (96.1 - 100.0) |
95.3 (78.1 - 100.0) |
100.0 (93.8 -100.0) |
95.3 (76.6 - 100.0) |
p = .007** | p = .001** |
|
| |||||||
| Intimacy | |||||||
| Cronbach’s alpha | .89 | .85 | .85 | .87 | .88 | ||
| Median (IQR) | 89.1 (68.8 - 98.4) |
98.4 (89.8 - 100.0) |
92.2 (82.8 - 98.4) |
96.9 (92.2 - 100.0) |
92.2 (76.6 - 100.0) |
p = .001** | p = .009** |
|
| |||||||
| Communication | |||||||
| Cronbach’s alpha | .74 | .46 | .64 | .56 | .69 | ||
| Median (IQR) | 82.1 (69.6 - 92.9) |
86.5 (82.1 - 91.6) |
85.7 (76.8 - 92.9) |
85.7 (78.6 - 92.9) |
85.7 (73.2 - 92.9) |
p = .000*** | p = 0.322 |
Scores on relationship quality scales are standardized to scale of 0 to 100, with higher scores denoting higher relationship satisfaction or quality.
Differences in relationship quality by marital status calculated using t-tests. Differences in relationship quality by gender calculated using paired t-tests.
IQR = interquartile range
p < .05
p < .01
p < .001
Including individuals in polygamous unions
Pearson’s correlation coefficient (r)
Values given are for the shortened 8-item scale. The original 14-item scale had Cronbach’s alpha of .51 (cohabiting women), .50 (married women), .23 (cohabiting men), .32 (married men), and .40 (total).
Table 4.
Pairwise bivariate correlations between relationship quality and sexual risk behaviors for women and men
| Women | Men | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | ||
| Women | |||||||||||||||||||
| 1 | Dyadic adjustment | 1.00 | |||||||||||||||||
| 2 | Sexual satisfaction | 0.62* | 1.00 | ||||||||||||||||
| 3 | Commitment | 0.62* | 0.49* | 1.00 | |||||||||||||||
| 4 | Intimacy | 0.72* | 0.47* | 0.84* | 1.00 | ||||||||||||||
| 5 | Communication | 0.69* | 0.56* | 0.52* | 0.55* | 1.00 | |||||||||||||
| 6 | CSP, past 6 months | −0.33* | −0.32* | −0.41* | −0.39* | −0.26* | 1.00 | ||||||||||||
| 7 | Sex with partner with CSPa | −0.31* | −0.21* | −0.31* | −0.28* | −0.17* | 0.20* | 1.00 | |||||||||||
| 8 | No condom useb | 0.29 | 0.01 | 0.00 | −0.01 | −0.01 | 0.06 | 0.01 | 1.00 | ||||||||||
| 9 | Alcohol use with sexc | −0.18* | −0.21* | −0.30* | −0.17* | −0.36* | 0.20* | 0.31* | −0.00 | 1.00 | |||||||||
|
| |||||||||||||||||||
| Men | |||||||||||||||||||
| 10 | Dyadic adjustment | 0.39* | 0.23* | 0.21* | 0.24* | 0.15 | −0.19* | −0.11 | 0.05 | 0.12 | 1.00 | ||||||||
| 11 | Sexual satisfaction | 0.39* | 0.37* | 0.10 | 0.15 | 0.27* | −0.06 | −0.13 | 0.04 | −0.03 | 0.42* | 1.00 | |||||||
| 12 | Commitment | 0.17* | 0.01 | 0.18* | 0.16* | 0.03 | −0.15 | −0.03 | −0.01 | 0.09 | 0.52* | 0.25* | 1.00 | ||||||
| 13 | Intimacy | 0.16* | 0.00 | 0.17* | 0.17* | 0.02 | −0.12 | −0.11 | −0.02 | −0.01 | 0.59* | 0.29* | 0.75* | 1.00 | |||||
| 14 | Communication | 0.33* | 0.27* | 0.16* | 0.10 | 0.27* | −0.07 | −0.13 | 0.03 | −0.07 | 0.50* | 0.43* | 0.27* | 0.30* | 1.00 | ||||
