Abstract
Social biases among healthcare providers could limit PrEP access. In this survey study of 115 US medical students, we examined associations between biases (racism and heterosexism) and PrEP clinical decision-making and explored prior PrEP education as a potential buffer. After viewing a vignette about a PrEP-seeking MSM patient, participants reported anticipated patient behavior (condomless sex, extra-relational sex, and adherence), intention to prescribe PrEP to the patient, biases, and background characteristics. Minimal evidence for racism affecting clinical decision-making emerged. In unadjusted analyses, heterosexism indirectly affected prescribing intention via all anticipated behaviors, tested as parallel mediators. Participants expressing greater heterosexism more strongly anticipated increased risk behavior and adherence problems, which were associated with lower prescribing intention. The indirect effect via condomless sex remained significant adjusting for background characteristics. Prior PrEP education did not buffer any indirect effects. Heterosexism may compromise PrEP provision to MSM and should be addressed in PrEP-related medical education.
Keywords: HIV, pre-exposure prophylaxis, African Americans, sexual minorities, prejudice, clinical decision-making
INTRODUCTION
Nationwide, men who have sex with men (MSM) account for approximately 70% of new HIV infections in the US [1] despite representing less than 3% of the adult population [2]. Whereas less than 1% of heterosexuals will acquire HIV in their lifetime, 9% of White MSM and 41% of Black MSM are projected to become HIV-positive [3]. This disproportionate HIV burden underscores the need to prioritize prevention efforts for MSM and Black MSM in particular. HIV pre-exposure prophylaxis (PrEP) can reduce the risk of HIV acquisition among HIV-negative MSM by over 90% when taken as prescribed [4,5]. Despite the promise of PrEP for limiting the spread of HIV among MSM and others, uptake has lagged [6], in part because some providers are reluctant to prescribe it [7]. In the present work, we used a vignette-based online survey of medical students to investigate how social biases may contribute to provider reluctance to prescribe PrEP to MSM. We extend past work related to race-related bias and focus in addition on heterosexism, which is “a set of attitudes, beliefs, behaviors, and social structures that favor heterosexual people over non-heterosexual people or otherwise mark non-heterosexual people as socially deviant” [8].
Background
Over the past two decades, attention to disparities in the quality of healthcare provided to socially advantaged versus disadvantaged groups has mounted, with substantial attention devoted to racial disparities in particular [9–11]. In light of this focus and because professional norms and standards encourage medical providers to provide comparable care to patients of differing social backgrounds, many providers consciously try to limit the extent to which their social biases affect their clinical recommendations [12]. However, social biases can operate in subtle and indirect ways, unconsciously affecting perceptions of patients who are members of socially disadvantaged groups in ways that lead to less favorable treatment, especially in circumstances where treatment course is highly discretionary [13, 14].
PrEP provision is one such circumstance that may be particularly vulnerable to social biases given the high level of discretion involved. Adoption of PrEP into clinical practice is currently optional and prescription may entail subjective judgments regarding patient eligibility. A primary mechanism through which bias is likely to influence prescribing intentions is by shaping expectations surrounding patient behavior. Survey, focus group, and interview research with providers has revealed that concerns about patient behavior function as prominent barriers to PrEP prescription [15–20]. These behavioral concerns include anticipated sexual risk compensation, or concern that patients will increase their sexual risk-taking in response to a perceived decrease in HIV susceptibility when taking PrEP. Such risk-taking could take several forms, such as lower condom use or a higher number of sexual partners. An additional behavioral concern involves patient adherence to the daily medication regimen, with anticipated adherence problems linked to a lower likelihood of prescribing PrEP [20]. Evidence suggests that the extent to which these patient behaviors actually occur or offset the benefit of PrEP is likely overestimated [21, 22]. Nonetheless, expectations surrounding a patient’s behavior may operate as potent deterrents to PrEP prescription among providers and are subject to bias based on social group stereotypes.
The impact of social bias on expectations about patient behavior and subsequent prescribing intention has previously been demonstrated with respect to race within a sample of US medical students [23]: After reading a clinical vignette about a hypothetical HIV-negative male patient who had an HIV-positive male partner and was seeking a prescription for PrEP, medical students judged the patient as more likely to engage in increased condomless sex while taking PrEP if the patient was described in the vignette as being Black rather than White. Beliefs about the patient’s likelihood of increased condomless sex, in turn, predicted lower intention to prescribe PrEP to the hypothetical patient. Thus, the race of the hypothetical patient indirectly affected PrEP clinical decision-making in a way that limited PrEP access for the Black patient [23].
Whereas this earlier research focused only on racial bias in the context of PrEP clinical decision-making, the present research investigated how bias related to sexual orientation can also independently or concomitantly affect expectations about patient behavior and influence clinical decisions about whether or not to prescribe PrEP to a patient. With MSM representing 40% of the 1.2 million US adults considered to be at high risk for HIV and likely to benefit from PrEP [24], manifestation of sexual orientation-based bias in clinical practice could be detrimental to PrEP access for many candidates. Heterosexist attitudes toward sexual minorities, including stereotypes, may heighten providers’ concerns about patient behavior when caring for MSM patients, ultimately compromising their willingness to prescribe PrEP to this priority group. Survey research suggests that promiscuity and irresponsibility are salient sexual stereotypes ascribed to gay men [25]. In qualitative studies, some health service providers have blatantly expressed such stereotypes of gay men when discussing them as PrEP candidates [17] or more subtly expressed heterosexism by indicating a greater willingness to prescribe PrEP in the context of conception versus non-reproductive sexual behavior [17, 26]. Providers with experience prescribing PrEP have also perceived a heterosexist bias in other providers’ judgment of patients, suggesting PrEP-related risk compensation is judged more harshly for gay men than for heterosexuals [27]. Providers with heterosexist beliefs may be more prone to biases in clinical judgment consistent with MSM stereotypes of sexual excess and irresponsibility, and these judgments could deter PrEP provision. Among providers espousing both heterosexist and racist beliefs, the influence of MSM stereotypes on judgment of Black MSM patients may be compounded by longstanding sexual stereotypes of Black men as hypersexual and promiscuous [28] and contemporary associations of Black MSM with disease [25, 29].
Study Objectives and Hypotheses
The primary purpose of the present study was to examine the relationship between social biases (racism and heterosexism) and PrEP clinical decision-making among medical students using a vignette-based survey design. Specifically, we investigated how racism and heterosexism indirectly impacted intention to prescribe PrEP to a hypothetical MSM patient through their effect on judgments about the patient’s behavior. We tested the hypothesized indirect effects using a multiple-mediator model in which anticipated increase in condomless sex, anticipated extra-relational sex (sexual partners outside of the primary partnership), and anticipated adherence operated as parallel pathways via which social biases were associated with intention to prescribe. We pursued two specific objectives and tested corresponding hypotheses:
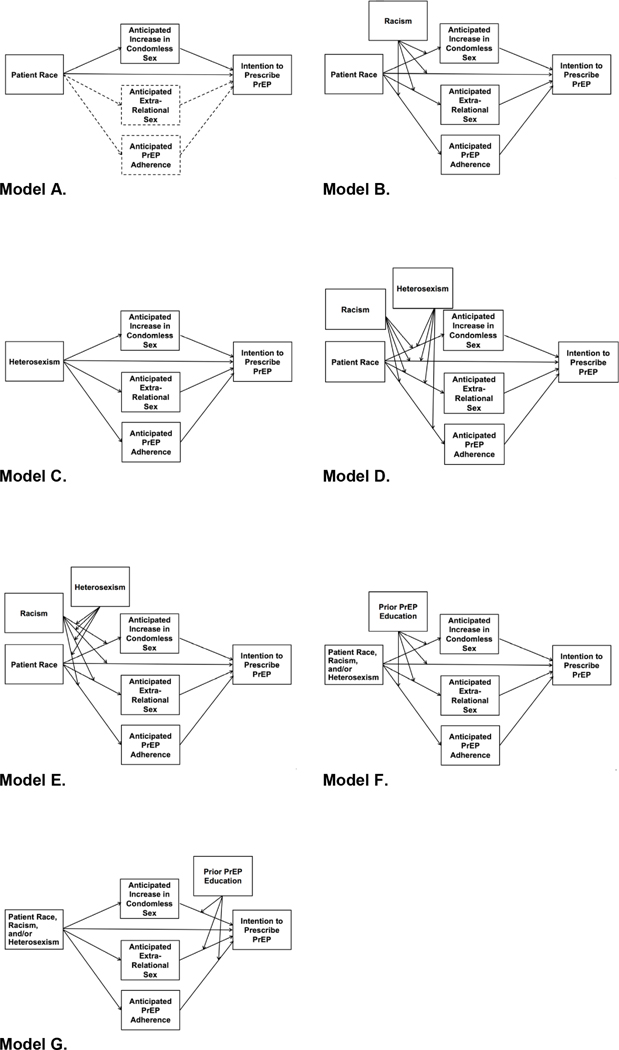
Racism objective and hypotheses: To build on previous research on the role of patient race in PrEP clinical decision-making among medical students [23], in the current study we investigated not only the role of patient race but also the role of participant racism, including explicit racism (self-reported attitudes toward Black Americans) and implicit racism (implicit racial prejudice and implicit risk-related racial stereotypes, both measured using implicit association tests [IATs]). Conceptual models are presented in Figure 1(Models A–B). We expected to replicate the previous finding that when the race of an MSM patient seeking PrEP was specified as being Black rather than White, medical students judged him to be more likely to engage in increased condomless sex while taking PrEP, which, in turn, was associated with lower intention to prescribe PrEP to him. In the present study, we examined two additional indirect pathways through which patient race could affect prescribing intention: anticipated extra-relational sex and anticipated adherence. We hypothesized that, as compared to the White MSM patient, the Black MSM patient would be judged as more likely to engage in extra-relational sex and less likely to adhere to his PrEP regimen, both of which would be associated with lower prescribing intention. We additionally hypothesized that the three indirect effects through anticipated condomless sex, extra-relational sex, and adherence would be moderated by explicit and/or implicit racism such that the differential judgment of Black and White patients would hold only for those expressing higher levels of racism. Likewise, we expected that when patient race was specified as being Black (but not when specified as White), racism would be indirectly associated with lower intention to prescribe.
Heterosexism objective and hypothesis: Expanding consideration of social bias in PrEP clinical decision-making beyond racism, we investigated the effect of explicit heterosexism (self-reported attitudes toward gay men) on anticipated patient behavior and intention to prescribe PrEP to an MSM patient (Figure 1: Model C). We predicted that participants who expressed stronger heterosexism would, regardless of the race of the MSM patient, judge him as being more likely to increase condomless sex, more likely to engage in extra-relational sex, and less likely to adhere to his PrEP regimen, and that these judgments about the patient would be associated with lower intention to prescribe PrEP to him.
Beyond our primary objectives and hypotheses, we also conducted exploratory analyses. Although the sample size produced limited statistical power for testing complex interactions, we investigated the combined effect of racism and heterosexism on PrEP clinical decision-making for a Black MSM patient (Figure 1: Models D–E). Additionally, with an eye toward solutions, we examined the extent to which prior PrEP education affected clinical judgments and buffered any indirect effects identified (Figure 1: Models F–G).
Figure 1. Conceptual models.
To test our racism hypotheses, anticipated increase in condomless sex was examined as a single mediator of the relationship between patient race and participants’ intention to prescribe PrEP to him. Two other anticipated behaviors (extra-relational sex and adherence) were added as parallel mediators in a multiple-mediator model (Model A). Racism was examined as a moderator of this multiple-mediator model (Model B). To test our heterosexism hypothesis, all three anticipated patient behaviors were considered as parallel mediators of the relationship between heterosexism and intention to prescribe (Model C). In our exploratory analyses, we tested racism and heterosexism as additive (Model D) and interactive (Model E) moderators of the multiple mediator model in which patient race indirectly affected intention to prescribe via the three anticipated patient behaviors. We also explored prior PrEP education as a moderator of any indirect effects identified in our primary analyses, considering prior PrEP education as a moderator of the pathways between the focal predictor (patient race, racism, and/or heterosexism) and clinical judgments (Model F) as well as considering prior PrEP education as a moderator of the pathways between anticipated patient behavior and intention to prescribe (Model G).
METHODS
Study procedures, the clinical vignette, and relevant survey measures were adapted from the earlier study reporting racial bias in medical students’ PrEP-related clinical decision-making [23].
Participants and Procedures
An online, clinical vignette-based survey was conducted with 115 US medical students. Participants were recruited via mass email to all students enrolled at two medical schools in the northeastern US in the fall of 2015 using internal email distribution lists. Participants were asked about their familiarity with PrEP and prior medical education about PrEP. Subsequently, they were provided with background information about PrEP, including the clinical efficacy and US Food and Drug Administration’s approval of Truvada® (i.e., tenofovir disoproxil fumarate with emtricitabine) for PrEP, as well as supporting and opposing arguments for prescribing PrEP. Participants were then presented with a clinical vignette describing a hypothetical patient requesting PrEP. Participants were asked to make a series of clinical judgments about the vignette patient, including anticipated behavior while taking PrEP and intention to prescribe PrEP to the patient. Additionally, they completed measures of racism, heterosexism, and background characteristics. At the conclusion of the survey, participants were presented with a statement of current evidence concerning PrEP use and risk compensation and provided with a link to the U.S. Centers for Disease Control and Prevention website for more information about PrEP. Participation was compensated via entry into a gift card lottery. This research was approved by Yale University’s institutional review board prior to inception.
Clinical Vignette
The vignette described a 31-year-old male patient requesting a prescription for PrEP. The patient was described as being in a monogamous relationship with a male sex partner who was HIV-infected and not virally suppressed, and using condoms inconsistently during anal sex with this partner. Participants were further informed that the patient was confirmed to be HIV-uninfected, was in good health with an otherwise unremarkable medical history, and had insurance that would cover the PrEP prescription. The vignette and preceding background information are provided in full in a supplemental electronic appendix (Appendix 1). As in the earlier study from which the vignette was adapted [23], we systematically varied the race of the patient. Participants were randomly assigned to read a vignette about a Black patient or a White patient. All other details of the vignette were held constant across participants.
Measures
PrEP familiarity was measured with a single item: “How would you describe your current knowledge/familiarity with PrEP?” Participants rated their familiarity on a four-point scale ranging from “Not familiar at all (this is my first time hearing about PrEP)” to “Very familiar (I know a lot of information about PrEP, including details such as recent clinical trial results).” The variable was subsequently dichotomized such that “Not familiar at all (this is my first time hearing about PrEP)” was recoded as “Never heard of PrEP” and the other three response options were recoded as “Heard of PrEP.” Prior PrEP education was measured with a single dichotomous (“Yes”/“No”) item: “Have you learned about PrEP as part of your medical or nursing school training?” The item was worded to be applicable to both medical and nursing school students because we had considered surveying both, but ultimately surveyed only medical students due to limited resources.
Clinical judgments about the vignette patient included anticipated patient behavior while taking PrEP (anticipated increase in condomless sex, anticipated extra-relational sex, and anticipated PrEP adherence) and intention to prescribe PrEP. All were single-item measures and most were derived from the earlier study [23]. Anticipated increase in condomless sex was measured with a single item: “How likely would this patient be to have MORE unprotected sex (sex without condoms) if he started taking Truvada as PrEP?” Participants responded using a five-point scale ranging from “Not at all likely” to “Extremely likely.” Anticipated extra-relational sex was measured with the item “How likely would this patient be to start having sex with other partners (outside of his current relationship) if he started taking Truvada as PrEP?,” for which participants used the same five-point rating scale. Anticipated PrEP adherence was measured with the item “If you were to prescribe Truvada to this patient as PrEP, how ADHERENT do you think he would be?”, to which participants responded using a five-point scale ranging from “Not at all adherent” to “Extremely adherent.” Finally, intention to prescribe PrEP was measured with the item “Would you prescribe Truvada as PrEP to this patient?”, to which participants responded using a five-point scale ranging from “Definitely not” to “Definitely yes.”
Social biases included three measures of racism and one measure of heterosexism. All were administered after clinical judgments about the vignette patient were completed.
Explicit racism was measured using the Modern Racism Scale [30], a widely-used, psychometrically-established, seven-item measure of anti-Black racial attitudes. Sample items include “Discrimination against Blacks is no longer a problem in the United States” and “Blacks should not push themselves where they are not wanted.” Participants rated their responses on a five-point scale ranging from “Strongly disagree” to “Strongly agree.” Items were reverse-scored as appropriate and averaged to create an index score of explicit racism (Cronbach’s α = .85), with higher index scores indicating higher racism (i.e., more negative attitudes toward Black people).
Two implicit forms of racism were measured using implicit association tests (IATs) [31, 32]. An IAT is a computerized measure of implicit bias assessed over a series of trials. Visual and verbal stimuli are presented on a computer screen and participant bias is determined by reaction time. Quicker reaction times occur with associated concepts. The IAT effect measure is a D score, which has a theoretical range of −2 to 2. For both IATs used in the present study, visual stimuli were changed from the standard IAT images used to assess racial bias (Black and White faces of both men and women) to be specific to Black and White MSM. This was done because our clinical vignette patients were Black and White MSM and we were aware that bias could vary substantially according to intersecting social statuses. For example, Black MSM and Black heterosexual men are differentially stereotyped despite both being Black [25]. By using visual stimuli representing Black and White MSM in particular, we hoped to capture implicit biases most relevant to these groups. Visual stimuli used to represent Black and White MSM included images of same-race male couples, same-race men’s hands intertwined, and men of each race standing alone in front of a rainbow flag (a symbol of gay pride).
Implicit racial prejudice was assessed using a standard set of verbal stimuli (e.g., “marvelous,” “superb,” “joyful,” “tragic,” “horrible,” “awful”) that participants classified as Good or Bad. Higher scores indicated a more negative general evaluation of Black MSM versus White MSM and, thus, higher implicit racial prejudice. In the absence of an existing IAT to measure implicit sexual risk stereotypes, implicit risk-related racial stereotypes were assessed using a newly created set of verbal stimuli (“safe,” “careful,” “condoms,” “conscientious,” “promiscuous,” “risky,” “careless,” “unprotected”) that participants classified as Sexually Responsible or Sexually Reckless. Higher scores indicated a stronger association of Black versus White MSM with sexual risk and thus stronger implicit risk-related racial stereotypes.