| 15 | CSP, past 6 months | −0.23* | −0.08 | −0.25* | −0.21* | −0.06 | 0.15 | 0.23* | −0.03 | 0.12 | −0.28* | −0.24* | −0.36* | −0.33* | −0.18* | 1.00 | |||
| 16 | Sex with partner with CSPa | −0.28* | −0.12 | −0.33* | −0.28* | −0.22* | 0.24* | 0.31* | 0.03 | 0.23* | −0.30* | −0.10 | −0.28* | −0.31* | −0.29* | 0.25* | 1.00 | ||
| 17 | No condom useb | −0.09 | −0.09 | −0.14 | −0.10 | −0.07 | 0.03 | −0.11 | 0.46* | −0.05 | −0.02 | 0.07 | −0.01 | −0.03 | 0.05 | −0.05 | 0.01 | 1.00 | |
| 18 | Alcohol use with sexc | −0.15 | −0.17* | −0.16* | −0.06 | −0.19* | 0.07 | 0.07 | 0.07 | 0.42* | 0.12 | −0.14 | 0.06 | 0.02 | −0.19* | 0.04 | 0.18* | −0.16* | 1.00 |
Pearson’s correlation coefficients (r); bold text indicates correlations between partners’ scores on the same variable.
p < .05
CSP = concurrent sexual partner(s), i.e. sexual partner(s) in addition to regular sexual partner or spouse(s) and not including polygamous men’s multiple wives
believes or suspects primary partner had CSP, past 6 months
with primary partner
either partner drunk at last sex with primary partner
Married women and men scored significantly higher (at p < .01) on the commitment scale than did cohabitors, with median scores of 100 on a 0 to 100 scale versus median scores of 91 and 95, respectively, for cohabiting women and men. Married individuals also scored significantly higher (at p < .01) on the intimacy scale than did cohabiting women (median scores of 98 versus 89 for women and 97 versus 92 for men). Although married individuals generally scored higher on the relationship quality scales, statistical comparison was hindered by the small number of married individuals, and no other differences by marital status were statistically significant at p < .05.
Actor and partner effects of relationship quality on sexual risk behaviors
In actor effects, individuals who reported higher relationship quality were significantly less likely to report having concurrent sexual partners, suspecting their partners of having concurrent sexual partners, or alcohol use with sex (Table 5). For women, higher relationship quality in every domain was significantly and negatively associated with reporting concurrent sexual partners in the past 6 months (p < .01 for all associations), with sexual satisfaction showing the largest effect size. Similarly, women’s higher dyadic adjustment, commitment, and intimacy were significantly and negatively associated with women thinking their primary sexual partners had or might have concurrent sexual partners (p < .01 for all associations). No domains of women’s relationship quality were significantly associated (at p < .05) with women’s condom use. Finally, women who reported higher dyadic adjustment, sexual satisfaction, commitment, and more constructive communication were significantly less likely to report alcohol use with sex, with the effect size being the largest for communication (p < .01 for all associations).
Table 5.