Heterosexism, operationalized as negative attitudes toward gay men, was measured using a published short form of the revised Attitudes Toward Gay Men Scale (ATG-R-S5) [33]. The measure included five items that assessed participants’ attitudes about male homosexuality, including “Male homosexuality is a natural expression of sexuality in men” (reverse-scored) and “Sex between two men is just plain wrong.” Participants rated their responses on a five-point scale ranging from “Strongly disagree” to “Strongly agree.” Items were reverse-scored as appropriate and averaged to create an index score of heterosexism (Cronbach’s α = .81), with higher index scores indicating stronger heterosexism (i.e., more negative attitudes toward gay men).
Background characteristics reported by participants included age, race/ethnicity, gender, sexual orientation, and years of medical school completed.
An attention/manipulation check item was included to verify that participants had appropriately attended to the race of the patient described in the clinical vignette. Specifically, they were asked to report patient race in a multiple-choice item positioned toward the end of the survey, deliberately separated from the vignette by multiple other measures.
Analyses
A total of 115 medical students completed all relevant survey measures and were included in the full analytic sample. The full analytic sample was used for analyses that did not include vignette patient race or implicit racism. For analyses including patient race, we restricted the analytic sample to participants who passed the attention/manipulation check by correctly identifying the vignette patient’s race (n = 76). For analyses including implicit racism, sample size was limited by non-completion of IATs (n = 27 non-completers of 115) and, among IAT completers, exclusion based on excessively high IAT completion times (>3 standard deviations above the mean; n = 2), resulting in an analytic sample of 86 participants. For analyses involving both patient race and implicit racism, both restrictions were imposed, resulting in an analytic sample of 62.
Statistical analyses were performed using IBM SPSS Statistics software (Version 24). Frequencies and means were calculated to describe the sample and measures of interest. Independent samples t-tests and bivariate correlations were conducted to assess associations among background characteristics, racism, heterosexism, and clinical judgments of patients. Mediation, moderation, and moderated mediation (conditional process) analyses were conducted using Hayes’ PROCESS macro (Version 2.16.3 and corresponding templates; www.processmacro.org) [34, 35]. Moderated mediation occurs when an indirect effect systematically differs based on the level of another variable (the moderator) [35]. For example, one of the models we explored examined whether the indirect effects of heterosexism on intention to prescribe PrEP varied based on prior PrEP education. For mediation and moderated mediation analyses, we used the PROCESS macro to generate 10,000 bootstrapped samples from which bias-corrected bootstrap confidence intervals were established to estimate indirect effects. Early analytic methods for testing mediation such as Baron and Kenny’s causal steps approach did not involve direct calculation of an indirect effect and instead inferred this effect from constituent paths. Bootstrapping is analytically superior because it directly quantifies the indirect effect. Additionally, bootstrapping is not preconditioned on the existence of a significant bivariate association between the focal predictor and outcome (e.g., heterosexism and intention to prescribe PrEP) [34].
Racism analyses
We performed mediation, moderation, and moderated mediation analyses to evaluate our racism hypotheses. We first tested the single-mediator model reported in the earlier medical student study [23], according to which patient race indirectly affected intention to prescribe PrEP via anticipated increase in condomless sex. We also tested a multiple-mediator model that included the other two anticipated patient behaviors (extra-relational sex and adherence) as parallel mediators (Figure 1: Model A). Subsequently, explicit and implicit measures of racism were tested in separate models as moderators of the relationship between patient race and each of the four clinical judgments (anticipated increase in condomless sex, anticipated extra-relational sex, anticipated adherence, and intention to prescribe PrEP). Any measure of racism that significantly moderated the effect of patient race on one or more clinical judgments was examined as a moderator of the multiple-mediator model, moderating the pathways between patient race and anticipated behavior as well the pathway between patient race and intention to prescribe PrEP (Figure 1: Model B; PROCESS Template Model 8). When significant effects of patient race were detected in the analyses testing our racism hypotheses, we repeated the analyses adding to the analytic sample those participants who failed the attention/manipulation check to determine whether results were maintained when the attention/manipulation check was not treated as a basis for exclusion.
Heterosexism analysis
To evaluate the hypothesized indirect effect of heterosexism on intention to prescribe PrEP to an MSM patient (irrespective of patient race), we tested a multiple-mediator model that included all three anticipated patient behaviors as parallel mediators of the relationship between heterosexism and intention to prescribe PrEP (Figure 1: Model C).
Exploratory analyses
Combined racism and heterosexism analyses
Our exploratory analyses related to the combined effect of racism and heterosexism on PrEP clinical-decision making were intended to determine whether these social biases could jointly or interactively affect intention to prescribe PrEP to a Black MSM patient. Merging the models assessed in the racism and heterosexism analyses, we considered racism and heterosexism as concurrent moderators of the indirect effect of patient race on intention to prescribe via the three anticipated patient behaviors. Specifically, with respect to the multiple-mediator model, we tested them as additive moderators of the pathways between patient race and all clinical judgments (Figure 1: Model D; PROCESS Template Model 10; “first stage dual moderated mediation” [35]). We repeated this analysis considering racism and heterosexism as interactive rather than additive moderators (Figure 1: Model E; PROCESS Template Model 12; “first stage moderated moderated mediation” [35, emphasis added]).
Prior PrEP education analyses
Our exploratory analyses related to prior PrEP education were intended to determine whether prior PrEP education may buffer the identified indirect effects. We assessed prior PrEP education as a moderator of the multiple-mediator models in which significant indirect effects were identified in our primary analyses. We considered both (a) prior PrEP education as a moderator of the pathways between the focal predictor and clinical judgments (Figure 1: Model F; PROCESS Template Model 8) and (b) prior PrEP education as a moderator of the pathways between anticipated patient behavior and intention to prescribe PrEP (Figure 1: Model G; PROCESS Template Model 14). For instance, when considering the multiple-mediator model in which heterosexism indirectly affected intention to prescribe via anticipated patient behavior, we tested both (a) prior PrEP education as a moderator of the path between heterosexism and clinical judgments (as education that the majority of MSM PrEP patients do not increase condomless sex, for example, may buffer the impact of heterosexism on anticipated increase in condomless sex) and (b) prior PrEP education as a moderator of the pathways between anticipated behavior and intention to prescribe PrEP (as education that the HIV protection conferred by PrEP is not fully offset by increased condomless sex, for example, may buffer the impact of anticipated increase in condomless sex on intention to prescribe PrEP).
For all primary and exploratory mediation, moderation, and moderated mediation analyses, analyses were repeated adjusting for relevant background characteristics to determine whether effects were maintained when these variables were included in the model. Relevant background characteristics included conceptually related sociodemographic characteristics and other background characteristics empirically related to one or more clinical judgments as determined by correlations and independent samples t-tests. Relevant background characteristics were gender, sexual orientation, race/ethnicity, and years of medical school completed. For analyses involving patient race, measures of racism (explicit racism, implicit racial prejudice, and implicit risk-related racial stereotypes) were also considered as potential covariates. Based on the random assignment of participants to the Black and White patient conditions, we anticipated comparable levels of racism across the two conditions. However, we found that explicit racism was higher in the Black patient condition in the unrestricted analytic sample (n = 115) as well as when the sample was restricted to those who passed the manipulation check (n = 76), had valid IATs (n = 86), or both (n = 62). No significant differences in the implicit measures were found across the two conditions. Therefore, in analyses involving patient race as the focal predictor but not focusing on the moderating effects of explicit racism (i.e., when unmoderated mediation or the moderating effects of implicit racism were of primary conceptual interest), we included explicit racism along with relevant background characteristics in adjusted models. In mediation and moderated mediation models considering heterosexism as the focal predictor, we included patient race (study condition) in adjusted models.
RESULTS
Sample characteristics
The original and follow-up reminder emails advertising the study were distributed to 854 US medical students (October–November 2015). A total of 169 individuals (20%) enrolled, 115 (68%) of whom completed all self-report survey measures and were therefore included in the full analytic sample. This overall response rate of 13% is similar to or higher than several other recently-published survey studies of provider attitudes toward PrEP [16, 36, 37], albeit lower than the study of medical students after which the present work was modeled [23]. We were unable to compare background characteristics of survey completers versus non-completers because items assessing these characteristics were presented toward the end of the survey, after most non-completers had discontinued participation. However, we were able to compare survey completers to combined enrollment statistics for the two medical schools and found that a larger percentage of our study sample was White (62% of study sample versus 50% of all medical students) and female (67% versus 49%, respectively). Participants ranged in age from 21 to 35 years [M(SD) = 24.58(2.25)]. The majority (85%) had previously heard of PrEP and 50% reported having learned about PrEP as part of their medical school training. Additional background characteristics are displayed in Table I.
Table I.
Sample Characteristics (n = 115)
| n (%) | |
|---|---|
| Age | |
| <25 years | 64 (55.7) |
| ≥25 years | 51 (44.3) |
| Race/Ethnicity | |
| White | 71 (61.7) |
| Asian | 30 (26.1) |
| Black/African American | 7 (6.1) |
| Latino/Hispanic | 5 (4.3) |
| Other | 2 (1.7) |
| Gender | |
| Female | 77 (67.0) |
| Male | 37 (32.2) |
| Other | 1 (0.9) |
| Sexual Orientation | |
| Heterosexual | 99 (86.1) |
| Bisexual | 6 (5.2) |
| Gay/Lesbian | 6 (5.2) |
| Other | 4 (3.5) |
| Years of Medical School Completed | |
| 0 | 26 (22.6) |
| 1 | 38 (33.0) |
| 2 | 27 (23.5) |
| 3 | 19 (16.5) |
| ≥4 | 5 (4.3) |
| PrEP Familiarity | |
| Heard of PrEP | 98 (85.2) |
| Never heard of PrEP | 17 (14.8) |
| Prior PrEP Education | |
| Learned about PrEP in medical school | 58 (50.4) |
| Did not learn about PrEP in medical school | 57 (49.6) |
No significant differences in explicit racism, implicit racial prejudice, implicit risk-related racial stereotypes, or heterosexism were found by age, race/ethnicity, gender, years of medical school completed, medical school attended, or prior PrEP education. The only background characteristic significantly associated with any social biases was sexual orientation, which was associated with explicit racism and heterosexism: Participants who identified as heterosexual reported higher levels of explicit racism (t(113) = 2.19, p = .030) and higher levels of heterosexism (t(110) = 5.98, p<.001) than those identifying with another sexual orientation.
Descriptive analyses of clinical judgments
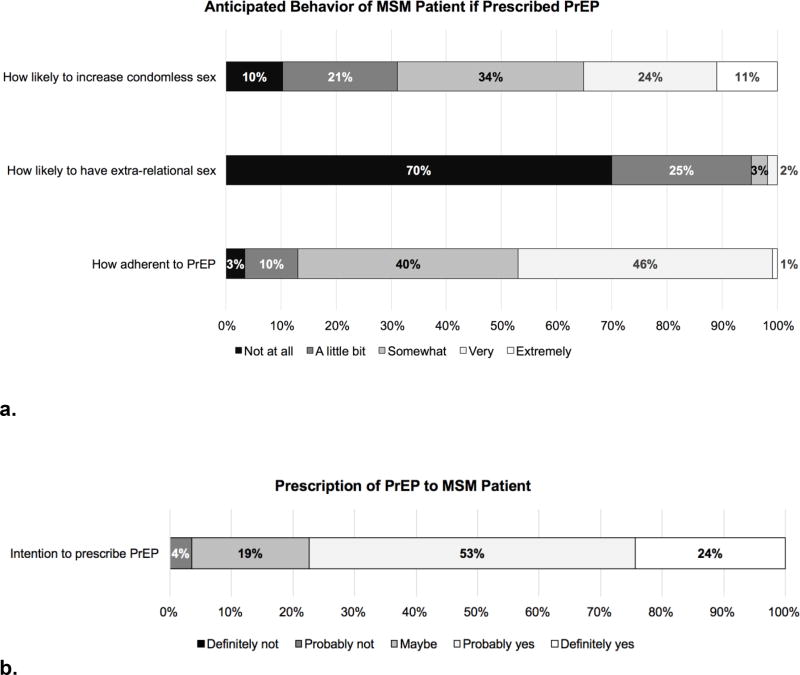
Clinical judgments about the vignette patient, including anticipated behavior while taking PrEP and intention to prescribe PrEP, are presented in Figure 2. Overall, participants commonly anticipated that the hypothetical patient would engage in risk compensation, with 90% of participants reporting some likelihood that the patient would engage in increased condomless sex and 30% reporting some likelihood that the patient would start having sex with other partners (despite the vignette explicitly stating that the patient and his partner were monogamous). Less than half of participants (47%) anticipated the patient would be “very” or “extremely” adherent to PrEP, suggesting most anticipated suboptimal adherence. The majority of participants (77%) reported that they would probably or definitely prescribe PrEP to the patient.
Figure 2. Clinical judgments of a hypothetical MSM patient seeking a prescription for PrEP (n = 115).
After being presented with a vignette describing an MSM patient seeking a prescription for PrEP, participants rated (a) anticipated patient behavior and (b) intention to prescribe PrEP.
Bivariate analyses of heterosexism, racism, and clinical judgments
Table II displays correlations among racism, heterosexism, and clinical judgments about the patient, including anticipated patient behavior while taking PrEP and intention to prescribe PrEP to the patient. Explicit racism was correlated with implicit risk-related racial stereotypes, anticipated extra-relational sex, and intention to prescribe PrEP, with participants higher in explicit racism exhibiting stronger risk-related racial stereotypes, judging the patient as more likely to engage in extra-relational sex, and reporting lower intention to prescribe. Implicit racial prejudice and implicit risk-related stereotypes were positively correlated with one another but unrelated to heterosexism, anticipated patient behavior, and intention to prescribe PrEP. Heterosexism was significantly correlated with anticipated patient behavior, with participants higher in heterosexism judging the patient to be more likely to increase condomless sex and less likely to be adherent. All three anticipated behaviors were significantly correlated with intention to prescribe PrEP, such that participants who judged the patient as more likely to increase condomless sex, more likely to engage in extra-relational sex, and less likely to be adherent expressed lower intention to prescribe PrEP to him. Correlations among racism, heterosexism, and clinical judgments stratified by patient race (study condition) are presented in Appendix 2: Table 1.
Table II.
Bivariate Correlations Among Main Measures and Differences in Means by Prior PrEP Education
| Pearson Correlation Coefficient (r) | Full Samplea |
Subsample with Prior PrEP Educationa |
Subsample with No Prior PrEP Educationa |
Prior PrEP Education vs. No prior PrEP Education |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||||||
| Measureb | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | M (SD) | M (SD) | M (SD) | p |
|
|
|
|||||||||||
| 1 Explicit Racism | - | 1.72 (.53) | 1.76 (.55) | 1.68 (.52) | .443 | |||||||
| 2 Implicit Racial Prejudice | .14 | - | .31 (.41) | .39 (.36) | .23 (.45) | .072† | ||||||
| 3 Implicit Risk-Related Racial Stereotypes | .26* | .24* | - | .13 (.39) | .07 (.39) | .21 (.38) | .101 | |||||
| 4 Heterosexism | .14 | .14 | .06 | - | 1.40 (.67) | 1.42 (.68) | 1.38 (.68) | .754 | ||||
| 5 Anticipated Increase in Condomless Sex | .05 | .10 | .15 | .20* | - | 3.03 (1.14) | 2.84 (1.14) | 3.23 (1.12) | .071† | |||
| 6 Anticipated Extra-Relational Sex | .24** | .16 | .13 | .17† | .05 | - | 1.37 (.64) | 1.36 (.64) | 1.39 (.65) | .843 | ||
| 7 Anticipated PrEP Adherence | −.11 | .14 | .13 | −.20* | −.13 | −.21* | - | 3.31 (.80) | 3.38 (.79) | 3.25 (.81) | .372 | |
| 8 Intention to Prescribe PrEP | −.20* | .04 | .04 | −.15 | −.28** | −.31** | .41** | - | 3.98 (.76) | 3.91 (.73) | 4.05 (.79) | .330 |
The full analytic sample included 115 participants (n = 58 with prior PrEP education, n = 57 with no prior PrEP education). For the implicit racism measures only, the analytic sample included 86 participants (n = 45 with prior PrEP education, n = 41 with no prior PrEP education).
Participants responded to self-report survey measures using five-point rating scales. Explicit racism represents an index score based on seven items assessing attitudes toward Black Americans (Modern Racism Scale), with higher values indicating stronger racism (more negative attitudes toward Black Americans). Heterosexism represents an index score based on five items assessing attitudes toward gay men (Attitudes Toward Gay Men Scale; ATG-R-S5), with higher values indicating stronger heterosexism (more negative attitudes toward gay men). Anticipated increase in condomless sex, anticipated extra-relational sex, anticipated PrEP adherence, and intention to prescribe PrEP represent single-item measures, with higher values indicating stronger anticipation or intention. Implicit racial prejudice and implicit risk-related racial stereotypes represent D scores generated by implicit association tests, which are computerized response-latency tasks that measure implicit bias. Higher scores indicate stronger prejudice toward Black versus White MSM and stronger association of Black versus White MSM with sexual risk, respectively.
p < .10
p < .05
p < .01
Table II also presents means and standard deviations for racism, heterosexism, and clinical judgments for the full sample and separately for participants with prior PrEP education and those without prior PrEP education. Independent samples t-tests detected no significant differences between PrEP education groups, suggesting prior PrEP education did not significantly impact social biases or clinical judgments of the patient.
Mediation, moderation, and moderated mediation analyses testing primary conceptual models
Racism analyses
Mediation analyses were performed to test for replication of the indirect effect of patient race on intention to prescribe PrEP via anticipated increase in condomless sex [23] as well as to test a multiple-mediator model in which anticipated extra-relational sex and anticipated adherence were added as parallel mediators (Figure 1: Model A). All indirect, contrast, direct, and total effects are presented in Appendix 2: Table 2. No significant indirect effect via anticipated increase in condomless sex was detected in the unadjusted or adjusted single- or multiple-mediator models. In the unadjusted multiple-mediator model, a single specific indirect effect emerged: The Black patient was judged as more likely than the White patient to engage in extra-relational sex, which, in turn, was associated with lower intention to prescribe. This effect was not significant in the adjusted model or when participants who failed the attention/manipulation check were included in the analytic sample.