Unstandardized estimates for actor and partner effects of five relationship quality constructs on four sexual risk behaviors
| CSP, past 6 months | Sex with partner with CSPa | No condom use with primary partner | Alcohol use with sexb | |
|---|---|---|---|---|
|
| ||||
| Estimate (SE) | Estimate (SE) | Estimate (SE) | Estimate (SE) | |
| Dyadic adjustment | ||||
| Actor effect: female RQ → female sexual risk behavior | −0.061 (0.022)** | −0.061 (0.019)*** | 0.003 (0.016) | −0.045 (0.016)**† |
| Partner effect: female RQ → male sexual risk behavior | −0.038 (0.018)* | −0.033 (0.015)* | 0.020 (0.015) | −0.041 (0.017)*‡ |
| Actor effect: male RQ → male sexual risk behavior | −0.053 (0.024)* | −0.056 (0.022)* | −0.000 (0.024) | 0.078 (0.040)* |
| Partner effect: male RQ → female sexual risk behavior | −0.023 (0.030) | 0.011 (0.019) | 0.013 (0.021) | 0.078 (0.029)** |
|
| ||||
| Sexual satisfaction | ||||
| Actor effect: female RQ → female sexual risk behavior | −0.066 (0.020)*** | −0.029 (0.017) | −0.001 (0.015) | −0.037 (0.014)** |
| Partner effect: female RQ → male sexual risk behavior | −0.010 (0.019) | −0.026 (0.016) | 0.031 (0.016)* | −0.023 (0.016) |
| Actor effect: male RQ → male sexual risk behavior | −0.075 (0.026)** | −0.014 (0.020) | −0.030 (0.025) | −0.020 (0.025) |
| Partner effect: male RQ → female sexual risk behavior | 0.015 (0.036) | 0.015 (0.020) | 0.021 (0.022) | 0.026 (0.023) |
|
| ||||
| Commitment | ||||
| Actor effect: female RQ → female sexual risk behavior | −0.046 (0.014)*** | −0.041 (0.013)*** | 0.001 (0.009) | −0.029 (0.009)** |
| Partner effect: female RQ → male sexual risk behavior | −0.017 (0.011) | −0.031 (0.010)** | 0.018 (0.009)* | −0.019 (0.010) |
| Actor effect: male RQ → male sexual risk behavior | −0.048 (0.015)*** | −0.031 (0.013)* | −0.003 (0.012) | 0.015 (0.017) |
| Partner effect: male RQ → female sexual risk behavior | −0.019 (0.016) | 0.009 (0.011) | −0.003 (0.012) | 0.033 (0.016)* |
|
| ||||
| Intimacy | ||||
| Actor effect: female RQ → female sexual risk behavior | −0.053 (0.016)*** | −0.037 (0.013)** | 0.000 (0.011) | −0.017 (0.010) |
| Partner effect: female RQ → male sexual risk behavior | −0.017 (0.012) | −0.031 (0.011)** | 0.015 (0.010) | −0.005 (0.012) |
| Actor effect: male RQ → male sexual risk behavior | −0.057 (0.019)** | −0.055 (0.017)** | 0.001 (0.017) | 0.009 (0.022) |
| Partner effect: male RQ → female sexual risk behavior | −0.021 (0.024) | −0.002 (0.015) | −0.008 (0.017) | 0.011 (0.017) |
|
| ||||
| Constructive communication | ||||
| Actor effect: female RQ → female sexual risk behavior | −0.061 (0.020)** | −0.022 (0.012) | −0.002 (0.013) | −0.058 (0.014)*** |
| Partner effect: female RQ → male sexual risk behavior | −0.002 (0.016) | −0.018 (0.012) | 0.014 (0.012) | −0.029 (0.014)* |
| Actor effect: male RQ → male sexual risk behavior | −0.040 (0.023) | −0.066 (0.021)** | −0.020 (0.022) | −0.037 (0.023) |
| Partner effect: male RQ → female sexual risk behavior | 0.002 (0.028) | −0.013 (0.018) | 0.010 (0.019) | 0.023 (0.020) |
Models include covariates of age, marital status, religion, education, and employment.
p < .05
p < .01
p < .001
CSP = concurrent sexual partner(s), i.e. sexual partner(s) in addition to regular sexual partner or spouse(s) and not including polygamous men’s multiple wives
SE = standard error
believes or suspects primary partner had CSP, past 6 months
either partner drunk at last sex with primary partner
= actor effects differ by gender (p = .001)
partner effects differ by gender (p < .001)
Men showed fewer significant associations between relationship quality and sexual risk behaviors than did women. Men’s higher relationship quality was significantly (at p < .05) and negatively associated with reporting concurrent sexual partners in the past 6 months for all relationship quality domains except for communication, with sexual satisfaction showing the largest effect size (as for women). Suspecting one’s primary sexual partner of having concurrent sexual partners was significantly associated for men (at p < .05) with all domains of relationship quality except sexual satisfaction. Also consistent with women’s actor effects, men showed no significant associations (at p < .05) between relationship quality and condom use. Men showed an unexpected actor effect between relationship quality and alcohol use with sex, with men with higher dyadic adjustment being more likely to report alcohol use with sex (significant at p < .05).