No interaction effects of race and racial bias on clinical judgment were detected for models in which racism was operationalized as explicit racism or implicit racial prejudice. This was true for both adjusted and unadjusted models. When racism was operationalized as risk-related racial stereotypes, a single significant interaction effect emerged in the unadjusted model (b = .69, SE = .33, p = .042; ΔR2 = .07). The Black patient was judged as more likely to engage in extra-relational sex than the White patient among medical students who more strongly endorsed risk-related racial stereotypes. This interaction was not significant in the adjusted model (b = .59, SE = .36, p =.108) or when participants who failed the attention/manipulation check were included in the analytic sample.
In approaching the moderated mediation analysis to test whether racism moderated the indirect effect of patient race on intention to prescribe via the three anticipated patient behaviors (Figure 1:Model B), we considered as potential moderators of the indirect effects only those racism measures that showed a significant interaction effect relative to any of the clinical judgments. A single racism measure – implicit risk-related racial stereotypes – met this criterion, so only this single racism measure was tested in the moderated mediation model. When testing implicit risk-related racial stereotypes as a moderator of the multiple-mediator model, indices of moderated mediation indicated no significant moderated mediation effects in either adjusted or unadjusted models. (See Appendix 2: Table 3 for index scores.)
Heterosexism analysis
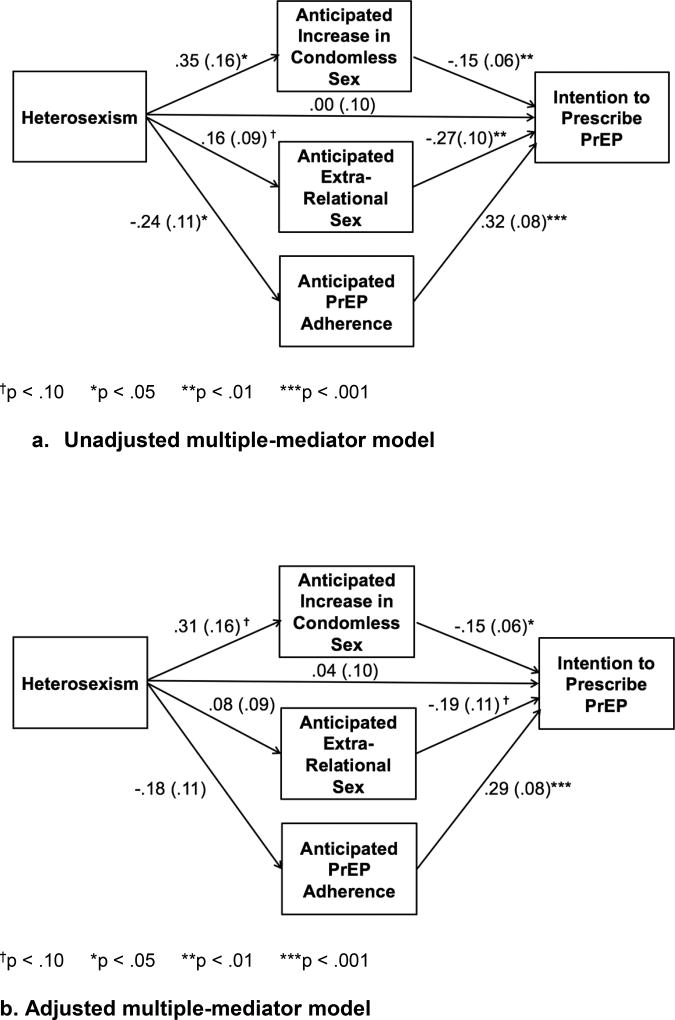
A multiple-mediator model was tested to examine the indirect effect of heterosexism on intention to prescribe PrEP via the three anticipated patient behaviors (Figure 1: Model C). Results of this analysis are displayed in Figure 3, with all indirect, contrast, direct, and total effects presented in Appendix 2: Table 2. Testing of our unadjusted multiple-mediator model, which contained all three anticipated behaviors (anticipated increase in condomless sex, anticipated extra-relational sex, and anticipated adherence) as parallel mediators, showed that each behavior uniquely mediated the relationship even when adjusting for the other two. Pairwise contrasts of specific indirect effects revealed no significant difference in their magnitude. The analysis was rerun adjusting for relevant background characteristics and patient race (i.e., study condition). In the adjusted model, only one of the three indirect effects, the one through anticipated increase in condomless sex, remained significant. However, none of the background characteristics were significantly associated with intention to prescribe PrEP in the adjusted multiple-mediator model and all pairwise contrasts of specific indirect effects were again non-significant, suggesting the magnitude of the indirect effects did not differ.
Figure 3. a and b. Results of Mediation Analyses.
Unstandardized coefficients and standard errors of all paths of the heterosexism multiple-mediator model, (a) unadjusted and (b) adjusted for relevant background characteristics (gender, sexual orientation, race, and years of medical school completed) and patient race (i.e., study condition). Bias-corrected 95% confidence intervals (CIs) were generated from 10,000 bootstrapped samples to estimate indirect effects. In the unadjusted model, all three specific indirect effects were significant (anticipated increase in condomless sex: −.05, SE = .03, CI = [−.142, −.011]; anticipated extra-relational sex: −.04, SE = .03, CI = [−.114, −.005]; anticipated PrEP adherence: −.08, SE = .04, CI = [−.190, −.012], p < .05). In the adjusted model, only the specific indirect effect via increased condomless sex remained significant (−.05, SE = .03, CI = [−.132, −.007], p < .05). Tests of moderated mediation (not shown) indicated that prior PrEP education did not significantly moderate either the unadjusted or adjusted multiple mediator model.
Exploratory analyses
The following results of exploratory analyses should be interpreted with caution because sample size limited statistical power to detect significant effects.
Combined racism and heterosexism analyses
In approaching the moderated mediation analyses combining racism and heterosexism in a single model, we considered only the single measure of racism that showed a significant interaction effect relative to any of the clinical judgments: implicit risk-related racial stereotypes. As indicated by indices of partial moderated mediation and moderated moderated mediation [35], there was no evidence of implicit risk-related stereotypes and heterosexism operating as either additive moderators (Figure 1: Model D) or interactive moderators (Figure 1: Model E) of the multiple-mediator model in which patient race was indirectly associated with intention to prescribe via the three anticipated patient behaviors. (See Appendix 2: Table 3 for index scores.)
Prior PrEP education analyses
For our exploratory analyses involving prior PrEP education, we investigated prior PrEP education as a moderator of those multiple-mediator models in which one or more significant indirect effects were identified in our primary analyses. This included the multiple-mediator model in which patient race was the focal predictor and that in which heterosexism was the focal predictor. Moderated mediation analyses did not support prior PrEP education as a significant moderator of either model. This was true whether we tested (a) prior PrEP education as a moderator of the pathways from the focal predictor (patient race or heterosexism) to clinical judgments (Figure 1: Model F) or (b) prior PrEP education as a moderator of the pathways from anticipated patient behavior to intention to prescribe PrEP (Figure 1: Model G). (See Appendix 2: Table 3 for index scores.)
DISCUSSION
With one in four sexually active MSM in the U.S. considered to be at high risk for HIV and indicated for PrEP [24] and nearly half of Black MSM predicted to acquire HIV in their lifetime [3], ensuring equitable access to PrEP and associated medical services is critical. Results of the present study highlight the potential for social biases held by healthcare providers to limit such access and suggest the need for PrEP education to more effectively address such biases. Whereas we found limited evidence for racial bias operating in medical students’ clinical judgments about the vignette patient, heterosexism indirectly affected intention to prescribe through multiple pathways: Medical students in our sample who expressed greater heterosexism more strongly anticipated risk compensation and adherence problems, and these anticipated patient behaviors were associated with lower intention to prescribe PrEP to the vignette patient. Prior PrEP education did not significantly affect clinical judgment and exploratory analyses did not yield support for prior PrEP education buffering these adverse effects.
Racism: Findings and Implications
The present work did not replicate previous vignette-based research demonstrating an indirect effect of patient race on intention to prescribe via anticipated increase in condomless sex [23], and we found only limited evidence of racial bias affecting intention to prescribe PrEP to a Black MSM patient in particular. This is especially notable because one of the two medical schools surveyed in the present research was the same medical school surveyed in the original study. Of the three indirect pathways hypothesized between patient race and prescribing intention, just one was significant: the Black patient was judged as more likely than the White patient to engage in extra-relational sex, which, in turn, was associated with lower intention to prescribe. Of the three measures of racial bias explored – explicit racism, implicit racial prejudice, and implicit risk-related racial stereotypes – only implicit risk-related racial stereotypes had a significant moderating effect on clinical judgment: Medical students who exhibited a stronger implicit association between Black MSM and sexual recklessness judged the Black patient as more likely than the White patient to engage in sex with new partners while taking PrEP, whereas students who exhibited the implicit Black MSM/recklessness association to a lesser extent did not demonstrate the same race-based difference in judgment. However, we note that neither of these race-related findings were maintained when we adjusted for relevant background characteristics and explicit racism, which by chance was higher among participants randomized to the Black patient condition. Thus, we consider these race-related findings to be tenuous, particularly when considered in the context of null findings relative to most of the race-related analyses conducted.