Fewer significant partner effects were observed, compared to actor effects. Women’s relationship quality was associated with men’s sexual risk behaviors for 7 of 20 pathways. Female partners of men who reported having concurrent sexual partners in the past 6 months reported lower dyadic adjustment (significant at p < .05). Women whose partners suspected them of having concurrent sexual partners reported lower dyadic adjustment (significant at p < .05), commitment (significant at p < .10), and intimacy (significant at p < .10). In the only two significant associations seen between condom use and relationship quality, women whose partners reported never using condoms in the partnership reported higher sexual satisfaction and commitment (both associations significant at p < .05). Consistent with the finding that women who reported alcohol use with sex also reported worse communication (actor effect), women whose male partners reported alcohol use with sex similarly reported worse communication (partner effect, significant at p < .05), suggesting consistency between women’s and men’s reports of alcohol use with sex. Women whose male partners reported alcohol use with sex also reported lower dyadic adjustment (significant at p < .05).
Only 2 of 20 pathways between men’s relationship quality and women’s sexual risk behavior were significant at p < .05. Both showed an unexpected positive association between men’s higher relationship quality and their female partners reporting alcohol use with sex. This association held true for men’s dyadic adjustment (significant at p < .01) and commitment (significant at p < .05). This finding concurs with the actor effect that men who reported alcohol use with sex also reported higher dyadic adjustment (significant at p < .05). In contrast, women reported lower relationship quality (in all domains except intimacy) when they reported alcohol use with sex (actor effects), and in couples in which the man reported alcohol use with sex women also reported lower dyadic adjustment and worse communication (partner effects). In other words, in couples who reported alcohol use with sex, there seemed to be a consistently negative effect on women’s relationship quality but a somewhat positive effect on men’s relationship quality. In addition, the only actor effects that differed significantly (at p < .05) by gender were the actor effects of dyadic adjustment on alcohol use at sex, and similarly the only partner effects that differed significantly (at p < .05) by gender were the partner effects of dyadic adjustment on alcohol use at sex (Table 5).
Discussion
The use of psychometric scales to measure couple relationship quality in African populations remains relatively rare, and to our knowledge the measures used in this research have never before been used in Uganda. The finding that relationship quality is consistently correlated with an individual’s sexual risk behaviors, particularly engaging in concurrent sexual partnerships, is novel. The observed correlations indicate predictive validity of these scales for this population and that relationship quality is linked to HIV risk through the mechanism of concurrent sexual partnerships.
We cannot determine based on these findings whether poor relationship quality causes or is caused by lack of sexual exclusivity in a relationship. Women and men who experience their relationships as deficient in areas such as sexual satisfaction, commitment, intimacy, and communication may be more likely to seek concurrent sexual partners or believe that their partners do so. Conversely, when one or both partners engages in concurrent sexual partnerships the relationship may be negatively impacted. More plausibly, causation may flow in both directions for different couples at different times. Women were more likely to suspect that their spouse or primary partner had a concurrent sexual partner, and this may provide a partial explanation for their lower relationship quality scores in all domains except sexual satisfaction. These findings suggest the presence of gender differences and that women may have less power in their relationships and less ability to leave unsatisfactory relationships. Recent research in Uganda has similarly identified women’s lack of relationship power as being a risk factor for HIV infection, specifically through the association of low relationship power with higher odds of forced and transactional sex (29).
Comparison of actor and partner effects shows that in this population, actor effects were primary. In other words, women’s and men’s relationship quality was much more strongly and consistently associated with their own sexual risk behaviors than with their partner’s sexual risk behaviors. In fact, men’s relationship quality was never associated with women’s sexual risk behavior, except for being positively associated with women’s report of alcohol use with sex. As we did not ask participants to identify which partner(s) were intoxicated, women’s reports of this risk behavior may in fact be reflecting their male partners’ alcohol use and not their own. Thus, men’s perception of higher relationship quality may be linked to their own alcohol consumption, and not to their partner’s behavior. The implication is that there may in fact be no evidence that men’s relationship quality influences women’s sexual risk behaviors, or that women’s sexual risk behaviors influence men’s relationship quality.
In contrast, several significant associations were seen between women’s relationship quality and men’s sexual risk behavior. This suggests that women’s perception of the quality of the relationship is more influenced by men’s behaviors than men’s perception of the relationship is influenced by women’s behaviors, or that women’s level of satisfaction in the relationship may have a causal effect on men engaging in risk behaviors. These differences by gender may be explained by the fact that men are more likely to engage in risk behaviors, and thus a stronger effect is seen on women’s relationship quality.
This study confirms that concurrent sexual partnerships are a major risk factor for HIV transmission in this community. A minority of participants (6% of women and 12% of men) reported concurrent sexual partners (other than multiple wives, for polygamous men) in the past 6 months. These data are similar to statistics reported in the HIV and AIDS Uganda Country Progress Report 2014 that among Ugandan adults aged 15–49, 8% of women and 22% of men reported multiple sexual partners in the past 12 months (30). In the current study, most women and nearly half of men reporting concurrent sexual partnerships said that they believed their secondary partner also had other sexual partners, suggesting the presence of dense sexual networks. Furthermore, more than half of women and men expressed doubts that their spouses or cohabiting partners were sexually faithful. For women, this suspicion of infidelity was as consistently correlated with poorer relationship quality as was reporting that a partner was known to be sexually unfaithful.
Alcohol use with sex was also correlated with women’s poorer relationship quality, adding to previous findings about alcohol use and negative relationship outcomes. Alcohol usage in Uganda is high, with 27% of Ugandan adults reporting that they currently consume alcohol and 10% of Ugandan adults being classified as having an alcohol use disorder (31). Previous research in Uganda has found that women who reported that either they or their partner consumed alcohol before sex were more likely to be HIV-infected and have a history of physical violence and sexual coercion (32). Additional studies have linked regular alcohol consumption to increased risk of HIV infection in fishing communities in Uganda (33) and hazardous drinking to higher risk of forced and transactional sex among women living with HIV (21).
Reported condom use with spouses or cohabiting partners was quite low, which accords with previous findings from Uganda that most adults in stable relationships engage in unprotected sex even when one or both partners is HIV-infected (34). We found no significant associations between condom use and relationship quality, with the exception that men who reported no condom use in their primary partnerships had female partners who reported higher sexual satisfaction and commitment. Participants were significantly more likely to report condom use with secondary partners. While some researchers view lack of condom use in long-term, committed partnerships as a risky decision which prioritizes relational or economic needs over physical health (4,35), this behavior may also reflect that women and men are accurately judging their risk of HIV acquisition to be lower in long-term and stable relationships, particularly marriage. We note that in this study, married individuals appeared to be in particularly stable, low-risk relationships. No married individuals reported concurrent sexual partnerships, and they reported significantly higher commitment than cohabiting individuals, as well as higher relationship quality generally.
Although risk of HIV transmission within HIV-discordant partnerships in Uganda is quite high (36), only 5% of all Ugandan couples are sero-discordant (29). According to data from the Rakai population cohort collected in the mid-2000s, only 14% of incident HIV infections were among identifiable sero-discordant couples whereas 43% were among individuals not in a stable consensual relationship and 26% were among individuals in concordant HIV-negative couples, suggesting infection through a concurrent sexual partnership (37). Similarly, the Masaka population cohort found that HIV incidence among unmarried individuals (separated, widowed, and never married) was 2.7 times the HIV incidence of married individuals (38). These data confirm that Ugandans in marriages and other stable relationships are on the whole at reduced risk of HIV, even if few use condoms in these relationships.
Some participants in this study, particularly women, were likely at risk of HIV infection within their primary partnerships. A number of participants believed their primary partners had concurrent sexual partners, and half of participants said they did not know whether their partners had concurrent partners. Our results suggest that condom promotion efforts should take into account the fact that not all adults are equally at risk of HIV acquisition and that many women and men may be accurately judging their risk, and thus focus on individuals who know themselves to be at higher risk through their own or partners’ concurrent sexual partnerships.