One possible explanation for the limited impact of patient race in the present research involves changes in the medical curriculum at the university surveyed at both time points. We are aware that between the two survey administrations (early 2013 and late 2015), an expert in cultural competence and implicit bias conducted training with medical students at that university, with much of the training focused on racial bias in particular. This training had not been offered prior to the first survey. Although we cannot be certain that all of the medical students from that university who completed the 2015 survey participated in the training, it is possible that for those who did, the training heightened awareness about their vulnerability to implicit bias and increased their conscientiousness about racial stereotyping when making judgments about the hypothetical patient in the present survey.
A second plausible explanation involves sociohistorical context: In the time that passed between administration of the original survey and the present one, the Black Lives Matter movement gained momentum and there was significant media attention related to racial profiling and the mistreatment of Black men. It is possible that this heightened social awareness about race, including contemporary race-related stereotypes, affected participants’ judgments of the Black MSM vignette patient. Indeed, the evolution of sociocultural context is a recognized barrier to exact study replication in the social sciences [38, 39].
Regardless of the reason for non-replication, our finding that patient race, participant racism, and their interaction appeared to have little effect on participants’ clinical judgments about the vignette patient is relatively encouraging with respect to actual patients of different races receiving equitable PrEP services within a clinical setting. Nevertheless, participants did show another form of bias that was systematically related to their intention to prescribe PrEP to an MSM patient: heterosexism.
Heterosexism: Findings and Implications
Overall, medical students commonly anticipated that the hypothetical MSM patient would engage in risk compensation if prescribed PrEP. This likely reflects pervasive sexual stereotypes of gay men as being promiscuous and sexually irresponsible [25]. Most participants also anticipated suboptimal adherence. Such assumptions are disconcerting because they were associated with lower intention to prescribe PrEP, suggesting that stereotypes could constrain PrEP access for MSM patients. These assumptions are additionally concerning because the description of the vignette patient was incompatible with the MSM promiscuity stereotype in several ways: The patient was described as being in a sexually monogamous relationship and had no history of sexually transmitted infections. He was also purposely described as medically uncomplicated with a clear indication for PrEP according to normative prescription guidance [40]. In actual clinical contexts, many MSM and other patients seeking PrEP are likely to have more complex social and medical circumstances that amplify concerns about risk compensation and adherence difficulties, ambiguate PrEP eligibility, and diminish prescribing intentions.
Our finding that heterosexism was indirectly related to intention to prescribe PrEP and therefore may operate as a barrier to PrEP access within the healthcare system is consistent with previous work implicating social [41] and structural [42] forms of heterosexism as barriers to PrEP access. To our knowledge, previous research has not directly examined the association between heterosexism and PrEP clinical decision-making among providers. To date, survey research that has assessed providers’ experiences prescribing PrEP or intentions to prescribe PrEP for MSM as compared to other HIV risk groups (such as heterosexual women and people who inject drugs) has not demonstrated a pattern of heterosexist bias [15, 43–48]. In fact, in multiple studies, providers have more commonly reported prior PrEP prescription [45–48] or intention/willingness to prescribe [15, 44] to MSM than to other groups. However, in qualitative research, some providers have expressed stereotypical views of MSM [17] and a corresponding preference to prescribe PrEP to heterosexual couples [17, 26]. Furthermore, current PrEP prescribers have reported observing a heterosexist bias in the clinical judgments made by other providers [27].
In addition to heterosexism interfering with PrEP access at social and structural levels, it could interfere at the individual level among MSM patients, deterring them from seeking PrEP, diminishing comfort disclosing same-sex behavior to providers, and reducing their likelihood of discussing PrEP with a provider [49, 50]. Thus, heterosexism could potentially limit PrEP access for MSM via multiple mechanisms and a multipronged approach to intervention will likely be necessary to preempt or reverse this outcome.
PrEP Education: Findings and Implications
Medical education is, in theory, a promising point of intervention to promote PrEP prescription and prevent provider bias from undermining PrEP access for MSM. Indeed, with respect to the limited impact of patient race and provider racial bias in the present research, we suggested that curricular innovations focusing on explicit and implicit racial bias may have been instrumental for reducing race-related biases in prescribing PrEP observed in earlier research. However, even if such an explanation were valid, we note the specificity of such effects: Although race and racial attitude effects were limited in the current sample, heterosexism was indirectly associated with lower prescribing intentions. Additionally, according to exploratory analyses, prior PrEP education in medical school—conceptualized generally as any versus none—did not appear to buffer adverse effects of patient race or heterosexism on PrEP clinical decision-making.
This pattern of evidence suggests that PrEP medical education programs that are specifically tailored to address particular types of social biases would be more effective than general PrEP medical education programs in promoting equitable clinical decision-making related to PrEP. Future studies are needed to determine the kinds of curriculum changes that will achieve this outcome. Incorporating information alerting medical students or practicing providers to how their attitudes toward different social groups can indirectly affect their decision about to whom they prescribe PrEP may be a particularly valuable element, and we recommend systematic comparison of programs that do and do not incorporate this content to evaluate the value added. Also, providing information about sexual behavior among patients to whom PrEP is prescribed, including concrete guidance about how to respond if PrEP patients report changing their behavior, within PrEP education programs may help to reduce uncertainty and prevent social biases from interfering with clinical judgment. Providers should be informed that risk compensation is not widely reported among PrEP users and is not a valid reason for withholding PrEP [51]. With respect to adherence, informing providers that there is some “forgiveness” associated with missing occasional doses of PrEP (MSM patients appear to obtain high protection even when taking only four of seven daily doses per week [5, 52]) may ease their concerns in this domain, as may information about the numerous adherence supports freely available to patients (e.g., smartphone apps [53]).
Many PrEP educational resources devote limited attention to cultural competence in caring for sexually diverse clientele. Familiarization with the disproportionate HIV risk of MSM and other social groups and training in patient-centered, non-judgmental sexual health communication should be integral components of PrEP educational programs. Use of a sex-positive approach that respects the sexual values, desires, and decisions of individual patients should be encouraged, and the potential for personal morals around partnering practices or other dimensions of sexuality to cloud clinical judgment [54] should be directly acknowledged. There are an increasing array of easily accessible in-person and online resources offering education about how to create safe and welcoming clinical environments for sexual and gender minority patients (e.g., www.lgbthealtheducation.org). Evidence-based educational strategies for combating bias and its harmful effects on patient care should also be incorporated, such as techniques that help people to recognize their biases, including those that are unconscious, and the unintentional impact on medical care that such biases may have [55].
Systematic evaluation of PrEP education with respect to both clinical and cultural competence outcomes is needed at all stages of medical training, from medical school through continuing medical education. Clinically, PrEP education should improve providers’ comfort and willingness to prescribe PrEP, particularly to patients who report ongoing behavior that puts them at substantial risk for HIV, as was the case with the patient in the study vignette. In terms of cultural competence evaluation, existing frameworks such as that put forward by Betancourt [56], which assesses change in attitudes, knowledge, and skill, are readily available and adaptable.
Limitations and Future Directions
This study had several limitations that are important to acknowledge and invite follow-up study. First, the sample was composed of medical students and findings do not necessarily generalize to practicing providers. Replication with practicing providers could lend insight into more immediate implementation challenges. That said, medical students are an important sector of health professionals to consider given their accessibility for early and accurate training and the decades of service they will subsequently offer. It is also important to note that our sample was drawn from medical schools in the northeastern US. Conducting similar studies with students and practicing providers from other healthcare professions and other geographic locations would help to establish generalizability and understand contextual nuances in PrEP-related training needs.
A second potential limitation is the background information about PrEP presented to participants prior to their completion of survey measures, provided in full in Appendix 1. Anticipating some students would have limited exposure to PrEP before taking the survey, we believed it was important to present both factual information about PrEP (e.g., clinical efficacy, US Food and Drug Administration’s approval) as well as arguments for and against its prescription to prepare them to make clinical judgments about a patient requesting PrEP. This presentation of background information was modeled after the original medical student study [23]. We used quotes from real people and websites to convey these arguments, including three supporting and three opposing claims to present a balanced view. Claims on both sides touched on risk compensation and adherence. This approach of presenting arguments for and against an issue and using quotations to communicate these arguments is a common technique used in social psychology. However, we acknowledge that the quoted material could have influenced participants’ clinical judgments about the vignette patient in either direction, and that participants with no prior learning about PrEP may have been especially impressionable. We think it is unlikely that the quotes presented influenced the effects of patient race, racism, heterosexism, or their interaction on clinical judgments, particularly because race and sexual orientation were not central to the quoted content. Nonetheless, future replication presenting only factual information would eliminate the possibility that the arguments for and against PrEP impacted results.
A third limitation is the measures we employed. Our measure of prior PrEP education was self-reported with a dichotomous “Yes”/“No” response option. Thus, we determined whether medical students had any prior PrEP education versus none, but did not capture dimensions of PrEP education such as content and format. Students from all years of medical school participated in our survey, and the nature and extent of prior PrEP education across years of medical school likely varied. More comprehensive measurement of PrEP-related medical education may help to capture these dimensions and differences and inform efforts to improve upon existing PrEP education programs.
An additional measurement consideration involves our measure of anticipated increase in condomless sex, which was a single item derived from the original medical student study [23]: “How likely would this patient be to have MORE unprotected sex (sex without condoms) if he started taking Truvada as PrEP?”. The item was developed based on healthcare providers’ commonly-expressed concern that patients may reduce condom use or otherwise increase their risk behavior with PrEP [15–20], and thus the wording of the item and response options (“Not at all likely” to “Extremely likely”) was designed to capture the magnitude of participants’ concern. This unidirectional approach to surveying providers about perceived impact of PrEP on risk behavior, according to which providers rate their perceptions related to a patient increasing (but not decreasing) such behavior, is consistent with past studies [16, 20]. However, it is possible that the directionality inherent in this phrasing may have been leading. Rewording the item and response options to also allow for reporting of anticipated decrease in condomless sex may yield a different response.
A final measurement consideration is our operationalization of heterosexism. The measure of heterosexism we used (ATG-R-S5 [33]) assessed self-reported agreement with a combination of statements expressing heterosexual presumption (i.e., the assumption that same-sex behavior is not normative) and deeper negative perceptions of MSM (e.g., as disgusting) that are more consistent with the older term “homophobia.” Both attitudinal dimensions of heterosexism could impede provision of evidence-based HIV prevention services and optimal patient care, and future work could tease apart how these and other dimensions of heterosexism differentially impact clinical decision-making. Also, we measured explicit sexual orientation attitudes in our study rather than including IATs or manipulating patient sexual orientation to tap into implicit manifestations of heterosexism. Replication of this work using heterosexism IATs or systematically varying patient sexual orientation and demonstrating that the mediational paths observed are stronger in a gay patient condition versus a heterosexual patient condition would strengthen our understanding about how sexual orientation negatively affects clinical decision-making related to PrEP.
Lastly, it is important to acknowledge that our sample size limited our statistical power to detect higher-order interaction effects. Thus, our null findings with respect to our exploratory analysis of the interactive moderating effect of racism and heterosexism should be interpreted with caution. A larger-scale study powered to detect such stigma interaction effects in this context is necessary to make more conclusive inferences.
Conclusion
This study advances our understanding of social biases in PrEP-related clinical decision-making and presents early evidence for the potential adverse impact of heterosexism. Medical students and practicing healthcare providers, like all members of society, are vulnerable to social biases. Whereas many healthcare providers may be familiar with race-based disparities in healthcare, and therefore may actively attempt to consider and correct for racial biases in their clinical practice [12], self-awareness about sexual orientation-based biases may be less common and manifest as unequal access to PrEP. Our findings call attention to the need for effective medical education to ensure that PrEP access for MSM and other social groups at disproportionately high risk for HIV is not compromised by heterosexism and other social biases.
Supplementary Material
Acknowledgments
The authors wish to thank the medical students who generously contributed their time and effort by participating in this study. We are also grateful to the medical faculty and student liaisons at participating institutions who supported our recruitment efforts. Funding and resources for this research were provided by the National Institute of Mental Health (NIMH) via Award Number K01-MH103080 (SKC). The efforts of SKC, DSK, and KU were supported by the NIMH via Award Numbers K01-MH103080 (SKC), K23-MH098795 (DSK), and K01-MH093273 (KU), and the efforts of VAE were supported by the Agency for Healthcare Research and Quality (AHRQ) via Award Number K12-HS022986. Additional support was provided through the District of Columbia Center for AIDS Research (P30-AI117870), the Yale University Center for Interdisciplinary Research on AIDS (P30-MH062294), and the Harvard University Center for AIDS Research (P30-AI060354), all funded by the National Institutes of Health. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH, AHRQ, or NIH.
SKC, DSK, and KHM have received compensation for their efforts in developing and/or delivering medical education related to PrEP. DSK and KHM have conducted research with unrestricted project support from Gilead Sciences and KHM has conducted research with unrestricted project support from Merck and ViiV Healthcare. KHM is a senior member of the faculty and advisory board of the National LGBT Health Education Center and an associate editor and contributor to educational materials provided through the organization’s website, to which readers of this article are referred. DSK and SKC have contributed to these educational materials as well.
Footnotes
Compliance with Ethical Standards
Research Involving Human Participants and/or Animals. All procedures performed in this study, which involved human participants, were in accordance with the ethical standards of Yale University’s institutional review board (IRB). IRB approval was obtained prior to study inception. This study did not involve non-human animals.
Disclosure of Potential Conflicts of Interest. The authors declare that they have no other conflicts of interest to disclose.
Informed Consent. Informed consent was obtained from all individual participants included in the study.
References
- 1.Centers for Disease Control and Prevention. HIV surveillance report: Diagnoses of HIV infections in the United States and dependent areas, 2015. 2016;27 available from: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf. [Google Scholar]
- 2.Purcell DW, Johnson CH, Lansky A, Prejean J, Stein R, Denning P, et al. Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. Open AIDS J. 2012;6(S1: M6):98–107. doi: 10.2174/1874613601206010098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hess KL, Hu X, Lansky A, Mermin J, Hall HA. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27(4):238–43. doi: 10.1016/j.annepidem.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson PL, Glidden DV, Liu A, Buchbinder S, Lama JR, Guanira JV, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4(151):151ra25. doi: 10.1126/scitranslmed.3004006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mera Giler R, Magnuson D, Trevor H, Bush S, Rawlings K, McCallister S. Changes in Truvada (TVD) for HIV pre-exposure prophylaxis (PrEP) utilization in the United States: (2012–2016). 9th International AIDS Society Conference on HIV Science (IAS 2017); Paris, France. 2017; [Abstract WEPEC0919] [Google Scholar]
- 7.Krakower DS, Mayer KH. The role of healthcare providers in the roll out of preexposure prophylaxis. Curr Opin HIV AIDS. 2016;11(1):41–8. doi: 10.1097/COH.0000000000000206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burke SE, Dovidio JF. Sexual prejudice (personality correlates of) In: Shackleford TK, Weekes-Shackleford V, editors. Encyclopedia of evolutionary psychological science. New York, NY: Springer; 2018. [Google Scholar]
- 9.Institute of Medicine. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 10.Penner LA, Blair IV, Albrecht TL, Dovidio JF. Reducing racial health care disparities: A social psychological analysis. Policy Insights Behav Brain Sci. 2014;1(1):204–12. doi: 10.1177/2372732214548430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Betancourt JR, Corbett J, Bondaryk MR. Addressing disparities and achieving equity: Cultural competence, ethics, and health-care transformation. Chest. 2014;145(1):143–8. doi: 10.1378/chest.13-0634. [DOI] [PubMed] [Google Scholar]
- 12.Penner LA, Dovidio JF. Racial color blindness and Black-White health care disparities. In: Neville HA, Gallardo ME, Sue DW, editors. The myth of racial color blindness: Manifestations, dynamics, and impact. Washington, DC: American Psychological Association; 2016. pp. 275–93. [Google Scholar]
- 13.Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: The implications of psychological processes for understanding racial disparities in health and health care. Soc Sci Med. 2008;67(3):478–86. doi: 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 14.Dovidio JF, Fiske ST. Under the radar: How unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. Am J Public Health. 2012;102(5):945–52. doi: 10.2105/AJPH.2011.300601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adams LM, Balderson B, Packett BJ, Brown KA, Catz SL. Providers' perspectives on prescribing pre-exposure prophylaxis (PrEP) for HIV prevention. HIV Specialist. 2015;7(1):18–25. [Google Scholar]
- 16.Blackstock OJ, Moore BA, Berkenblit GV, Calabrese SK, Cunningham CO, Fiellin DA, et al. A cross-sectional online survey of HIV pre-exposure prophylaxis adoption among primary care physicians. J Gen Intern Med. 2016 doi: 10.1007/s11606-016-3903-z. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Doblecki-Lewis S, Jones D. Community federally qualified health centers as homes for HIV preexposure prophylaxis: Perspectives from South Florida. J Int Assoc Provid AIDS Care. 2016;15(6):522–8. doi: 10.1177/2325957416661422. [DOI] [PubMed] [Google Scholar]