This study faced a number of limitations, including that all data were self-reported. Participants may have shaped their responses in socially desirable ways, such as by presenting their relationships in overly positive terms or under-reporting stigmatized behaviors such as concurrent sexual partnerships. A further limitation relates to the relationship quality measures used and the fact that they have not been widely used or validated in populations similar to the study population. The low Cronbach’s alpha of the sexual satisfaction scale was of particular concern, and suggests that this scale may not have been a valid measure of sexual satisfaction in this population, although it had predictive validity for sexual risk behavior. We note the need for further work to validate psychometric measures of relationship quality in African populations, as well as the need for caution in generalizing the findings from this study population to other Ugandan or African populations. A number of additional limitations have already been discussed, including our inability to establish the direction of causality for associations between relationship quality and sexual risk behaviors.
Conclusion
We echo previous calls for a greater investment in research into couple relationships as well as couple-based approaches to HIV prevention in African populations. Most relationship quality scales used in this study showed high reliability and associations with multiple sexual risk behaviors, despite not having been used previously in Uganda. This indicates that such scales have validity across sociocultural contexts and that they can identify individuals and couples whose relationships and health are at risk. More work is needed to develop and validate measures of relationship quality for use in Uganda and other African populations. Our finding that poor relationship quality is consistently linked to sexual risk behaviors points to the need to develop and test interventions to strengthen couple relationships, which may reduce HIV risk through multiple pathways. We believe that developing and implementing evidence-based behavioral HIV prevention for couples has the potential not only to reduce transmission of HIV but also to strengthen couple relationships in ways that will benefit couples, families, and communities.
Acknowledgments
This research was supported by a grant from The New Paradigm Fund. Dr. Ruark was supported by a post-doctoral fellowship through the National Institute on Drug Abuse (Grant Number T32DA13911). We thank the Ugandan facilitators and research assistants who participated in the intervention and research: Jamillah Naamala, Dativa Ssozi, Francis Ssozi, Marvin Katerega, Catherine Kiyenje, Josephine Nabukera, Ritah Nassaka, and Claire Seremba. Our sincere thanks to the participants and community leaders in Tebuyoleka Zone who made the research possible.
A. Ruark serves on the Advisory Board of the New Paradigm Fund (NPF) and received funding from NPF and from the National Institute on Drug Abuse (Grant Number T32DA13911). P. Kajubi and S. Ruteikara received funding from NPF. E. C. Green is President and Director of NPF. N. Hearst serves on the Board of Directors of NPF.
Footnotes
Compliance with Ethical Standards
Ethical Approval, Research Involving Human Participants All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1.Jiwatram-Negrón T, El-Bassel N. Systematic review of couple-based HIV intervention and prevention studies: advantages, gaps, and future directions. AIDS Behav. 