- 18.Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers' perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: A qualitative study. AIDS Behav. 2014;18(9):1712–21. doi: 10.1007/s10461-014-0839-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mullins TL, Zimet G, Lally M, Kahn JA. Adolescent human immunodeficiency virus care providers' attitudes toward the use of oral pre-exposure prophylaxis in youth. AIDS Patient Care STDS. 2016;30(7):339–48. doi: 10.1089/apc.2016.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petroll AE, Walsh JL, Owczarzak JL, McAuliffe TL, Bogart LM, Kelly JA. PrEP awareness, familiarity, comfort, and prescribing experience among US primary care providers and HIV specialists. AIDS Behav. 2017;21(5):1256–67. doi: 10.1007/s10461-016-1625-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Calabrese SK, Magnus M, Mayer KH, Krakower DS, Eldahan AI, Hawkins LAG, et al. Putting PrEP into practice: Lessons learned from early-adopting US providers' firsthand experiences providing HIV pre-exposure prophylaxis and associated care. PLoS One. 2016;11(6):e0157324. doi: 10.1371/journal.pone.0157324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krakower DS, Maloney KM, Grasso C, Melbourne K, Mayer KH. Primary care clinicians' experiences prescribing HIV pre-exposure prophylaxis at a specialized community health centre in Boston: Lessons from early adopters. J Int AIDS Soc. 2016;19(1):21165. doi: 10.7448/IAS.19.1.21165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Calabrese SK, Earnshaw VA, Underhill K, Hansen NB, Dovidio JF. The impact of patient race on clinical decisions related to prescribing HIV pre-exposure prophylaxis (PrEP): Assumptions about sexual risk compensation and implications for access. AIDS Behav. 2014;18(2):226–40. doi: 10.1007/s10461-013-0675-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith DK, Van Handel M, Wolitski RJ, Stryker JE, Hall HI, Prejean J, et al. Vital signs: Estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition - United States, 2015. Morb Mortal Wkly Rep. 2015;64(46):1291–5. doi: 10.15585/mmwr.mm6446a4. [DOI] [PubMed] [Google Scholar]
- 25.Calabrese SK, Earnshaw VA, Magnus M, Hansen NB, Krakower DS, Underhill K, et al. Sexual stereotypes ascribed to Black men who have sex with men: An intersectional analysis. Arch Sex Behav. 2017 doi: 10.1007/s10508-016-0911-3. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Puro V, Palummieri A, De Carli G, Piselli P, Ippolito G. Attitude towards antiretroviral pre-exposure prophylaxis (PrEP) prescription among HIV specialists. BMC Infect Dis. 2013;13:217. doi: 10.1186/1471-2334-13-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Calabrese SK, Magnus M, Mayer KH, Krakower DS, Eldahan AI, Gaston Hawkins LA, et al. “Support your client at the space that they’re in”: Pre-exposure prophylaxis (PrEP) prescribers’ perspectives on PrEP-related risk compensation. AIDS Patient Care STDS. 2017;31(4):196–204. doi: 10.1089/apc.2017.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Collins PH. Black sexual politics: African Americans, gender, and the new racism. New York, NY: Routledge; 2005. [Google Scholar]
- 29.McCune JQ., Jr . Sexual discretion: Black masculinity and the politics of passing. Chicago, IL: The University of Chicago Press; 2014. [Google Scholar]
- 30.McConahay JB. Modern racism, ambivalence, and the Modern Racism Scale. In: Dovidio JF, Gaertner SL, editors. Prejudice, discrimination, and racism. San Diego, CA: Academic Press; 1986. pp. 91–125. [Google Scholar]
- 31.Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: The implicit association test. J Pers Soc Psychol. 1998;74(6):1464–80. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- 32.Greenwald AG, Nosek BA, Banaji MR. Understanding and using the implicit association test: I. An improved scoring algorithm. J Pers Soc Psychol. 2003;85(2):197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- 33.Herek GM, McLemore KA. Attitudes toward lesbians and gay men scale. In: Fisher TD, Davis CM, Yarber WL, Davis SL, editors. Handbook of Sexuality-Related Measures. 3. New York, NY: Routledge; 2011. pp. 415–6. [Google Scholar]
- 34.Hayes AF. Introduction to mediation, moderation, and conditional process analysis. New York: Guilford Press; 2013. [Google Scholar]
- 35.Hayes AF. Partial, conditional, and moderated moderated mediation: Quantification, inference, and interpretation. Commun Monogr. 2017 Advance online publication. [Google Scholar]
- 36.Adams LM, Balderson BH. HIV providers' likelihood to prescribe pre-exposure prophylaxis (PrEP) for HIV prevention differs by patient type: A short report. AIDS Care. 2016;28(9):1154–8. doi: 10.1080/09540121.2016.1153595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bacon O, Gonzalez R, Andrew E, Potter MB, Iniguez JR, Cohen SE, et al. Brief report: Informing strategies to build PrEP capacity among San Francisco Bay Area clinicians. J Acquir Immune Defic Syndr. 2017;74(2):175–9. doi: 10.1097/QAI.0000000000001182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dovidio JF. Commentary: A big problem requires a foundational change. J Exp Soc Psychol. 2016;66:159–65. [Google Scholar]
- 39.Crandall CS, Sherman JW. On the scientific superiority of conceptual replications for scientific progress. J Exp Soc Psychol. 2016;66:93–9. [Google Scholar]
- 40.U.S. Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States: A clinical practice guideline. 2014 Available from: https://www.cdc.gov/hiv/pdf/prepguidelines2014.pdf.
- 41.Calabrese SK, Underhill K, Earnshaw VA, Hansen NB, Kershaw TS, Magnus M, et al. Framing HIV pre-exposure prophylaxis (PrEP) for the general public: How inclusive messaging may prevent prejudice from diminishing public support. AIDS Behav. 2016;20(7):1499–513. doi: 10.1007/s10461-016-1318-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oldenburg CE, Perez-Brumer AG, Hatzenbuehler ML, Krakower D, Novak DS, Mimiaga MJ, et al. State-level structural sexual stigma and HIV prevention in a national online sample of HIV-uninfected MSM in the United States. AIDS. 2015;29(7):837–45. doi: 10.1097/QAD.0000000000000622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hakre S, Blaylock JM, Dawson P, Beckett C, Garges EC, Michael NL, et al. Knowledge, attitudes, and beliefs about HIV pre-exposure prophylaxis among US Air Force health care providers. Medicine. 2016;95(32):e4511. doi: 10.1097/MD.0000000000004511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Edelman EJ, Moore BA, Calabrese SK, Berkenblit GV, Cunningham C, Patel V, et al. Primary care physicians’ willingness to prescribe HIV pre-exposure prophylaxis for people who inject drugs. AIDS Behav. 2017;21(4):1025–33. doi: 10.1007/s10461-016-1612-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smith DK, Mendoza MC, Stryker JE, Rose CE. PrEP awareness and attitudes in a national survey of primary care clinicians in the United States, 2009–2015. PLoS One. 2016;11(6):e0156592. doi: 10.1371/journal.pone.0156592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Krakower DS, Oldenburg CE, Mitty JA, Wilson IB, Kurth AE, Maloney KM, et al. Knowledge, beliefs and practices regarding antiretroviral medications for HIV prevention: Results from a survey of healthcare providers in New England. PLoS One. 2015;10(7):e0132398. doi: 10.1371/journal.pone.0132398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tellalian D, Maznavi K, Bredeek UF, Hardy WD. Pre-exposure prophylaxis (PrEP) for HIV infection: Results of a survey of HIV healthcare providers evaluating their knowledge, attitudes, and prescribing practices. AIDS Patient Care STDS. 2013;27(10):553–9. doi: 10.1089/apc.2013.0173. [DOI] [PubMed] [Google Scholar]
- 48.Weiser J, Garg S, Beer L, Skarbinski J. Prescribing of human immunodeficiency virus (HIV) pre-exposure prophylaxis by HIV medical providers in the United States, 2013–2014. Open Forum Infect Dis. 2017;4(1):ofx003. doi: 10.1093/ofid/ofx003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garcia J, Parker C, Parker RG, Wilson PA, Philbin M, Hirsch JS. Psychosocial implications of homophobia and HIV stigma in social support networks: Insights for high-impact HIV prevention among Black men who have sex with men. Health Educ Behav. 2016;43(2):217–25. doi: 10.1177/1090198115599398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maloney KM, Krakower DS, Ziobro D, Rosenberger JG, Novak D, Mayer KH. Culturally competent sexual healthcare as a prerequisite for obtaining preexposure prophylaxis: Findings from a qualitative study. LGBT Health. 2017 doi: 10.1089/lgbt.2016.0068. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Calabrese SK, Underhill K, Mayer KH. HIV Preexposure prophylaxis and condomless sex: Disentangling personal values from public health priorities. Am J Public Health. 2017 doi: 10.2105/AJPH.2017.303966. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: A cohort study. Lancet Infect Dis. 2014;14(9):820–9. doi: 10.1016/S1473-3099(14)70847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dayer L, Heldenbrand S, Anderson P, Gubbins PO, Martin BC. Smartphone medication adherence apps: Potential benefits to patients and providers. J Am Pharm Assoc. 2013;53(2):172–81. doi: 10.1331/JAPhA.2013.12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Calabrese SK, Mayer KH, Krakower DS, Magnus M, Underhill K, Earnshaw VA, Hansen NB, Kershaw TS, Betancourt JR, Dovidio JF. The potential for condom ideology to cloud clinical judgment around prescribing HIV pre-exposure prophylaxis (PrEP). HIV Research for Prevention Conference (HIVR4P 2016); Chicago, IL. 2016; [Abstract OA03.05] [Google Scholar]
- 55.Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: Lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–7. doi: 10.1007/s11606-007-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Betancourt JR. Cross-cultural medical education: Conceptual approaches and frameworks for evaluation. Acad Med. 2003;78(6):560–9. doi: 10.1097/00001888-200306000-00004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.