2014;18(10):1864–87. doi: 10.1007/s10461-014-0827-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwena Z, Mwanzo I, Shisanya C, Camlin C, Turan J, Achiro L, et al. Predictors of extra-marital partnerships among women married to fishermen along Lake Victoria in Kisumu County, Kenya. PLOS ONE. 2014;9(4):e95298. doi: 10.1371/journal.pone.0095298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leddy A, Chakravarty D, Dladla S, de Bruyn G, Darbes L. Sexual communication self-efficacy, hegemonic masculine norms and condom use among heterosexual couples in South Africa. AIDS Care. 2016;28(2):228–33. doi: 10.1080/09540121.2015.1080792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vamos S, Cook R, Chitalu N, Mumbi M, Weiss SM, Jones D. Quality of relationship and sexual risk behaviors among HIV couples in Lusaka, Zambia. AIDS Care. 2013;25(9):1102–8. doi: 10.1080/09540121.2012.749339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Conroy AA, McGrath N, van Rooyen H, Hosegood V, Johnson MO, Fritz K, et al. Power and the association with relationship quality in South African couples: implications for HIV/AIDS interventions. Soc Sci Med. 2016;153:1–11. doi: 10.1016/j.socscimed.2016.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wabwire-Mangen F, Odiit M, Kirungi W, Kisitu DK, Wanyama JO. Uganda HIV prevention response and modes of transmission analysis. Kampala, Uganda: Uganda AIDS Commission; 2009. [Google Scholar]
- 7.Ministry of Health Uganda AIDS Indicator Survey. Kampala, Uganda: MInistry of Health and ICF International; 2011. 2012. [Google Scholar]
- 8.Green EC, Halperin DT, Nantulya V, Nantulya V, Hogle JA. Uganda’s HIV prevention success: the role of sexual behavior change and the national response. AIDS Behav. 2006;10(4):335–46. doi: 10.1007/s10461-006-9073-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Low-Beer D, Stoneburner R. Uganda and the challenge of HIV/AIDS. In: Poku NK, Whiteside A, editors. The political economy of AIDS in Africa Farnham. United Kingdom: Ashgate; 2010. pp. 165–90. [Google Scholar]
- 10.Green EC. Rethinking AIDS prevention: learning from successes in developing countries. Westport, CT: Praeger; 2003. [Google Scholar]
- 11.Slutkin G, Okware S, Naamara W, Sutherland D, Flanagan D, Caraël M, et al. How Uganda reversed its HIV epidemic. AIDS Behav. 2006;10(4):351–60. doi: 10.1007/s10461-006-9118-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stoneburner RL, Low-Beer D. Population-level HIV declines and behavioral risk avoidance in Uganda. Science. 2004;304(5671):714–8. doi: 10.1126/science.1093166. [DOI] [PubMed] [Google Scholar]
- 13.Kirby D. Changes in sexual behaviour leading to the decline in the prevalence of HIV in Uganda: confirmation from multiple sources of evidence. Sex Transm Infect. 2008;84(Suppl 2):ii35–ii41. doi: 10.1136/sti.2008.029892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Opio A, Mishra V, Hong R, Musinguzi J, Kirungi W, Cross A, et al. Trends in HIV-related behaviors and knowledge in Uganda, 1989–2005: evidence of a shift toward more risk-taking behaviors. JAIDS. 2008;49(3):320–6. doi: 10.1097/QAI.0b013e3181893eb0. [DOI] [PubMed] [Google Scholar]
- 15.Kajubi P, Green EC, Hudes ES, Kamya MR, Ruark A, Hearst N. Multiple sexual partnerships among poor urban dwellers in Kampala, Uganda. JAIDS. 2011;57(2):153–6. doi: 10.1097/QAI.0b013e318211b466. [DOI] [PubMed] [Google Scholar]
- 16.Hearst N, Kajubi P, Hudes ES, Maganda AK, Green EC. Prevention messages and AIDS risk behavior in Kampala, Uganda. AIDS Care. 2012;24(1):87–90. doi: 10.1080/09540121.2011.582478. [DOI] [PubMed] [Google Scholar]
- 17.Green EC, Kajubi P, Ruark A, Kamya S, D’Errico N, Hearst N. The need to reemphasize behavior change for HIV prevention in Uganda: a qualitative study. Stud Fam Plan. 2013;44(1):25–43. doi: 10.1111/j.1728-4465.2013.00342.x. [DOI] [PubMed] [Google Scholar]
- 18.Higgins JA, Mathur S, Eckel E, Kelly L, Nakyanjo N, Sekamwa R, et al. Importance of relationship context in HIV transmission: results from a qualitative case-control study in Rakai, Uganda. Am J Public Health. 2014;104(4):612–20. doi: 10.2105/AJPH.2013.301670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Larsson EC, Thorson A, Nsabagasani X, Namusoko S, Popenoe R, Ekström AM. Mistrust in marriage- reasons why men do not accept couple HIV testing during antenatal care- a qualitative study in eastern Uganda. BMC Public Health. 2010;10:769. doi: 10.1186/1471-2458-10-769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agol D, Bukenya D, Seeley J, Kabunga E, Katahoire A. Marriage, intimacy and risk of HIV infection in South West Uganda: original research article. African Journal of Reproductive Health. 2014;18(4):86. [PubMed] [Google Scholar]
- 21.Conroy AA, Tsai AC, Clark GM, Boum Y, Hatcher AM, Kawuma A, et al. Relationship power and sexual violence among HIV-positive women in rural Uganda. AIDS Behav. 2016 Apr 6;20(9):2045–53. doi: 10.1007/s10461-016-1385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mah TL, Shelton JD. Concurrency revisited: Increasing and compelling epidemiological evidence. J Int AIDS Soc. 2011;14:33. doi: 10.1186/1758-2652-14-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kajubi P, Kamya MR, Kamya S, Chen S, McFarland W, Hearst N. Increasing condom use without reducing HIV risk: results of a controlled community trial in Uganda. JAIDS. 2005;40(1):77–82. doi: 10.1097/01.qai.0000157391.63127.b2. [DOI] [PubMed] [Google Scholar]
- 24.Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38(1):15–28. [Google Scholar]
- 25.Hudson WW, Harrison DF, Crosscup PC. A short-form scale to measure sexual discord in dyadic relationships. The Journal of Sex Research. 1981;17(2):157–74. [Google Scholar]
- 26.Sternberg RJ. Construct validation of a triangular love scale. Eur J Soc Psychol. 1997;27(3):313–35. [Google Scholar]
- 27.Heavey CL, Larson BM, Zumtobel DC, Christensen A. The Communication Patterns Questionnaire: The reliability and validity of a constructive communication subscale. J Marriage Fam. 1996;58(3):796–800. [Google Scholar]
- 28.Kenny DA, Kashy DA, Cook WL. Dyadic Data Analysis. New York: Guilford Press; 2006. [Google Scholar]
- 29.Uganda AIDS Commission. HIV and AIDS Uganda country progress report 2014. Kampala, Uganda: Uganda AIDS Commission; 2015. [Google Scholar]
- 30.Kabwama SN, Ndyanabangi S, Mutungi G, Wesonga R, Bahendeka SK, Guwatudde D. Alcohol use among adults in Uganda: findings from the countrywide non-communicable diseases risk factor cross-sectional survey. Global Health Action. 2016;9(0):1945. doi: 10.3402/gha.v9.31302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zablotska IB, Gray RH, Koenig MA, Serwadda D, Nalugoda F, Kigozi G, et al. Alcohol Use, Intimate Partner Violence, Sexual Coercion and HIV among Women Aged 15–24 in Rakai, Uganda. AIDS Behav. 2009;13(2):225–33. doi: 10.1007/s10461-007-9333-5. [DOI] [PubMed] [Google Scholar]
- 32.Seeley J, Nakiyingi-Miiro J, Kamali A, Mpendo J, Asiki G, Abaasa A, et al. High HIV incidence and socio-behavioral risk patterns in fishing communities on the shores of Lake Victoria, Uganda. Sex Transm Dis. 2012;39(6):433–9. doi: 10.1097/OLQ.0b013e318251555d. [DOI] [PubMed] [Google Scholar]
- 33.Parikh SA. The political economy of marriage and HIV: the ABC approach, “safe” infidelity, and managing moral risk in Uganda. Am J Public Health. 2007;97(7):1198–208. doi: 10.2105/AJPH.2006.088682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Biraro S, Ruzagira E, Kamali A, Whitworth J, Grosskurth H, Weiss HA. HIV-1 transmission within marriage in rural Uganda: a longitudinal study. PLOS ONE. 2013;8(2):e55060–9. doi: 10.1371/journal.pone.0055060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kenyon CR, Kirungi W, Kaharuza F, Buyze J, Bunnell R. Who knows their partner’s HIV status? results from a nationally representative survey in Uganda. JAIDS. 2015;69:92–7. doi: 10.1097/QAI.0000000000000546. [DOI] [PubMed] [Google Scholar]
- 36.Gray R, Ssempiija V, Shelton J, Serwadda D, Nalugoda F, Kagaayi J, et al. The contribution of HIV-discordant relationships to new HIV infections in Rakai, Uganda. AIDS. 2011;25(6):863–5. doi: 10.1097/QAD.0b013e3283448790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ruzagira E, Wandiembe S, Abaasa A, Levin J, Bwanika A, Bahemuka U, et al. Prevalence and incidence of HIV in a rural community-based HIV vaccine preparedness cohort in Masaka, Uganda. PLOS ONE. 2011;6(6):e20684. doi: 10.1371/journal.pone.0020684. [DOI] [PMC free article] [PubMed] [Google Scholar]


